A Pilot Safety Assessment for Recombinant Epinephelus lanceolatus Piscidin Yeast Powder as a Drug Food Additive after Subacute and Subchronic Administration to SD Rats
Abstract
1. Introduction
2. Results
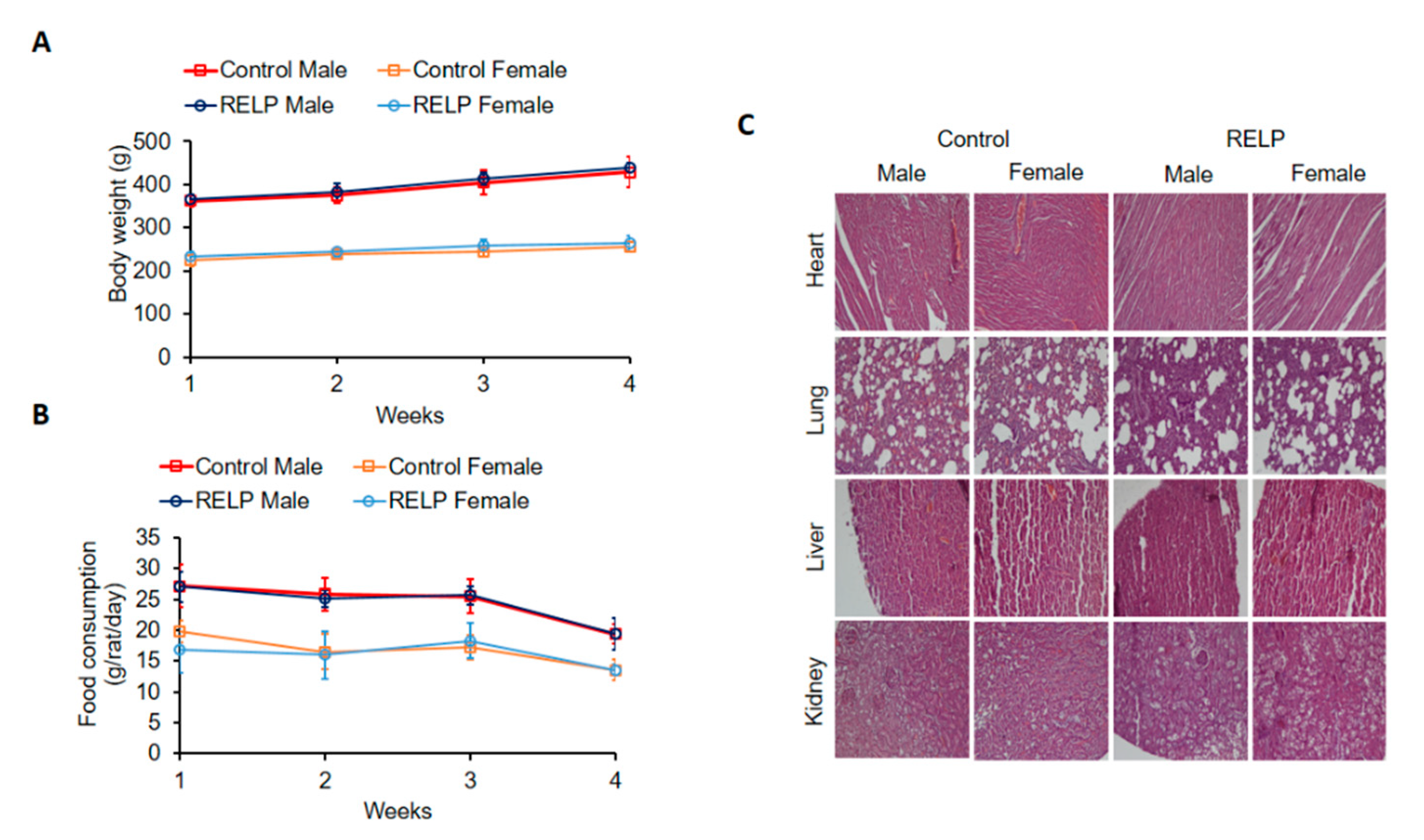
2.1. Subacute Toxicity of RELP in SD Rats
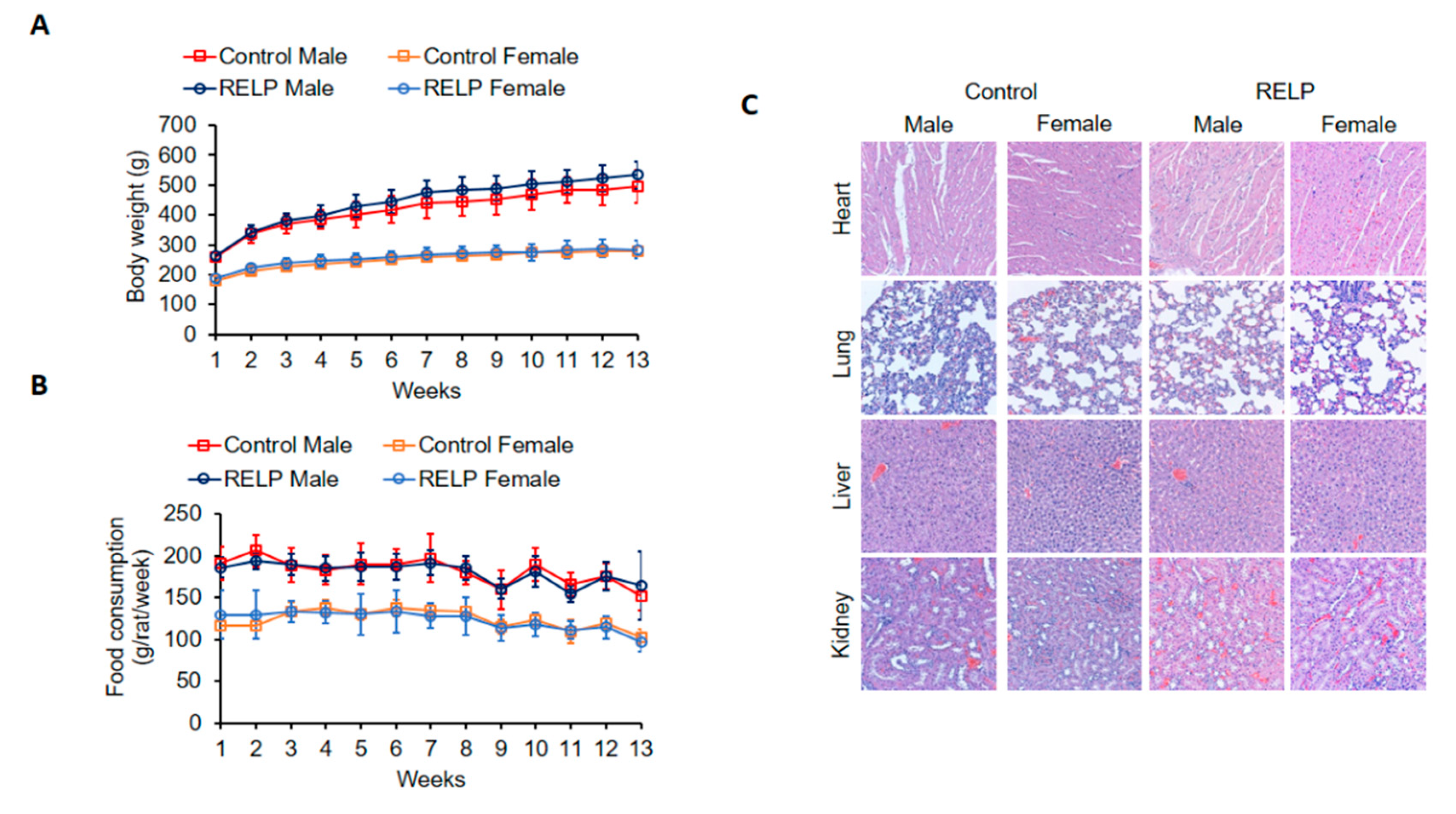
2.2. Subchronic Toxicity of RELP in SD Rats
3. Discussion
4. Materials and Methods
4.1. Recombinant Epinephelus Lanceolatus Piscidin Yeast Powder
4.2. Animals and Experimental Design
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Martin, M.J.; Thottathil, S.E.; Newman, T.B. Antibiotics Overuse in Animal Agriculture: A Call to Action for Health Care Providers. Am. J. Public Health 2015, 105, 2409–2410. [Google Scholar] [CrossRef] [PubMed]
- Maron, D.F.; Smith, T.J.S.; Nachman, K.E. Restrictions on antimicrobial use in food animal production: An international regulatory and economic survey. Glob. Health 2013, 9, 48. [Google Scholar] [CrossRef] [PubMed]
- Lillehoj, H.; Liu, Y.H.; Calsamiglia, S.; Fernandez-Miyakawa, M.E.; Chi, F.; Cravens, R.L.; Oh, S.; Gay, C.G. Phytochemicals as antibiotic alternatives to promote growth and enhance host health. Vet. Res. 2018, 49, 76. [Google Scholar] [CrossRef] [PubMed]
- Tai, H.M.; Huang, H.N.; Tsai, T.Y.; You, M.F.; Wu, H.Y.; Rajanbabu, V.; Chang, H.Y.; Pan, C.Y.; Chen, J.Y. Dietary supplementation of recombinant antimicrobial peptide Epinephelus lanceolatus piscidin improves growth performance and immune response in Gallus gallus domesticus. PLoS ONE 2020, 15, e023002. [Google Scholar] [CrossRef]
