Detection and Evaluation for High-Quality Cardiopulmonary Resuscitation Based on a Three-Dimensional Motion Capture System: A Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
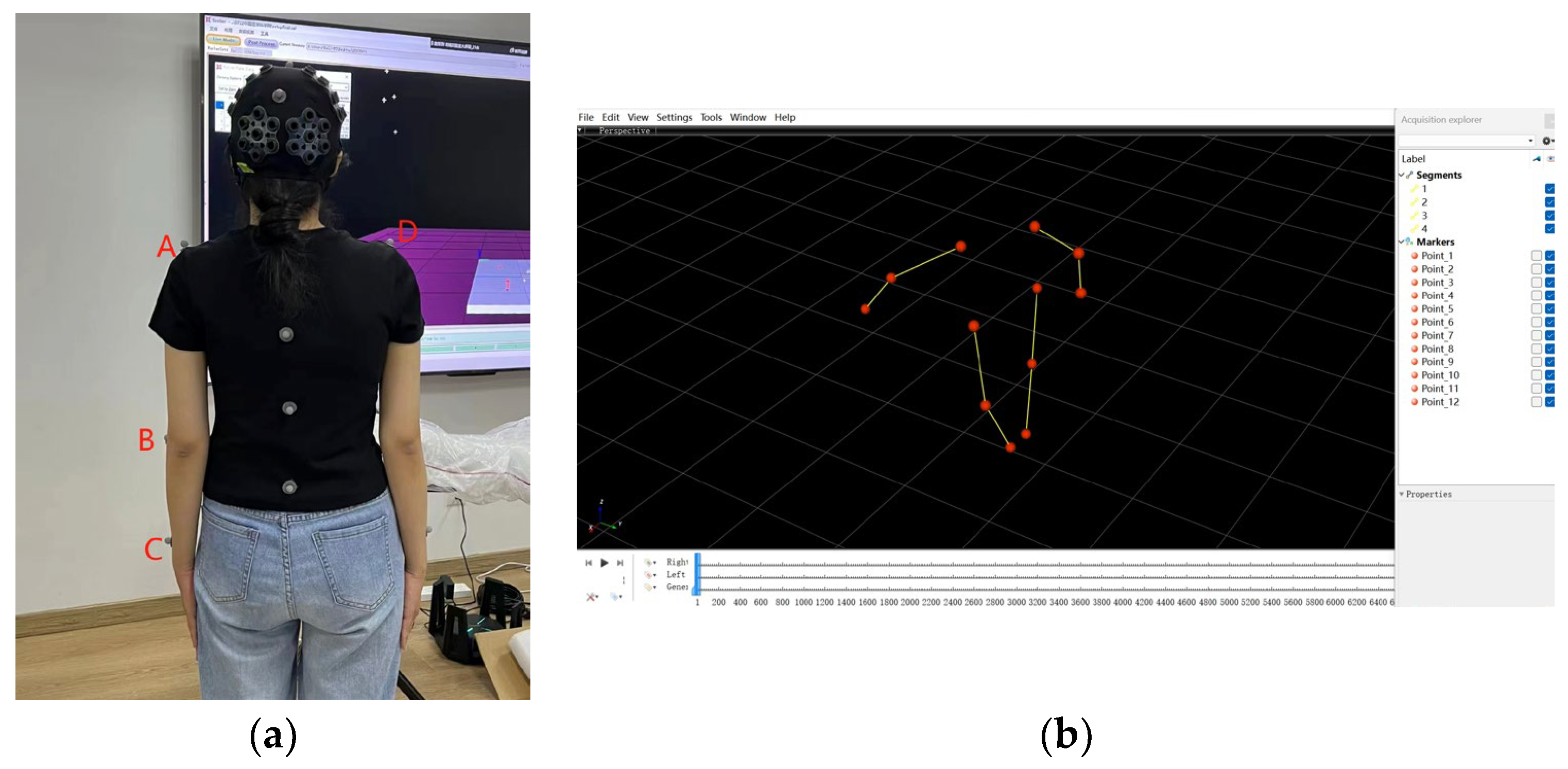
2.2. Experimental Setup
2.3. Procedures
2.4. Data Processing
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nishiyama, C.; Kiguchi, T.; Okubo, M.; Alihodzic, H.; Al-Araji, R.; Baldi, E.; Beganton, F.; Booth, S.; Bray, J.; Christensen, E.; et al. Three-year trends in out-of-hospital cardiac arrest across the world: Second report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 2023, 186, 109757. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Lai, H.Y.; Hsieh, T.C.; Wu, W.R. Using real-time device-based visual feedback in CPR recertification programs: A prospective randomised controlled study. Nurse Educ. Today 2023, 124, 105755. [Google Scholar] [CrossRef] [PubMed]
- Shao, F.; Li, H.; Ma, S.; Li, D.; Li, C. Outcomes of out-of-hospital cardiac arrest in Beijing: A 5-year cross-sectional study. BMJ Open 2021, 11, e041917. [Google Scholar] [CrossRef]
- Myat, A.; Song, K.J.; Rea, T. Out-of-hospital cardiac arrest: Current concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Lien, W.C.; Chang, C.H.; Chang, W.T.; Chen, W.J. Ultrasonographic Assessment During Cardiopulmonary Resuscitation. J. Vis. Exp. 2020, 164, e59144. [Google Scholar]
- Soreide, E.; Morrison, L.; Hillman, K.; Monsieurs, K.; Sunde, K.; Zideman, D.; Eisenberg, M.; Sterz, F.; Nadkarni, V.M.; Soar, J.; et al. The formula for survival in resuscitation. Resuscitation 2013, 84, 1487–1493. [Google Scholar] [CrossRef] [PubMed]
