2D Collagen Membranes from Marine Demosponge Chondrosia reniformis (Nardo, 1847) for Skin-Regenerative Medicine Applications: An In Vitro Evaluation
Abstract
:1. Introduction
2. Results
2.1. Chondrosia reniformis Fibrillar Extract Extraction and Purification
2.2. 2D Collagen Membrane Permeability Tests
2.2.1. Water Permeability Test
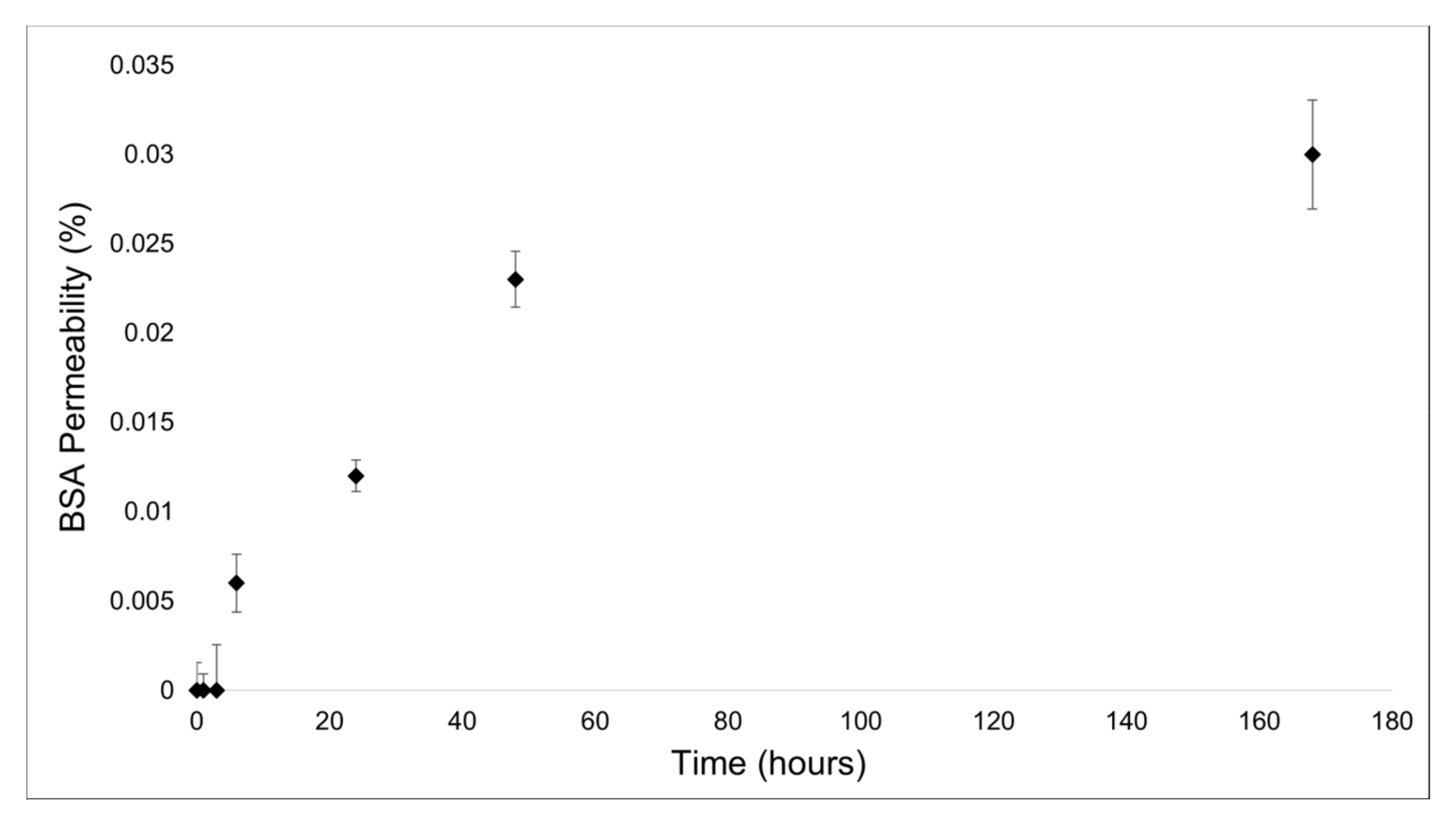
2.2.2. Protein Permeability Test
2.3. Bacteria Infiltration Tests
2.4. Bacteriostaticity Test
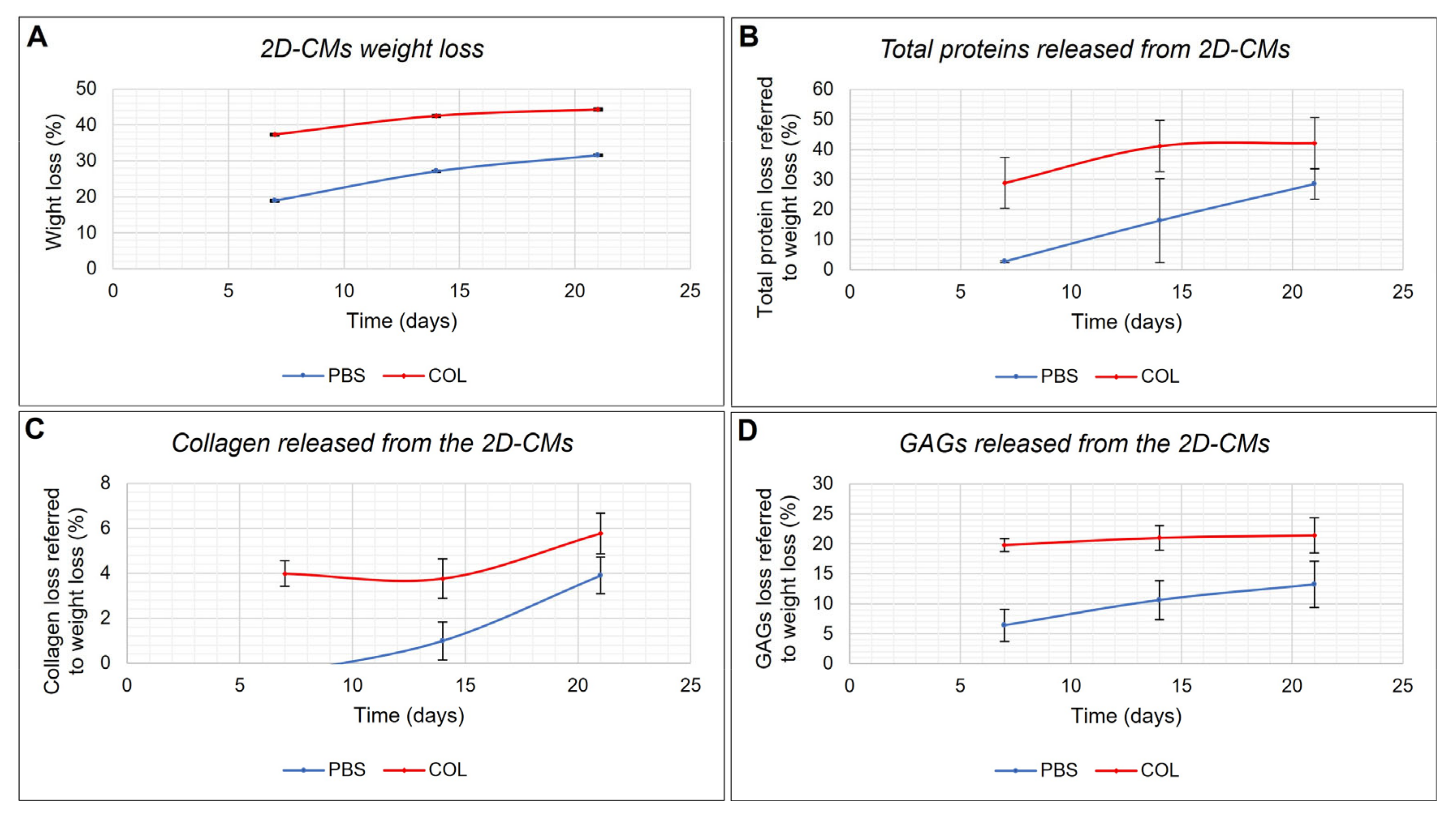
2.5. In Vitro Biodegradability Test
2.6. Effect of the 2D Collagen Membranes on Fibroblasts
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Sponge Sampling
4.3. Chondrosia reniformis Fibrillar Collagen Extraction and Purification
4.4. Production of 2D Collagen Membranes
4.5. 2D Collagen Membranes Permeability Tests
4.5.1. Water Permeability Test
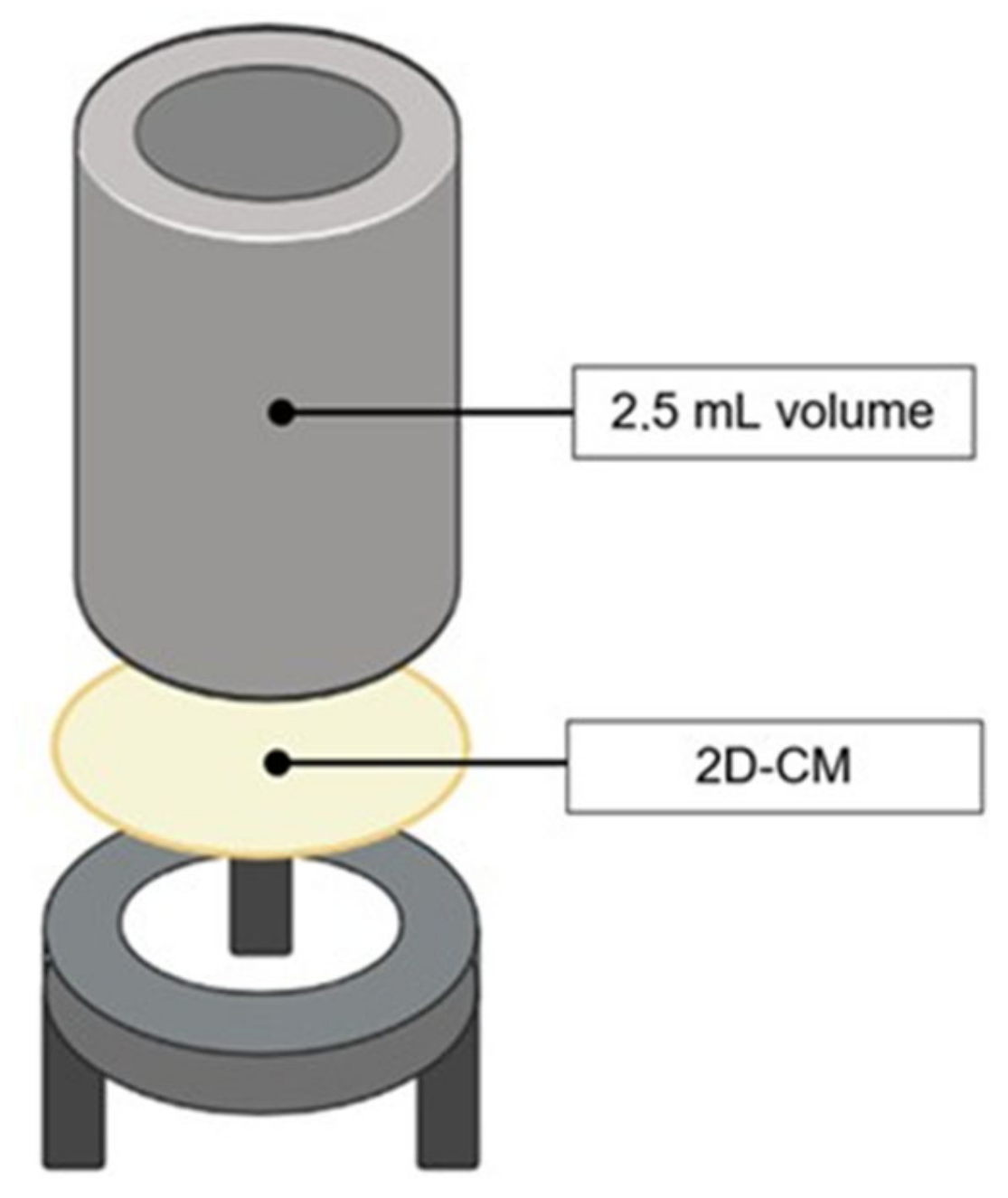
4.5.2. Protein Permeability Test
4.6. Bacteria Infiltration Tests
4.7. Bacteriostaticity Test
4.8. In Vitro Biodegradability Test
Evaluation of the Material Released into the Incubation Media
4.9. Effect of 2D Collagen Membranes on Fibroblasts
4.9.1. Cell Cultures
4.9.2. Fibroblast Gene Expression Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human Skin Wounds: A Major and Snowballing Threat to Public Health and the Economy. Wound Repair Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [Green Version]
- Oualla-Bachiri, W.; Fernández-González, A.; Quiñones-Vico, M.I.; Arias-Santiago, S. From Grafts to Human Bioengineered Vascularized Skin Substitutes. Int. J. Mol. Sci. 2020, 21, 8197. [Google Scholar] [CrossRef]