- Su, Y.L.; Chen, G.; Chen, L.S.; Li, J.Z.; Wang, G.; He, J.Y.; Zhan, T.Y.; Li, Y.W.; Yan, M.T.; Huang, Y.H.; et al. Effects of antimicrobial peptides on serum biochemical parameters, antioxidant activity and non-specific immune responses in Epinephelus coioides. Fish Shellfish Immun. 2019, 86, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Ting, C.H.; Pan, C.Y.; Chen, Y.C.; Lin, Y.C.; Chen, T.Y.; Rajanbabu, V.; Chen, J.Y. Impact of Tilapia hepcidin 2-3 dietary supplementation on the gut microbiota profile and immunomodulation in the grouper (Epinephelus lanceolatus). Sci. Rep. 2019, 9, 1–17. [Google Scholar] [CrossRef]
- Chen, H.C.; Pan, C.Y.; Rajanbabu, V.; Lee, Y.Y.; Tsai, W.R.; Chen, J.Y. Lack of Acute Toxicity and Mutagenicity from Recombinant Epinephelus lanceolatus Piscidin Expressed in Pichia pastoris. Mar. Drugs 2020, 18, 206. [Google Scholar] [CrossRef]
- Wang, S.; Zeng, X.F.; Yang, Q.; Qiao, S.Y. Antimicrobial Peptides as Potential Alternatives to Antibiotics in Food Animal Industry. Int. J. Mol. Sci. 2016, 17, 603. [Google Scholar] [CrossRef]
- Li, Z.; Hu, Y.H.; Yang, Y.Y.; Lu, Z.Q.; Wang, Y.Z. Antimicrobial resistance in livestock: Antimicrobial peptides provide a new solution for a growing challenge. Anim. Front. 2018, 8, 21–29. [Google Scholar] [CrossRef]
- Liu, Q.; Yao, S.H.; Chen, Y.; Gao, S.; Yang, Y.Y.; Deng, J.L.; Ren, Z.H.; Shen, L.H.; Cui, H.M.; Hu, Y.C.; et al. Use of antimicrobial peptides as a feed additive for juvenile goats. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Lima, S.M.F.; Freire, M.S.; Gomes, A.L.O.; Cantuaria, A.P.C.; Dutra, F.R.P.; Magalhaes, B.S.; Sousa, M.G.C.; Migliolo, L.; Almeida, J.A.; Franco, O.L.; et al. Antimicrobial and immunomodulatory activity of host defense peptides, clavanins and LL-37, in vitro: An endodontic perspective. Peptides 2017, 95, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.C.; Liu, X.M.; Bu, L.Z.; Li, H.Y.; Zhang, S.C. Antimicrobial-immunomodulatory activities of zebrafish phosvitin-derived peptide Pt5. Peptides 2012, 37, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Huang, C.L.; Wang, J.J.; Zhou, H.; Lu, Y.Y.; Lou, L.H.; Zheng, J.Y.; Tian, L.; Wang, X.P.; Cao, Z.W.; et al. Dysbiosis of intestinal microbiota and decrease in paneth cell antimicrobial peptide level during acute necrotizing pancreatitis in rats. PLoS ONE 2017, 12, e0176583. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, B.; Munoz-Garay, C. Marine Antimicrobial Peptides: A Promising Source of New Generation Antibiotics and Other Bio-active Molecules. Int. J. Pept. Res. Ther. 2019, 25, 1441–1450. [Google Scholar] [CrossRef]
- Guex, C.G.; Reginato, F.Z.; Figueredo, K.C.; da Silva, A.R.H.D.; Pires, F.B.; Jesus, R.D.; Lhamas, C.L.; Lopes, G.H.H.; Bauermann, L.D. Safety assessment of ethanolic extract of Olea europaea L. leaves after acute and subacute administration to Wistar rats. Regul. Toxicol. Pharm. 2018, 95, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Assad, N.; Sood, A.; Campen, M.J.; Zychowski, K.E. Metal-Induced Pulmonary Fibrosis. Curr. Environ. Health Rep. 2018, 5, 486–498. [Google Scholar] [CrossRef]
- Orr, S.E.; Bridges, C.C. Chronic Kidney Disease and Exposure to Nephrotoxic Metals. Int. J. Mol. Sci. 2017, 18, 1039. [Google Scholar]
- Baralic, K.; Djordjevic, A.B.; Zivancevic, K.; Antonijevic, E.; Andelkovic, M.; Javorac, D.; Curcic, M.; Bulat, Z.; Antonijevic, B.; Dukic-Cosic, D. Toxic Effects of the Mixture of Phthalates and Bisphenol A-Subacute Oral Toxicity Study in Wistar Rats. Int. J. Environ. Res. Public Health 2020, 17, 746. [Google Scholar] [CrossRef]
- Figueredo, K.C.; Guex, C.G.; Reginato, F.Z.; da Silva, A.R.H.; Cassanego, G.B.; Lhamas, C.L.; Boligon, A.A.; Lopes, G.H.H.; Bauermann, L.D. Safety assessment of Morus nigra L. leaves: Acute and subacute oral toxicity studies in Wistar rats. J. Ethnopharmacol. 2018, 224, 290–296. [Google Scholar] [CrossRef]