- Olasveengen, T.M.; Semeraro, F.; Ristagno, G.; Castren, M.; Handley, A.; Kuzovlev, A.; Monsieurs, K.G.; Raffay, V.; Smyth, M.; Soar, J.; et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation 2021, 161, 98–114. [Google Scholar] [CrossRef] [PubMed]
- Panchal, A.R.; Bartos, J.A.; Cabanas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (Suppl. S2), S366–S468. [Google Scholar] [CrossRef] [PubMed]
- Hartslief, B.; Janse van Rensburg, C.; Maartens, A.; Marais, P.G.; Meyer, E.T.; Cairncross, J.P.; Joubert, G.; Steinberg, W.J. Accuracy of two-rescuer adult CPR performed by medical registrars at a South African university. Afr. J. Emerg. Med. 2023, 13, 199–203. [Google Scholar] [CrossRef]
- Di Mitri, D.; Schneider, J.; Specht, M.; Drachsler, H. Detecting Mistakes in CPR Training with Multimodal Data and Neural Networks. Sensors 2019, 19, 3099. [Google Scholar] [CrossRef]
- Steenbergen-Hu, S.; Cooper, H. A meta-analysis of the effectiveness of intelligent tutoring systems on college students’ academic learning. J. Educ. Psychol. 2014, 106, 331–347. [Google Scholar] [CrossRef]
- VanLehn, K. The relative effectiveness of human tutoring, intelligent tutoring systems, and other tutoring systems. Educ. Psychol. 2011, 46, 197–221. [Google Scholar] [CrossRef]
- Lukas, R.P.; Van Aken, H.; Engel, P.; Bohn, A. Real-time feedback systems for improvement of resuscitation quality. Anaesthesist 2011, 60, 653–660. [Google Scholar] [CrossRef]
- Gonzalez-Otero, D.M.; Ruiz, J.M.; Ruiz de Gauna, S.; Gutierrez, J.J.; Daya, M.; Russell, J.K.; Azcarate, I.; Leturiondo, M. Monitoring chest compression quality during cardiopulmonary resuscitation: Proof-of-concept of a single accelerometer-based feedback algorithm. PLoS ONE 2018, 13, e0192810. [Google Scholar] [CrossRef] [PubMed]
