A Model for the Production of Regulatory Grade Viral Hemorrhagic Fever Exposure Stocks: From Field Surveillance to Advanced Characterization of SFTSV
Abstract
:1. Introduction
2. Materials and Methods
2.1. Human SFTS Case
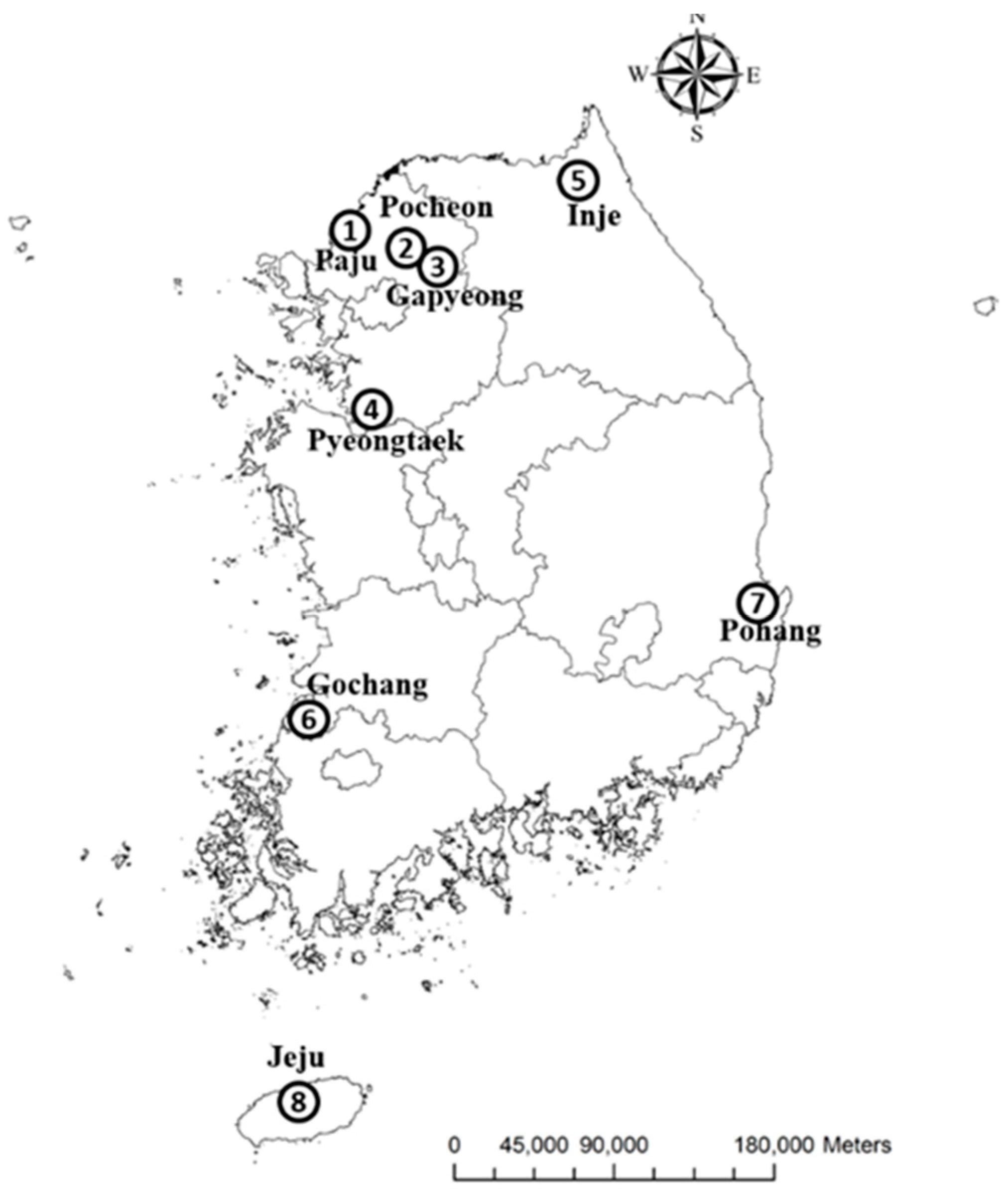
2.2. Tick Specimens
2.3. SFTSV Detection by Molecular Assays
2.4. Viral Isolation and Characterization
2.4.1. Viral Isolation and Titration
2.4.2. Transmission Electron Microscopy
2.4.3. Immunofluorescence Microscopy
2.5. Target-Enrichment Whole-Genome Sequencing
2.6. Genomic Characterization
2.7. Phylogenetic Analysis and Haplotype Network
2.8. IFNAR-/- Mice Infections
3. Results
3.1. Detection of SFTSV in Ticks
3.2. Isolation and Characterization of the SFTS Virus from the Tick Pool
3.2.1. Viral isolation and Titration in Vero E6 Cells
3.2.2. SFTSV Particles Co-Located with the Golgi Apparatus in Vero E6 Cells
3.3. Target-Enrichment Whole-Genome Sequencing
3.4. Phylogenetic Analysis
3.5. Genomic Analysis
3.6. Lethality in IFNAR-/- Mice
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kuhn, J.H.; Adkins, S.; Alioto, D.; Alkhovsky, S.V.; Amarasinghe, G.; Anthony, S.J.; Avšič-Županc, T.; Ayllón, M.A.; Bahl, J.; Balkema-Buschmann, A.; et al. 2020 Taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the lathe orders Bunyavirales and Mononegavirales. Arch. Virol. 2020, in press. [Google Scholar]
- Yu, X.-J.; Liang, M.-F.; Zhang, S.-Y.; Liu, Y.; Li, J.D.; Sun, Y.-L.; Zhang, L.; Zhang, Q.-F.; Popov, V.L.; Li, C.; et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N. Engl. J. Med. 2011, 364, 1523–1532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silvas, J.A.; Aguilar, P.V. The emergence of severe fever with thrombocytopenia syndrome virus. Am. J. Trop. Med. Hyg. 2017, 97, 992–996. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.-H.; Yi, J.; Kim, G.; Choi, S.J.; Jun, K.I.; Kim, N.-H.; Choe, P.G.; Kim, N.-J.; Lee, J.-K.; Oh, M.-D. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerg. Infect. Dis. 2013, 19, 1892–1894. [Google Scholar] [CrossRef] [PubMed]
- Takhampunya, R.; Kim, H.-C.; Chong, S.-T.; Korkusol, A.; Tippayachai, B.; Davidson, S.A.; Petersen, J.M.; Klein, T.A. Francisella-like endosymbiont detected in Haemaphysalis ticks (Acari: Ixodidae) from the Republic of Korea. J. Med. Entomol. 2017, 54, 1735–1742. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.-L.; Ou, S.-C.; Maeda, K.; Shimoda, H.; Chan, J.P.-W.; Tu, W.-C.; Hsu, W.-L.; Chou, C.-C. The first discovery of severe fever with thrombocytopenia syndrome virus in Taiwan. Emerg. Microbes Infect. 2020, 9, 148–151. [Google Scholar] [CrossRef]