- Kamsani, N.E.; Zakaria, Z.A.; Nasir, N.L.M.; Mohtarrudin, N.; Alitheen, N.B.M. Safety Assessment of Methanol Extract of Melastoma malabathricum L. Leaves following the Subacute and Subchronic Oral Consumptions in Rats and Its Cytotoxic Effect against the HT29 Cancer Cell Line. Evid. Based Complement. Altern. Med. 2019, 2019, 5207958. [Google Scholar] [CrossRef]
- Miners, J.O.; Yang, X.; Knights, K.M.; Zhang, L. The Role of the Kidney in Drug Elimination: Transport, Metabolism, and the Impact of Kidney Disease on Drug Clearance. Clin. Pharmacol. Ther. 2017, 102, 436–449. [Google Scholar] [CrossRef] [PubMed]
- Elston, A.C.; Bayliss, M.K.; Park, G.R. Effect of Renal-Failure on Drug-Metabolism by the Liver. Br. J. Anaesth. 1993, 71, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Vanbezooijen, C.F.A.; Trommelen, G.; Vanoorschot, R.; Sakkee, N.; Groen, C. The Effect of Age on the Metabolism of Drugs by the Liver. Age 1987, 10, 104. [Google Scholar]
- Nistiar, F.; Racz, O.; Lukacinova, A.; Hubkova, B.; Novakova, J.; Lovasova, E.; Sedlakova, E. Age dependency on some physiological and biochemical parameters of male Wistar rats in controlled environment. J. Environ. Sci. Health A 2012, 47, 1224–1233. [Google Scholar] [CrossRef]
- Bhatt, V.; Saleem, A. Drug-induced neutropenia—Pathophysiology, clinical features, and management. Ann. Clin. Lab. Sci. 2004, 34, 131–137. [Google Scholar]
- EFSA Panel on Additives and Products or Substances used in Animal Feed. Guidance on the assessment of the safety of feed additives for the target species. EFSA J. 2017, 15, e05021. [Google Scholar]
| Male | Female | |||
|---|---|---|---|---|
| Control (n = 5) | RELP (n = 5) | Control (n = 5) | RELP (n = 5) | |