- Huang, H.; Dong, Z.; Ren, X.; Jia, B.; Li, G.; Zhou, S.; Zhao, X.; Wang, W. High-Strength Hydrogels: Fabrication, Reinforcement Mechanisms, and Applications. Nano Res. 2023, 16, 3475–3515. [Google Scholar] [CrossRef]
- Shores, J.T.; Gabriel, A.; Gupta, S. Skin Substitutes and Alternatives: A Review. Adv. Ski. Wound Care 2007, 20, 493. [Google Scholar] [CrossRef]
- Hernández-Rangel, A.; Martin-Martinez, E.S. Collagen Based Electrospun Materials for Skin Wounds Treatment. J. Biomed. Mater. Res. A 2021, 109, 1751–1764. [Google Scholar] [CrossRef]
- Davison-Kotler, E.; Marshall, W.S.; García-Gareta, E. Sources of Collagen for Biomaterials in Skin Wound Healing. Bioengineering 2019, 6, 56. [Google Scholar] [CrossRef] [Green Version]
- De Melo Oliveira, V.; Assis, C.R.D.; de Aquino Marques Costa, B.; de Araújo Neri, R.C.; Monte, F.T.D.; da Costa Vasconcelos Freitas, H.M.S.; França, R.C.P.; Santos, J.F.; de Souza Bezerra, R.; Porto, A.L.F. Physical, Biochemical, Densitometric and Spectroscopic Techniques for Characterization Collagen from Alternative Sources: A Review Based on the Sustainable Valorization of Aquatic by-Products. J. Mol. Struct. 2021, 1224, 129023. [Google Scholar] [CrossRef]
- Liu, S.; Lau, C.-S.; Liang, K.; Wen, F.; Teoh, S.H. Marine Collagen Scaffolds in Tissue Engineering. Curr. Opin. Biotechnol. 