A Novel Bacterium-Like Particle-Based Vaccine Displaying the SUDV Glycoprotein Induces Potent Humoral and Cellular Immune Responses in Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Construction and Expression of Recombinant Baculoviruses
2.2. Expression Analyses of Recombinant Baculoviruses
2.3. Preparation of SUDV BLP (SBLP) Vaccine
2.4. Identification of GEM Particle Binding
2.5. Immunizations of Mice and the Associated Ethics Statement
2.6. Analysis of Mouse Antibody Titers by Indirect ELISA
2.7. Pseudovirion Neutralization Assay
2.8. IFN-γ, IL-4, and TNF-α ELISpot Assays
2.9. ELISA Measurement of Cytokine Secretion
2.10. Statistical Analysis
3. Results
3.1. Expression of SUDV eGP-PA Fusion Protein
3.2. Location of the Fusion Protein on GEM Particles
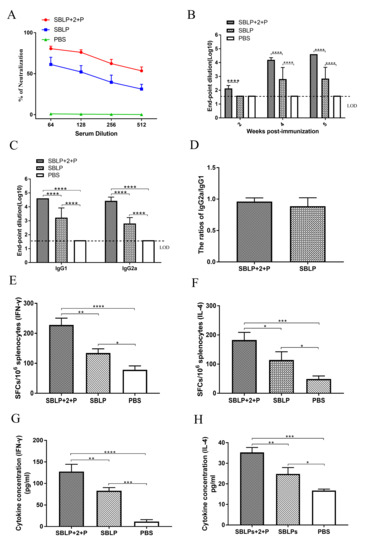
3.3. Antibody Responses Induced by SBLP
3.4. Antigen-Specific Cellular Immune Responses
3.5. SBLP Vaccine-Enhanced Splenocyte Cytokine Secretion
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sylvain, B.; Delphine, P.; Lisa, O.; Toni, R.; Lamine, K.; N’Faly, M.; Barrè, S.; Mamadou Saliou, S.; Sakoba, K.T.; Hilde, D.C. Emergence of Zaire Ebola virus disease in Guinea. N. Engl. J. Med. 2014, 371, 1418–1425. [Google Scholar]
- Murin, C.D.; Bruhn, J.F.; Bornholdt, Z.A.; Copps, J.; Stanfield, R.; Ward, A.B. Structural Basis of Pan-Ebolavirus Neutralization by an Antibody Targeting the Glycoprotein Fusion Loop. Cell Rep. 2018, 24, 2723–2732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobinger, G.P.; Anders, L.; James, N.; Richardson, J.S.; Darryl, F.; Greg, S.; Kevin, T.; Ami, P.; Weingartl, H.M. Replication, pathogenicity, shedding, and transmission of Zaire ebolavirus in pigs. J. Infect. Dis. 2011, 204, 200–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de la Calle-Prieto, F.; Arsuaga-Vicente, M.; Mora-Rillo, M.; Arnalich-Fernandez, F.; Arribas, J.R. Ebola virus disease: Update. Enferm. Infecc. Y Microbiol. Clin. 2016, 34, 452. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ebola virus disease. Available online: https://www.who.int/en/news-room/fact-sheets/detail/ebola-virus-disease (accessed on 8 December 2019).
