Osteomyelitis Possibly Caused by Exfoliation of Primary Teeth in a Patient with Osteopetrosis
Abstract
:1. Introduction
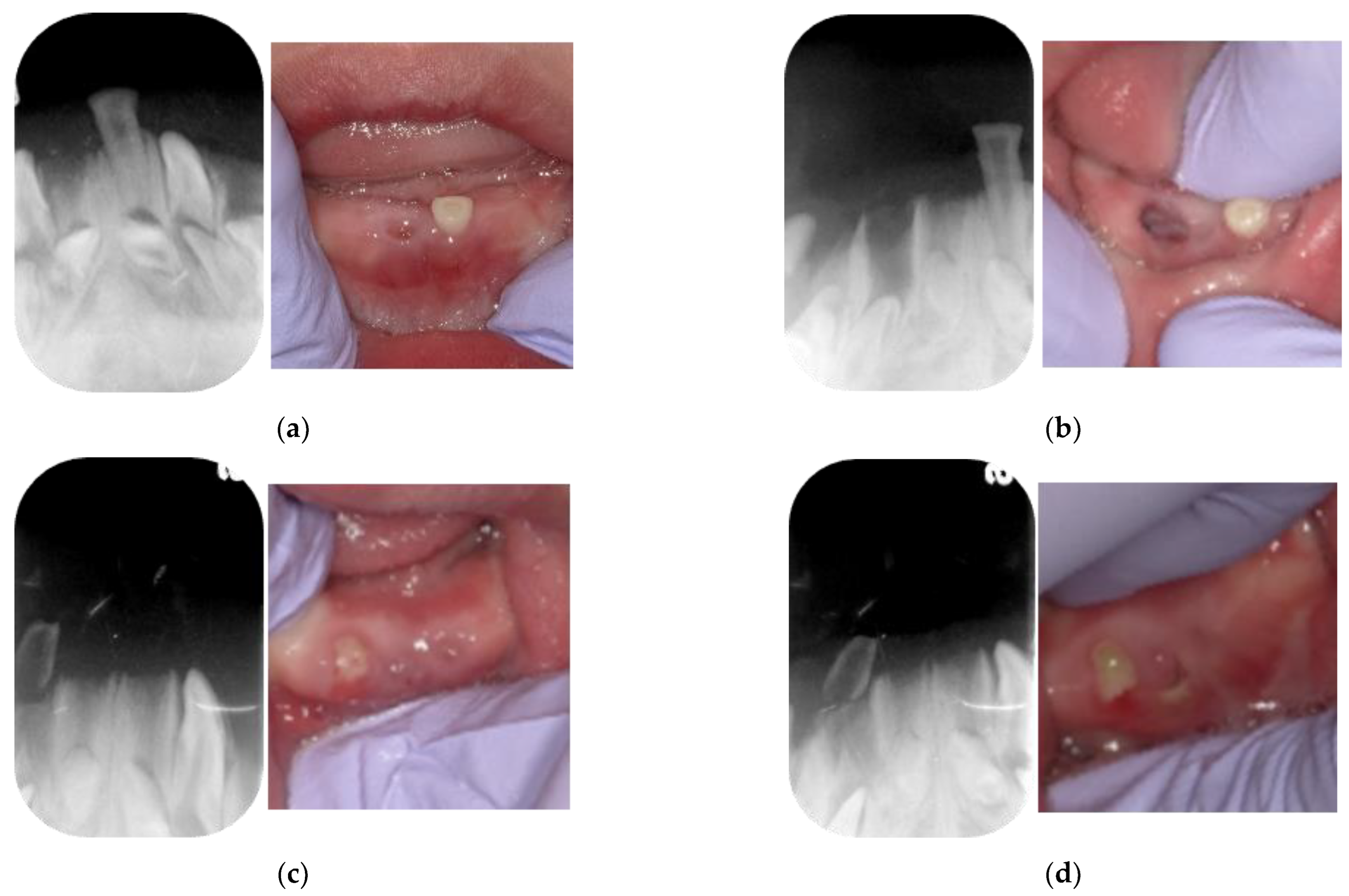
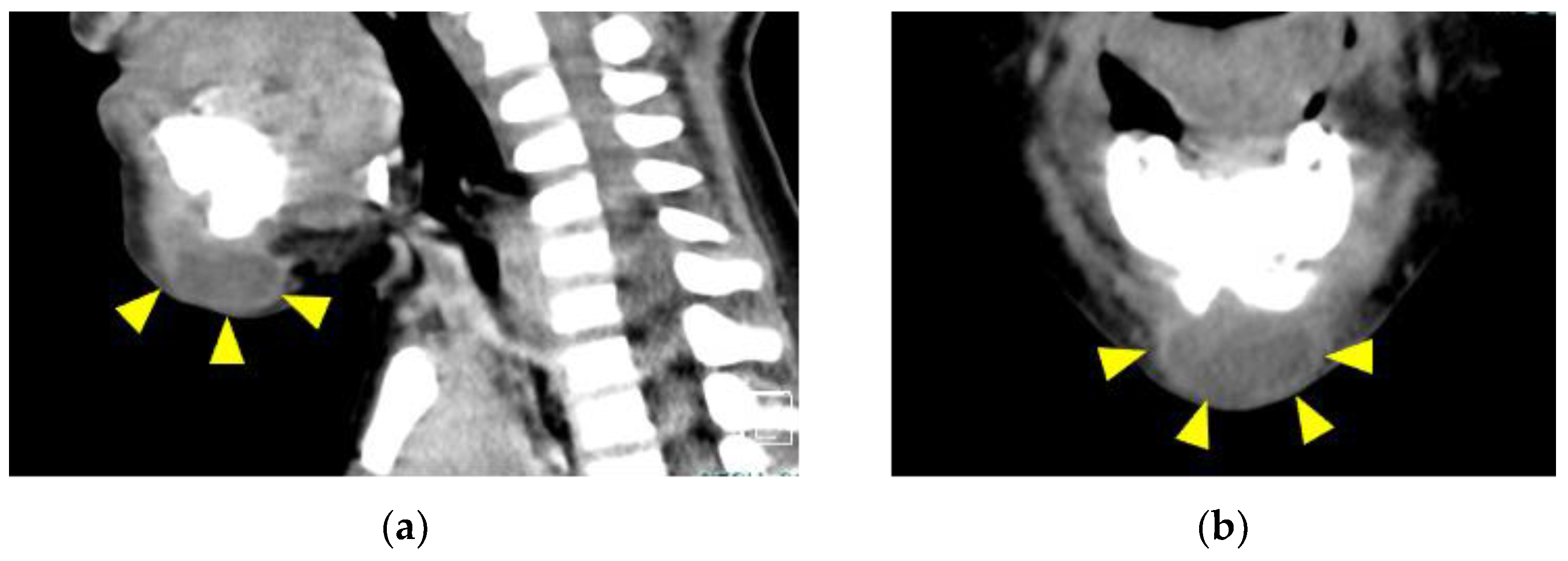
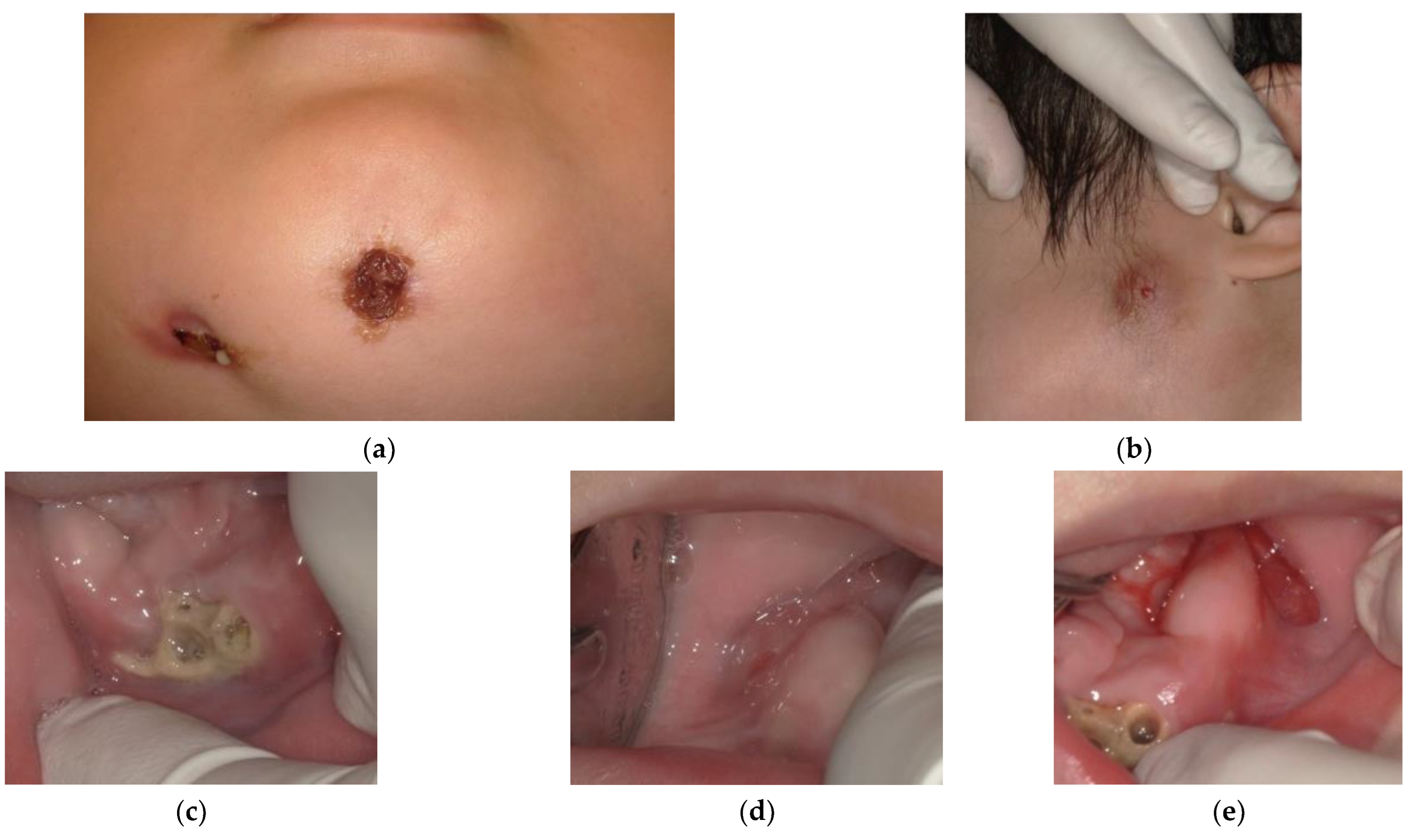
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stark, Z.; Savarirayan, R. Osteopetrosis. Orphanet J. Rare Dis. 2009, 4, 5. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.C.; Econs, M.J.; DiMeglio, L.A.; Insogna, K.L.; Levine, M.A.; Orchard, P.J.; Miller, W.P.; Petryk, A.; Rush, E.T.; Shoback, D.M.; et al. Diagnosis and Management of Osteopetrosis: Consensus Guidelines From the Osteopetrosis Working Group. J. Clin. Endocrinol. Metab. 2017, 102, 3111–3123. [Google Scholar] [CrossRef] [Green Version]
- Sawamura, K.; Mishima, K.; Matsushita, M.; Kamiya, Y.; Kitoh, H. A cross-sectional nationwide survey of osteosclerotic skeletal dysplasias in Japan. J. Orthop. Sci. 2021, 27, 1139–1142. [Google Scholar] [CrossRef]
- Toranzo Fernandez, J.M.; Noyola Frias, M.A.; Hernandez Duarte, S.P. Infantile osteopetrosis: A case report with osteomyelitis of the maxilla. J. Clin. Pediatr. Dent. 2002, 27, 77–80. [Google Scholar] [CrossRef]
- Luzzi, V.; Consoli, G.; Daryanani, V.; Santoro, G.; Sfasciotti, G.L.; Polimeni, A. Malignant infantile osteopetrosis: Dental effects in paediatric patients. Case reports. Eur. J. Paediatr. Dent. 2006, 7, 39–44. [Google Scholar]