2022, 74, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Coppola, D.; Oliviero, M.; Vitale, G.A.; Lauritano, C.; D’Ambra, I.; Iannace, S.; de Pascale, D. Marine Collagen from Alternative and Sustainable Sources: Extraction, Processing and Applications. Mar. Drugs 2020, 18, 214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, M.K.; Mir, S.H.; Parvez, R. Marine Collagen: Promising Biomaterial in Delivery of Therapeutics for Cancer Therapy. In Marine Biomaterials: Drug Delivery and Therapeutic Applications; Jana, S., Jana, S., Eds.; Springer Nature: Singapore, 2022; pp. 251–279. ISBN 9789811647871. [Google Scholar]
- Lin, Z.; Tao, Y.; Huang, Y.; Xu, T.; Niu, W. Applications of Marine Collagens in Bone Tissue Engineering. Biomed. Mater. 2021, 16, 042007. [Google Scholar] [CrossRef]
- Lin, Z.; Solomon, K.L.; Zhang, X.; Pavlos, N.J.; Abel, T.; Willers, C.; Dai, K.; Xu, J.; Zheng, Q.; Zheng, M. In Vitro Evaluation of Natural Marine Sponge Collagen as a Scaffold for Bone Tissue Engineering. Int. J. Biol. Sci. 2011, 7, 968–977. [Google Scholar] [CrossRef] [Green Version]
- Pallela, R.; Venkatesan, J.; Janapala, V.R.; Kim, S.-K. Biophysicochemical Evaluation of Chitosan-Hydroxyapatite-Marine Sponge Collagen Composite for Bone Tissue Engineering. J. Biomed. Mater. Res. Part A 2012, 100A, 486–495. [Google Scholar] [CrossRef]
- Granito, R.N.; Custódio, M.R.; Rennó, A.C.M. Natural Marine Sponges for Bone Tissue Engineering: The State of Art and Future Perspectives. J. Biomed. Mater. Res. Part B Appl. Biomater. 2017, 105, 1717–1727. [Google Scholar] [CrossRef] [PubMed]