- Awah, P.K.; Boock, A.U.; Kum, K.A. Ebola Virus Diseases in Africa: A commentary on its history, local and global context. Pan Afr. Med J. 2015, 22 (Suppl 1), 18. [Google Scholar]
- Albariño, C.G.; Shoemaker, T.; Khristova, M.L.; Wamala, J.F.; Muyembe, J.J.; Balinandi, S.; Tumusiime, A.; Campbell, S.; Cannon, D.; Gibbons, A. Genomic analysis of filoviruses associated with four viral hemorrhagic fever outbreaks in Uganda and the Democratic Republic of the Congo in 2012. Virology 2013, 442, 97–100. [Google Scholar] [CrossRef] [Green Version]
- Dias, J.M.; Kuehne, A.I.; Abelson, D.M.; Bale, S.; Wong, A.C.; Halfmann, P.; Muhammad, M.A.; Fusco, M.L.; Zak, S.E.; Kang, E. A shared structural solution for neutralizing ebolaviruses. Nat. Struct. Mol. Biol. 2012, 18, 1424–1427. [Google Scholar] [CrossRef] [PubMed]
- Volchkov, V.E.; Volchkova, V.A.; Dolnik, O.; Feldmann, H.; Klenk, H.D. Polymorphism of Filovirus Glycoproteins. Adv. Virus Res. 2005, 64, 359–381. [Google Scholar]
- Qiu-Dong, S.; Shi-Hua, H.; Yao, Y.; Feng, Q.; Xue-Xin, L.; Zhi-Yuan, J.; Qing-Ling, M.; Xue-Ting, F.; Rui-Guang, T.; Jonathan, A. Intranasal vaccination with ebola virus GP amino acids 258–601 protects mice against lethal challenge. Vaccine 2018, 36, 6053–6060. [Google Scholar]
- Grant-Klein, R.J.; Altamura, L.A.; Badger, C.V.; Bounds, C.E.; Van Deusen, N.M.; Kwilas, S.A.; Vu, H.A.; Warfield, K.L.; Hooper, J.W.; Hannaman, D. Codon-optimized filovirus DNA vaccines delivered by intramuscular electroporation protect cynomolgus macaques from lethal Ebola and Marburg virus challenges. Hum. Vaccin. Immunother. 2015, 11, 1991–2004. [Google Scholar] [CrossRef]
- Stanley, D.A.; Honko, A.N.; Asiedu, C.; Trefry, J.C.; Lau-Kilby, A.W.; Johnson, J.C.; Hensley, L.; Ammendola, V.; Abbate, A.; Grazioli, F. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat. Med. 2014, 20, 1126–1129. [Google Scholar] [CrossRef]
- Agnandji, S.T.; Huttner, A.; Zinser, M.E.; Njuguna, P.; Dahlke, C.; Fernandes, J.F.; Yerly, S.; Dayer, J.A.; Kraehling, V.; Kasonta, R. Phase 1 Trials of rVSV Ebola Vaccine in Africa and Europe - Preliminary Report. N. Engl. J. Med. 2016, 374, 1647. [Google Scholar] [CrossRef] [PubMed]
- Warfield, K.L.; Swenson, D.L.; Olinger, G.G.; Kalina, W.V.; Aman, M.J.; Bavari, S. Ebola Virus-Like Particle-Based Vaccine Protects Nonhuman Primates against Lethal Ebola Virus Challenge. J. Infect. Dis. 2007, 196 (Suppl 2), S430. [Google Scholar] [CrossRef] [Green Version]
- Martins, K.A.; Jahrling, P.B.; Bavari, S.; Kuhn, J.H. Ebola Virus Disease Candidate Vaccines Under Evaluation in Clinical Trials. Expert Rev. Vaccines 2016, 15, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Lambe, T.; Bowyer, G.; Ewer, K.J. A review of Phase I trials of Ebola virus vaccines: What can we learn from the race to develop novel vaccines? Philos. Trans. of the R. Soc. B Biol. Sci. 2017, 372, 20160295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henaorestrepo, A.M.; Camacho, A.; Longini, I.M.; Watson, C.H.; Edmunds, W.J.; Egger, M.; Carroll, M.W.; Dean, N.E.; Diatta, I.; Doumbia, M. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: Final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 2016, 386, 857–866. [Google Scholar] [CrossRef]