- Lu, T.C.; Chen, Y.; Ho, T.W.; Chang, Y.T.; Lee, Y.T.; Wang, Y.S.; Chen, Y.P.; Fu, C.M.; Chiang, W.C.; Ma, M.H.; et al. A novel depth estimation algorithm of chest compression for feedback of high-quality cardiopulmonary resuscitation based on a smartwatch. J. Biomed. Inform. 2018, 87, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Engan, K.; Hinna, T.; Ryen, T.; Birkenes, T.S.; Myklebust, H. Chest compression rate measurement from smartphone video. Biomed. Eng. Online 2016, 15, 95. [Google Scholar] [CrossRef]
- Wang, J.C.; Tsai, S.H.; Chen, Y.H.; Chen, Y.L.; Chu, S.J.; Liao, W.I. Kinect-based real-time audiovisual feedback device improves CPR quality of lower-body-weight rescuers. Am. J. Emerg. Med. 2018, 36, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Semeraro, F.; Frisoli, A.; Loconsole, C.; Banno, F.; Tammaro, G.; Imbriaco, G.; Marchetti, L.; Cerchiari, E.L. Motion detection technology as a tool for cardiopulmonary resuscitation (CPR) quality training: A randomised crossover mannequin pilot study. Resuscitation 2013, 84, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, I.K. A Novel Approach and Apparatus for the Measurement and Evaluation of the Quality of Cardiopulmonary Resuscitation. medRxiv 2023. [Google Scholar] [CrossRef]
- Bucki, B.; Waniczek, D.; Michnik, R.; Karpe, J.; Bieniek, A.; Niczyporuk, A.; Makarska, J.; Stepien, T.; Myrcik, D.; Misiolek, H. The assessment of the kinematics of the rescuer in continuous chest compression during a 10-min simulation of cardiopulmonary resuscitation. Eur. J. Med. Res. 2019, 24, 9. [Google Scholar] [CrossRef]