- Takahashi, T.; Maeda, K.; Suzuki, T.; Ishido, A.; Shigeoka, T.; Tominaga, T.; Kamei, T.; Honda, M.; Ninomiya, D.; Sakai, T.; et al. The first identification and retrospective study of severe fever with thrombocytopenia syndrome in Japan. J. Infect. Dis. 2014, 209, 816–827. [Google Scholar] [CrossRef]
- Tran, X.C.; Yun, Y.; Van An, L.; Kim, S.-H.; Thao, N.T.P.; Man, P.K.C.; Yoo, J.R.; Heo, S.T.; Cho, N.-H.; Lee, K.H. Endemic severe fever with thrombocytopenia syndrome, Vietnam. Emerg. Infect. Dis. 2019, 25, 1029–1031. [Google Scholar] [CrossRef]
- Meng, K.; Sun, W.; Cheng, Z.; Guo, H.; Liu, J.; Chai, T. First detection of severe fever with thrombocytopenia syndrome virus in the tick species Haemaphysalis concinna in Shandong Province, China. Parasitol. Res. 2015, 114, 4703–4707. [Google Scholar] [CrossRef]
- Yun, S.-M.; Lee, Y.-J.; Choi, W.; Kim, H.-C.; Chong, S.-T.; Chang, K.-S.; Coburn, J.M.; Klein, T.A.; Lee, W.-J. Molecular detection of severe fever with thrombocytopenia syndrome and tick-borne encephalitis viruses in ixodid ticks collected from vegetation, Republic of Korea, 2014. Ticks Tick Borne Dis. 2016, 7, 970–978. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.-Z.; He, Y.-W.; Dai, Y.-A.; Xiong, Y.; Zheng, H.; Zhou, D.-J.; Li, J.; Sun, Q.; Luo, X.-L.; Cheng, Y.-L.; et al. Hemorrhagic fever caused by a novel bunyavirus in China: Pathogenesis and correlates of fatal outcome. Clin. Infect. Dis. 2012, 54, 527–533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhuang, L.; Sun, Y.; Cui, X.-M.; Tang, F.; Hu, J.-G.; Wang, L.-Y.; Cui, N.; Yang, Z.-D.; Huang, D.-D.; Zhang, X.-A.; et al. Transmission of severe fever with thrombocytopenia syndrome virus by Haemaphysalis longicornis ticks, China. Emerg. Infect. Dis. 2018, 24, 868–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gai, Z.; Liang, M.; Zhang, Y.; Zhang, S.; Jin, C.; Wang, S.-W.; Sun, L.; Zhou, N.; Zhang, Q.; Sun, Y.; et al. Person-to-person transmission of severe fever with thrombocytopenia syndrome bunyavirus through blood contact. Clin. Infect. Dis. 2012, 54, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Zhai, S.; Wen, H.; Cui, F.; Chi, Y.; Wang, L.; Xue, F.; Wang, Q.; Wang, Z.; Zhang, S.; et al. Severe fever with thrombocytopenia syndrome virus, Shandong Province, China. Emerg. Infect. Dis. 2012, 18, 963–965. [Google Scholar] [CrossRef]
- Niu, G.; Li, J.; Liang, M.; Jiang, X.; Jiang, M.; Yin, H.; Wang, Z.; Li, C.; Zhang, Q.; Jin, C.; et al. Severe fever with thrombocytopenia syndrome virus among domesticated animals, China. Emerg. Infect. Dis. 2013, 19, 756–763. [Google Scholar] [CrossRef]