- Suder, E.; Furuyama, W.; Feldmann, H.; Marzi, A.; De, W.E. The vesicular stomatitis virus-based Ebola virus vaccine: From concept to clinical trials. Hum. Vaccin. Immunother. 2018, 14, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Ríos-Huerta, R.; Monreal-Escalante, E.; Govea-Alonso, D.O.; Angulo, C.; Rosales-Mendoza, S. Expression of an immunogenic LTB-based chimeric protein targeting Zaire ebolavirus epitopes from GP1 in plant cells. Plant Cell Rep. 2016, 36, 1–11. [Google Scholar] [CrossRef]
- Konduru, K.; Shurtleff, A.C.; Bradfute, S.B.; Nakamura, S.; Bavari, S.; Kaplan, G. Ebolavirus Glycoprotein Fc Fusion Protein Protects Guinea Pigs against Lethal Challenge. PLoS ONE 2016, 11, e0162446. [Google Scholar] [CrossRef]
- Sang, Y.L.; Choi, J.H.; Xu, Z. Microbial cell-surface display. Trends Biotechnol. 2003, 21, 45–52. [Google Scholar]
- Bosma, T.; Kanninga, R.; Neef, J.; Audouy, S.; Van Roosmalen, M.; Steen, A.; Buist, G.; Kok, J.; Kuipers, O.; Robillard, G. Novel surface display system for proteins on non-genetically modified gram-positive bacteria. Appl. Environ. Microbiol. 2006, 72, 880–889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, D.; Lu, J.; Yu, J.; Hou, H.; Leenhouts, K.; Roosmalen, M.L.V.; Gu, T.; Jiang, C.; Kong, W.; Wu, Y. A Novel PspA Protein Vaccine Intranasal Delivered by Bacterium-Like Particles Provides Broad Protection Against Pneumococcal Pneumonia in Mice. Immunol. Investig. 2018, 47, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Van Roosmalen, M.L.; Rolf, K.; Mohamed, E.K.; Jolanda, N.; Sandrine, A.; Tjibbe, B.; Anneke, K.; Eduard, P.; Anton, S.; Jan, K. Mucosal vaccine delivery of antigens tightly bound to an adjuvant particle made from food-grade bacteria. Methods 2006, 38, 144–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, P.C.; Qiao, X.W.; Zheng, Q.S.; Hou, J.B. Immunogenicity and immunoprotection of porcine circovirus type 2 (PCV2) Cap protein displayed by Lactococcus lactis. Vaccine 2016, 34, 696–702. [Google Scholar] [CrossRef]
- Li, E.; Chi, H.; Huang, P.; Yan, F.; Zhang, Y.; Liu, C.; Wang, Z.; Li, G.; Zhang, S.; Mo, R.; et al. A Novel Bacterium-Like Particle Vaccine Displaying the MERS-CoV Receptor-Binding Domain Induces Specific Mucosal and Systemic Immune Responses in Mice. Viruses 2019, 11, 799. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Ye, L.; Lin, F.; Gomaa, Y.; Flyer, D.; Carrion, R.; Patterson, J.L.; Prausnitz, M.R.; Smith, G.; Glenn, G. Intradermal immunization by Ebola virus GP subunit vaccines using microneedle patches protects mice against lethal EBOV challenge. Sci. Rep. 2018, 8, 11193. [Google Scholar] [CrossRef]
- Wu, X.-X.; Yao, H.-P.; Wu, N.-P.; Gao, H.-N.; Wu, H.-B.; Jin, C.-Z.; Lu, X.-Y.; Xie, T.-S.; Li, L.-J. Ebolavirus Vaccines: Progress in the Fight Against Ebola Virus Disease. Cell Physiol. Biochem. 2015, 37, 1641–1658. [Google Scholar] [CrossRef]
- Lehrer, A.T.; Wong, T.A.S.; Lieberman, M.M.; Humphreys, T.; Clements, D.E.; Bakken, R.R.; Hart, M.K.; Pratt, W.D.; Dye, J.M. Recombinant proteins of Zaire ebolavirus induce potent humoral and cellular immune responses and protect against live virus infection in mice. Vaccine 2017, 36, S0264410X17301482. [Google Scholar] [CrossRef]
