Biomechanical Strategies to Improve Running: Cadence, Footwear, and Orthoses—A Quasi-Experimental Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Participants
2.3. Material
- -
- (I) Pelvis Markers: Bilateral anterior superior iliac spines (ASIS) and sacrum.
- -
- (II) Thigh Markers: Lateral femoral condyle, anterior tibial tuberosity, and a technical marker positioned above the patella.
- -
- (III) Shank Markers: Lateral malleolus only, placed directly on the skin for precise tracking.
- -
- (IV) Foot Markers: Second and fifth metatarsal heads (placed on the shoes) and calcaneus (placed on the shoes).
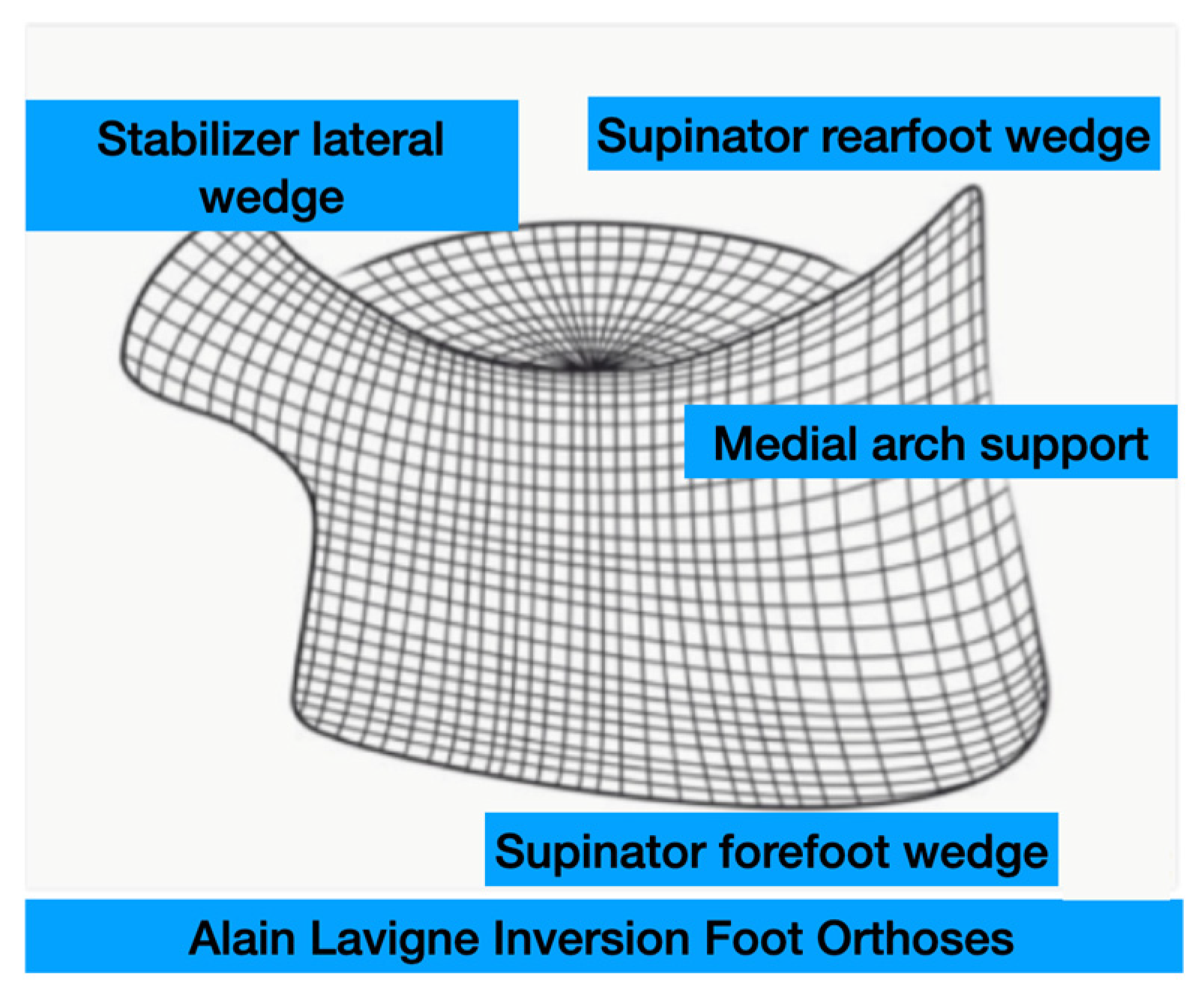
Foot Orthoses
2.4. Design
2.5. Outcome Measures
- Ankle Dorsiflexion (AF): Measured at foot strike (FS) and peak timing (MAX).
- Knee Flexion (KF): Measured at FS and peak timing.
- Hip Adduction (HA): Measured at FS and peak timing.
2.6. Sample Size
2.7. Statistical Analysis
3. Results
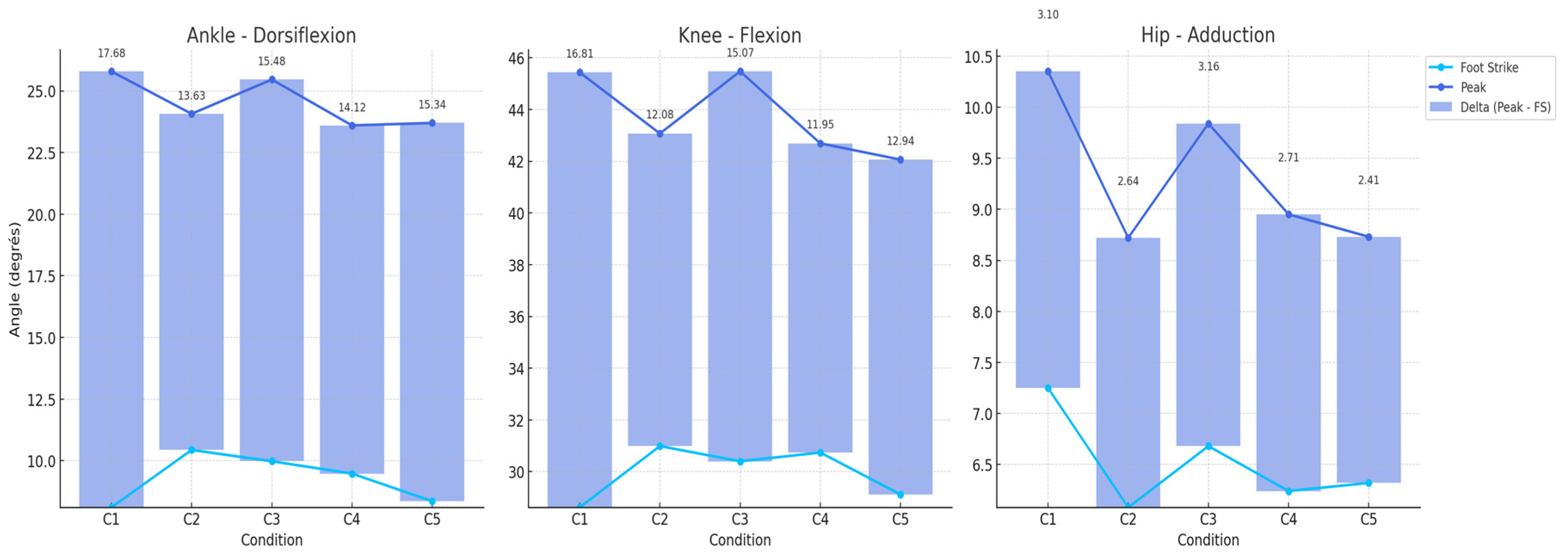
3.1. Ankle Dorsiflexion (AF)
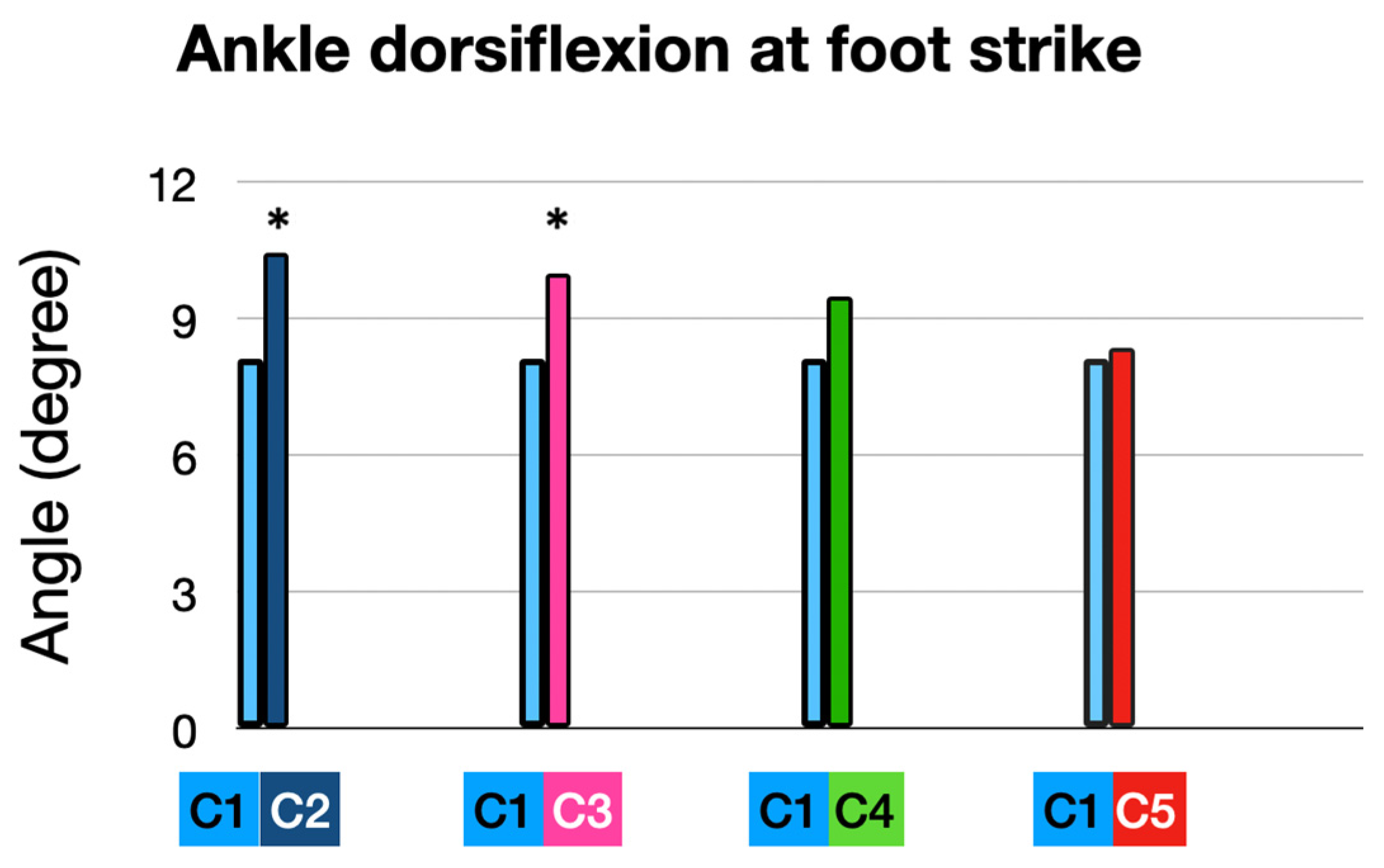
3.1.1. At Foot Strike (FS): (Figure 4)
3.1.2. At Peak Timing (MAX): (Figure 5 and Figure 6)


3.1.3. Root Mean Square Deviation (RMSD) (Table 2)
| Stride Cycle | C1/C2 | C1/C3 | C1/C4 | C1/C5 |
|---|---|---|---|---|
| 0–10% | 2.1938 | 1.9377 | 1.1584 | 0.1894 |
| 10–20% | 1.1205 | 1.369 | 0.3508 | 0.5252 |
| 20–30% | 0.2697 | 0.7646 | 1.0402 | 1.1168 |
| 30–40% | 0.7926 | 0.3316 | 1.6005 | 1.6131 |
| 40–50% | 1.4316 | 1.1692 | 2.0218 | 1.9715 |
| 50–60% | 2.1906 | 0.7145 | 2.3309 | 2.1029 |
| 60–70% | 2.8769 | 1.4178 | 2.4349 | 1.8182 |
| 70–80% | 3.186 | 2.0816 | 2.1884 | 1.0881 |
| 80–90% | 3.2148 | 2.7118 | 1.6716 | 0.3553 |
| 90–100% | 2.8176 | 2.9954 | 0.8049 | 1.3843 |
3.2. Knee Flexion (KF)
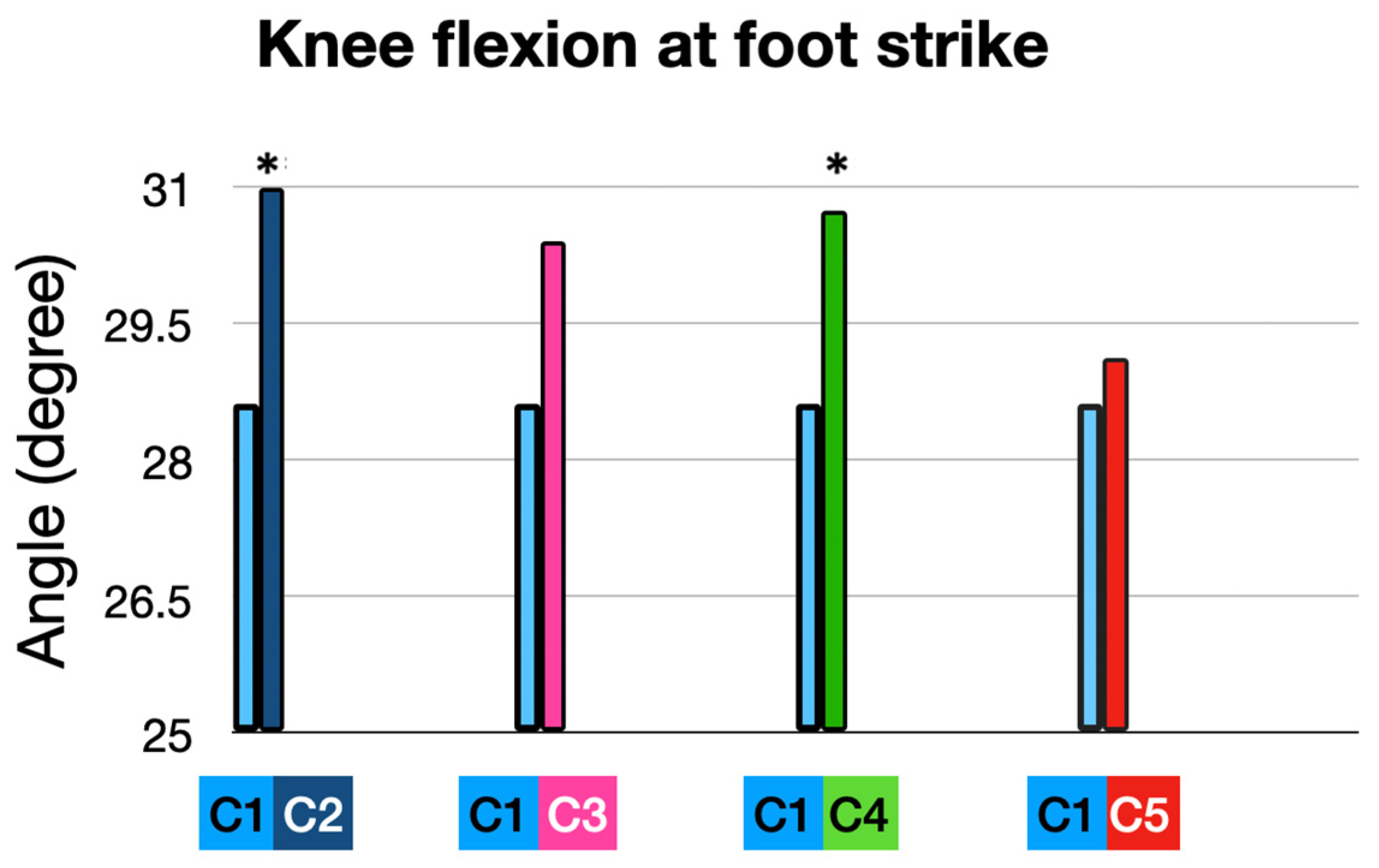
3.2.1. At Foot Strike (FS) (Table 3 and Figure 7 and Figure 8)
| Biomechanical Criteria | Mean 1st Condition C1 | Condition | Mean 2nd Condition | Delta | p-Value | Cohen’s d |
|---|---|---|---|---|---|---|
| Ankle dorsiflexion at foot strike | 8.11° | C2 | 10.44° | 2.33° | 0.0055 * | 0.94 |
| C3 | 9.98 | 1.87° | 0.0360 * | 0.75 | ||
| C4 | 9.48° | 1.37° | 0.1790 | 0.55 | ||
| C5 | 8.36° | 0.26° | 0.99 | 0.10 | ||
| Peak ankle dorsiflexion | 25.79° | C2 | 24.07° | −1.72° | 0.0962 | −0.88 |
| C3 | 25.46° | −0.33° | 0.923 | −0.84 | ||
| C4 | 23.6° | −2.19° | 0.0316 * | 0.96 | ||
| C5 | 23.70 | −2.09 | 0.0714 | 0.76 | ||
| Knee flexion at foot strike | 28.62° | C2 | 30.99° | 2.37° | 0.0255 * | 0.85 |
| C3 | 30.40° | 1.88° | 0.13 | 0.20 | ||
| C4 | 30.74° | 2.12° | 0.05 * | −0.95 | ||
| C5 | 29.12° | 0.5° | 0.9 | −1.10 | ||
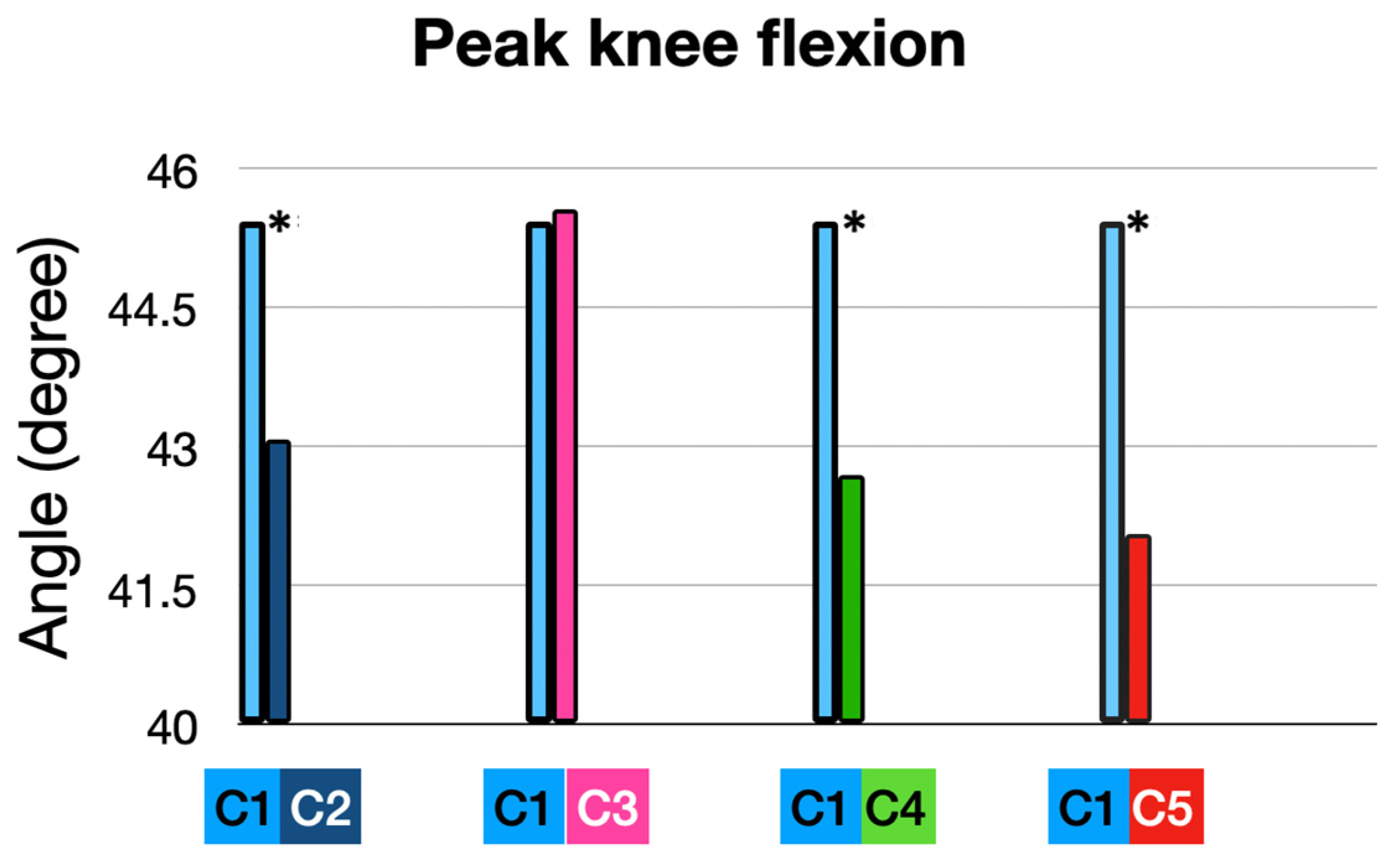
| Peak knee flexion | 45.43° | C2 | 43.07° | −2.36° | 0.0318 * | −1.36 |