- Kizil, M. Determining the effectiveness of cardiopulmonary resuscitation using a manikin. Hastan. Öncesi Derg. 2023, 7, 303–316. [Google Scholar] [CrossRef]
- Ho, C.S.; Hsu, Y.J.; Li, F.; Tang, C.C.; Yang, C.P.; Huang, C.C.; Ho, C.S.; Chang, C.H. Effect of Ambulance Stretcher Bed Height Adjustment on CPR Quality and Rescuer Fatigue in a Laboratory Environment. Int. J. Med. Sci. 2021, 18, 2783–2788. [Google Scholar] [CrossRef] [PubMed]
- Sugerman, N.T.; Edelson, D.P.; Leary, M.; Weidman, E.K.; Herzberg, D.L.; Vanden Hoek, T.L.; Becker, L.B.; Abella, B.S. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: A prospective multicenter study. Resuscitation 2009, 80, 981–984. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.E.; Kolbe, M.; Nef, A.; Grande, B.; Kalirajan, B.; Meboldt, M.; Lohmeyer, Q. Data-driven resuscitation training using pose estimation. Adv. Simul. 2023, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Mayrand, K.P.; Fischer, E.J.; Ten Eyck, R.P. A Simulation-based Randomized Controlled Study of Factors Influencing Chest Compression Depth. West. J. Emerg. Med. 2015, 16, 1135–1140. [Google Scholar] [CrossRef]
- Chen, K.Y.; Ko, Y.C.; Hsieh, M.J.; Chiang, W.C.; Ma, M.H. Interventions to improve the quality of bystander cardiopulmonary resuscitation: A systematic review. PLoS ONE 2019, 14, e0211792. [Google Scholar] [CrossRef]
- Birkun, A.A.; Gautam, A.; Bottiger, B.W.; Delphi Study Investigators. An expert consensus-based checklist for quality appraisal of educational resources on adult Basic Life Support: A Delphi study. Clin. Exp. Emerg. Med. 2023, 10, 400. [Google Scholar] [CrossRef] [PubMed]