- Krishnamurthy, K.; Bradfute, S.B.; Jerome, J.; Mohanraj, M.; Siham, N.; Sufi, M.; Wood, S.C.; Sina, B.; Kaplan, G.G. Ebola virus glycoprotein Fc fusion protein confers protection against lethal challenge in vaccinated mice. Vaccine 2011, 29, 2968–2977. [Google Scholar]
- Bazzill, J.D.; Stronsky, S.M.; Kalinyak, L.C.; Ochyl, L.J.; Steffens, J.T.; Van Tongeren, S.A.; Cooper, C.L.; Moon, J.J. Vaccine nanoparticles displaying recombinant Ebola virus glycoprotein for induction of potent antibody and polyfunctional T cell responses. Nanomedicine 2019, 18, 414–425. [Google Scholar] [CrossRef]
- Salminen, S.; Wright, A.V.; Morelli, L.; Marteau, P.; Brassart, D.; Vos, W.M.D.; Fondén, R.; Saxelin, M.; Collins, K.; Mogensen, G. Demonstration of safety of probiotics — A review. Int. J. Food Microbiol. 1998, 44, 93–106. [Google Scholar] [CrossRef]
- Cheng, H.; Chen, J.; Cai, Z.; Du, L.; Hou, J.; Qiao, X.; Zheng, Q. Development of GEM-PA-nanotrap for purification of foot-and-mouth disease virus. Vaccine 2019, 37, 3205–3213. [Google Scholar] [CrossRef] [PubMed]
- Waranyoo, P.; Dye, J.M.; Jacquelyn, K.; Khanrat, P.; Pratt, W.D.; Arntzen, C.J.; Qiang, C.; Mason, H.S.; Herbst-Kralovetz, M.M. A nonreplicating subunit vaccine protects mice against lethal Ebola virus challenge. Proc. Natl. Acad. Sci. USA 2011, 108, 20695–20700. [Google Scholar]
- Bengtsson, K.L.; Song, H.; Stertman, L.; Liu, Y.; Flyer, D.C.; Massare, M.J.; Xu, R.H.; Zhou, B.; Lu, H.; Kwilas, S.A. Matrix-M adjuvant enhances antibody, cellular and protective immune responses of a Zaire Ebola/Makona virus glycoprotein (GP) nanoparticle vaccine in mice. Vaccine 2016, 34, 1927–1935. [Google Scholar] [CrossRef] [Green Version]
- Pérez-Girón, J.V.; Alan, B.V.; Ebrahim, H.; Sergio, G.M.; Cruz, J.L.G.; Anja, L.; Paula, R.; Albrecht, R.A.; Adolfo, G.S.; César, M.O.F. Mucosal polyinosinic-polycytidylic acid improves protection elicited by replicating influenza vaccines via enhanced dendritic cell function and T cell immunity. J. Immunol. 2014, 193, 1324–1332. [Google Scholar] [CrossRef]
- Audouy, S.A.L.; Saskia, V.S.; Roosmalen, M.L.; van Eduard, P.; Rolf, K.; Jolanda, N.; Silvia, E.O.; Nieuwenhuis, E.E.S.; Adrian, P.V.; Kees, L. Development of lactococcal GEM-based pneumococcal vaccines. Vaccine 2007, 25, 2497–2506. [Google Scholar] [CrossRef]
- Saluja, V.; Visser, M.R.; Ter Veer, W.; Roosmalen, M.L.; van Leenhouts, K.; Hinrichs, W.L.J.; Huckriede, A.; Frijlink, H.W. Influenza antigen-sparing by immune stimulation with Gram-positive enhancer matrix (GEM) particles. Vaccine 2010, 28, 7963–7969. [Google Scholar] [CrossRef]
- Saluja, V.; Amorij, J.P.; Roosmalen, M.L.V.; Leenhouts, K.; Huckriede, A.; Hinrichs, W.L.J.; Frijlink, H.W. Intranasal Delivery of Influenza Subunit Vaccine Formulated with GEM Particles as an Adjuvant. Aaps J. 2010, 12, 109–116. [Google Scholar] [CrossRef] [Green Version]
- Florence, B.; Mensink, R.P.; Karin, V.D.H.; Adriaan, D.; Jogchum, P. TLR2 activation is essential to induce a Th1 shift in human peripheral blood mononuclear cells by plant stanols and plant sterols. J. Biol. Chem. 2010, 285, 2951–2958. [Google Scholar]