| C3 | 45.47° | 1 | −0.66 | |||
| C4 | 42.69° | −2.74° | 0.0066 * | −0.65 | ||
| C5 | 42.06° | −3.37 | 0.001 * | 0.94 | ||
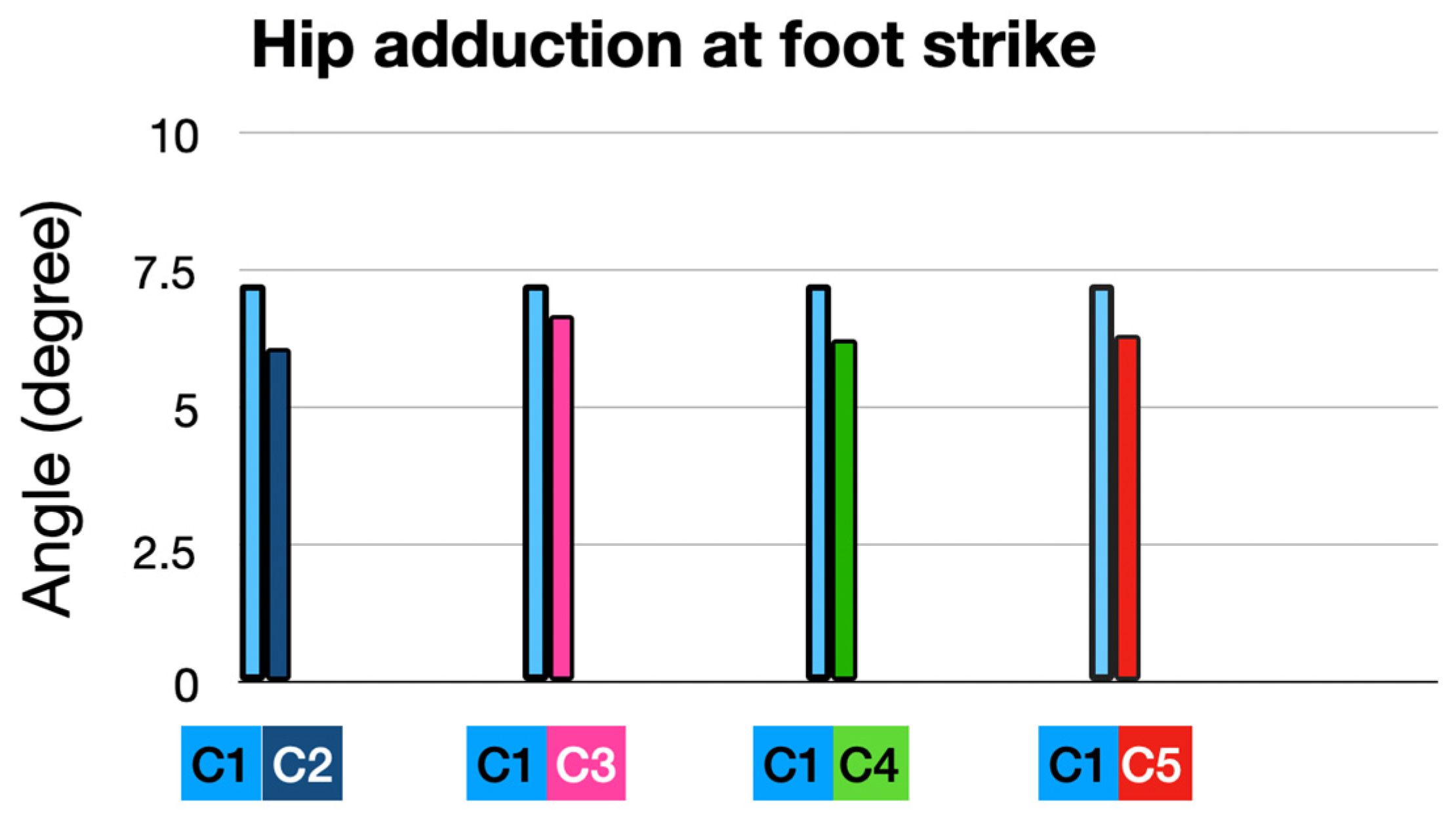
| Hip adduction at foot strike | 7.25° | C2 | 6.08° | −1.17° | 0.15 | 0.75 |
| C3 | 6.68° | −0.67° | 0.72 | 0.55 | ||
| C4 | 6.24° | −1.01° | 0.25 | 0.10 | ||
| C5 | 6.32° | −0.95° | 0.32 | −0.88 | ||
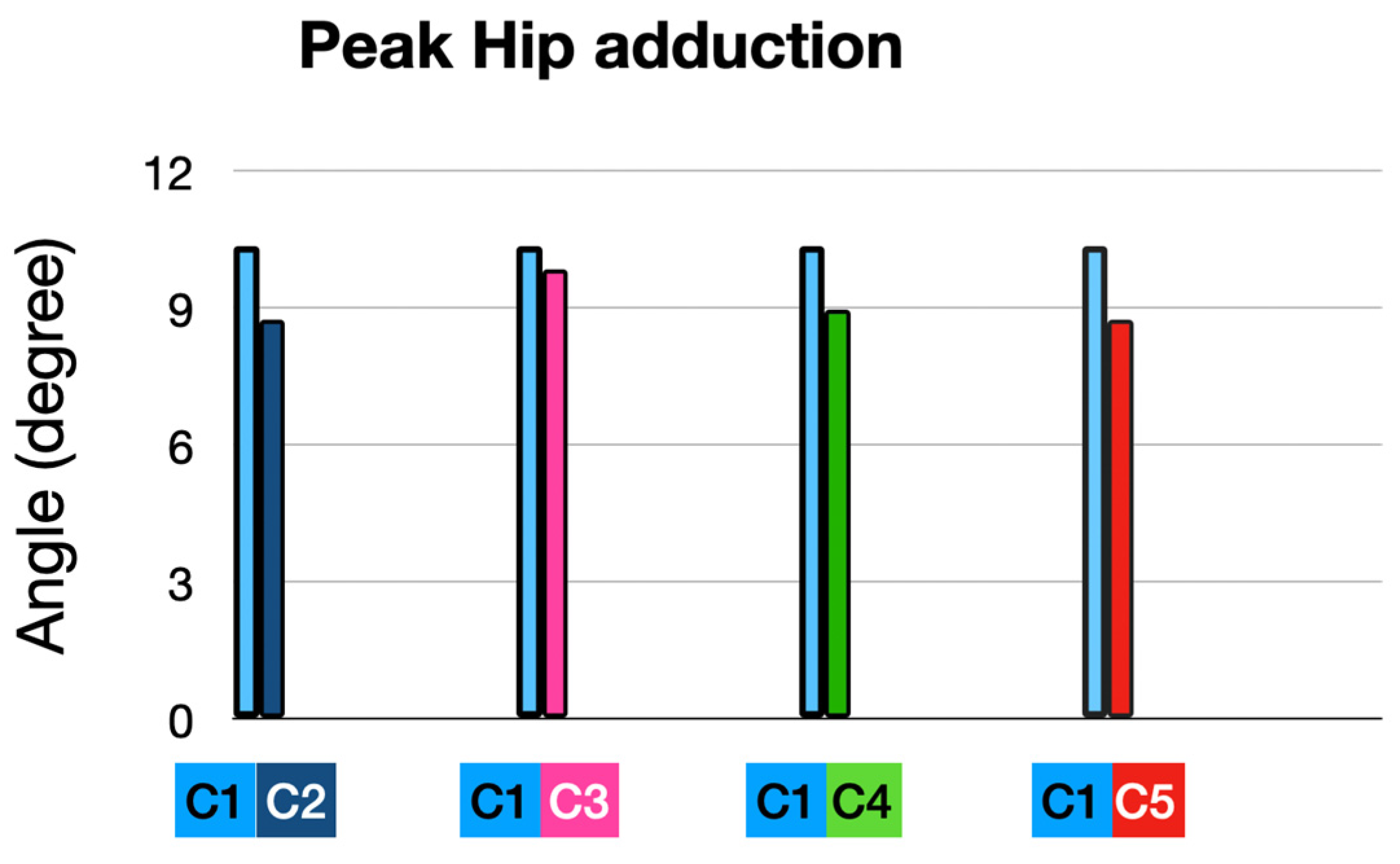
| Peak hip adduction | 10.35° | C2 | 8.72° | −1.63 | 0.15 | −0.84 |
| C3 | 9.84° | −0.51 | 0.9 | 0.96 | ||
| C4 | 8.95° | −1.40° | 0.23 | 0.76 | ||
| C5 | 8.73° | −1.62 | 0.16 | 0.85 |
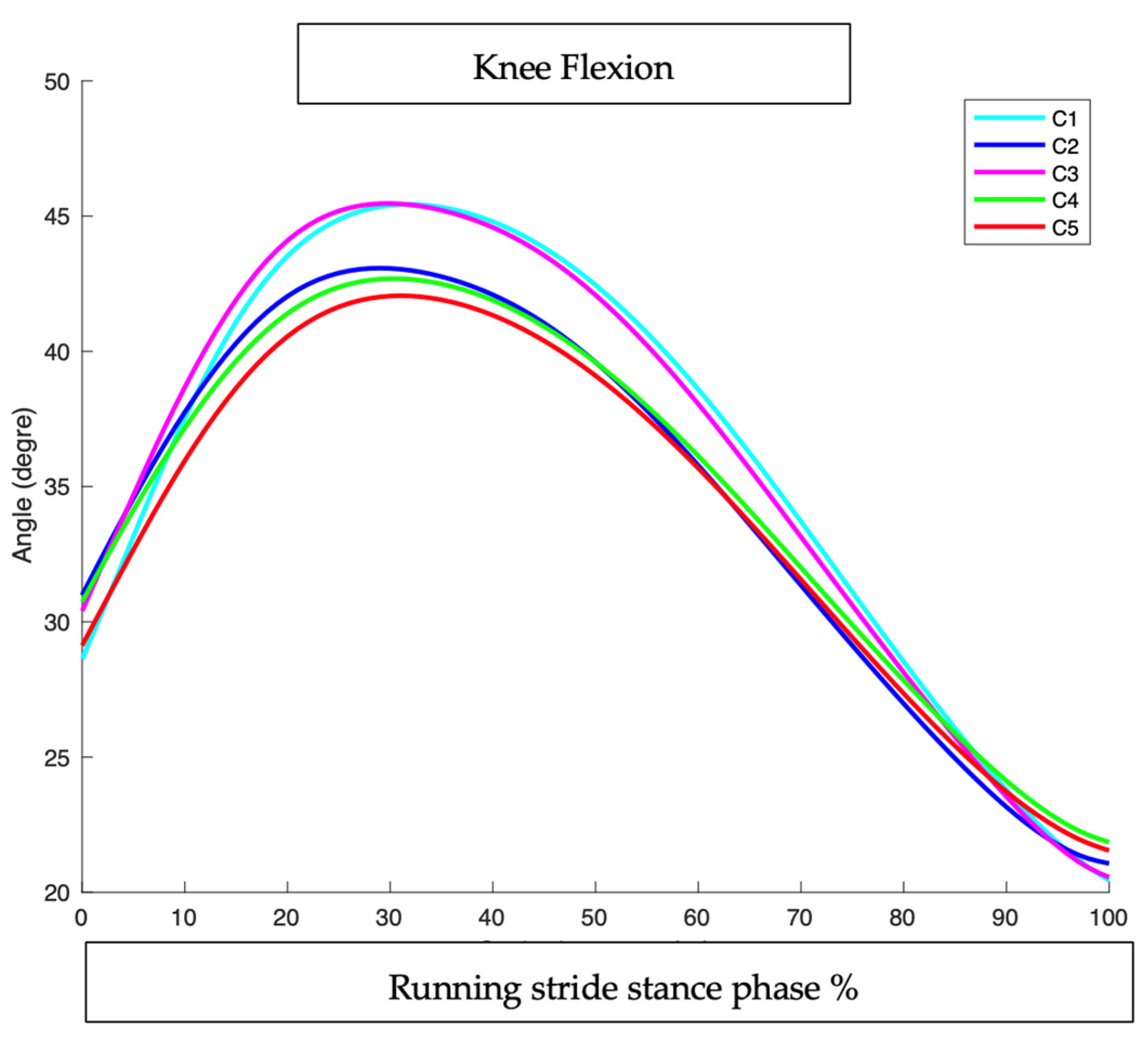
3.2.2. At Peak Timing (MAX): (Figure 8 and Figure 9 and Table 3)
3.2.3. Root Mean Square Deviation (RMSD) (Table 4)
| Stride Cycle | C1/C2 | C1/C3 | C1/C4 | C1/C5 |
|---|---|---|---|---|
| 0–10% | 1.6 | 1.55 | 1.28 | 0.73 |
| 10–20% | 0.82 | 0.88 | 1.39 | 2.35 |
| 20–30% | 1.93 | 0.37 | 2.45 | 3.19 |
| 30–40% | 2.53 | 0.12 | 2.82 | 3.41 |
| 40–50% | 2.78 | 0.28 | 2.91 | 3.44 |
| 50–60% | 2.86 | 0.46 | 2.72 | 3.19 |
| 60–70% | 2.65 | 0.57 | 2.16 | 2.6 |
| 70–80% | 2.03 | 0.5 | 1.29 | 1.75 |
| 80–90% | 1.18 | 0.33 | 0.38 | 0.76 |
| 90–100% | 0.37 | 0.16 | 0.87 | 0.58 |
3.3. Hip Adduction
3.3.1. At Foot Strike (FS):
3.3.2. At Peak Timing (MAX): (Table 3 and Figure 11 and Figure 12)
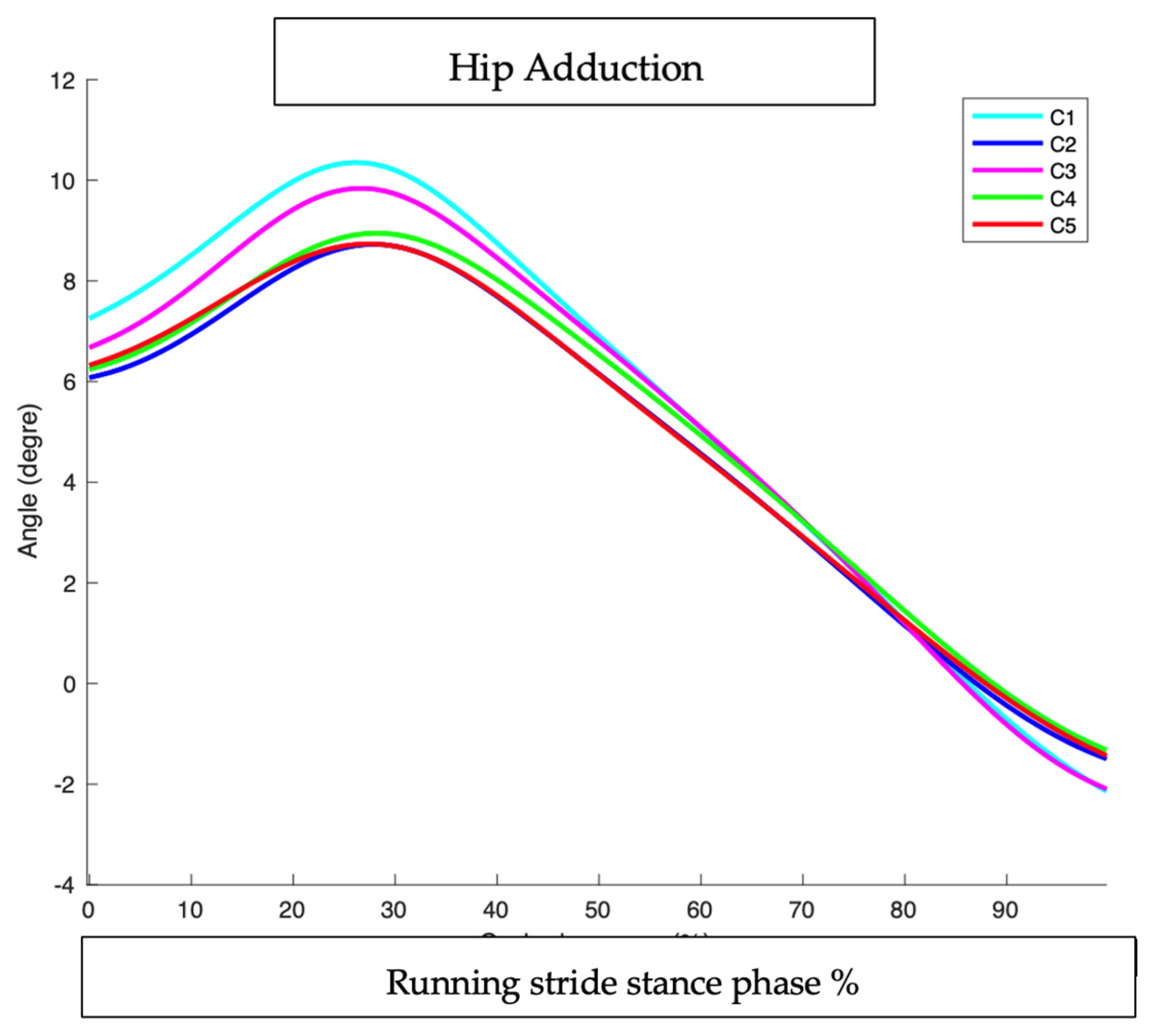
3.3.3. Root Mean Square Deviation (RMSD) (Table 5)
| Stride Cycle | C1/C2 | C1/C3 | C1/C4 | C1/C5 |
|---|---|---|---|---|
| 0–10% | 1.3833 | 0.6213 | 1.1824 | 1.0823 |
| 10–20% | 1.6662 | 0.5977 | 1.4336 | 1.4257 |
| 20–30% | 1.672 | 0.5256 | 1.4542 | 1.6167 |
| 30–40% | 1.3083 | 0.4008 | 1.0377 | 1.3048 |
| 40–50% | 0.9155 | 0.212 | 0.5601 | 0.9082 |
| 50–60% | 0.6492 | 0.054 | 0.2692 | 0.6661 |
| 60–70% | 0.425 | 0.0252 | 0.0872 | 0.4381 |
| 70–80% | 0.2313 | 0.0237 | 0.1026 | 0.19 |
| 80–90% | 0.1225 | 0.0901 | 0.3461 | 0.223 |
| 90–100% | 0.4546 | 0.0757 | 0.6606 | 0.567 |
4. Discussion
4.1. Impact of Full Interventions (C2: HTD + Cadence + ALIFOrthoses)
4.1.1. Effects of C2 on the Ankle
4.1.2. Effects of C2 on Knee Flexion (KF)
4.1.3. Effects of C2 on Hip Adduction (HA)
- -
- The addition of HTD and ALIFOorthoses is harmful and decreases the impact of increasing step rate on the hip kinematics.
- -
- Our study recruited healthy runners whereas most studies showing good results on peak hip adduction were on PFPS runners with a greater peak hip adduction at baseline. Both Neal’s [38] and Bramah’s [37] study with increased cadence intervention showed an average peak hip adduction at baseline of around 15°. In our study, the average at baseline was only 10.35. This low peak adduction in healthy runners may explain the lack of significance of C2 on hip adduction.
