Chitosan/Albumin Coating Factorial Optimization of Alginate/Dextran Sulfate Cores for Oral Delivery of Insulin
Abstract
1. Introduction
2. Results and Discussion
2.1. Preparation and Characterization of Nanoparticles
2.2. Fitting Data of Dependent Variables to Model Statistics
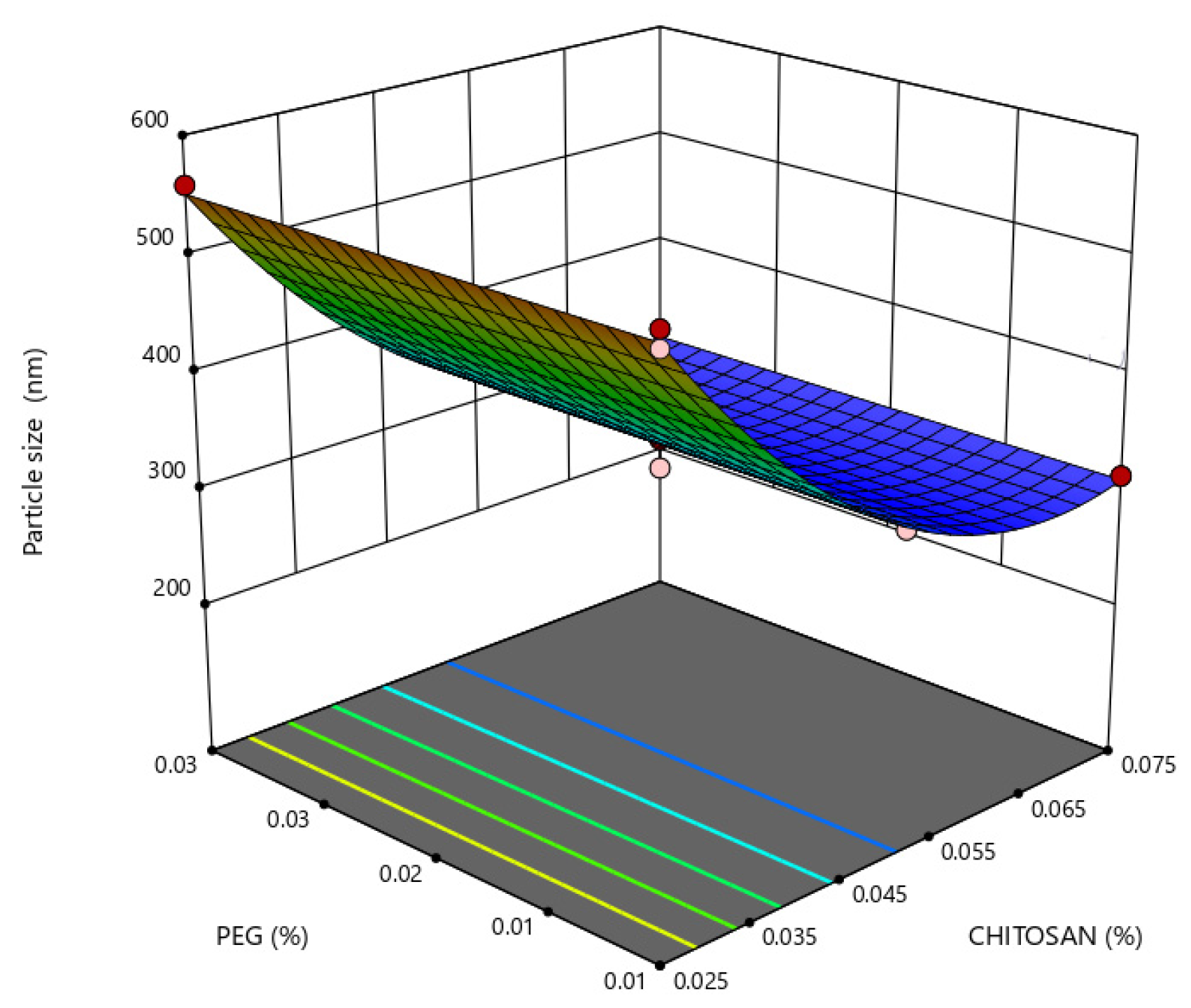
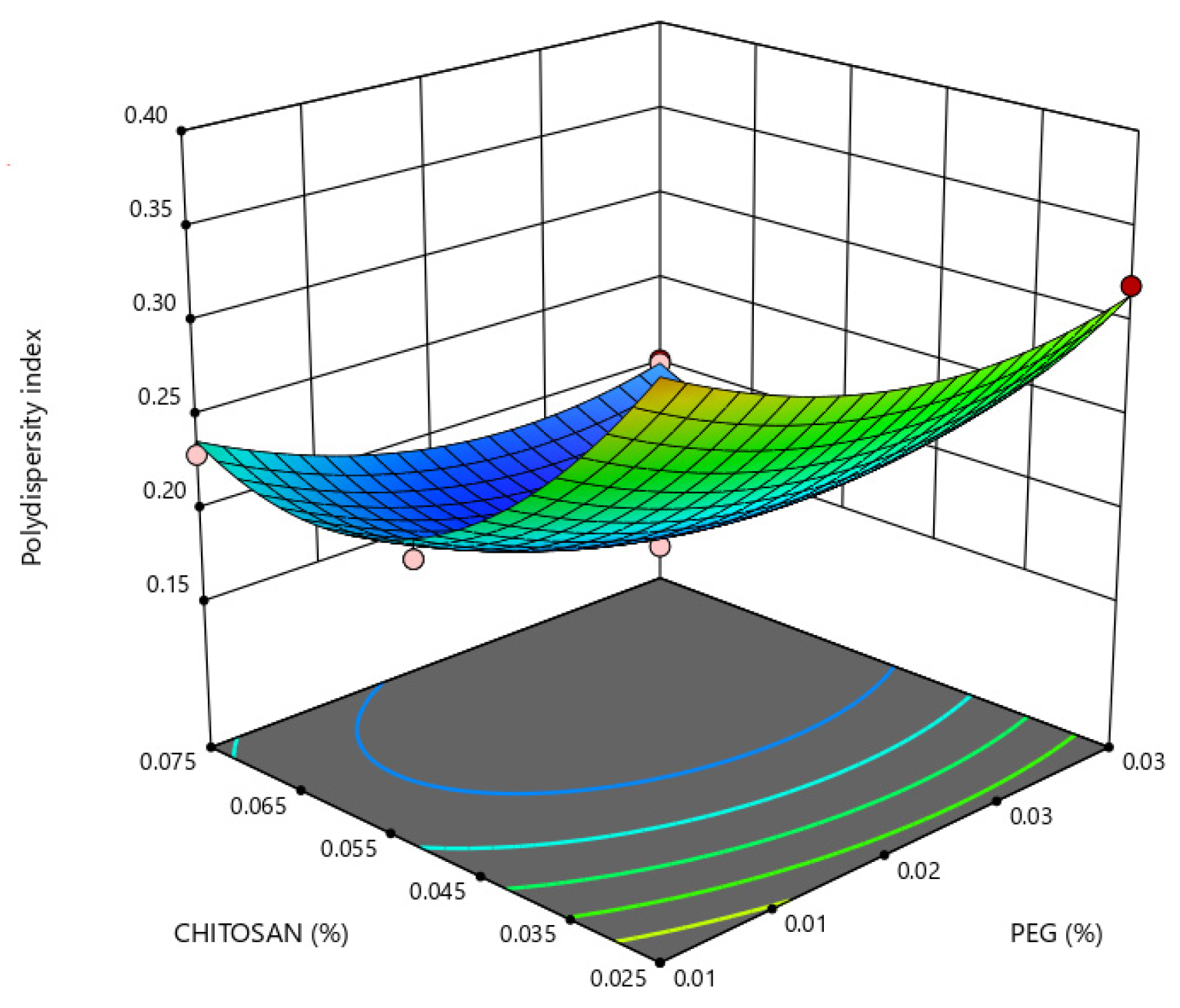
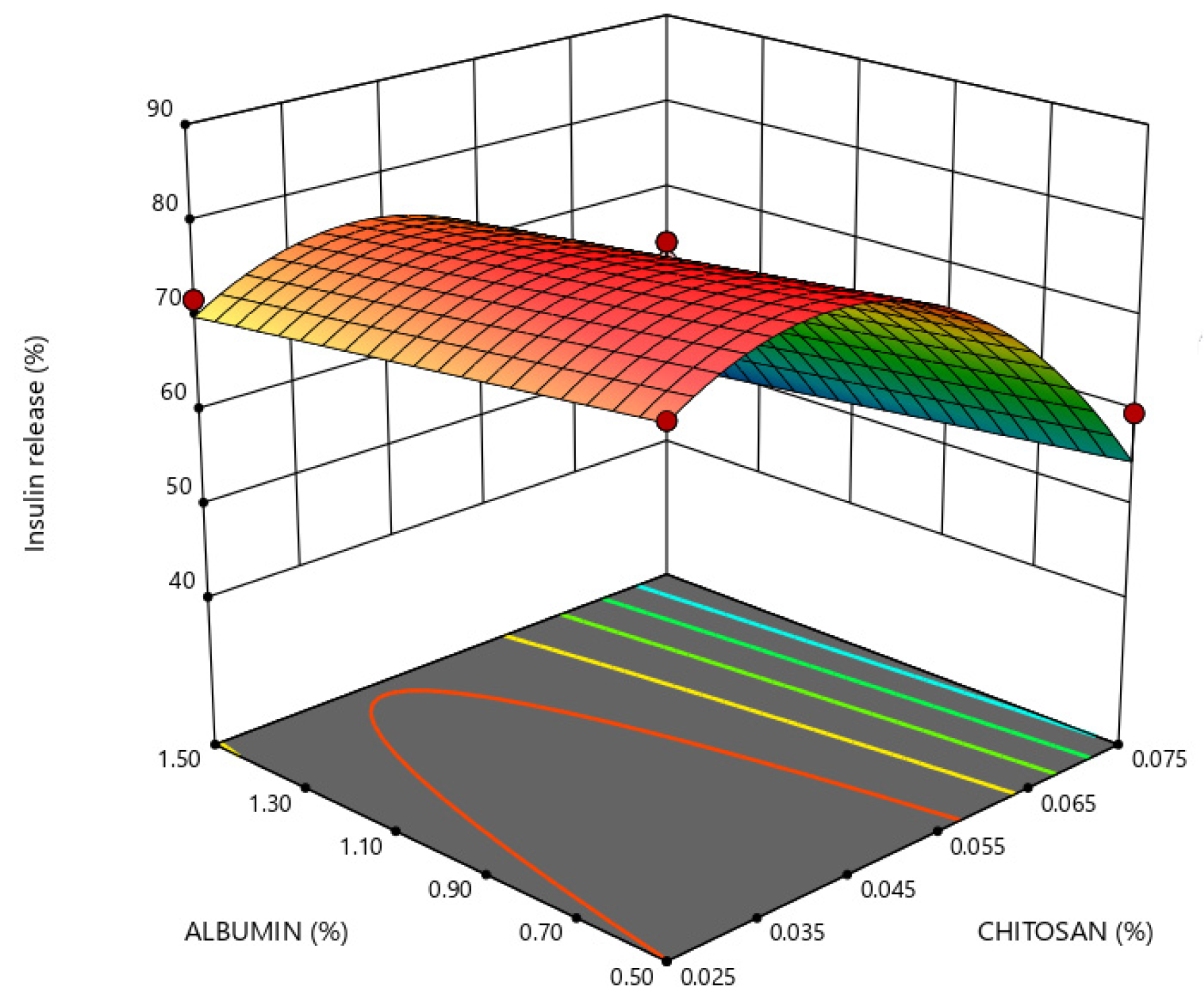
2.3. Response Surface Analysis
2.4. Optimization and Model Validation
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Methods
4.2.1. Preparation of Nanoparticles
4.2.2. Particle Size Analysis
4.2.3. Zeta Potential Analysis
4.2.4. Insulin Release Studies
4.2.5. Insulin Determination
4.2.6. Conformational Stability of Insulin
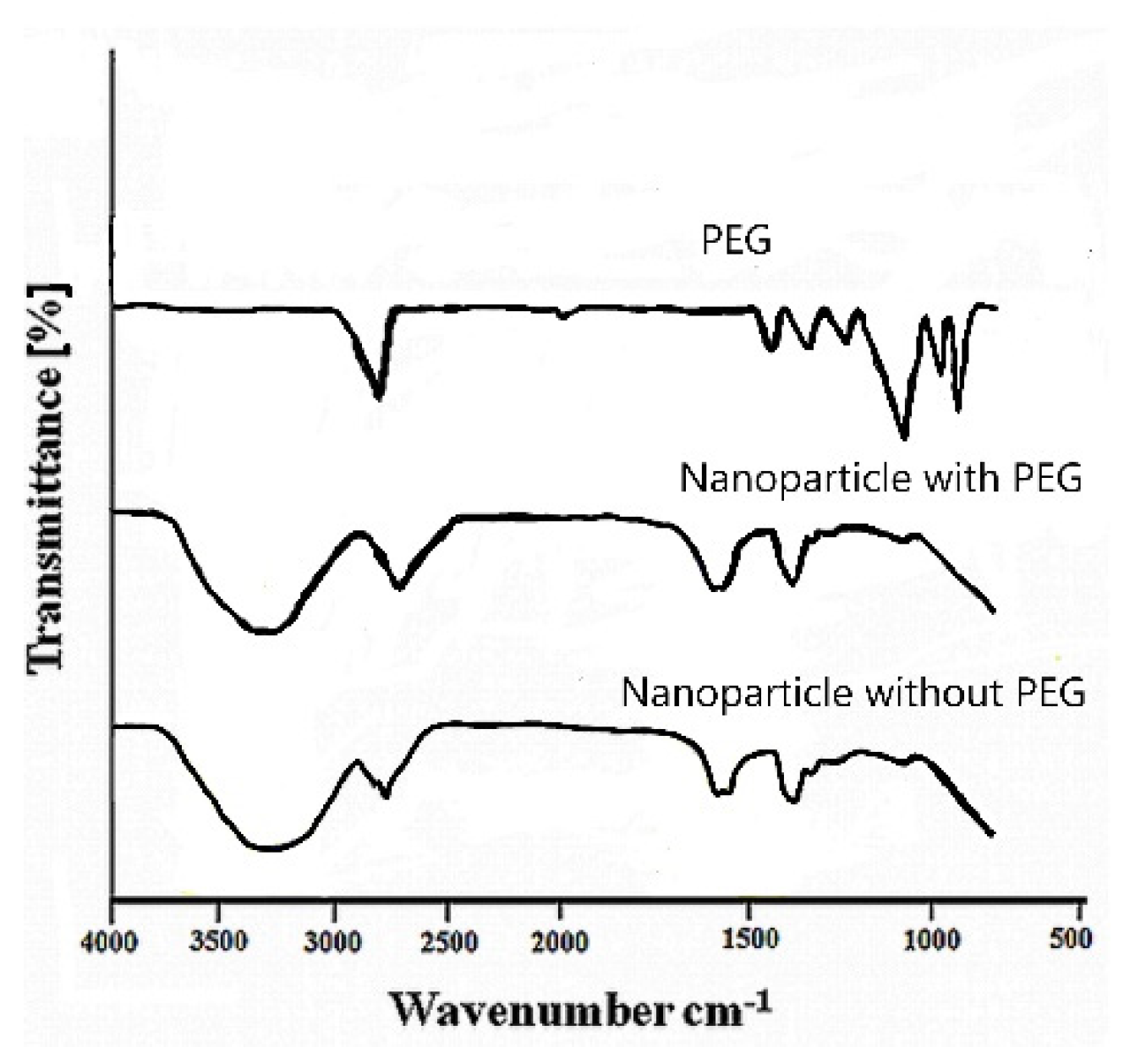
4.2.7. Fourier Transform Infrared (FTIR) Spectroscopy
4.2.8. Experimental Design
4.2.9. Analysis of Experimental Data and Model Validation
4.2.10. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Drucker, D.J. Transforming Type 1 Diabetes: The next Wave of Innovation. Diabetologia 2021, 64, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Singh, A.; Singh, R.; Misra, A. Once-Weekly Basal Insulin Icodec: Looking ONWARDS from Pharmacology to Clinical Trials. Diabetes Metab. Syndr. Clin. Res. Rev. 2022, 16, 102615. [Google Scholar] [CrossRef] [PubMed]
- Halberg, I.B.; Lyby, K.; Wassermann, K.; Heise, T.; Zijlstra, E.; Plum-Mörschel, L. Efficacy and Safety of Oral Basal Insulin versus Subcutaneous Insulin Glargine in Type 2 Diabetes: A Randomised, Double-Blind, Phase 2 Trial. Lancet Diabetes Endocrinol. 2019, 7, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J. Advances in Oral Peptide Therapeutics. Nat. Rev. Drug Discov. 2020, 19, 277–289. [Google Scholar] [CrossRef]
- Oramed Announces Top-Line Results from Phase 3 Trial of ORMD-0801 for the Treatment of Type 2 Diabetes—Oramed Pharmaceuticals. Available online: https://oramed.com/oramed-announces-top-line-results-from-phase-3-trial-of-ormd-0801-for-the-treatment-of-type-2-diabetes/ (accessed on 1 February 2023).
- Lopes, M.; Simões, S.; Veiga, F.; Seiça, R.; Ribeiro, A. Why Most Oral Insulin Formulations Do Not Reach Clinical Trials. Ther. Deliv. 2015, 6, 973–987. [Google Scholar] [CrossRef]
- Ribeiro, A.J.; Seiça, R.; Veiga, F. Nanoparticles for Oral Delivery of Insulin. In Drug Delivery Systems: Advanced Technologies Potentially Applicable in Personalised Treatment; Coelho, J., Ed.; Springer: Dordrecht, The Netherlands, 2013; Volume 4, pp. 109–125. [Google Scholar]