- Qiu, X.; Lisa, F.; Alimonti, J.B.; Leno, M.P.; Friedericke, F.; Daryl, D.; Ute, S.; Heinz, F.; Jones, S.M.; Derya, U. Mucosal Immunization of Cynomolgus Macaques with the VSVΔG/ZEBOVGP Vaccine Stimulates Strong Ebola GP-Specific Immune Responses. PLoS ONE 2009, 4, e5547. [Google Scholar] [CrossRef]
- Shoufeng, R.; Qimei, W.; Liya, C.; Xuejing, Y.; Cuicui, X.; Feng, T.; Leavenworth, J.W.; Liang, S.; Liu, W. Alphavirus Replicon DNA Vectors Expressing Ebola GP and VP40 Antigens Induce Humoral and Cellular Immune Responses in Mice. Front. Microbiol. 2018, 8, 2662. [Google Scholar]
- Choi, J.H.; Schafer, S.C.; Zhang, L.; Kobinger, G.P.; Juelich, T.; Freiberg, A.N.; Croyle, M.A. A Single Sublingual Dose of an Adenovirus-Based Vaccine Protects against Lethal Ebola Challenge in Mice and Guinea Pigs. Mol. Pharm. 2012, 9, 156–167. [Google Scholar] [CrossRef] [Green Version]
- Lai, C.Y.; Strange, D.P.; Wong, T.A.; Lehrer, A.T.; Verma, S. Ebola Virus Glycoprotein Induces an Innate Immune Response In vivo via TLR4. Front. Microbiol. 2017, 8, 1571. [Google Scholar] [CrossRef] [Green Version]
- Callendret, B.; Vellinga, J.; Wunderlich, K.; Rodriguez, A.; Steigerwald, R.; Dirmeier, U.; Cheminay, C.; Volkmann, A.; Brasel, T.; Carrion, R. A prophylactic multivalent vaccine against different filovirus species is immunogenic and provides protection from lethal infections with Ebolavirus and Marburgvirus species in non-human primates. PLoS ONE 2018, 13, e0192312. [Google Scholar]
- Ibrahim, E.S.; Gamal, W.M.; Hassan, A.I.; Mahdy, E.D.; Hegazy, A.Z.; Abdel-Atty, M.M. Comparative study on the immunopotentiator effect of ISA 201, ISA 61, ISA 50, ISA 206 used in trivalent foot and mouth disease vaccine. Vet. World 2015, 8, 1189–1198. [Google Scholar] [CrossRef]
- Thomas, M.; Wang, Z.; Sreenivasan, C.C.; Hause, B.M.; Renukaradhya, G.J.; Li, F.; Francis, D.H.; Kaushik, R.S.; Khatri, M. Poly I:C adjuvanted inactivated swine influenza vaccine induces heterologous protective immunity in pigs. Vaccine 2015, 33, 542–548. [Google Scholar] [CrossRef]
- Mcnally, B.; Willette, M.; Ye, F.; Partidasanchez, S.; Flaño, E. Intranasal Administration of dsRNA Analog Poly(I:C) Induces Interferon-α Receptor-Dependent Accumulation of Antigen Experienced T Cells in the Airways. PLoS ONE 2012, 7, e51351. [Google Scholar] [CrossRef] [Green Version]
- Marzi, A.; Engelmann, F.; Feldmann, F.; Haberthur, K.; Shupert, W.L.; Brining, D.; Scott, D.P.; Geisbert, T.W.; Kawaoka, Y.; Katze, M.G. Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc. Natl. Acad. Sci. USA 2013, 110, 1893–1898. [Google Scholar] [CrossRef] [Green Version]
- Mehrizi, A.A.; Rezvani, N.; Zakeri, S.; Gholami, A.; Babaeekhou, L. Poly(I:C) adjuvant strongly enhances parasite-inhibitory antibodies and Th1 response against Plasmodium falciparum merozoite surface protein-1 (42-kDa fragment) in BALB/c mice. Med. Microbiol. Immunol. 2018, 207, 1–16. [Google Scholar] [CrossRef]
- Jang, S.I.; Lillehoj, H.S.; Lee, S.H.; Lee, K.W.; Park, M.S.; Bauchan, G.R.; Lillehoj, E.P.; Bertrand, F.; Dupuis, L.; Deville, S. Immunoenhancing effects of Montanide ISA oil-based adjuvants on recombinant coccidia antigen vaccination against Eimeria acervulina infection. Vet. Parasitol. 2010, 172, 221–228. [Google Scholar] [CrossRef]