- Minna, S.; Leena, H.; Tommi, K. How to evaluate first aid skills after training: A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2022, 30, 56. [Google Scholar] [CrossRef] [PubMed]
- Riggs, M.; Franklin, R.; Saylany, L. Associations between cardiopulmonary resuscitation (CPR) knowledge, self-efficacy, training history and willingness to perform CPR and CPR psychomotor skills: A systematic review. Resuscitation 2019, 138, 259–272. [Google Scholar] [CrossRef]
- Cho, B.J.; Kim, S.R. A study on the Quality Analysis of CPR Techniques after CPR Simulation Education. Ann. Rom. Soc. Cell Biol. 2021, 25, 1105–1112. [Google Scholar]
- Leo, W.Z.; Chua, D.; Tan, H.C.; Ho, V.K. Chest compression quality and patient outcomes with the use of a CPR feedback device: A retrospective study. Sci. Rep. 2023, 13, 19852. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, J.; Joo, S.; Na, S.H.; Lee, S.; Ko, S.B.; Lee, J.; Oh, S.Y.; Ha, E.J.; Ryu, H.G. The effect of audiovisual feedback of monitor/defibrillators on percentage of appropriate compression depth and rate during cardiopulmonary resuscitation. BMC Anesthesiol. 2023, 23, 334. [Google Scholar] [CrossRef] [PubMed]

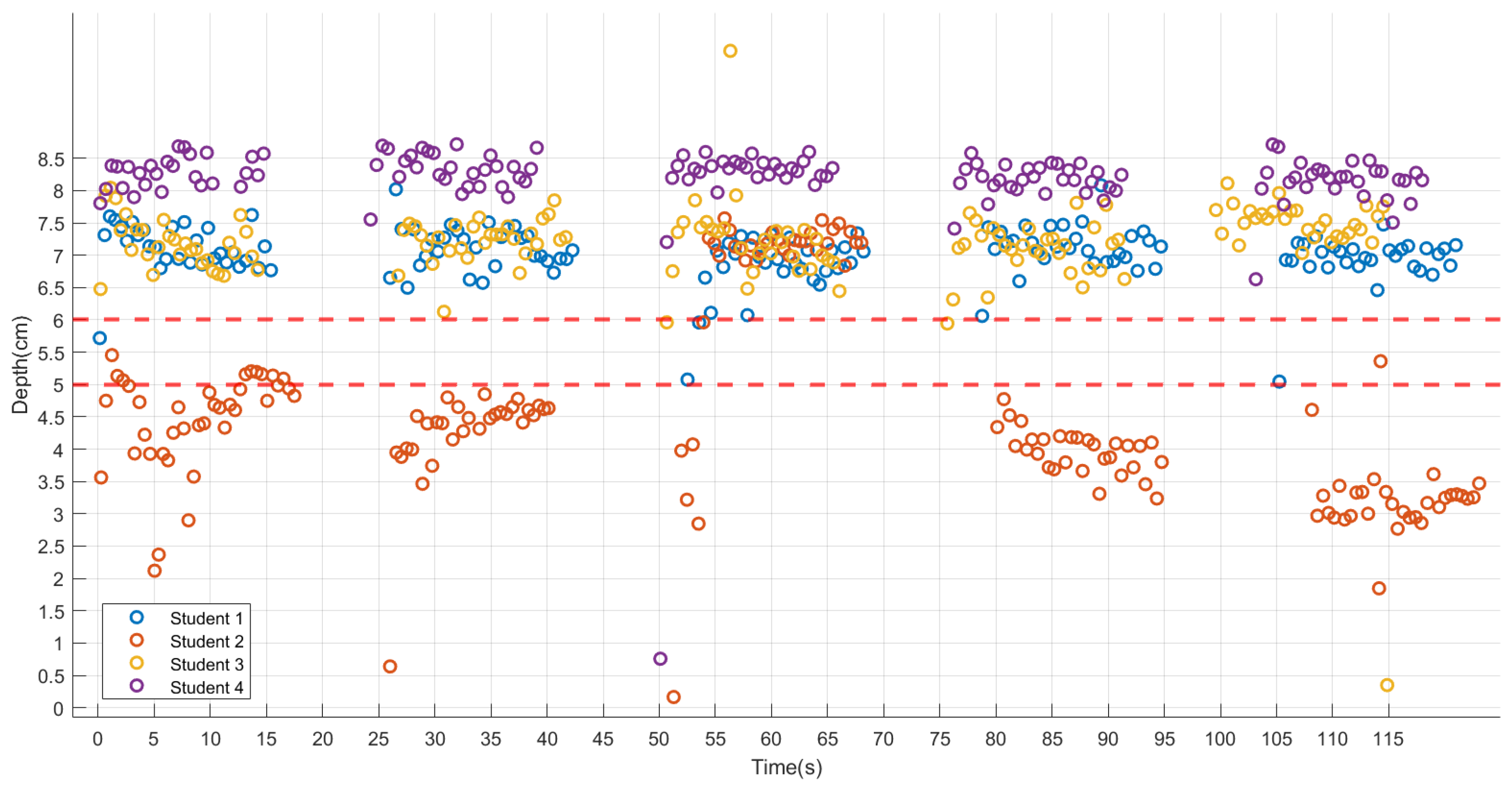

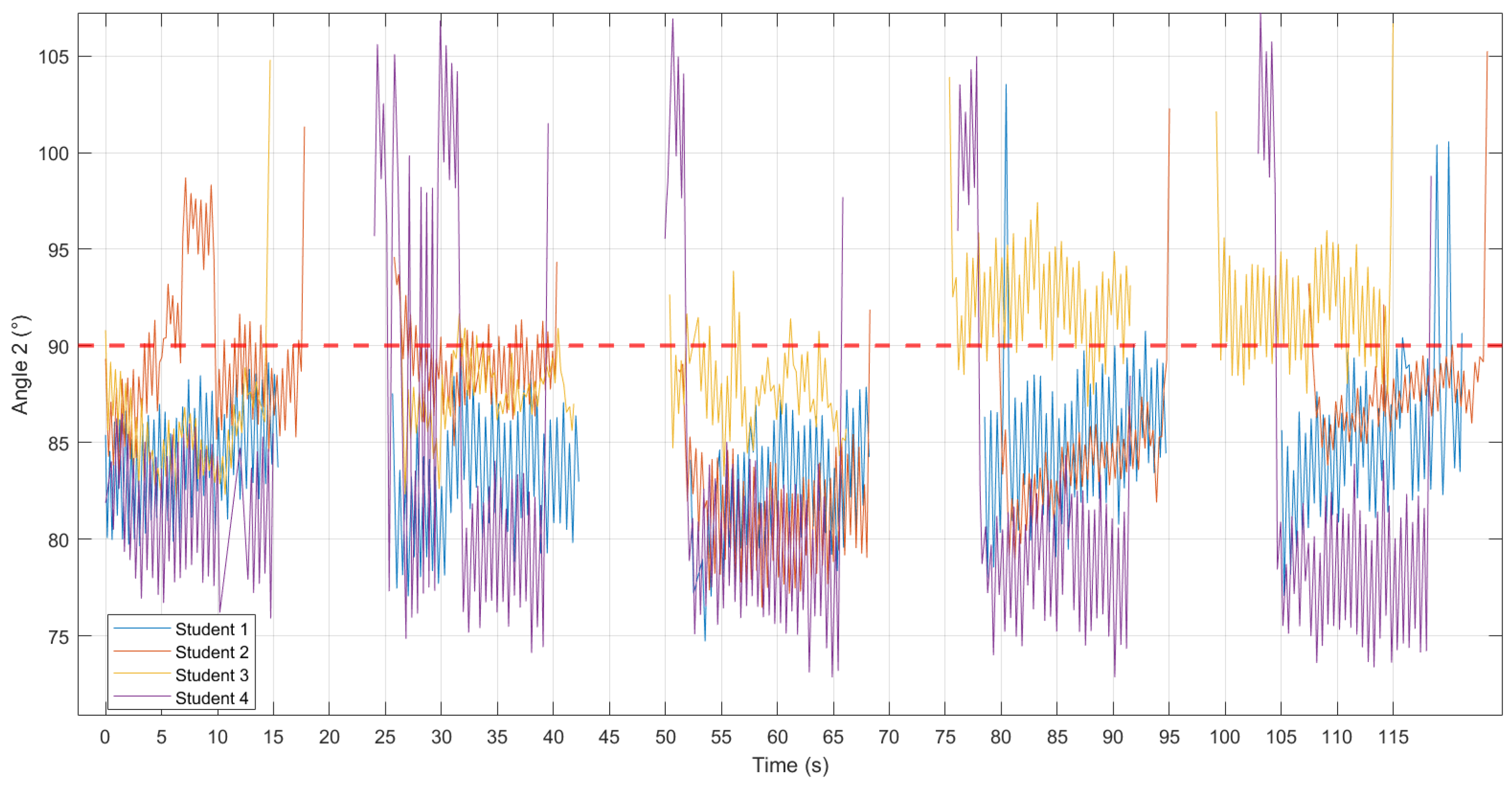
| Student | Cycle | Depth (cm) | Angle 1′ (°) | Angle 2′ (°) | |||
|---|---|---|---|---|---|---|---|
| Median (P25, P75) | H(p) | Median (P25, P75) | H(p) | Median (P25, P75) | H(p) | ||
| 1 | 1 | 7.14(6.89, 7.43) | 14.00 (0.007) | 9.71(9.39, 10.06) | 63.73 (<0.001) | 8.84(7.45, 9.96) | 20.29 (<0.001) |