- Lam, D.K.; Sándor, G.K.; Holmes, H.I.; Carmichael, R.P.; Clokie, C.M. Marble bone disease: A review of osteopetrosis and its oral health implications for dentists. J. Can. Dent. Assoc. 2007, 73, 839–843. [Google Scholar]
- Bansal, V.; Kumar, S.; Arunkumar, K.V.; Mowar, A.; Khare, G. Dental management in autosomal recessive (intermediate) osteopetrosis: A case report. Pediatr. Dent. 2010, 32, 542–545. [Google Scholar]
- Detailleur, V.; Vansteenkiste, G.; Renard, M.; Verdonck, A. Dental care approach in patients with osteopetrosis. Eur. Arch. Paediatr. Dent. 2016, 17, 435–443. [Google Scholar] [CrossRef]
- Vinay, C.; Uloopi, K.S.; Rao, R.C.; Kumar, R.S.; Madhuri, V. Oligodontia associated with osteopetrosis: A rare case report. J. Dent. Child 2011, 78, 53–56. [Google Scholar]
- Sekerci, A.E.; Sisman, Y.; Ertas, E.T.; Sahman, H.; Aydinbelge, M. Infantile malignant osteopetrosis: Report of 2 cases with osteomyelitis of the jaws. J. Dent. Child 2012, 79, 93–99. [Google Scholar]
- Reddy, M.R. Osteopetrosis (Marble Bone Disease): A Rare Disease in Children. Int. J. Clin. Pediatr. Dent. 2011, 4, 232–234. [Google Scholar] [CrossRef]
- Machado, C.V.; da Rocha, M.C.; Telles, P.D. Infantile osteopetrosis associated with osteomyelitis. BMJ Case Rep. 2015, 2015, bcr2014208085. [Google Scholar] [CrossRef] [Green Version]