| Mean bodyweight (g) | 424.32 ± 29.95 | 422.34 ± 46.4 | 241.42 ± 10.59 | 253.94 ± 17.21 |
| Lung (g) | 1.6 ± 0.31 | 1.7 ± 0.14 | 1.2 ± 0.08 | 1.26 ± 0.22 |
| Liver (g) | 12.48 ± 1.66 | 13.16 ± 0.83 | 7.77 ± 1.3 | 7.89 ± 0.83 |
| Heart (g) | 1.64 ± 0.22 | 1.72 ± 0.2 | 1 ± 0.09 | 0.95 ± 0.11 |
| Kidney (g) | 2.14 ± 0.23 | 2.25 ± 0.32 | 1.28 ± 0.14 | 1.27 ± 0.19 |
| Parameters | Male | Female | ||
|---|---|---|---|---|
| Control (n = 5) | RELP (n = 5) | Control (n = 5) | RELP (n = 5) | |
| WBC (K/μL) | 8.99 ± 4.56 | 9.76 ± 5.46 | 11.34 ± 6.47 | 4.42 ± 1.15 |
| NEU (K/μL) | 0.84 ± 0.47 | 1.08 ± 0.85 | 0.79 ± 0.53 | 0.47 ± 0.28 |
| LYM (K/μL) | 7.72 ± 3.91 | 8.08 ± 4.62 | 10.15 ± 5.73 | 3.79 ± 1.01 |
| MONO (K/μL) | 0.35 ± 0.26 | 0.46 ± 0.41 | 0.29 ± 0.25 | 0.13 ± 0.07 |
| EOS (K/μL) | 0.07 ± 0.06 | 0.10 ± 0.11 | 0.08 ± 0.07 | 0.02 ± 0.01 |
| BASO (K/μL) | 0.02 ± 0.02 | 0.04 ± 0.03 | 0.03 ± 0.02 | 0.01 ± 0.01 |
| RBC (M/μL) | 9.37 ± 0.31 | 9.00 ± 0.74 | 8.69 ± 0.66 | 8.46 ± 0.52 |
| HGB (g/dL) | 17.14 ± 0.63 | 16.82 ± 1.40 | 15.9 ± 1.09 | 15.43 ± 0.84 |
| HCT (%) | 52.86 ± 1.30 | 50.66 ± 4.77 | 48.74 ± 3.99 | 46.75 ± 2.63 |
| MCV (fL) | 56.44 ± 0.84 | 56.26 ± 0.93 | 56.04 ± 1.11 | 55.28 ± 1.11 |
| MCH (pg) | 18.28 ± 0.44 | 18.72 ± 0.46 | 18.30 ± 0.53 | 18.25 ± 0.17 |
| MCHC (g/dL) | 32.42 ± 0.63 | 33.24 ± 0.76 | 32.64 ± 0.65 | 33.00 ± 0.35 |
| RDW (%) | 20.00 ± 0.39 | 19.70 ± 1.53 | 18.96 ± 0.83 | 18.98 ± 1.00 |
| RET (K/μL) | 240.12 ± 48.68 | 241.88 ± 41.57 | 273.66 ± 62.79 | 243.93 ± 13.40 |
| PLT (109/L) | 812 ± 348.23 | 837.00 ± 161.20 | 1078.80 ± 176.70 | 920.25 ± 85.47 |
| MPV (fL) | 8.18 ± 0.19 | 8.52 ± 0.26 | 8.26 ± 0.34 | 8.63 ± 0.05 |
| PCT (%) | 0.77 ± 0.33 | 0.85 ± 0.16 | 0.90 ± 0.13 | 0.81 ± 0.08 |
| PDW (fL) | 9.32 ± 0.51 | 9.82 ± 0.30 | 8.60 ± 0.39 | 9.05 ± 0.34 |
| Parameters | Male | Female | ||
|---|---|---|---|---|
