1. Introduction
A lung abscess is a circumscribed, thick-walled cavity in the lung that contains purulent material resulting from the suppuration and necrosis of the involved lung parenchyma [
1,
2]. There are two main types of lung abscesses in children: primary, in which there are no predisposing factors, or secondary, in which there are underlying predisposing factors, either based in the lung or systemic [
1]. Other reported classifications include multiloculated and uniloculated, aspirational and hematogenous, or putrid and non-putrid (aerobic and anaerobic) [
3]. It can also be classified depending on the duration of the illness into acute, when it lasts 4 weeks or less, or chronic when it lasts longer than 4 weeks [
4,
5]. Primary lung abscess is predominantly caused by Streptococcus pneumoniae or Staphylococcus aureus [
3], whereas secondary lung abscess can be due to anaerobes (27%), Pseudomonas aeruginosa, (13%) Staphylococcus aureus (13%), Streptococcus pneumonia (7%), Haemophilus influenza (7%) [
2], Escherichia coli, or klebsiella [
4]. Secondary lung abscess is due to several possible structural or functional lung diseases, such as congenital lung malformations, ciliary disorders, cystic fibrosis, immunodeficiencies, aspirations, or infections [
1]. Although uncommon, lung abscesses can be further complicated by tuberculosis [
6]. The pathophysiology often starts as lung inflammation, followed by necrosis, progressive fibrosis, and cavity formation, leading to the suppurative destruction of lung parenchyma with central cavitation [
4]. Lung abscess is a relatively uncommon pediatric illness, with an incidence as low as 0.7/100.000 admissions/year, as reported by Patradoon-Ho and Fitzgerald, and 39 cases/10 years, as reported by Madhani et al. [
3]. The morbidity of pediatric lung abscesses was also lower than that in adults [
7]. It is rare in neonates and more common in fall and wintertime [
8]. Diagnosis is confirmed by chest X-rays, ultrasonography, and computed tomography. Prolonged treatment with empiric broad-spectrum antibiotics is initiated until the causative organism is identified via respiratory culture, which may not be possible in some cases [
3]. However, interventional radiology is an alternative that introduces treatment through catheter placement when possible. This treatment approach has the advantage of allowing for quicker recovery from fever and other symptoms, as well as shorter hospitalization times. Other surgical approaches include drainage, aspiration, and resection [
5,
9]. This report presents three cases of secondary lung abscess and one case of primary lung abscess in children ranging from 13 months to 7 years.
3. Discussion
The literature on pediatric lung abscess case series is scarce [
3]. Dhanushke et al. reported unwarranted variation in the management of pediatric lung abscesses with an alarmingly prolonged hospitalization [
10]. Studies have reported fever, cough, and dyspnea as the most common symptoms of lung abscess [
11,
12].
In our study, the most common symptoms were fever (100%), cough (75%), chest/abdominal pain (50%), and dyspnea (50%), with a mean duration of 13 days (range 3–56). This matches what has been reported in the literature [
3,
11,
12]. The patients in our cases had a dry, non-productive cough initially, but when communication with the airway happened, the cough changed to be wet and productive [
11,
12]; none were clubbed, which could be seen in severe cases.
Lung abscesses can develop in any part of the lung [
11], and the most common site of the abscess varies between reported studies. Two of our cases had left-sided lung abscesses, while the other two had right-sided lung abscesses, and 50% of our cases were in the left lower lobe, similar to Madhani et al., 33% [
3].
The differential diagnosis may include congenital lung cyst, hydatid cyst, and mycobacterium [
5].
The organism was identified in two cases, 50% (the second case from the aspirated fluid and the fourth case from the sputum culture). Despite the appropriate antibiotic based on sensitivity, the second patient progressed to surgical intervention due to the presence of sequestration as a predisposing factor. The yield of blood cultures in our cases was negative. Currently, the increase in the interventional approach might increase the yield of pathogens responsible for lung abscess from 30% to potentially 60% [
10,
13,
14].