- Ribeiro, A. Editorial Thematic Issue: Nanotechnology as a Strategy to Improve Treatment of Diabetes. Curr. Pharm. Biotechnol. 2014, 15, 589. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.; Rodriguez-Torres, M.D.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano Based Drug Delivery Systems: Recent Developments and Future Prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef]
- Pinto Reis, C.; Neufeld, R.J.; Ribeiro, A.J.; Veiga, F. Nanoencapsulation II. Biomedical Applications and Current Status of Peptide and Protein Nanoparticulate Delivery Systems. Nanomedicine 2006, 2, 53–65. [Google Scholar] [CrossRef]
- Jaafar, M.H.M.; Hamid, K.A. Chitosan-Coated Alginate Nanoparticles Enhanced Absorption Profile of Insulin via Oral Administration. Curr. Drug Deliv. 2019, 16, 672–686. [Google Scholar] [CrossRef]
- Freitas, A.A.R.; Ribeiro, A.J.; Santos, A.C.; Veiga, F.; Nunes, L.C.C.; Silva, D.A.; Soares-Sobrinho, J.L.; Silva-Filho, E.C. Sterculia Striata Gum as a Potential Oral Delivery System for Protein Drugs. Int. J. Biol. Macromol. 2020, 164, 1683–1692. [Google Scholar] [CrossRef]
- Collado-González, M.; Ferreri, M.C.; Freitas, A.R.; Santos, A.C.; Ferreira, N.R.; Carissimi, G.; Sequeira, J.A.D.; Díaz Baños, F.G.; Villora, G.; Veiga, F.; et al. Complex Polysaccharide-Based Nanocomposites for Oral Insulin Delivery. Mar. Drugs 2020, 18, 55. [Google Scholar] [CrossRef] [PubMed]
- Vodyashkin, A.A.; Kezimana, P.; Vetcher, A.A.; Stanishevskiy, Y.M. Biopolymeric Nanoparticles—Multifunctional Materials of the Future. Polymers 2022, 14, 2287. [Google Scholar] [CrossRef] [PubMed]
- Sarmento, B.; Ribeiro, A.J.; Veiga, F.; Ferreira, D.C.; Neufeld, R.J. Insulin-Loaded Nanoparticles Are Prepared by Alginate Ionotropic Pre-Gelation Followed by Chitosan Polyelectrolyte Complexation. J. Nanosci. Nanotechnol. 2007, 7, 2833–2841. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.; Abrahim, B.; Veiga, F.; Seiça, R.; Cabral, L.M.; Arnaud, P.; Andrade, J.C.; Ribeiro, A.J. Preparation Methods and Applications behind Alginate-Based Particles. Expert. Opin. Drug Deliv. 2017, 14, 769–782. [Google Scholar] [CrossRef] [PubMed]
- Benediktsdóttir, B.E. Chitosan and Trimethyl Chitosan (TMC) as Drug Absorption Enhancers. In Encyclopedia of Marine Biotechnology; Wiley: Hoboken, NJ, USA, 2020; pp. 2773–2795. [Google Scholar]