4.2. Impact of Structural Modifications Alone (C3: HTD + ALIFOrthoses)
4.2.1. Effects of C3 on the Ankle
4.2.2. Effects of C3 on Knee Flexion and Hip Adduction (KF)
4.3. Impact of Condition C4 (HTD + Cadence)
4.3.1. Effects of C4 on the Ankle
4.3.2. Effects of C4 on the Knee and the Hip
4.4. Effectiveness of Cadence Adjustment Alone (C5)
4.5. Clinical Implications
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, D.-C.; Pate, R.R.; Lavie, C.J.; Sui, X.; Church, T.S.; Blair, S.N. Leisure-time running reduces all-cause and cardiovascular mortality risk. J. Am. Coll. Cardiol. 2014, 64, 472–481. [Google Scholar] [CrossRef]
- Oja, P.; Titze, S.; Kokko, S.; Kujala, U.M.; Heinonen, A.; Kelly, P.; Koski, P.; Foster, C. Health benefits of different sport disciplines for adults: Systematic review of observational and intervention studies with meta-analysis. Br. J. Sports Med. 2015, 49, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Szabo, A.; Abrahám, J. The psychological benefits of recreational running: A field study. Psychol. Health Med. 2013, 18, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Kakouris, N.; Yener, N.; Fong, D.T.P. A systematic review of running-related musculoskeletal injuries in runners. J. Sport Health Sci. 2021, 10, 513–522. [Google Scholar] [CrossRef] [PubMed]
- van Mechelen, W. Running injuries. A review of the epidemiological literature. Sports Med. Auckl. NZ 1992, 14, 320–335. [Google Scholar] [CrossRef]
- van Gent, R.N.; Siem, D.; van Middelkoop, M.; van Os, A.G.; Bierma-Zeinstra, S.M.A.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480. [Google Scholar] [CrossRef]
- Aicale, R.; Tarantino, D.; Maffulli, N. Overuse injuries in sport: A comprehensive overview. J. Orthop. Surg. 2018, 13, 309. [Google Scholar] [CrossRef]
- Edwards, W.B. Modeling Overuse Injuries in Sport as a Mechanical Fatigue Phenomenon. Exerc. Sport Sci. Rev. 2018, 46, 224–231. [Google Scholar] [CrossRef]
- Garza-Borjón, A.; González-González, M.; de la Garza-Salazar, J.F.; Simental-Mendía, M.; Acosta-Olivo, C. Understanding the patho-anatomy of patellofemoral pain: A crucial foundation for comprehensive management. Orthop. Rev. 2024, 16, 125840. [Google Scholar] [CrossRef]
- Noehren, B.; Hamill, J.; Davis, I. Prospective evidence for a hip etiology in patellofemoral pain. Med. Sci. Sports Exerc. 2013, 45, 1120–1124. [Google Scholar] [CrossRef]
- Noehren, B.; Pohl, M.B.; Sanchez, Z.; Cunningham, T.; Lattermann, C. Proximal and distal kinematics in female runners with patellofemoral pain. Clin. Biomech. 2012, 27, 366–371. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Best, T.M.; Liu, H.; Yu, B. Knee biomechanical factors associated with patellofemoral pain in recreational runners. Knee 2022, 35, 87–97. [Google Scholar] [CrossRef]