| 2 | 7.10(6.89, 7.39) | 10.32(9.84, 11.41) | 9.57(8.65, 11.29) | ||||
| 3 | 6.89(6.70, 7.10) | 12.35(11.96, 13.66) | 9.84(8.48, 10.83) | ||||
| 4 | 7.13(6.94, 7.36) | 12.91(11.35, 14.12) | 8.12(6.90, 9.65) | ||||
| 5 | 7.01(6.83, 7.12) | 13.15(10.89, 16.61) | 8.07(6.96, 9.26) | ||||
| Total | 7.06(6.85, 7.27) | 11.53(9.88, 13.17) | 8.98(7.50, 10.24) | ||||
| 2 | 1 | 4.69(4.15, 5.00) | 87.08 (<0.001) | 27.76(24.89, 30.88) | 120.05 (<0.001) | 4.10(2.74, 5.82) | 108.60 (<0.001) |
| 2 | 4.48(4.12, 4.62) | 28.80(25.47, 32.51) | 2.63(2.06, 3.31) | ||||
| 3 | 7.18(6.92, 7.27) | 9.14(8.13, 9.70) | 11.63(10.60, 12.32) | ||||
| 4 | 4.05(3.72, 4.16) | 7.80(7.37, 8.02) | 7.23(6.40, 8.71) | ||||
| 5 | 3.23(2.97, 3.34) | 30.56(27.14, 32.82) | 3.64(2.95, 4.44) | ||||
| Total | 4.33(3.58, 4.98) | 24.18(8.68, 30.16) | 4.92(3.10, 8.48) | ||||
| 3 | 1 | 7.11(6.91, 7.39) | 22.25 (<0.001) | 25.15(24.17, 25.99) | 102.88 (<0.001) | 6.26(4.48, 7.08) | 96.108 (<0.001) |
| 2 | 7.30(7.10, 7.45) | 26.43(24.94, 27.69) | 3.44(2.32, 4.33) | ||||
| 3 | 7.22(6.87, 7.41) | 26.09(24.63, 27.96) | 3.57(2.67, 4.55) | ||||
| 4 | 7.15(6.80, 7.31) | 36.07(33.80, 37.54) | 0.84(0.33, 1.48) | ||||
| 5 | 7.54(7.29, 7.68) | 29.99(28.47, 31.45) | 1.09(0.55, 1.69) | ||||
| Total | 7.26(7.02, 7.47) | 27.72(25.38, 31.51) | 2.57(1.04, 4.42) | ||||
| 4 | 1 | 8.27(8.08, 8.47) | 11.58 (0.021) | 22.31(22.16, 23.30) | 70.53 (<0.001) | 12.01(11.13, 12.51) | 52.61 (<0.001) |
| 2 | 8.36(8.16, 8.56) | 24.67(23.86, 25.36) | 13.85(13.05, 14.96) | ||||
| 3 | 8.34(8.21, 8.43) | 20.63(19.88, 22.76) | 13.99(13.47, 14.91) | ||||
| 4 | 8.17(8.04, 8.34) | 23.85(23.57, 24.98) | 14.16(12.88, 15.04) | ||||