- Bjorvatn, K.; Gilhuus-Moe, O.; Aarskog, D. Oral aspects of osteopetrosis. Scand. J. Dent. Res. 1979, 87, 245–252. [Google Scholar] [CrossRef]
- Rehani, U.; Adlakha, V.K.; Chandna, P.; Agarwal, A.; Rana, V.; Malik, P. Prosthetic Rehabilitation in Marble Bone Disease. Int. J. Clin. Pediatr. Dent. 2010, 3, 207–210. [Google Scholar] [CrossRef]
- Er, N.; Kasaboğlu, O.; Atabek, A.; Oktemer, K.; Akkocaoğlu, M. Topical phenytoin treatment in bimaxillary osteomyelitis secondary to infantile osteopetrosis: Report of a case. J. Oral Maxillofac. Surg. 2006, 64, 1160–1164. [Google Scholar] [CrossRef]
- Yamada, T.; Mishima, K.; Imura, H.; Ueno, T.; Matsumura, T.; Moritani, N.; Sugahara, T. Osteomyelitis of the mandible secondary to infantile osteopetrosis: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, e25–e29. [Google Scholar] [CrossRef] [PubMed]
- Bedi, R.S.; Goel, P.; Pasricha, N.; Sachin; Goel, A. Osteopetrosis-A rare entity with osteomyelitis. Ann. Maxillofac. Surg. 2011, 1, 155–159. [Google Scholar] [PubMed] [Green Version]
- Gomes, M.F.; Rangel, D.C.; Starling, C.C.; Goulart, M. Familial malignant osteopetrosis in children: A case report. Spec. Care Dentist. 2006, 26, 106–110. [Google Scholar] [CrossRef]
- Okawa, R.; Fujita, K.; Naka, S.; Nakano, K. Epulis appeared after exfoliation of natal tooth in infant Japanese boy. Ped. Dent. J. 2014, 24, 189–191. [Google Scholar] [CrossRef]