- Boling, M.; Padua, D.; Marshall, S.; Guskiewicz, K.; Pyne, S.; Beutler, A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand. J. Med. Sci. Sports 2010, 20, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.S.; Barton, C.J.; Birn-Jeffery, A.; Morrissey, D. Increased hip adduction during running is associated with patellofemoral pain and differs between males and females: A case-control study. J. Biomech. 2019, 91, 133–139. [Google Scholar] [CrossRef]
- Sanchez-Alvarado, A.; Bokil, C.; Cassel, M.; Engel, T. Effects of conservative treatment strategies for iliotibial band syndrome on pain and function in runners: A systematic review. Front. Sports Act. Living 2024, 6, 1386456. [Google Scholar] [CrossRef]
- Aderem, J.; Louw, Q.A. Biomechanical risk factors associated with iliotibial band syndrome in runners: A systematic review. BMC Musculoskelet. Disord. 2015, 16, 356. [Google Scholar] [CrossRef] [PubMed]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical Risk Factors Associated with Running-Related Injuries: A Systematic Review. Sports Med. Auckl. NZ 2019, 49, 1095–1115. [Google Scholar] [CrossRef]
- Milner, C.E.; Foch, E.; Gonzales, J.M.; Petersen, D. Biomechanics associated with tibial stress fracture in runners: A systematic review and meta-analysis. J. Sport Health Sci. 2023, 12, 333–342. [Google Scholar] [CrossRef]
- Daoud, A.I.; Geissler, G.J.; Wang, F.; Saretsky, J.; Daoud, Y.A.; Lieberman, D.E. Foot strike and injury rates in endurance runners: A retrospective study. Med. Sci. Sports Exerc. 2012, 44, 1325–1334. [Google Scholar] [CrossRef]
- Alexander, J.L.N.; Culvenor, A.G.; Johnston, R.R.T.; Ezzat, A.M.; Barton, C.J. Strategies to prevent and manage running-related knee injuries: A systematic review of randomised controlled trials. Br. J. Sports Med. 2022, 56, 1307–1319. [Google Scholar] [CrossRef]
- Dutton, R.A.; Khadavi, M.J.; Fredericson, M. Update on Rehabilitation of Patellofemoral Pain. Curr. Sports Med. Rep. 2014, 13, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Saltychev, M.; Dutton, R.; Laimi, K.; Beaupré, G.; Virolainen, P.; Fredericson, M. Effectiveness of conservative treatment for patellofemoral pain syndrome: A systematic review and meta-analysis. J. Rehabil. Med. 2018, 50, 393–401. [Google Scholar] [CrossRef]
- de Souza Júnior, J.R.; Rabelo, P.H.R.; Lemos, T.V.; Esculier, J.-F.; Barbosa, G.M.P.; Matheus, J.P.C. Effects of two gait retraining programs on pain, function, and lower limb kinematics in runners with patellofemoral pain: A randomized controlled trial. PLoS ONE 2024, 19, e0295645. [Google Scholar] [CrossRef]