- Park, E.-S.; Shimojima, M.; Nagata, N.; Ami, Y.; Yoshikawa, T.; Iwata-Yoshikawa, N.; Fukushi, S.; Watanabe, S.; Kurosu, T.; Kataoka, M.; et al. Severe fever with thrombocytopenia syndrome phlebovirus causes lethal viral hemorrhagic fever in cats. Sci. Rep. 2019, 9, 11990. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.-W.; Wen, H.-L.; Fang, L.-Z.; Zhang, Z.-T.; He, S.-T.; Xue, Z.-F.; Ma, D.-Q.; Zhang, X.-S.; Wang, T.; Yu, H.; et al. Prevalence of SFTSV among Asian house shrews and rodents, China, January-August 2013. Emerg. Infect. Dis. 2014, 20, 2126–2128. [Google Scholar] [CrossRef]
- Chen, C.; Li, P.; Li, K.-F.; Wang, H.-L.; Dai, Y.-X.; Cheng, X.; Yan, J.-B. Animals as amplification hosts in the spread of severe fever with thrombocytopenia syndrome virus: A systematic review and meta-analysis. Int. J. Infect. Dis. 2019, 79, 77–84. [Google Scholar] [CrossRef] [Green Version]
- Xing, X.; Guan, X.; Liu, L.; Zhan, J.; Jiang, H.; Liu, L.; Li, G.; Xiong, J.; Tan, L.; Xu, J.; et al. Natural transmission model for severe fever with thrombocytopenia syndrome bunyavirus in villages of Hubei Province, China. Medicine 2016, 95, e2533. [Google Scholar] [CrossRef]
- Liu, Q.; He, B.; Huang, S.-Y.; Wei, F.; Zhu, X.-Q. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect. Dis. 2014, 14, 763–772. [Google Scholar] [CrossRef]
- Lv, Q.; Zhang, H.; Tian, L.; Zhang, R.; Zhang, Z.; Li, J.; Tong, Y.; Fan, H.; Carr, M.J.; Shi, W. Novel sub-lineages, recombinants and reassortants of severe fever with thrombocytopenia syndrome virus. Ticks Tick Borne Dis. 2017, 8, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.T.; Kim, H.C.; Lee, I.-Y.; Kollars, T.M., Jr.; Sancho, A.R.; Sames, W.J.; Chae, J.-S.; Klein, T.A. Seasonal distribution of ticks in four habitats near the demilitarized zone, Gyeonggi-do (Province), Republic of Korea. Korean J. Parasitol. 2013, 51, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.T.; Kim, H.C.; Lee, I.-Y.; Kollars, T.M., Jr.; Sancho, A.R.; Sames, W.J.; Klein, T.A. Comparison of dragging and sweeping methods for collecting ticks and determining their seasonal distributions for various habitats, Gyeonggi Province, Republic of Korea. J. Med. Entomol. 2013, 50, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Coburn, J.M.; Chong, S.-T.; Kim, H.-C.; Chang, N.W.; Calix, L.C.; Resto, K.; Lee, D.-J.; Johnson, J.L.; Robbins, R.G.; Klein, T.A. Tick surveillance in four southwestern provinces of the Republic of Korea during 2013. Syst. Appl. Acarol. 2016, 21, 147–165. [Google Scholar]