- Balan, A.; Girija, K.L.; Ranimol, P. Osteomyelitis of Maxilla in Infantile Osteopetrosis: A Case Report with Review of Literature. Int. J. Clin. Pediatr. Dent. 2011, 4, 125–128. [Google Scholar] [CrossRef]
- Managutti, S.; Managutti, A.; Pragasm, M. Infantile osteomyelitis secondary to malignant osteopetrosis. J. Maxillofac. Oral Surg. 2012, 11, 109–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, S.S.; Saravanan, C.; Sathyabama, V.; Satish, C. Osteopetrosis of the mandible masquerading as tubercular osteomyelitis. BMJ Case Rep. 2013, 2013, bcr2012007487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jayachandran, S.; Kumar, M.S. A paradoxical presentation of rickets and secondary osteomyelitis of the jaw in Type II autosomal dominant osteopetrosis: Rare case reports. Indian J. Dent. Res. 2016, 27, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Ingole, S.N.; Deshpande, M.D.; Kazi, N.; Meshram, D.; Ranadive, P. A Rare Case of Osteoclast-poor Osteopetrosis (RANKL Mutation) with Recurrent Osteomyelitis of Mandible: A Case Report. Int. J. Clin. Pediatr. Dent. 2020, 13, 717–721. [Google Scholar] [CrossRef]
- Sarnat, B.G.; Robinson, I.B. Surgery of the mandible; some clinical and experimental considerations. Plast. Reconstr. Surg. 1956, 17, 27–57. [Google Scholar] [CrossRef]