| Control (n = 5) | RELP (n = 5) | Control (n = 5) | RELP (n = 5) | |
| GOT (U/L) | 96.40 ± 24.53 | 98.40 ± 36.25 | 78.40 ± 16.91 | 65.60 ± 14.94 |
| GPT (U/L) | 30.40 ± 3.91 | 50.60 ± 26.59 | 28.40 ± 6.88 | 29.80 ± 10.45 |
| LDH (U/L) | 452.80 ± 250.21 | 538.80 ± 85.53 | 217.60 ± 64.02 | 258.40 ± 107.16 |
| ALP (U/L) | 611.20 ± 186.06 | 513.00 ± 68.60 | 303.00 ± 110.77 | 278.40 ± 64.31 |
| TBIL (mg/dL) | 0.44 ± 0.15 | 0.70 ± 0.35 | 0.40 ± 0.7 | 0.36 ± 0.05 |
| TP (g/dL) | 6.64 ± 0.30 | 7.22 ± 1.51 | 7.46 ± 0.48 | 7.38 ± 0.65 |
| IP (mg/dL) | 11.08 ± 0.87 | 12.08 ± 1.54 | 9.32 ± 1.40 | 8.62 ± 0.58 |
| BUN (mg/dL) | 14.34 ± 2.09 | 16.10 ± 4.04 | 13.82 ± 3.15 | 14.16 ± 2.35 |
| CRE (mg/dL) | 0.36 ± 0.13 | 0.36 ± 0.15 | 0.24 ± 0.05 | 0.26 ± 0.09 |
| UA (mg/dL) | 2.38 ± 0.80 | 3.40 ± 1.47 | 1.98 ± 0.67 | 2.10 ± 0.68 |
| Ca (mg/dL) | 11.35 ± 0.72 | 11.92 ± 1.61 | 11.40 ± 0.55 | 11.40 ± 0.37 |
| Mg (mg/dL) | 3.54 ± 0.27 | 4.12 ± 0.75 | 3.28 ± 0.43 | 3.4 ± 0.25 |
| ALB (g/dL) | 4.60 ± 0.32 | 4.94 ± 0.55 | 5.14 ± 0.50 | 4.78 ± 0.24 |
| NH3 (μg/dL) | 187.60 ± 41.05 | 207.75 ± 46.80 | 147.60 ± 33.95 | 162.20 ± 31.09 |
| Male | Female | |||
|---|---|---|---|---|
| Control (n = 5) | RELP (n = 5) | Control (n = 4) | RELP (n = 4) | |
| Mean bodyweight (g) | 496.32 ± 52.1 | 534.2 ± 41.8 | 278.8 ± 11.8 | 284.2 ± 28.4 |
| Lung (g) | 2 ± 0.2 | 2.1 ± 0.2 | 1.5 ± 0.1 | 1.6 ± 0.1 |
| Liver (g) | 15.9 ± 2.9 | 18.5 ± 2.3 | 9.4 ± 1 | 9.69 ± 0.9 |
| Heart (g) | 1.7 ± 0.3 | 1.7 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.1 |
| Kidney (g) | 3.7 ± 0.5 | 4.1 ± 0.3 | 2.2 ± 0.2 | 2.2 ± 0.1 |
| Parameters | Male | Female | ||
|---|---|---|---|---|
| Control (n = 5) | RELP (n = 5) | Control (n = 4) | RELP (n = 4) | |
| WBC (K/μL) | 8.51 ± 2.81 | 6.47 ± 1.41 | 6.61 ± 1.93 | 6.14 ± 2.84 |
