Contact-free Measurement of Heart Rate Variability via a Microwave Sensor
Abstract
:1. Introduction
2. Description of the Microwave Sensor
3. Signal Recording and Analyzing
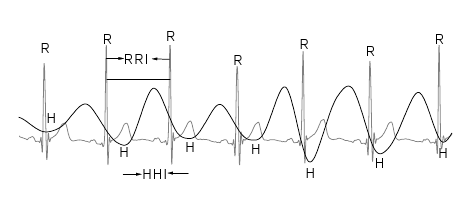
3.1. Extraction of HRV Signals Derived from ECG and Heartbeat
3.2. Measuring Parameters in RRI and HHI Recordings
3.2.1. Time Domain Parameters
3.2.2. Frequency Fomain Parameters
3.2.3. Poincaré Parameters
3.3. Statistical Analysis
4. Experimental Results
5. Discussion
6. Safety
Acknowledgments
References
- Hon, E.H.; Lee, S.T. Electronic evaluation of the fetal heart rate pattern preceding fetal death, further observation. Am. J. Obste. Gynecol. 1963, 87, 814–826. [Google Scholar]
- Ewing, D.J.; Martyn, C.N.; Young, R.J.; Clarke, B.F. The value of cardiovascular autonomic function tests: 10 years experience in diabetes. Diabetes Care 1985, 8, 491–498. [Google Scholar]
- Tulen, J.H.M.; Man int Veld, A.J.; van Steenis, H.G.; Mechelse, K. Sleep patterns and blood pressure variability in patients with pure autonomic failure. Clin. Auton. Res. 1991, 1, 309–315. [Google Scholar]
- Guzzetti, S.; Rovere, M.T.L.; Pinna, G.D.; Maestri, R.; Borroni, E.; Porta, A.; Mortara, A.; Malliani, A. Different spectral components of 24 h heart rate variability are related to different modes of death in chronic heart failure. Eur. Heart J. 2005, 26, 357–362. [Google Scholar]
- Chattipakorn, N.; Incharoen, T.; Kanlop, N. Chattipakorn, S. Heart rate variability in myocardial infarction and heart failure. Int. J. Cardio. 2007, 120, 289–296. [Google Scholar]
- Challoner, A.V.J.; Ramsay, C.A. A photoelectric plethysmograph for the measurement of cutaneous blood flow. Phys. Med. Biol. 1974, 19, 317–328. [Google Scholar]
- Dei, D.; Grazzini, G.; Luzi, G.; Pieraccini, M.; Atzeni, C.; Boncinelli, S.; Camiciottoli, G.; Castellani, W.; Marsili, M.; Dico, J.L. Non-contact detection of breathing using a microwave sensor. Sensors 2009, 9, 2574–2585. [Google Scholar]
- Xiao, Y.; Li, C.; Lin, J. A portable noncontact heartbeat and respiration monitoring system using 5-GHz radar. IEEE Sens. J. 2007, 7, 1042–1043. [Google Scholar]
- Brink, M.; Muller, C.H.; Schierz, C. Contact-free measurement of heart rate, respiration rate, and body movements during sleep. Behav. Res. Method. 2006, 38, 511–521. [Google Scholar]
- Kim, H.J.; Kim, K.H.; Hong, Y.S.; Choi, J.J. Measurement of human heartbeat and respiration signals using phase detection radar. Rev. Sci. Instr. 2007, 78, 104703. [Google Scholar]
- Matthews, G.; Sudduth, B.; Burrow, M. A non-contact vital signs monitor. Criti. Rev. Biomed. Eng. 2000, 28, 173–178. [Google Scholar]
- Caro, C.G.; Bloice, J.A. Contactless apnoea detector based on radar. Lancet 1971, 2, 959–961. [Google Scholar]
- Chen, K.M.; Huang, Y.; Zhang, J.; Norman, A. Microwave life-detection systems for searching human subjects under earthquake rubble or behind barrier. IEEE Trans. Biomed. Eng. 2000, 47, 105–114. [Google Scholar]
- Boric-Lubecke, O.; Lin, J.; Lubecke, V.M.; Host-Madsen, A.; Sizer, T. Microwave and millimeter-wave Doppler radar heart sensing; SPIE: Orlando, FL, USA, 2007; pp. 65470–65478. [Google Scholar]
- Hafner, N.; Mostafanezhad, I.; Lubecke, V.M.; Boric-Lubecke, O.; Host-Madsen, A. Non-contact cardiopulmonary sensing with a baby monitor. Proceedings of Annual International Conference of the IEEE Engineering in Medicine & Biology Society, Lyon, France; 2007; pp. 2300–2302. [Google Scholar]
- Greneker, E.F., III; Asbell, O.D.; Geisheimer, J.L. Radar detection device employing a scanning antenna system. U.S. Patent 7,199,749, 2007. [Google Scholar]
- Mcgrath, W.R. Remote-sensing method and device. U.S. Patent 7,272,431, 2007. [Google Scholar]
- Wang, J.Q.; Zheng, C.X.; Jin, X.J.; Lu, G.H.; Wang, H.B.; Ni, A.S. Study on a non-contact life parameter detection system using millimeter wave. Hangtian Yixue Yu Yixue Gongcheng/Space Med. Med. Eng. 2004, 17, 157–161. [Google Scholar]
- So, H.H.; Chan, K.L. Development of QRS detection method for real-time ambulatorycardiac monitor. Proceedings of IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA; 1997; pp. 289–292. [Google Scholar]
- Malik, M.; Bigger, J.T.; Camm, A. J.; Kleiger, R.E.; Malliani, A.; Moss, A.J.; Schwartz, P.J. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Eur. Heart J. 1996, 17, 354–381. [Google Scholar]