- Willwacher, S.; Kurz, M.; Robbin, J.; Thelen, M.; Hamill, J.; Kelly, L.; Mai, P. Running-Related Biomechanical Risk Factors for Overuse Injuries in Distance Runners: A Systematic Review Considering Injury Specificity and the Potentials for Future Research. Sports Med. Auckl. NZ 2022, 52, 1863–1877. [Google Scholar] [CrossRef] [PubMed]
- Hryvniak, D.; Magrum, E.; Wilder, R. Patellofemoral Pain Syndrome: An Update. Curr. Phys. Med. Rehabil. Rep. 2014, 2, 16–24. [Google Scholar] [CrossRef]
- Bonacci, J.; Vicenzino, B.; Spratford, W.; Collins, P. Take your shoes off to reduce patellofemoral joint stress during running. Br. J. Sports Med. 2014, 48, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Lashien, S.A.; Abdelnaeem, A.O.; Gomaa, E.F. Effect of hip abductors training on pelvic drop and knee valgus in runners with medial tibial stress syndrome: A randomized controlled trial. J. Orthop. Surg. 2024, 19, 700. [Google Scholar] [CrossRef]
- Räisänen, A.M.; Pasanen, K.; Krosshaug, T.; Vasankari, T.; Kannus, P.; Heinonen, A.; Kujala, U.M.; Avela, J.; Perttunen, J.; Parkkari, J. Association between frontal plane knee control and lower extremity injuries: A prospective study on young team sport athletes. BMJ Open Sport Exerc. Med. 2018, 4, e000311. [Google Scholar] [CrossRef]
- Ford, K.R.; Myer, G.D.; Hewett, T.E. Valgus knee motion during landing in high school female and male basketball players. Med. Sci. Sports Exerc. 2003, 35, 1745–1750. [Google Scholar] [CrossRef]
- Anderson, L. What is the Effect of Changing Running Step Rate on Injury, Performance and Biomechanics? A Systematic Review and Meta-analysis. Sports Med. 2022, 8, 112. [Google Scholar] [CrossRef]
- Dos Santos, A.F.; Nakagawa, T.H.; Lessi, G.C.; Luz, B.C.; Matsuo, H.T.M.; Nakashima, G.Y.; Maciel, C.D.; Serrão, F.V. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys. Ther. Sport Off. J. Assoc. Chart. Physiother. Sports Med. 2019, 36, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.J.; Munteanu, S.E.; Menz, H.B.; Crossley, K.M. The efficacy of foot orthoses in the treatment of individuals with patellofemoral pain syndrome: A systematic review. Sports Med. Auckl. NZ 2010, 40, 377–395. [Google Scholar] [CrossRef]
- Boldt, A.R.; Willson, J.D.; Barrios, J.A.; Kernozek, T.W. Effects of medially wedged foot orthoses on knee and hip joint running mechanics in females with and without patellofemoral pain syndrome. J. Appl. Biomech. 2013, 29, 68–77. [Google Scholar] [CrossRef]
- Esculier, J.-F.; Bouyer, L.J.; Dubois, B.; Fremont, P.; Moore, L.; McFadyen, B.; Roy, J.-S. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain?A randomised clinical trial. Br. J. Sports Med. 2018, 52, 659–666. [Google Scholar] [CrossRef]
- Musgjerd, T.; Anason, J.; Rutherford, D.; Kernozek, T.W. Effect of Increasing Running Cadence on Peak Impact Force in an Outdoor Environment. Int. J. Sports Phys. Ther. 2021, 16, 1076–1083. [Google Scholar] [CrossRef]