- Johnson, J.L.; Kim, H.-C.; Coburn, J.M.; Chong, S.-T.; Chang, N.W.; Robbins, R.G.; Klein, T.A. Tick surveillance in two southeastern provinces, including three metropolitan areas, of the Republic of Korea during 2014. Syst. Appl. Acarol. 2017, 22, 271–288. [Google Scholar]
- Sun, Y.; Liang, M.; Qu, J.; Jin, C.; Zhang, Q.; Li, J.; Jiang, X.; Wang, Q.; Lu, J.; Gu, W.; et al. Early diagnosis of novel SFTS bunyavirus infection by quantitative real-time RT-PCR assay. J. Clin. Virol. 2012, 53, 48–53. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Liu, J.; Kline, B.A.; Kenny, T.A.; Smith, D.R.; Soloveva, V.; Beitzel, B.; Pang, S.; Lockett, S.; Hess, H.F.; Palacios, G.; et al. A novel sheet-like virus particle array is a hallmark of Zika virus infection. Emerg. Microbes Infect. 2018, 7, 69. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, E.S. The use of lead citrate at high pH as an electron-opaque stain in electron microscopy. J. Cell Biol. 1963, 17, 208–212. [Google Scholar] [CrossRef] [Green Version]
- Mate, S.E.; Kugelman, J.R.; Nyenswah, T.G.; Ladner, J.T.; Wiley, M.R.; Cordier-Lassalle, T.; Christie, A.; Schroth, G.P.; Gross, S.M.; Davies-Wayne, G.J.; et al. Molecular evidence of sexual transmission of Ebola virus. N. Engl. J. Med. 2015, 373, 2448–2454. [Google Scholar] [CrossRef] [Green Version]
- Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet.journal 2011, 17, 10–12. [Google Scholar] [CrossRef]
- Schmieder, R.; Edwards, R. Quality control and preprocessing of metagenomic datasets. Bioinformatics 2011, 27, 863–864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ladner, J.T.; Wiley, M.R.; Mate, S.; Dudas, G.; Prieto, K.; Lovett, S.; Nagle, E.R.; Beitzel, B.; Gilbert, M.L.; Fakoli, L.; et al. Evolution and spread of Ebola virus in Liberia, 2014–2015. Cell Host Microbe 2015, 18, 659–669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langmead, B.; Salzberg, S.L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R. 1000 Genome Project Data Processing Subgroup, The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef] [Green Version]
- Edgar, R.C. MUSCLE: Multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res. 2004, 32, 1792–1797. [Google Scholar] [CrossRef] [Green Version]
- Kugelman, J.R.; Wiley, M.R.; Nagle, E.R.; Reyes, D.; Pfeffer, B.P.; Kuhn, J.H.; Sanchez-Lockhart, M.; Palacios, G.F. Error baseline rates of five sample preparation methods used to characterize RNA virus populations. PLoS ONE 2017, 12, e0171333. [Google Scholar] [CrossRef]