| NEU (K/μL) | 1.47 ± 0.79 | 1.09 ± 0.60 | 0.99 ± 0.46 | 1.22 ± 0.84 |
| LYM (K/μL) | 6.53 ± 2.47 | 4.37 ± 2.12 | 5.17 ± 1.38 | 4.59 ± 1.96 |
| MONO (K/μL) | 0.37 ± 0.14 | 0.19 ± 0.07 | 0.35 ± 0.18 | 0.23 ± 0.18 |
| EOS (K/μL) | 0.13 ± 0.06 | 0.15 ± 0.07 | 0.09 ± 0.02 | 0.10 ± 0.04 |
| BASO (K/μL) | 0.01 ± 0.01 | 0.01 ± 0.01 | 0.01 ± 0.01 | 0.01 ± 0.00 |
| RBC (M/μL) | 9.11 ± 0.73 | 9.22 ± 0.35 | 8.22 ± 0.27 | 7.91 ± 0.79 |
| HGB (g/dL) | 15.67 ± 1.02 | 15.43 ± 0.78 | 14.98 ± 0.46 | 14.13 ± 0.94 |
| HCT (%) | 50.26 ± 4.44 | 49.77 ± 2.38 | 46.44 ± 2.21 | 45.08 ± 4.00 |
| MCV (fL) | 55.16 ± 1.63 | 53.98 ± 2.08 | 56.50 ± 1.15 | 57.02 ± 0.93 |
| MCH (pg) | 17.23 ± 0.53 | 16.73 ± 0.59 | 18.24 ± 0.26 | 17.90 ± 0.71 |
| MCHC (g/dL) | 31.26 ± 0.81 | 31.00 ± 0.40 | 32.30 ± 0.89 | 31.40 ± 0.84 |
| RDW (%) | 21.04 ± 1.34 | 21.80 ± 0.67 | 17.94 ± 1.23 | 17.83 ± 1.87 |
| RET (K/μL) | 245.51 ± 39.99 | 230.62 ± 24.02 | 233.16 ± 26.69 | 244.77 ± 31.13 |
| PLT (109/L) | 579.29 ± 330.14 | 769.67 ± 90.10 | 712.80 ± 138.34 | 612.50 ± 395.52 |
| MPV (fL) | 7.87 ± 1.10 | 7.62 ± 0.45 | 7.88 ± 0.40 | 7.63 ± 0.33 |
| PCT (%) | 0.46 ± 0.24 | 0.69 ± 0.04 | 0.60 ± 0.07 | 0.50 ± 0.28 |
| PDW (fL) | 7.71 ± 0.31 | 8.22 ± 0.57 | 7.90 ± 0.24 | 8.17 ± 0.51 |
| Parameters | Male | Female | ||
|---|---|---|---|---|
| Control (n = 5) | RELP (n = 5) | Control (n = 4) | RELP (n = 4) | |
| GOT (U/L) | 145.57 ± 108.95 | 117.33 ± 44.03 | 81.60 ± 11.84 | 82.67 ± 25.93 |
| GPT (U/L) | 47.43 ± 21.49 | 41.50 ± 7.82 | 39.00 ± 10.34 | 36.83 ± 8.93 |
| LDH (U/L) | 1496.29 ± 1129.76 | 1496.67 ± 615.96 | 485.40 ± 431.91 | 947.67 ± 503.84 |
| ALP (U/L) | 930.71 ± 522.37 | 805.50 ± 95.69 | 322.80 ± 53.42 | 938.67 ± 511.45 |
| TBIL (mg/dL) | 0.53 ± 0.45 | 0.30 ± 0.09 | 0.28 ± 0.08 | 0.27 ± 0.08 |
| TP (g/dL) | 6.33 ± 0.49 | 6.20 ± 0.45 | 6.52 ± 0.29 | 6.55 ± 0.46 |