- Liu, Y.; Qi, Y.; Song, Y.; Feng, L.; Wang, L. Influences of altering footstrike pattern and cadence on lower extremity joint coordination and variability among runners with patellofemoral pain. PLoS ONE 2023, 18, e0280477. [Google Scholar] [CrossRef]
- Bramah, C.; Preece, S.J.; Gill, N.; Herrington, L. A 10% Increase in Step Rate Improves Running Kinematics and Clinical Outcomes in Runners With Patellofemoral Pain at 4 Weeks and 3 Months. Am. J. Sports Med. 2019, 47, 3406–3413. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.S.; Barton, C.J.; Birn-Jeffrey, A.; Daley, M.; Morrissey, D. The effects & mechanisms of increasing running step rate: A feasibility study in a mixed-sex group of runners with patellofemoral pain. Phys. Ther. Sport Off. J. Assoc. Chart. Physiother. Sports Med. 2018, 32, 244–251. [Google Scholar] [CrossRef]
- Del Duchetto, F.; Dussault-Picard, C.; Gagnon, M.; Dixon, P.; Cherni, Y. Can Foot Orthoses Benefit Symptomatic Runners? Mechanistic and Clinical Insights Through a Scoping Review. Sports Med.—Open 2024, 10, 108. [Google Scholar] [CrossRef]
- Chen, Z.; Wu, J.; Wang, X.; Ren, Z. The effect of foot orthoses for patients with patellofemoral pain syndrome: A systematic review and meta-analysis. Heliyon 2022, 8, e09656. [Google Scholar] [CrossRef]
- Crossley, K.M.; Stefanik, J.J.; Selfe, J.; Collins, N.J.; Davis, I.S.; Powers, C.M.; McConnell, J.; Vicenzino, B.; Bazett-Jones, D.M.; Esculier, J.-F.; et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br. J. Sports Med. 2016, 50, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhou, X.; Zhang, L.; Liu, H.; Yu, B. The effect of heel-to-toe drop of running shoes on patellofemoral joint stress during running. Gait Posture 2022, 93, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Boling, M.C.; Padua, D.A.; Marshall, S.W.; Guskiewicz, K.; Pyne, S.; Beutler, A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: The Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am. J. Sports Med. 2009, 37, 2108–2116. [Google Scholar] [CrossRef]
- Pohl, M.B.; Mullineaux, D.R.; Milner, C.E.; Hamill, J.; Davis, I.S. Biomechanical predictors of retrospective tibial stress fractures in runners. J. Biomech. 2008, 41, 1160–1165. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, A.; Lescure, Y.; Delacroix, S. La podologie orthopédique avancée. Rev. Podol. 2017, 13, 8–10. [Google Scholar] [CrossRef]
- Yu, P.; He, Y.; Gu, Y.; Liu, Y.; Xuan, R.; Fernandez, J. Acute Effects of Heel-to-Toe Drop and Speed on Running Biomechanics and Strike Pattern in Male Recreational Runners: Application of Statistical Nonparametric Mapping in Lower Limb Biomechanics. Front. Bioeng. Biotechnol. 2022, 9, 821530. [Google Scholar] [CrossRef]