- Ribeiro, A.; Lopes, M.; Abrahim-Vieira, B.; Fonte, P.; Souza, A.; Lira, T.; Sequeira, J.; Rodrigues, C.; Cabral, L.; Sarmento, B.; et al. Probing Insulin Bioactivity in Oral Nanoparticles Produced by Ultrasonication-Assisted Emulsification/Internal Gelation. Int. J. Nanomed. 2015, 10, 5865. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.; Derenne, A.; Pereira, C.; Veiga, F.; Seiça, R.; Sarmento, B.; Ribeiro, A. Impact of the in Vitro Gastrointestinal Passage of Biopolymer-Based Nanoparticles on Insulin Absorption. RSC Adv. 2016, 6, 20155–20165. [Google Scholar] [CrossRef]
- Lopes, M.; Shrestha, N.; Correia, A.; Shahbazi, M.-A.; Sarmento, B.; Hirvonen, J.; Veiga, F.; Seiça, R.; Ribeiro, A.; Santos, H.A. Dual Chitosan/Albumin-Coated Alginate/Dextran Sulfate Nanoparticles for Enhanced Oral Delivery of Insulin. J. Control Rel. 2016, 232, 29–41. [Google Scholar] [CrossRef]
- Chen, Y.; Mohanraj, V.J.; Parkin, J.E. Chitosan-Dextran Sulfate Nanoparticles for Delivery of an Anti-Angiogenesis Peptide. Int. J. Pept. Res. 2003, 10, 621–629. [Google Scholar] [CrossRef]
- Wiggers, H.A.; Fin, M.T.; Khalil, N.M.; Mainardes, R.M. Polyethylene Glycol-Stabilized Zein Nanoparticles Containing Gallic Acid. Food Technol. Biotechnol. 2022, 60, 145–154. [Google Scholar] [CrossRef]
- Reis, C.P.; Figueiredo, I.V.; Carvalho, R.A.; Jones, J.; Nunes, P.; Soares, A.F.; Silva, C.F.; Ribeiro, A.J.; Veiga, F.J.; Damgé, C.; et al. Toxicological Assessment of Orally Delivered Nanoparticulate Insulin. Nanotoxicology 2008, 2, 205–217. [Google Scholar] [CrossRef]
- Spada, A.; Emami, J.; Tuszynski, J.A.; Lavasanifar, A. The Uniqueness of Albumin as a Carrier in Nanodrug Delivery. Mol. Pharm. 2021, 18, 1862–1894. [Google Scholar] [CrossRef] [PubMed]
- Sreekumar, S.; Goycoolea, F.M.; Moerschbacher, B.M.; Rivera-Rodriguez, G.R. Parameters Influencing the Size of Chitosan-TPP Nano- and Microparticles. Sci. Rep. 2018, 8, 4695. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.R.; Xu, W.; Mráz, J. Formulation and Characterization of Zein/Chitosan Complex Particles Stabilized Pickering Emulsion with the Encapsulation and Delivery of Vitamin D3. J. Sci. Food Agric. 2021, 101, 5419–5428. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Zhang, B.; Whent, M.; Yu, L.L.; Wang, Q. Preparation and Characterization of Zein/Chitosan Complex for Encapsulation of α-Tocopherol, and Its in Vitro Controlled Release Study. Colloids Surf. B Biointerfaces 2011, 85, 145–152. [Google Scholar] [CrossRef]
- Mahmoudi, M. The Need for Robust Characterization of Nanomaterials for Nanomedicine Applications. Nat. Commun. 2021, 12, 5246. [Google Scholar] [CrossRef]