- Valentini, V.; Califano, L.; Cassoni, A.; Marco, D.M.; Raponi, I.; Priore, P.; Fadda, M.T.; Dell’Aversana Orabona, G.; Terenzi, V. Maxillo-Mandibular Reconstruction in Pediatric Patients: How To Do It? J. Craniofac. Surg. 2018, 29, 761–766. [Google Scholar] [CrossRef]
- Raiteb, M.; Elmrini, S.; Slimani, F. Surgical management of chronic osteomyelitis with benign osteopetrosis: A case report. Ann. Med. Surg. 2021, 65, 102296. [Google Scholar] [CrossRef]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okawa, R.; Yokota, Y.; Morita, Y.; Mikasa, Y.; Nakano, K. Osteomyelitis Possibly Caused by Exfoliation of Primary Teeth in a Patient with Osteopetrosis. Children 2022, 9, 1894. https://doi.org/10.3390/children9121894
Okawa R, Yokota Y, Morita Y, Mikasa Y, Nakano K. Osteomyelitis Possibly Caused by Exfoliation of Primary Teeth in a Patient with Osteopetrosis. Children. 2022; 9(12):1894. https://doi.org/10.3390/children9121894
Chicago/Turabian StyleOkawa, Rena, Yusuke Yokota, Yoshihiro Morita, Yusuke Mikasa, and Kazuhiko Nakano. 2022. "Osteomyelitis Possibly Caused by Exfoliation of Primary Teeth in a Patient with Osteopetrosis" Children 9, no. 12: 1894. https://doi.org/10.3390/children9121894
APA StyleOkawa, R., Yokota, Y., Morita, Y., Mikasa, Y., & Nakano, K. (2022). Osteomyelitis Possibly Caused by Exfoliation of Primary Teeth in a Patient with Osteopetrosis. Children, 9(12), 1894. https://doi.org/10.3390/children9121894