- Van Hooren, B.; Fuller, J.T.; Buckley, J.D.; Miller, J.R.; Sewell, K.; Rao, G.; Barton, C.; Bishop, C.; Willy, R.W. Is Motorized Treadmill Running Biomechanically Comparable to Overground Running? A Systematic Review and Meta-Analysis of Cross-Over Studies. Sports Med. Auckl. NZ 2020, 50, 785–813. [Google Scholar] [CrossRef]
- Sekine, M.; Tamura, T.; Yoshida, M.; Suda, Y.; Kimura, Y.; Miyoshi, H.; Kijima, Y.; Higashi, Y.; Fujimoto, T. A gait abnormality measure based on root mean square of trunk acceleration. J. Neuroengineering Rehabil. 2013, 10, 118. [Google Scholar] [CrossRef]
- Farina, K.A.; Hahn, M.E. Increasing Step Rate Affects Rearfoot Kinematics and Ground Reaction Forces during Running. Biology 2021, 11, 8. [Google Scholar] [CrossRef]
- Roper, J.L.; Doerfler, D.; Kravitz, L.; Dufek, J.S.; Mermier, C. Gait Retraining From Rearfoot Strike to Forefoot Strike does not change Running Economy. Int. J. Sports Med. 2017, 38, 1076–1082. [Google Scholar] [CrossRef]
- Zhang, M.; Shi, H.; Liu, H.; Zhou, X. Biomechanical Analysis of Running in Shoes with Different Heel-to-Toe Drops. Appl. Sci. 2021, 11, 12144. [Google Scholar] [CrossRef]
- Sinclair, J.K. Effects of a 10 week footstrike transition in habitual rearfoot runners with patellofemoral pain. Comp. Exerc. Physiol. 2016, 12, 141–150. [Google Scholar] [CrossRef]
- Dixon, S.J.; McNally, K. Influence of orthotic devices prescribed using pressure data on lower extremity kinematics and pressures beneath the shoe during running. Clin. Biomech. Bristol Avon 2008, 23, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.J.; Menz, H.B.; Crossley, K.M. Clinical predictors of foot orthoses efficacy in individuals with patellofemoral pain. Med. Sci. Sports Exerc. 2011, 43, 1603–1610. [Google Scholar] [CrossRef] [PubMed]
- Jor, A.; Lau, N.W.K.; Daryabor, A.; Koh, M.W.P.; Lam, W.-K.; Hobara, H.; Kobayashi, T. Effects of foot orthoses on running kinetics and kinematics: A systematic review and meta-analysis. Gait Posture 2024, 109, 240–258. [Google Scholar] [CrossRef] [PubMed]
- Lescure, Y. Le syndrome fémoro-patellaire du coureur à pied. Rev. Podol. 2017, 13, 13–15. [Google Scholar] [CrossRef]
- Foroughi, N.; Smith, R.; Vanwanseele, B. The association of external knee adduction moment with biomechanical variables in osteoarthritis: A systematic review. Knee 2009, 16, 303–309. [Google Scholar] [CrossRef]
- Toda, Y.; Tsukimura, N.; Kato, A. The effects of different elevations of laterally wedged insoles with subtalar strapping on medial compartment osteoarthritis of the knee. Arch. Phys. Med. Rehabil. 2004, 85, 673–677. [Google Scholar] [CrossRef]