- Raftery, R.M.; Tierney, E.G.; Curtin, C.M.; Cryan, S.A.; O’Brien, F.J. Development of a Gene-Activated Scaffold Platform for Tissue Engineering Applications Using Chitosan-PDNA Nanoparticles on Collagen-Based Scaffolds. J. Control. Rel. 2015, 210, 84–94. [Google Scholar] [CrossRef]
- Morris, G.A.; Castile, J.; Smith, A.; Adams, G.G.; Harding, S.E. Macromolecular Conformation of Chitosan in Dilute Solution: A New Global Hydrodynamic Approach. Carbohydr. Polym. 2009, 76, 616–621. [Google Scholar] [CrossRef]
- Zhou, J.; Ralston, J.; Sedev, R.; Beattie, D.A. Functionalized Gold Nanoparticles: Synthesis, Structure and Colloid Stability. J. Colloid Interface Sci. 2009, 331, 251–262. [Google Scholar] [CrossRef]
- Echeverri-Cuartas, C.E.; Gartner, C.; Lapitsky, Y. PEGylation and Folate Conjugation Effects on the Stability of Chitosan-Tripolyphosphate Nanoparticles. Int. J. Biol. Macromol. 2020, 158, 1055–1065. [Google Scholar] [CrossRef]
- Amin, M.K.; Boateng, J.S. Enhancing Stability and Mucoadhesive Properties of Chitosan Nanoparticles by Surface Modification with Sodium Alginate and Polyethylene Glycol for Potential Oral Mucosa Vaccine Delivery. Mar. Drugs 2022, 20, 156. [Google Scholar] [CrossRef]
- Liu, X.; Meng, H. Consideration for the Scale-up Manufacture of Nanotherapeutics—A Critical Step for Technology Transfer. VIEW 2021, 2, 20200190. [Google Scholar] [CrossRef]
- Ho, H.M.K.; Craig, D.Q.M.; Day, R.M. Design of Experiment Approach to Modeling the Effects of Formulation and Drug Loading on the Structure and Properties of Therapeutic Nanogels. Mol. Pharm. 2022, 19, 602–615. [Google Scholar] [CrossRef] [PubMed]
- Tavares Luiz, M.; Santos Rosa Viegas, J.; Palma Abriata, J.; Viegas, F.; Testa Moura de Carvalho Vicentini, F.; Lopes Badra Bentley, M.V.; Chorilli, M.; Maldonado Marchetti, J.; Tapia-Blácido, D.R. Design of Experiments (DoE) to Develop and to Optimize Nanoparticles as Drug Delivery Systems. Eur. J. Pharm. Biopharm. 2021, 165, 127–148. [Google Scholar] [CrossRef] [PubMed]
- Sah, A.K.; Suresh, P.K. Loteprednol Etabonate Nanoparticles: Optimization via Box-Behnken Design Response Surface Methodology and Physicochemical Characterization. Curr. Drug Deliv. 2017, 14, 676–689. [Google Scholar] [CrossRef] [PubMed]
- Beg, S.; Akhter, S. Box–Behnken Designs and Their Applications in Pharmaceutical Product Development. In Design of Experiments for Pharmaceutical Product Development; Springer: Singapore, 2021; pp. 77–85. [Google Scholar]