- Martins, E.; Rocha, M.S.; Silva, T.H.; Reis, R.L. Remarkable Body Architecture of Marine Sponges as Biomimetic Structure for Application in Tissue Engineering. In Marine-Derived Biomaterials for Tissue Engineering Applications; Choi, A.H., Ben-Nissan, B., Eds.; Springer Series in Biomaterials Science and Engineering; Springer: Singapore, 2019; pp. 27–50. ISBN 9789811388552. [Google Scholar]
- Cruz, M.A.; Fernandes, K.R.; Parisi, J.R.; Vale, G.C.A.; Junior, S.R.A.; Freitas, F.R.; Sales, A.F.S.; Fortulan, C.A.; Peitl, O.; Zanotto, E.; et al. Marine Collagen Scaffolds and Photobiomodulation on Bone Healing Process in a Model of Calvaria Defects. J. Bone Min. Metab. 2020, 38, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Pozzolini, M.; Tassara, E.; Dodero, A.; Castellano, M.; Vicini, S.; Ferrando, S.; Aicardi, S.; Cavallo, D.; Bertolino, M.; Petrenko, I.; et al. Potential Biomedical Applications of Collagen Filaments Derived from the Marine Demosponges Ircinia oros (Schmidt, 1864) and Sarcotragus foetidus (Schmidt, 1862). Mar. Drugs 2021, 19, 563. [Google Scholar] [CrossRef] [PubMed]
- Van Soest, R.W.M.V.; Boury-Esnault, N.; Vacelet, J.; Dohrmann, M.; Erpenbeck, D.; Voogd, N.J.D.; Santodomingo, N.; Vanhoorne, B.; Kelly, M.; Hooper, J.N.A. Global Diversity of Sponges (Porifera). PLoS ONE 2012, 7, e35105. [Google Scholar] [CrossRef] [PubMed]
- Van Soest, R.; Boury-Esnault, N.; Hooper, J.; Rützler, K.; de Voogd, N.; Alvarez, B.; Hajdu, E.; Pisera, A.; Manconi, R.; Schönberg, C.; et al. World Porifera Database. Available online: marinespecies.org (accessed on 5 June 2023).