- Darryl, F.; Geisbert, T.W.; Heinz, F. Progress in filovirus vaccine development: Evaluating the potential for clinical use. Expert Rev. Vaccines 2011, 10, 63–77. [Google Scholar]
- Gary, W.; Richardson, J.S.; Stéphane, P.; Ami, P.; Xiangguo, Q.; Judie, A.; Jeff, H.; Yi, Z.; Ayato, T.; Heinz, F. Immune parameters correlate with protection against ebola virus infection in rodents and nonhuman primates. Sci. Transl. Med. 2012, 4, 158ra146. [Google Scholar]
- Gary, W.; Kobinger, G.P.; Xiangguo, Q. Characterization of host immune responses in Ebola virus infections. Expert Rev. Clin. Immunol. 2014, 10, 781–790. [Google Scholar]
- Gai, W.; Zheng, X.; Wang, C.; Wang, H.; Zhao, Y.; Wang, Q.; Wong, G.; Zhang, W.; Feng, N.; Qiu, B. Marburg virus-like particles by co-expression of glycoprotein and matrix protein in insect cells induces immune responses in mice. Virol. J. 2017, 14, 204. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Primer | Sequence (5’–3’) | Restriction Enzyme Site |
|---|---|---|
| eGP F 1 | CTTACATCTATGCGGCCGCTTCTAGAATGCTACTAGTAAATCAGTCACACCA | XbaI |
| Linker-eGP R | ACCAGAACCACCACCAGAACCACCACGCCAGCCAGTCCACCAATTATCAT | - |
| Linker-PA F 2 | GGTGGTTCTGGTGGTGGTTCTGGTGATGGTGCTTCTTCAG | - |
| Linker-PA R 1 | TAGTACTTCTCGACAAGCTTGGTACCTTACTTGATACGCAGGTATTGACCGATC | KpnI |
| Group | n | Immunization Route | Antigen | Adjuvant |
|---|---|---|---|---|
| SBLP + 2 + P | 8 | intramuscular | 10 μg eGP-PA-GEM | 201VG + Poly(I:C) |
| SBLP + 201 | 8 | intramuscular | 10 μg eGP-PA-GEM | 201VG |
| SBLP + PolyI:C | 8 | intramuscular | 10 μg eGP-PA-GEM | Poly (I:C) |
| SBLP + Alum | 8 | intramuscular | 10 μg eGP-PA-GEM | Alum |
| SBLP | 8 | Intramuscular | 10 μg eGP-PA-GEM | - |
| GEM | 8 | intramuscular | GEM | - |
| PBS | 8 | intramuscular | PBS | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, S.; Jiao, C.; Jin, H.; Li, W.; Li, E.; Cao, Z.; Shi, Z.; Yan, F.; Zhang, S.; He, H.; et al. A Novel Bacterium-Like Particle-Based Vaccine Displaying the SUDV Glycoprotein Induces Potent Humoral and Cellular Immune Responses in Mice. Viruses 2019, 11, 1149. https://doi.org/10.3390/v11121149
Xu S, Jiao C, Jin H, Li W, Li E, Cao Z, Shi Z, Yan F, Zhang S, He H, et al. A Novel Bacterium-Like Particle-Based Vaccine Displaying the SUDV Glycoprotein Induces Potent Humoral and Cellular Immune Responses in Mice. Viruses. 2019; 11(12):1149. https://doi.org/10.3390/v11121149
Chicago/Turabian StyleXu, Shengnan, Cuicui Jiao, Hongli Jin, Wujian Li, Entao Li, Zengguo Cao, Zhikang Shi, Feihu Yan, Shengnan Zhang, Hongbin He, and et al. 2019. "A Novel Bacterium-Like Particle-Based Vaccine Displaying the SUDV Glycoprotein Induces Potent Humoral and Cellular Immune Responses in Mice" Viruses 11, no. 12: 1149. https://doi.org/10.3390/v11121149
APA StyleXu, S., Jiao, C., Jin, H., Li, W., Li, E., Cao, Z., Shi, Z., Yan, F., Zhang, S., He, H., Chi, H., Feng, N., Zhao, Y., Gao, Y., Yang, S., Wang, J., Wang, H., & Xia, X. (2019). A Novel Bacterium-Like Particle-Based Vaccine Displaying the SUDV Glycoprotein Induces Potent Humoral and Cellular Immune Responses in Mice. Viruses, 11(12), 1149. https://doi.org/10.3390/v11121149