- Woitiski, C.B.; Veiga, F.; Ribeiro, A.; Neufeld, R. Design for Optimization of Nanoparticles Integrating Biomaterials for Orally Dosed Insulin. Eur. J. Pharm. Biopharm. 2009, 73, 25–33. [Google Scholar] [CrossRef] [PubMed]
- De Marchi, J.G.B.; Cé, R.; Onzi, G.; Alves, A.C.S.; Santarém, N.; Cordeiro da Silva, A.; Pohlmann, A.R.; Guterres, S.S.; Ribeiro, A.J. IgG Functionalized Polymeric Nanoparticles for Oral Insulin Administration. Int. J. Pharm. 2022, 622, 121829. [Google Scholar] [CrossRef]
- Wong, C.Y.; Luna, G.; Martinez, J.; Al-Salami, H.; Dass, C.R. Bio-Nanotechnological Advancement of Orally Administered Insulin Nanoparticles: Comprehensive Review of Experimental Design for Physicochemical Characterization. Int. J. Pharm. 2019, 572, 118720. [Google Scholar] [CrossRef]
- Thu, B.; Bruheim, P.; Espevik, T.; Smidsrød, O.; Soon-Shiong, P.; Skjåk-Bræk, G. Alginate Polycation Microcapsules. Biomaterials 1996, 17, 1031–1040. [Google Scholar] [CrossRef]
- Reis, C.P.; Veiga, F.J.; Ribeiro, A.J.; Neufeld, R.J.; Damgé, C. Nanoparticulate Biopolymers Deliver Insulin Orally Eliciting Pharmacological Response. J. Pharm. Sci. 2008, 97, 5290–5305. [Google Scholar] [CrossRef]
- Woitiski, C.B.; Neufeld, R.J.; Ribeiro, A.J.; Veiga, F. Colloidal Carrier Integrating Biomaterials for Oral Insulin Delivery: Influence of Component Formulation on Physicochemical and Biological Parameters. Acta Biomater. 2009, 5, 2475–2484. [Google Scholar] [CrossRef]
- Sarmento, B.; Ribeiro, A.; Veiga, F.; Ferreira, D.; Neufeld, R. Oral Bioavailability of Insulin Contained in Polysaccharide Nanoparticles. Biomacromolecules 2007, 8, 3054–3060. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Huang, J.; Chen, T.; Wang, X.; Zhang, H.; Chen, Q. Insight into the Interaction between Chitosan and Bovine Serum Albumin. Carbohydr. Polym. 2017, 176, 75–82. [Google Scholar] [CrossRef]
- Milião, G.L.; de Souza Soares, L.; Balbino, D.F.; Barbosa, É.D.; Bressan, G.C.; de Carvalho Teixeira, A.V.; dos Reis Coimbra, J.S.; de Oliveira, E.B. PH Influence on the Mechanisms of Interaction between Chitosan and Ovalbumin: A Multi-Spectroscopic Approach. Food Hydrocoll. 2022, 123, 107137. [Google Scholar] [CrossRef]
- Benita, S.; Levy, M.Y. Submicron Emulsions as Colloidal Drug Carriers for Intravenous Administration: Comprehensive Physicochemical Characterization. J. Pharm. Sci. 1993, 82, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Honary, S.; Zahir, F. Effect of Zeta Potential on the Properties of Nano-Drug Delivery Systems—A Review (Part 1). Trop. J. Pharm. Res. 2013, 12, 255–264. [Google Scholar] [CrossRef]