| 5 | 8.20(8.03, 8.30) | 21.78(21.20, 23.14) | 15.08(14.49, 15.76) | ||||
| Total | 8.27(8.09, 8.41) | 23.21(21.70, 24.19) | 14.02(12.76, 14.10) | ||||
| Angle 1′ (°) | Angle 2′ (°) | |
|---|---|---|
| Depth (cm) | 0.017 | 0.079 |
| Angle 1′ (°) | 0.203 * |
| Angle 1′ (°) | Angle 2′ (°) | |
|---|---|---|
| Depth (cm) | −0.209 ** | 0.467 ** |
| Angle 1′ (°) | −0.581 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, X.; Wang, Y.; Ma, H.; Wang, A.; Zhou, Y.; Li, S.; Pei, R.; Cui, H.; Peng, Y.; Piao, M. Detection and Evaluation for High-Quality Cardiopulmonary Resuscitation Based on a Three-Dimensional Motion Capture System: A Feasibility Study. Sensors 2024, 24, 2154. https://doi.org/10.3390/s24072154
Tang X, Wang Y, Ma H, Wang A, Zhou Y, Li S, Pei R, Cui H, Peng Y, Piao M. Detection and Evaluation for High-Quality Cardiopulmonary Resuscitation Based on a Three-Dimensional Motion Capture System: A Feasibility Study. Sensors. 2024; 24(7):2154. https://doi.org/10.3390/s24072154
Chicago/Turabian StyleTang, Xingyi, Yan Wang, Haoming Ma, Aoqi Wang, You Zhou, Sijia Li, Runyuan Pei, Hongzhen Cui, Yunfeng Peng, and Meihua Piao. 2024. "Detection and Evaluation for High-Quality Cardiopulmonary Resuscitation Based on a Three-Dimensional Motion Capture System: A Feasibility Study" Sensors 24, no. 7: 2154. https://doi.org/10.3390/s24072154
APA StyleTang, X., Wang, Y., Ma, H., Wang, A., Zhou, Y., Li, S., Pei, R., Cui, H., Peng, Y., & Piao, M. (2024). Detection and Evaluation for High-Quality Cardiopulmonary Resuscitation Based on a Three-Dimensional Motion Capture System: A Feasibility Study. Sensors, 24(7), 2154. https://doi.org/10.3390/s24072154