- Johnston, W.; Mendelson, Y. Extracting heart rate variability from a wearable reflectance pulse oximeter. Proceedings of the IEEE 31st Annual Northeast Bioengineering Conference, Hoboken, NJ, USA; 2005; pp. 157–158. [Google Scholar]
- Selvaraj, N.; Jaryal, A.; Santhosh, J.; Deepak, K.K.; Anand, S. Assessment of heart rate variability derived from finger-tip photoplethysmography as compared to electrocardiography. J. Med. Eng. Tech 2008, 32, 479–484. [Google Scholar]
- Chawla, M.P.S.; Verma, H.K.; Kumar, V. A new statistical PCA-ICA algorithm for location of R-peaks in ECG. Int. J. Cardio. 2008, 129, 146–148. [Google Scholar]
- Laguna, P.; Jané, R.; Olmos, S.; Thakor, N.; Rix, H.; Caminal, P. Adaptive estimation of QRS complex wave features of ECG signal by the hermite model. Med. Biolo. Eng. Comput. 1996, 34, 58–68. [Google Scholar]
- Matsui, T.; Arai, I.; Gotoh, S.; Hattori, H.; Takase, B.; Kikuchi, M.; Ishihara, M. A novel apparatus for non-contact measurement of heart rate variability: a system to prevent secondary exposure of medical personnel to toxic materials under biochemical hazard conditions, in monitoring sepsis or in predicting multiple organ dysfunction syndrome. Biom. Pharmacother. 2005, 59, S188–S191. [Google Scholar]
- Suzuki, S.; Matsui, T.; Gotoh, S.; Mori, Y.; Takase, B.; Ishihara, M. Development of Non-contact Monitoring System of Heart Rate Variability (HRV)–An Approach of Remote Sensing for Ubiquitous Technology. In Ergonomics and Health Aspects of Work with Computers; Springer: New York, NY, USA, 2009; pp. 195–203. [Google Scholar]
- Tavakolian, K.; Zadeh, F.M.; Chuo, Y.; Vaseghi, A.; Kaminska, B. Development of a novel contactless mechanocardiograph device. Int. J. Telemed. Appl. 2008. [Google Scholar] [CrossRef]
- Kondo, T.; Uhlig, T.; Pemberton, P.; Sly, P.D. Laser monitoring of chest wall displacement. Eur. Resp. J. 1997, 10, 1865–1869. [Google Scholar]
- Wang, J.; Zheng, C.; Lu, G.; Jing, X. A New Method for Identifying the Life Parameters via Radar. EURASIP J. Adv. Signal Process. 2007, 101, 8–16. [Google Scholar]
- Morgan, R.D.; Zierdt, G.M. Novel signal processing techniques for Doppler radar cardiopulmonary sensing. Signal Process 2009, 89, 45–66. [Google Scholar]
- Adam, S.F. Microwave theory and applications; Prentice-Hall: Upper Saddle River, NJ, USA, 1969. [Google Scholar]
- Zhang, J.; Yang, M.; Zheng, S.; Sun, X. A low-cost Doppler radar system with 24 GHz PLL for remote detection of heart beat. Micro. Optical Tech. Lett. 2008, 50, 3139–3142. [Google Scholar]
- Lin, J.C. A new IEEE standard for safety levels with respect to human exposure to radio-frequency radiation. IEEE Ant. Propag. Mag. 2006, 48, 157–159. [Google Scholar]



| Parameters | ECG | Heartbeat | P value |
|---|---|---|---|
| Time domain | |||
| Mean NN (ms) | 858.00 ± 127.14 | 857.99 ± 127.20 | 0.99 |
| SDNN (ms) | 50.72 ± 28.67 | 52.11 ± 28.42 | 0.39 |
| RMSSD (ms) | 47.88 ± 34.59 | 50.77 ± 34.02 | 0.25 |
| PNN50 (%) | 20.35 ± 17.88 | 23.00 ± 18.26 | 0.37 |
| Frequency domain | |||
| Log of LF Power | 2.43 ± 0.46 | 2.45 ± 0.45 | 0.86 |
| Log of HF Power | 2.30 ± 0.46 | 2.34 ± 0.45 | 0.67 |
| Lg(LF)/Lg(HF) | 1.07 ± 0.19 | 1.06 ± 0.17 | 0.72 |
| Poincare' plot | |||
| SD1 (ms) | 34.35 ± 24.70 | 36.45 ± 24.25 | 0.27 |
| SD2 (ms) | 72.10 ± 33.17 | 73.06 ± 33.18 | 0.83 |
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Lu, G.; Yang, F.; Tian, Y.; Jing, X.; Wang, J. Contact-free Measurement of Heart Rate Variability via a Microwave Sensor. Sensors 2009, 9, 9572-9581. https://doi.org/10.3390/s91209572
Lu G, Yang F, Tian Y, Jing X, Wang J. Contact-free Measurement of Heart Rate Variability via a Microwave Sensor. Sensors. 2009; 9(12):9572-9581. https://doi.org/10.3390/s91209572
Chicago/Turabian StyleLu, Guohua, Fang Yang, Yue Tian, Xijing Jing, and Jianqi Wang. 2009. "Contact-free Measurement of Heart Rate Variability via a Microwave Sensor" Sensors 9, no. 12: 9572-9581. https://doi.org/10.3390/s91209572
APA StyleLu, G., Yang, F., Tian, Y., Jing, X., & Wang, J. (2009). Contact-free Measurement of Heart Rate Variability via a Microwave Sensor. Sensors, 9(12), 9572-9581. https://doi.org/10.3390/s91209572