- Phan, H.T.; Haes, A.J. What Does Nanoparticle Stability Mean? J. Phys. Chem. C 2019, 123, 16495–16507. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, P.; Chakraborty, S.; Bhattacharya, S.; Mishra, R.; Kundu, P.P. PH-Sensitive Chitosan/Alginate Core-Shell Nanoparticles for Efficient and Safe Oral Insulin Delivery. Int. J. Biol. Macromol. 2015, 72, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Jiang, G.; Yu, W.; Liu, D.; Chen, H.; Liu, Y.; Tong, Z.; Kong, X.; Yao, J. Preparation of Chitosan-Based Multifunctional Nanocarriers Overcoming Multiple Barriers for Oral Delivery of Insulin. Mater. Sci. Eng. C 2017, 70, 278–286. [Google Scholar] [CrossRef]
- Wallace, B.A. Protein Characterisation by Synchrotron Radiation Circular Dichroism Spectroscopy. Q. Rev. Biophys. 2009, 42, 317–370. [Google Scholar] [CrossRef]
- Lassenberger, A.; Bixner, O.; Gruenewald, T.; Lichtenegger, H.; Zirbs, R.; Reimhult, E. Evaluation of High-Yield Purification Methods on Monodisperse PEG-Grafted Iron Oxide Nanoparticles. Langmuir 2016, 32, 4259–4269. [Google Scholar] [CrossRef]
- Kolhe, P.; Kannan, R.M. Improvement in Ductility of Chitosan through Blending and Copolymerization with PEG: FTIR Investigation of Molecular Interactions. Biomacromolecules 2003, 4, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Kataria, D.; Zafar, A.; Ali, J.; Khatoon, K.; Khan, S.; Imam, S.S.; Yasir, M.; Ali, A. Formulation of Lipid-Based Nanocarriers of Lacidipine for Improvement of Oral Delivery: Box-Behnken Design Optimization, In Vitro, Ex Vivo, and Preclinical Assessment. Assay. Drug Dev. Technol. 2022, 20, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Rajaonarivony, M.; Vauthier, C.; Couarraze, G.; Puisieux, F.; Couvreur, P. Development of a New Drug Carrier Made from Alginate. J. Pharm. Sci. 1993, 82, 912–917. [Google Scholar] [CrossRef] [PubMed]
- The United States Pharmacopeia 36 (USP- 36). National Formulary 31 (NF-31); United States Pharmacopeial Convention: Rockville, MD, USA, 1998. [Google Scholar]
- Motwani, S.K.; Chopra, S.; Talegaonkar, S.; Kohli, K.; Ahmad, F.J.; Khar, R.K. Chitosan-Sodium Alginate Nanoparticles as Submicroscopic Reservoirs for Ocular Delivery: Formulation, Optimisation and in Vitro Characterisation. Eur. J. Pharm. Biopharm. 2008, 68, 513–525. [Google Scholar] [CrossRef]