- Bonasoro, F.; Wilkie, I.C.; Bavestrello, G.; Cerrano, C.; Carnevali, M.D.C. Dynamic Structure of the Mesohyl in the Sponge Chondrosia reniformis (Porifera, Demospongiae). Zoomorphology 2001, 121, 109–121. [Google Scholar] [CrossRef]
- Orel, B.; Giovine, M.; Ilan, M. On the Path to Thermo-Stable Collagen: Culturing the Versatile Sponge Chondrosia reniformis. Mar. Drugs 2021, 19, 669. [Google Scholar] [CrossRef]
- Pozzolini, M.; Gallus, L.; Ghignone, S.; Ferrando, S.; Candiani, S.; Bozzo, M.; Bertolino, M.; Costa, G.; Bavestrello, G.; Scarfì, S. Insights into the Evolution of Metazoan Regenerative Mechanisms: Roles of TGF Superfamily Members in Tissue Regeneration of the Marine Sponge Chondrosia reniformis. J. Exp. Biol. 2019, 222, jeb207894. [Google Scholar] [CrossRef] [Green Version]
- Pozzolini, M.; Scarfì, S.; Gallus, L.; Ferrando, S.; Cerrano, C.; Giovine, M. Silica-Induced Fibrosis: An Ancient Response from the Early Metazoans. J. Exp. Biol. 2017, 220, 4007–4015. [Google Scholar] [CrossRef] [Green Version]
- Pozzolini, M.; Scarfì, S.; Gallus, L.; Castellano, M.; Vicini, S.; Cortese, K.; Gagliani, M.C.; Bertolino, M.; Costa, G.; Giovine, M. Production, Characterization and Biocompatibility Evaluation of Collagen Membranes Derived from Marine Sponge Chondrosia reniformis Nardo, 1847. Mar. Drugs 2018, 16, 111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrone, R.; Huc, A.; Junqua, S. Fine Structure and Physicochemical Studies on the Collagen of the Marine Sponge Chondrosia reniformis Nardo. J. Ultrastruct. Res. 1975, 52, 261–275. [Google Scholar] [CrossRef] [PubMed]
- Imhoff, J.M.; Garrone, R. Solubilization and Characterization of Chondrosia reniformis Sponge Collagen. Connect. Tissue Res. 1983, 11, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Tassara, E.; Orel, B.; Ilan, M.; Cavallo, D.; Dodero, A.; Castellano, M.; Vicini, S.; Giovine, M.; Pozzolini, M. Seasonal Molecular Difference in Fibrillar Collagen Extracts Derived from the Marine Sponge Chondrosia reniformis (Nardo, 1847) and Their Impact on Its Derived Biomaterials. Mar. Drugs 2023, 21, 210. [Google Scholar] [CrossRef]
- Berillis, P. Marine collagen: Extraction and applications. In Research Trends in Biochemistry, Molecular Biology, and Microbiology; SM Group: Dover, DE, USA, 2015; pp. 1–13. [Google Scholar]
- Pozzolini, M.; Millo, E.; Oliveri, C.; Mirata, S.; Salis, A.; Damonte, G.; Arkel, M.; Scarfì, S. Elicited ROS Scavenging Activity, Photoprotective, and Wound-Healing Properties of Collagen-Derived Peptides from the Marine Sponge Chondrosia reniformis. Mar. Drugs 2018, 16, 465. [Google Scholar] [CrossRef] [Green Version]
- Fassini, D.; Duarte, A.R.C.; Reis, R.L.; Silva, T.H. Bioinspiring Chondrosia reniformis (Nardo, 1847) Collagen-Based Hydrogel: A New Extraction Method to Obtain a Sticky and Self-Healing Collagenous Material. Mar. Drugs 2017, 15, 380. [Google Scholar] [CrossRef] [Green Version]
- Swatschek, D.; Schatton, W.; Kellermann, J.; Müller, W.E.G.; Kreuter, J. Marine Sponge Collagen: Isolation, Characterization and Effects on the Skin Parameters Surface-PH, Moisture and Sebum. Eur. J. Pharm. Biopharm. 2002, 53, 107–113. [Google Scholar] [CrossRef]