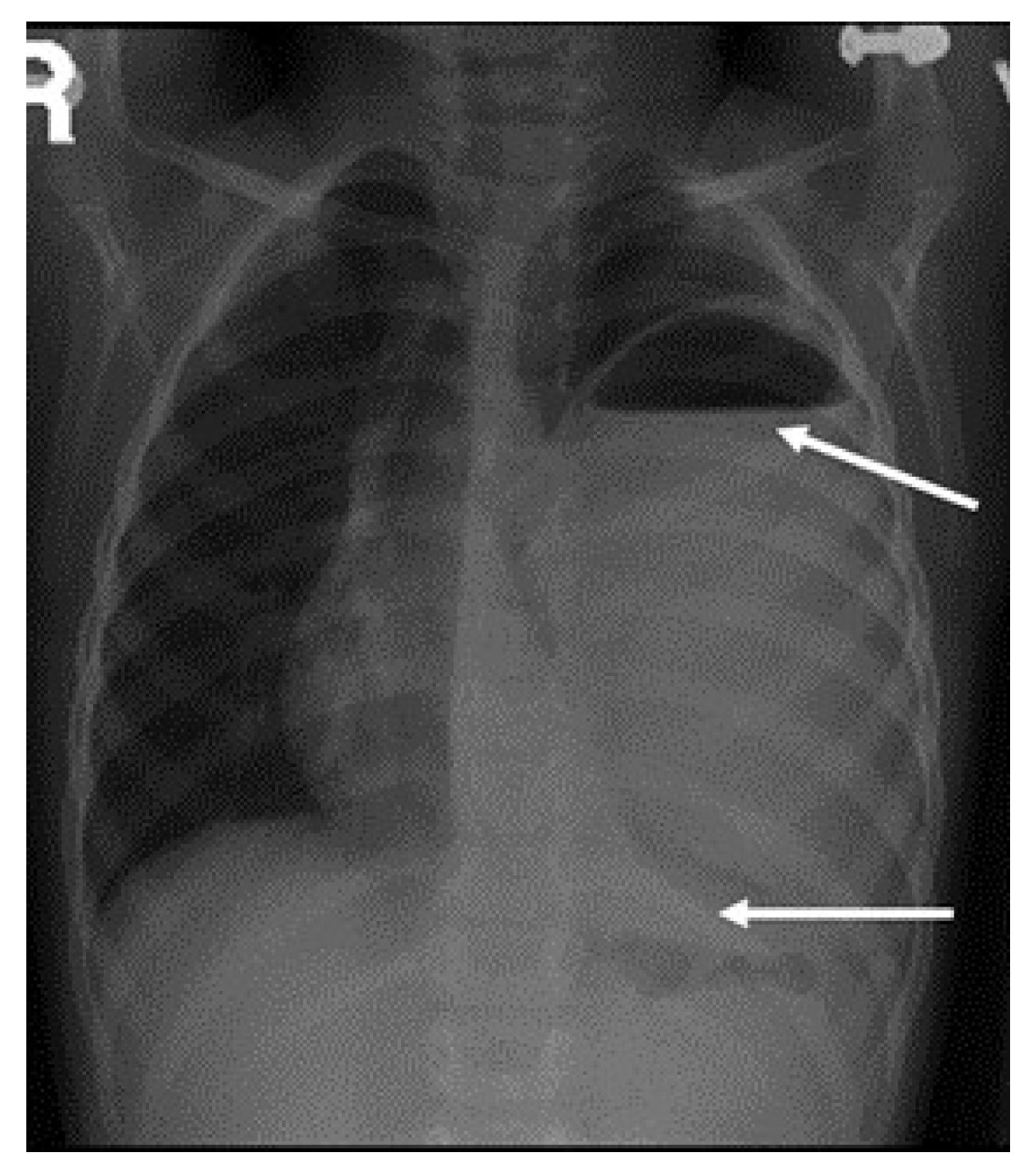
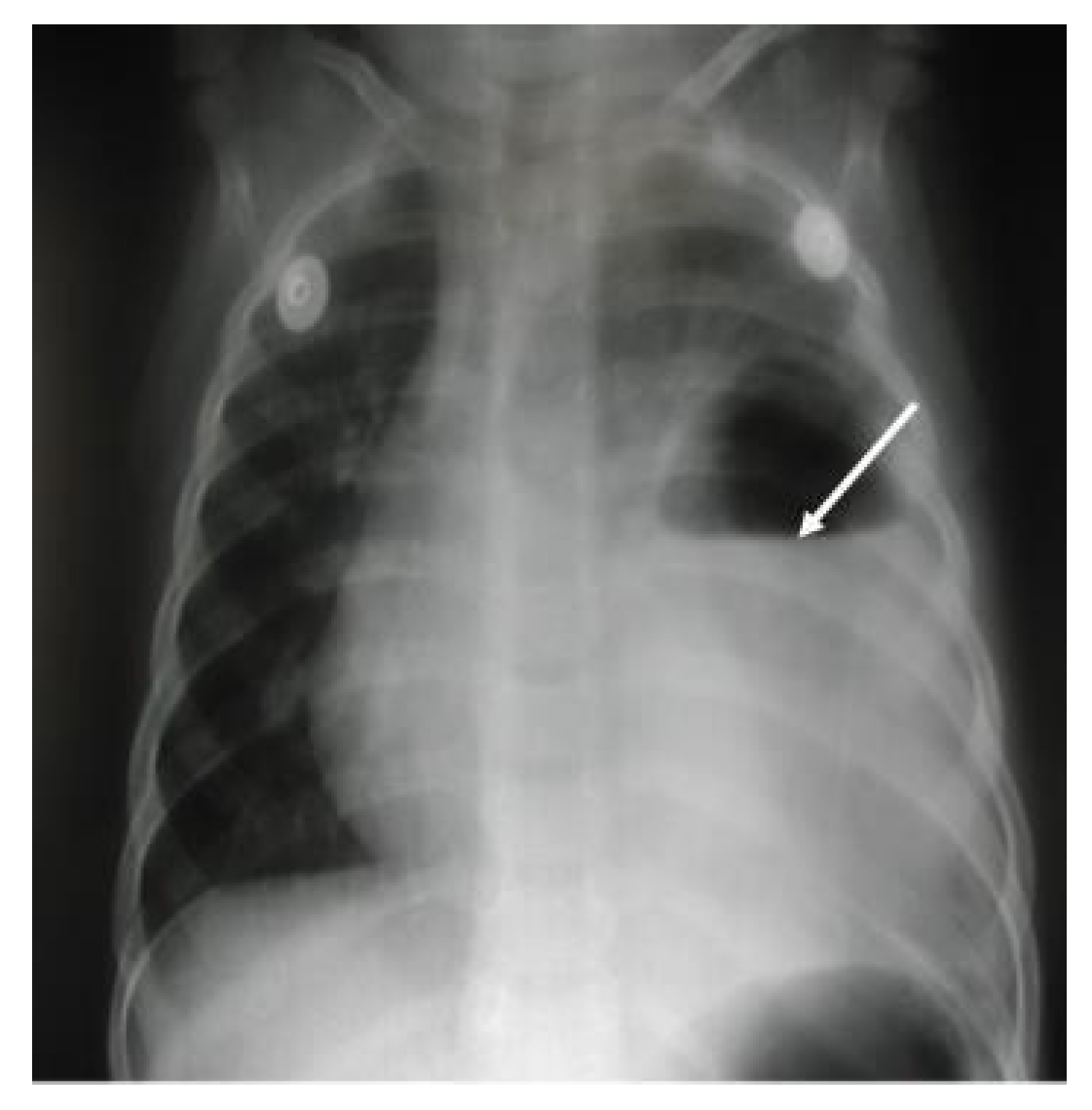
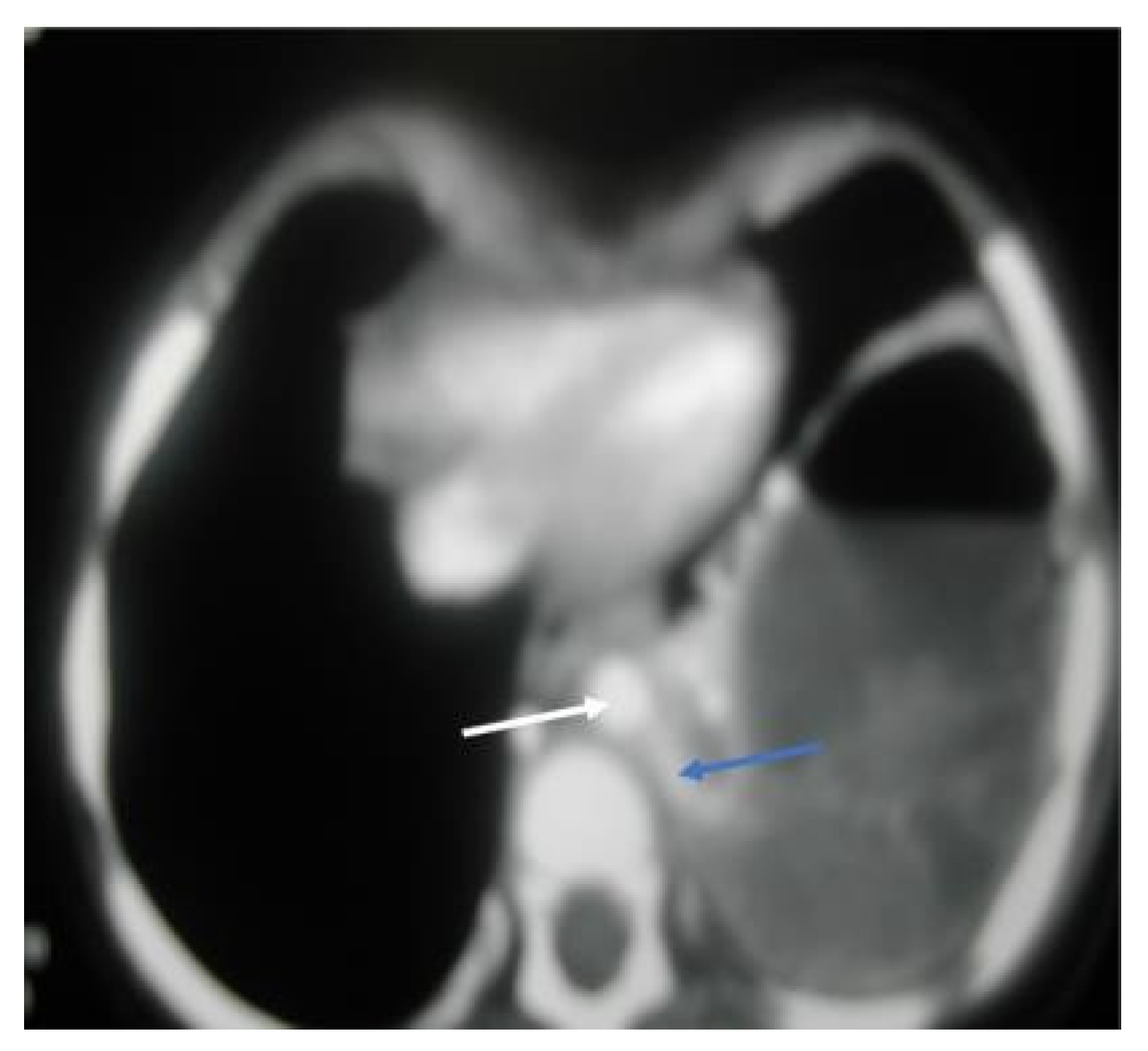
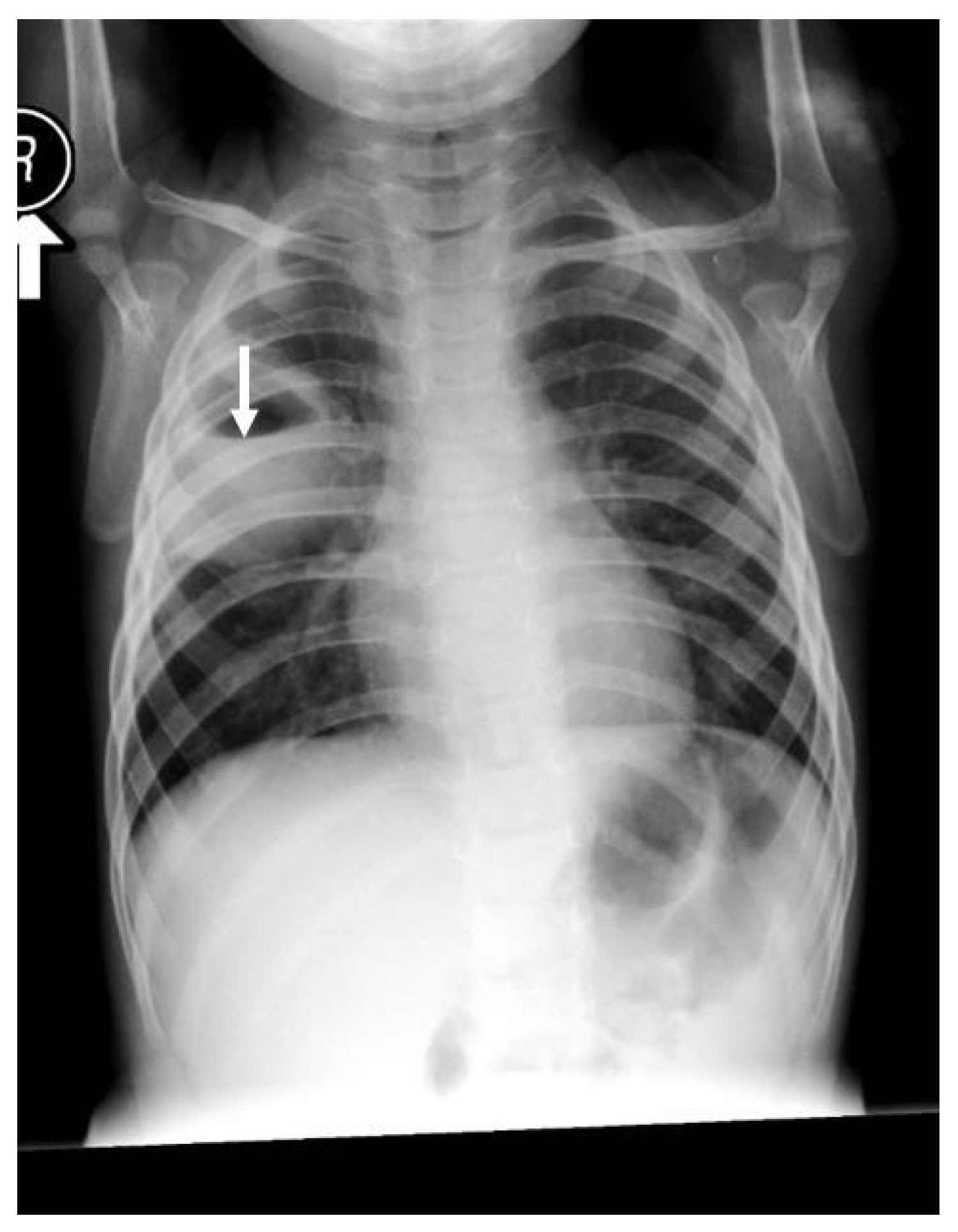
Chest radiography is often the diagnostic method of choice as in our cases [
3]; however, chest CT is often indicated in suboptimal response prior to intervention, differentiating lung abscess from empyema and ruling out potential lung malformation [
12,
14].
Yunus found that 42% of 19 patients with lung abscesses encountered no complication in CT guidance catheter placement. The most common complication was pneumothorax (26%). Luckily, no complication was reported in our cases [
15].
Bronchoscopy and lavage could be utilized if the patient is still symptomatic after the first week of conservative therapy to retrieve organisms and exclude endobronchial obstruction [
5]. Contributing factors to lung abscess in children should be looked at carefully, including lung malformation such as as congenital cyst, gastroesophageal reflux disease, immunodeficiency, weak cough, and immunosuppressive agents [
5,
9,
12]. Three of our cases were secondary lung abscesses, and only one was primary. However, in a newly published Australian study, it was found that among 68 cases, 81% were predominantly primary and Staphylococcus aureus (including MRSA) was the commonest organism at 80% [
10].
There are several approaches to treating lung abscesses, ranging from conservative approaches such as standard therapy to different types of surgical interventions [
1,
3,
5,
9,
12].