- Myers, R.H.; Montgomery, D.C.; Anderson-Cook, C.M. Multiple Response Optimization. In Response Surface Methodology: Process and Product Optimization Using Designed Experiments; Wiley: Hoboken, NJ, USA, 2016; pp. 325–357. ISBN 9781118916032. [Google Scholar]



| Formulation | Independent Variables | Dependent Variables | ||||||
|---|---|---|---|---|---|---|---|---|
| X1 (%) | X2 (%) | X3 (%) | Y1 (nm) mean ± SD | Y2 mean ± SD | Y3 mV ± SD | Y4 % ± SD | Y5 %± SD | |
| 1 | 0.01 | 0.025 | 1.0 | 547 ± 21 | 0.36 ± 0.04 | −43.0 ± 1.3 | 16 ± 2 | 74 ± 2 |
| 2 | 0.03 | 0.025 | 1.0 | 559 ± 23 | 0.32 ± 0.02 | −41.0 ± 1.5 | 19 ± 3 | 70 ± 3 |
| 3 | 0.01 | 0.075 | 1.0 | 313 ± 13 | 0.23 ± 0.02 | −31.0 ± 0.7 | 0 | 50 ± 4 |
| 4 | 0.03 | 0.075 | 1.0 | 317 ± 15 | 0.20 ± 0.03 | −30.0 ± 0.8 | 0 | 52 ± 6 |
| 5 | 0.01 | 0.050 | 0.5 | 378 ± 20 | 0.22 ± 0.04 | −34.0 ± 1.5 | 37 ± 3 | 78 ± 3 |
| 6 | 0.03 | 0.050 | 0.5 | 362 ± 17 | 0.27 ± 0.04 | −31.0 ± 1.3 | 35 ± 4 | 76 ± 3 |
| 7 | 0.01 | 0.050 | 1.0 | 339 ± 14 | 0.22 ± 0.03 | −36.0 ± 0.7 | 6 ± 4 | 76 ± 5 |
| 8 | 0.03 | 0.050 | 1.5 | 376 ± 13 | 0.17 ± 0.01 | −34.0 ± 0.8 | 0 | 76 ± 3 |
| 9 | 0.02 | 0.025 | 0.5 | 585 ± 13 | 0.27 ± 0.03 | −44.0 ± 1.8 | 60 ± 5 | 76 ± 4 |
| 10 | 0.02 | 0.075 | 0.5 | 342 ± 15 | 0.27 ± 0.02 | −32.0 ± 0.8 | 32 ± 4 | 60 ± 3 |
| 11 | 0.02 | 0.025 | 1.5 | 563 ± 24 | 0.39 ± 0.05 | −40.0 ± 1.2 | 12 ± 3 | 72 ± 4 |
| 12 | 0.02 | 0.075 | 1.5 | 314 ± 14 | 0.18 ± 0.02 | −29.0 ± 0.7 | 0 | 46 ± 6 |
| 13 * | 0.02 | 0.050 | 1.0 | 320 ± 26 | 0.19 ± 0.02 | −34.0 ± 2.2 | 6 ± 2 | 78 ± 3 |
| 14 * | 0.02 | 0.050 | 1.0 | 345 ± 14 | 0.18 ± 0.03 | −33.0 ± 2.1 | 5 ± 3 | 76 ± 4 |
| 15 * | 0.02 | 0.050 | 1.0 | 347 ± 13 | 0.19 ± 0.01 | −33.0 ± 1.1 | 4 ± 2 | 78 ± 4 |
| Terms | Y1 | Y2 | Y3 | Y4 | Y5 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C | SE | Range * | C | SE | Range * | C | SE | Range * | C | SE | Range * | C | SE | Range * | |
| b0 | 341.19 | 5.01 | 330.04 to 332.35 | 0.185 | 0.006 | 0.170 to 0.200 | −35 | 0.53 | −36 to −34 | 4.14 | 0.93 | 2.02 to 6.25 | 76.46 | 1.01 | 74.23 to 78.69 |
| b1 | - | - | - | −0.02 | 0.004 | −0.03 to −0.01 | - | - | - | - | - | - | - | - | |
| b2 | −121.00 | 4.03 | −129.97 to −112.03 | −0.06 | 0.004 | −0.07 to −0.05 | 5.75 | 0.73 | 4.17 to 7.33 | −9.38 | 0.76 | −11.07 to −7.68 | −19.50 | 0.94 | −12.56 to −8.44 |
| b3 | - | - | - | - | - | - | - | - | −18.98 | 0.82 | −20.82 to −17.13 | - | - | ||