- Ferrario, C.; Rusconi, F.; Pulaj, A.; Macchi, R.; Landini, P.; Paroni, M.; Colombo, G.; Martinello, T.; Melotti, L.; Gomiero, C.; et al. From Food Waste to Innovative Biomaterial: Sea Urchin-Derived Collagen for Applications in Skin Regenerative Medicine. Mar. Drugs 2020, 18, 414. [Google Scholar] [CrossRef]
- Bereket, W.; Hemalatha, K.; Getenet, B.; Wondwossen, T.; Solomon, A.; Zeynudin, A.; Kannan, S. Update on Bacterial Nosocomial Infections. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1039–1044. [Google Scholar]
- Darby, I.A.; Hewitson, T.D. Fibroblast Differentiation in Wound Healing and Fibrosis. In International Review of Cytology; Academic Press: Cambridge, MA, USA, 2007; Volume 257, pp. 143–179. [Google Scholar]
- Eckes, B.; Zigrino, P.; Kessler, D.; Holtkötter, O.; Shephard, P.; Mauch, C.; Krieg, T. Fibroblast-Matrix Interactions in Wound Healing and Fibrosis. Matrix Biol. 2000, 19, 325–332. [Google Scholar] [CrossRef]
- Sugni, M.; Fassini, D.; Barbaglio, A.; Biressi, A.; Di Benedetto, C.; Tricarico, S.; Bonasoro, F.; Wilkie, I.C.; Candia Carnevali, M.D. Comparing Dynamic Connective Tissue in Echinoderms and Sponges: Morphological and Mechanical Aspects and Environmental Sensitivity. Mar. Environ. Res. 2014, 93, 123–132. [Google Scholar] [CrossRef]
- Fassini, D.; Wilkie, I.C.; Pozzolini, M.; Ferrario, C.; Sugni, M.; Rocha, M.S.; Giovine, M.; Bonasoro, F.; Silva, T.H.; Reis, R.L. Diverse and Productive Source of Biopolymer Inspiration: Marine Collagens. Biomacromolecules 2021, 22, 1815–1834. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.C.; Barros, A.A.; Aroso, I.M.; Fassini, D.; Silva, T.H.; Reis, R.L.; Duarte, A.R.C. Extraction of Collagen/Gelatin from the Marine Demosponge Chondrosia reniformis (Nardo, 1847) Using Water Acidified with Carbon Dioxide—Process Optimization. Ind. Eng. Chem. Res. 2016, 55, 6922–6930. [Google Scholar] [CrossRef]
- Gilbert, D.L.; Okano, T.; Miyata, T. Sung Wan Kim Macromolecular Diffusion through Collagen Membranes. Int. J. Pharm. 1988, 47, 79–88. [Google Scholar] [CrossRef]
- Xu, R.; Xia, H.; He, W.; Li, Z.; Zhao, J.; Liu, B.; Wang, Y.; Lei, Q.; Kong, Y.; Bai, Y.; et al. Controlled Water Vapor Transmission Rate Promotes Wound-Healing via Wound Re-Epithelialization and Contraction Enhancement. Sci. Rep. 2016, 6, 24596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hentschel, U.; Piel, J.; Degnan, S.M.; Taylor, M.W. Genomic Insights into the Marine Sponge Microbiome. Nat. Rev. Microbiol. 2012, 10, 641–654. [Google Scholar] [CrossRef]
- Esposito, R.; Federico, S.; Glaviano, F.; Somma, E.; Zupo, V.; Costantini, M. Bioactive Compounds from Marine Sponges and Algae: Effects on Cancer Cell Metabolome and Chemical Structures. Int. J. Mol. Sci. 2022, 23, 10680. [Google Scholar] [CrossRef]
- Scarfì, S.; Pozzolini, M.; Oliveri, C.; Mirata, S.; Salis, A.; Damonte, G.; Fenoglio, D.; Altosole, T.; Ilan, M.; Bertolino, M.; et al. Identification, Purification and Molecular Characterization of Chondrosin, a New Protein with Anti-Tumoral Activity from the Marine Sponge Chondrosia reniformis Nardo 1847. Mar. Drugs 2020, 18, 409. [Google Scholar] [CrossRef]