| IP (mg/dL) | 7.83 ± 1.43 | 8.07 ± 1.01 | 6.96 ± 0.85 | 7.63 ± 0.79 |
| BUN (mg/dL) | 17.37 ± 1.71 | 18.50 ± 2.43 | 16.56 ± 3.40 | 18.13 ± 1.59 |
| CRE (mg/dL) | 0.30 ± 0.06 | 0.31 ± 0.06 | 0.36 ± 0.11 | 0.31 ± 0.07 |
| UA (mg/dL) | 1.74 ± 0.44 | 2.38 ± 0.63 | 1.72 ± 0.40 | 1.52 ± 0.37 |
| Ca (mg/dL) | 9.77 ± 0.33 | 10.32 ± 0.67 | 10.88 ± 0.39 | 10.93 ± 1.12 |
| Mg (mg/dL) | 2.54 ± 0.36 | 3.28 ± 0.52 | 2.60 ± 0.19 | 2.98 ± 0.26 |
| ALB (g/dL) | 4.40 ± 0.61 | 4.30 ± 0.32 | 4.82 ± 0.52 | 4.95 ± 0.72 |
| NH3 (μg/dL) | 159.29 ± 68.63 | 220.17 ± 72.45 | 132.80 ± 39.18 | 155.83 ± 29.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, B.-C.; Li, C.-C.; Liu, C.-W.; Chen, J.-Y. A Pilot Safety Assessment for Recombinant Epinephelus lanceolatus Piscidin Yeast Powder as a Drug Food Additive after Subacute and Subchronic Administration to SD Rats. Mar. Drugs 2020, 18, 586. https://doi.org/10.3390/md18120586
Su B-C, Li C-C, Liu C-W, Chen J-Y. A Pilot Safety Assessment for Recombinant Epinephelus lanceolatus Piscidin Yeast Powder as a Drug Food Additive after Subacute and Subchronic Administration to SD Rats. Marine Drugs. 2020; 18(12):586. https://doi.org/10.3390/md18120586
Chicago/Turabian StyleSu, Bor-Chyuan, Chao-Chin Li, Chia-Wen Liu, and Jyh-Yih Chen. 2020. "A Pilot Safety Assessment for Recombinant Epinephelus lanceolatus Piscidin Yeast Powder as a Drug Food Additive after Subacute and Subchronic Administration to SD Rats" Marine Drugs 18, no. 12: 586. https://doi.org/10.3390/md18120586
APA StyleSu, B.-C., Li, C.-C., Liu, C.-W., & Chen, J.-Y. (2020). A Pilot Safety Assessment for Recombinant Epinephelus lanceolatus Piscidin Yeast Powder as a Drug Food Additive after Subacute and Subchronic Administration to SD Rats. Marine Drugs, 18(12), 586. https://doi.org/10.3390/md18120586