| b1b2 | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| b1b3 | - | - | - | −0.05 | 0.007 | −0.07 to−0.03 | - | - | - | - | - | - | - | - | |
| b2b3 | - | - | - | −0.05 | 0.005 | −007 to −0.04 | - | - | - | 4.00 | 1.06 | 1.60 to 6.40 | - | - | |
| b12 | - | - | - | 0.03 | 0.006 | 0.01 to 0.04 | - | - | - | - | - | - | - | ||
| b22 | 89.36 | 5.95 | 76.11 to 102.61 | 0.07 | 0.006 | 0.05 to −0.08 | - | - | - | 5.73 | 1.11 | 3.22 to 8.24 | −13.96 | 1.38 | −17.00 to −10.92 |
| b32 | 23.88 | 5.95 | −10.64 to 37.14 | 0.03 | 0.006 | 0.01 to 0.05 | - | - | - | 15.02 | 1.11 | 12.51 to 17.53 | - | - | |
| Dependent Variable | Predicted Response | Experimental Response | Predicted (%) |
|---|---|---|---|
| Particle size (nm) | 357 | 366 | +2.5 |
| Polydispersity index (PDI) | 0.193 | 0.202 | +4.4 |
| Zeta potential (mV) | −35 | −34 | +2.9 |
| Insulin escape in gastric medium (%) | 0 | 0 | 0 |
| Intestinal release in intestinal medium (%) | 76 | 73 | −5.0 |
| Parameter | Levels | ||
|---|---|---|---|
| Independent variables | −1 | 0 | 1 |
| Polyethylene glycol (PEG) % (w/v) | 0.01 | 0.02 | 0.03 |
| Chitosan % (w/v) | 0.025 | 0.050 | 0.075 |
| BSA %(w/v) | 0.5 | 1.0 | 1.5 |
| Dependent variables | Constraint | ||
| Particle size (nm) | Minimize | ||
| Polydispersity index (PDI) | Minimize | ||
| Zeta potential (mV) | Less than −30 mv | ||
| Insulin escape in gastric medium (%) | Minimize | ||
| Intestinal release in intestinal medium (%) | Maximize | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pessoa, B.; Collado-Gonzalez, M.; Sandri, G.; Ribeiro, A. Chitosan/Albumin Coating Factorial Optimization of Alginate/Dextran Sulfate Cores for Oral Delivery of Insulin. Mar. Drugs 2023, 21, 179. https://doi.org/10.3390/md21030179
Pessoa B, Collado-Gonzalez M, Sandri G, Ribeiro A. Chitosan/Albumin Coating Factorial Optimization of Alginate/Dextran Sulfate Cores for Oral Delivery of Insulin. Marine Drugs. 2023; 21(3):179. https://doi.org/10.3390/md21030179
Chicago/Turabian StylePessoa, Bruno, Mar Collado-Gonzalez, Giuseppina Sandri, and António Ribeiro. 2023. "Chitosan/Albumin Coating Factorial Optimization of Alginate/Dextran Sulfate Cores for Oral Delivery of Insulin" Marine Drugs 21, no. 3: 179. https://doi.org/10.3390/md21030179
APA StylePessoa, B., Collado-Gonzalez, M., Sandri, G., & Ribeiro, A. (2023). Chitosan/Albumin Coating Factorial Optimization of Alginate/Dextran Sulfate Cores for Oral Delivery of Insulin. Marine Drugs, 21(3), 179. https://doi.org/10.3390/md21030179