- Sheikholeslam, M.; Wright, M.E.E.; Jeschke, M.G.; Amini-Nik, S. Biomaterials for Skin Substitutes. Adv. Healthc. Mater. 2018, 7, 1700897. [Google Scholar] [CrossRef]
- Eming, S.A.; Martin, P.; Tomic-Canic, M. Wound Repair and Regeneration: Mechanisms, Signaling, and Translation. Sci. Transl. Med. 2014, 6, 265sr6. [Google Scholar] [CrossRef] [Green Version]
- Pilcher, B.K.; Wang, M.; Qin, X.-J.; Parks, W.C.; Senior, R.M.; Welgus, H.G. Role of Matrix Metalloproteinases and Their Inhibition in Cutaneous Wound Healing and Allergic Contact Hypersensitivity. Ann. N. Y. Acad. Sci. 1999, 878, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Rousselle, P.; Montmasson, M.; Garnier, C. Extracellular Matrix Contribution to Skin Wound Re-Epithelialization. Matrix Biol. 2019, 75–76, 12–26. [Google Scholar] [CrossRef] [PubMed]
- Cutroneo, K.R. TGF-β–Induced Fibrosis and SMAD Signaling: Oligo Decoys as Natural Therapeutics for Inhibition of Tissue Fibrosis and Scarring. Wound Repair Regen. 2007, 15, S54–S60. [Google Scholar] [CrossRef] [PubMed]
- Schwarzbauer, J.E. Fibronectin: From Gene to Protein. Curr. Opin. Cell Biol. 1991, 3, 786–791. [Google Scholar] [CrossRef]
- Heino, J.; Kapyla, J. Cellular Receptors of Extracellular Matrix Molecules. Curr. Pharm. Des. 2009, 15, 1309–1317. [Google Scholar] [CrossRef]
- Pozzolini, M.; Bruzzone, F.; Berilli, V.; Mussino, F.; Cerrano, C.; Benatti, U.; Giovine, M. Molecular Characterization of a Nonfibrillar Collagen from the Marine Sponge Chondrosia reniformis Nardo 1847 and Positive Effects of Soluble Silicates on Its Expression. Mar. Biotechnol. 2012, 14, 281–293. [Google Scholar] [CrossRef]
- Yuan, J.; Liu, M.; Yang, L.; Tu, G.; Zhu, Q.; Chen, M.; Cheng, H.; Luo, H.; Fu, W.; Li, Z.; et al. Acquisition of Epithelial-Mesenchymal Transition Phenotype in the Tamoxifen-Resistant Breast Cancer Cell: A New Role for G Protein-Coupled Estrogen Receptor in Mediating Tamoxifen Resistance through Cancer-Associated Fibroblast-Derived Fibronectin and Β1-Integrin Signaling Pathway in Tumor Cells. Breast Cancer Res. 2015, 17, 69. [Google Scholar] [CrossRef]
- Marconi, G.D.; Fonticoli, L.; Rajan, T.S.; Pierdomenico, S.D.; Trubiani, O.; Pizzicannella, J.; Diomede, F. Epithelial-Mesenchymal Transition (EMT): The Type-2 EMT in Wound Healing, Tissue Regeneration and Organ Fibrosis. Cells 2021, 10, 1587. [Google Scholar] [CrossRef]
- Lenselink, E.A. Role of Fibronectin in Normal Wound Healing. Int. Wound J. 2015, 12, 313–316. [Google Scholar] [CrossRef]
- Mercado, A.M.; Padgett, D.A.; Sheridan, J.F.; Marucha, P.T. Altered Kinetics of IL-1 Alpha, IL-1 Beta, and KGF-1 Gene Expression in Early Wounds of Restrained Mice. Brain Behav. Immun. 2002, 16, 150–162. [Google Scholar] [CrossRef] [Green Version]