The standard course of treatment involves an extended period of intravenous antibiotics for 24 days [
3]. However, Chan et al. found the mean duration of IV antibiotic treatment was 40 days [
9]. Madhani et al. reported patients who received IV antibiotics to be 28 days for primary lung abscess and 45 days for secondary lung abscess. Third-generation cephalosporin (cefotaxime or ceftriaxone) and clindamycin were the initial therapies in 75% of our cases, similar to what has been recommended by Madhani et al. [
3]. The duration of therapies in our cases ranged from 3 weeks, as in the fourth case, to 8 weeks, as in the first one. Combination therapies can be tailored according to the response, radiological change, and acute phase reactants result as in the first case in which a more potent antibiotic commenced [
11,
16].
Treatment with IV antibiotics can fail if the abscess is larger than 6 cm or if the patient has other contributing factors [
17]. The next treatment option is surgical intervention, which ranges from chest tube insertion, pigtail catheter placement, video-assisted thoracoscopy, or lobectomy [
5,
14].
Pigtail catheter has shown a quicker recovery time from fever and other symptoms, as well as less overall hospitalization for lung abscess [
5,
9].
The three secondary lung abscesses in our study were treated with IV antibiotics for a prolonged period, after which a lobectomy was performed, whereas the primary lung abscess case was managed with IV antibiotics only and had a full recovery. As the literature suggests, pediatric patients who have complicated cases of lung abscess or do not show clinical or radiological improvements in their condition after being on the recommended course of IV antibiotics or after having simple drainage performed might need surgical procedures such as lobectomy [
11].
Similarly, Wali et al. argued that although 80–90% of patients with lung abscesses can be successfully treated with antibiotics, this treatment can also fail. If that happens, pulmonary resection is the advised course of treatment [
13].
In our study, the first case was referred to the tertiary hospital for further evaluation for complicated pneumonia. Her left-sided lung abscess was confirmed via CT scans, and she was managed non-surgically through IV antibiotics of vancomycin and meropenem for a period of 4 weeks. After that, the patient received a lobectomy of the left lower lobe and an additional 4 weeks of antibiotics. Similarly, the second case was also a complicated case of pneumonia and was referred to the hospital for further evaluation. The patient had a wet cough and a high-grade, persistent fever. The CT scans revealed complicated pneumonia with a suspected lung abscess.
The patient was started on IV antibiotics of clindamycin and cefotaxime, and drainage was performed. She completed 14 days of IV antibiotics and was slightly improving before returning 5 days later with a worsening condition. The patient was diagnosed with a left-sided lung abscess secondary to pulmonary sequestration and was put on further antibiotics until she improved. She was then treated with lobectomy. The third case was a 21-month-old boy with a fever and cough, and reduced breath sounds on the right side but an otherwise normal exam. Blood culture was negative, and CT scans showed a right lower lobe lung abscess and sequestrated right lower lobe. The patient was treated with cefotaxime and vancomycin for 3 weeks and scheduled back for a lobectomy after 6 weeks of IV antibiotic treatment due to the large size of her lung abscess and sequestration. The only case in this study that was managed by antibiotics alone was the only patient with a primary lung abscess. This patient, who was previously well, had an acute history of fever, cough, and chest pain for 3 days. The sputum culture was positive for Staphylococcus aureus, and the chest X-ray showed a small right-sided lung abscess. The patient received ceftriaxone and clindamycin, and by the fourth day, CT scans already showed resolution of the fluid. The patient received a total of three weeks of treatment with complete resolution of lung cavitation on chest X-ray.
Based on our surgical cases, the interventions’ duration varied (four weeks, one week, and six weeks) with a mean of 3.7 weeks which is approaching the definition of chronic illness, which lasts more than 4 weeks [
5].
In a retrospective review of cases in the literature, Yen et al. reported that 39% of their patients had been treated non-operatively by IV antibiotics solely or together with a percutaneous drainage procedure [
11]. While surgical intervention is not always the selected approach [
3], the remaining majority, i.e., 61%, had to be managed surgically [
11]. Madhani et al. found that only 10 cases out of 39 had received surgical intervention [
3]. Based on the presented cases and the data available in the literature, surgical treatment for lung abscess might be needed when a lung abscess patient does not respond to intravenous antibiotic treatment alone [
11,
16,
18]. Surgical drainage under CT guidance with a pigtail catheter is very beneficial when the response is unsatisfactory [
5]. Video-assisted thoracoscopy is gaining popularity, whereas lobectomy is rare nowadays [
5,
9].