- Arnold, J.B.; Wong, D.X.; Jones, R.K.; Hill, C.L.; Thewlis, D. Lateral Wedge Insoles for Reducing Biomechanical Risk Factors for Medial Knee Osteoarthritis Progression: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2016, 68, 936–951. [Google Scholar] [CrossRef]
- Radzimski, A.O.; Mündermann, A.; Sole, G. Effect of footwear on the external knee adduction moment—A systematic review. Knee 2012, 19, 163–175. [Google Scholar] [CrossRef]
- Roper, J.L.; Harding, E.M.; Doerfler, D.; Dexter, J.G.; Kravitz, L.; Dufek, J.S.; Mermier, C.M. The effects of gait retraining in runners with patellofemoral pain: A randomized trial. Clin. Biomech. Bristol Avon 2016, 35, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.J.; Bonanno, D.R.; Carr, J.; Neal, B.S.; Malliaras, P.; Franklyn-Miller, A.; Menz, H.B. Running retraining to treat lower limb injuries: A mixed-methods study of current evidence synthesised with expert opinion. Br. J. Sports Med. 2016, 50, 513–526. [Google Scholar] [CrossRef] [PubMed]
- Bonacci, J.; Hall, M.; Saunders, N.; Vicenzino, B. Gait retraining versus foot orthoses for patellofemoral pain: A pilot randomised clinical trial. J. Sci. Med. Sport 2018, 21, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Roosens, E.; Beaufils, C.; Busegnies, Y.; Van Tiggelen, D. Intrinsic risk factors associated with iliotibial band syndrome: A systematic review. Spor Hekim. Derg. 2023, 58, 094–101. [Google Scholar] [CrossRef]

| Mean | SD | |
|---|---|---|
| Age/years | 26.4 | ±4.3 |
| Height/cm | 174 | ±7.8 |
| Weight/kg | 68.3 | ±9.6 |
| Body Mass Index | 22.5 | ±2.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lescure, Y.; Nicolas, M.A.; Perrin, E.; Sanchis-Sales, E.; Lopezosa-Reca, E.; Travouillon, C.; Gijon-Nogueron, G. Biomechanical Strategies to Improve Running: Cadence, Footwear, and Orthoses—A Quasi-Experimental Study. Sensors 2025, 25, 2414. https://doi.org/10.3390/s25082414
Lescure Y, Nicolas MA, Perrin E, Sanchis-Sales E, Lopezosa-Reca E, Travouillon C, Gijon-Nogueron G. Biomechanical Strategies to Improve Running: Cadence, Footwear, and Orthoses—A Quasi-Experimental Study. Sensors. 2025; 25(8):2414. https://doi.org/10.3390/s25082414
Chicago/Turabian StyleLescure, Yves, Marie Adelaide Nicolas, Eleonore Perrin, Enrique Sanchis-Sales, Eva Lopezosa-Reca, Corentin Travouillon, and Gabriel Gijon-Nogueron. 2025. "Biomechanical Strategies to Improve Running: Cadence, Footwear, and Orthoses—A Quasi-Experimental Study" Sensors 25, no. 8: 2414. https://doi.org/10.3390/s25082414
APA StyleLescure, Y., Nicolas, M. A., Perrin, E., Sanchis-Sales, E., Lopezosa-Reca, E., Travouillon, C., & Gijon-Nogueron, G. (2025). Biomechanical Strategies to Improve Running: Cadence, Footwear, and Orthoses—A Quasi-Experimental Study. Sensors, 25(8), 2414. https://doi.org/10.3390/s25082414