- Gross, J.; Sokal, Z.; Rougvie, M. Structural and Chemical Studies on the Connective Tissue of Marine Sponges. J. Histochem. Cytochem. 1956, 4, 227–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Chang, Y.; Wu, F.; Xu, X.; Xue, C. Fucosylated Chondroitin Sulfate Is Covalently Associated with Collagen Fibrils in Sea Cucumber Apostichopus japonicus Body Wall. Carbohydr. Polym. 2018, 186, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Bradford, M.M. A Rapid and Sensitive Method for the Quantitation of Microgram Quantities of Protein Utilizing the Principle of Protein-Dye Binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.K.; Krohn, R.I.; Hermanson, G.T.; Mallia, A.K.; Gartner, F.H.; Provenzano, M.D.; Fujimoto, E.K.; Goeke, N.M.; Olson, B.J.; Klenk, D.C. Measurement of Protein Using Bicinchoninic Acid. Anal. Biochem. 1985, 150, 76–85. [Google Scholar] [CrossRef]
- Kesava Reddy, G.; Enwemeka, C.S. A Simplified Method for the Analysis of Hydroxyproline in Biological Tissues. Clin. Biochem. 1996, 29, 225–229. [Google Scholar] [CrossRef]
- Bjornsson, S. Simultaneous Preparation and Quantitation of Proteoglycans by Precipitation with Alcian Blue. Anal. Biochem. 1993, 210, 282–291. [Google Scholar] [CrossRef]

| Time Point | “Dry-Wet” Condition | “Wet-Wet” Condition |
|---|---|---|
| 0 h | 0 | 0 |
| 1 h | 0 | 0 |
| 3 h | 0 | 0 |
| 6 h | 0 | 0 |
| 24 h | 0 | 0.1 ± 0.0043 |
| 48 h | 0 | 0.15 ± 0.27 |
| 7 days | 0 | 0.5 ± 0.0078 |
| Experiment | S. aureus | P. aeruginosa | E. coli |
|---|---|---|---|
| 1st | 0 | 0 | 0 |
| 2nd | 0 | 30 | 20 |
| 3rd | 0 | 10 | 120 |
| Mean | 0 | 20 | 70 |
| Infiltrated bacteria (%) | 0 | 0.0002 | 0.0007 |
| ±SD | 0 | 0.000153 | 0.000643 |
| Retained bacteria (%) | 100 | 99.9998 | 99.9993 |
| Sample | S. aureus | P. aeruginosa | E. coli |
|---|---|---|---|
| Control | 5.6 × 108 ± 1.9 × 108 | 1.28 × 108 ± 1.9 × 108 | 1.41 × 108 ± 2.08 × 108 |
| Presence of 2D-CM | 6.1 × 108 ± 1.6 × 108 | 1.9 × 108 ± 0.7 × 108 | 1.47 × 108 ± 2.41 × 108 |
| Sample | COL1A1 | FN | MMP3 | TGF-β | FGF | IL-1β |
|---|---|---|---|---|---|---|
| 24 h | 0.94 ± 0.05 | 1.23 ± 0.2 | 1.25 ± 0.23 | 0.79 ± 0.05 * | 0.66 ± 0.28 | 1.08 ± 0.21 |
| 120 h | 1.27 ± 0.20 | 1.46 ± 0.13 * | 1.20 ± 0.55 | 0.94 ± 0.24 | 0.76 ± 0.16 | 1.30 ± 0.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tassara, E.; Oliveri, C.; Vezzulli, L.; Cerrano, C.; Xiao, L.; Giovine, M.; Pozzolini, M. 2D Collagen Membranes from Marine Demosponge Chondrosia reniformis (Nardo, 1847) for Skin-Regenerative Medicine Applications: An In Vitro Evaluation. Mar. Drugs 2023, 21, 428. https://doi.org/10.3390/md21080428
Tassara E, Oliveri C, Vezzulli L, Cerrano C, Xiao L, Giovine M, Pozzolini M. 2D Collagen Membranes from Marine Demosponge Chondrosia reniformis (Nardo, 1847) for Skin-Regenerative Medicine Applications: An In Vitro Evaluation. Marine Drugs. 2023; 21(8):428. https://doi.org/10.3390/md21080428
Chicago/Turabian StyleTassara, Eleonora, Caterina Oliveri, Luigi Vezzulli, Carlo Cerrano, Lian Xiao, Marco Giovine, and Marina Pozzolini. 2023. "2D Collagen Membranes from Marine Demosponge Chondrosia reniformis (Nardo, 1847) for Skin-Regenerative Medicine Applications: An In Vitro Evaluation" Marine Drugs 21, no. 8: 428. https://doi.org/10.3390/md21080428