- Yun, S.-M.; Park, S.-J.; Kim, Y.-I.; Park, S.-W.; Yu, M.-A.; Kwon, H.-I.; Kim, E.-H.; Yu, K.-M.; Jeong, H.W.; Ryou, J.; et al. Genetic and pathogenic diversity of severe fever with thrombocytopenia syndrome virus (SFTSV) in South Korea. JCI Insight 2020, 5, e129531. [Google Scholar] [CrossRef] [Green Version]
- Katoh, K.; Standley, D.M. MAFFT multiple sequence alignment software version 7: Improvements in performance and usability. Mol. Biol. Evol. 2013, 30, 772–780. [Google Scholar] [CrossRef] [Green Version]
- Price, M.N.; Dehal, P.S.; Arkin, A.P. FastTree 2—Approximately maximum-likelihood trees for large alignments. PLoS ONE 2010, 5, e9490. [Google Scholar] [CrossRef]
- Hasegawa, M.; Kishino, H.; Yano, T. Dating of the human-ape splitting by a molecular clock of mitochondrial DNA. J. Mol. Evol. 1985, 22, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Lanave, C.; Preparata, G.; Saccone, C.; Serio, G. A new method for calculating evolutionary substitution rates. J. Mol. Evol. 1984, 20, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Darriba, D.; Taboada, G.L.; Doallo, R.; Posada, D. jModelTest 2: More models, new heuristics and parallel computing. Nat. Methods 2012, 9, 772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferreira, M.A.R.; Suchard, M.A. Bayesian analysis of elapsed times in continuous-time Markov chains. Can. J. Stat. 2008, 36, 355–368. [Google Scholar] [CrossRef]
- Rambaut, A.; Drummond, A.J.; Xie, D.; Baele, G.; Suchard, M.A. Posterior summarization in Bayesian phylogenetics using Tracer 1.7. Syst. Biol. 2018, 67, 901–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drummond, A.J.; Rambaut, A. BEAST: Bayesian evolutionary analysis by sampling trees. BMC Evol. Biol. 2007, 7, 214. [Google Scholar] [CrossRef] [Green Version]
- Lundu, T.; Tsuda, Y.; Ito, R.; Shimizu, K.; Kobayashi, S.; Yoshii, K.; Yoshimatsu, K.; Arikawa, J.; Kariwa, H. Targeting of severe fever with thrombocytopenia syndrome virus structural proteins to the ERGIC (endoplasmic reticulum Golgi intermediate compartment) and Golgi complex. Biomed. Res. 2018, 39, 27–38. [Google Scholar] [CrossRef] [Green Version]
- Plegge, T.; Hofmann-Winkler, H.; Spiegel, M.; Pöhlmann, S. Evidence that processing of the severe fever with thrombocytopenia syndrome virus Gn/Gc polyprotein is critical for viral infectivity and requires an internal Gc signal peptide. PLoS ONE 2016, 11, e0166013. [Google Scholar] [CrossRef]
- Brennan, B.; Li, P.; Zhang, S.; Li, A.; Liang, M.; Li, D.; Elliott, R.M. Reverse genetics system for severe fever with thrombocytopenia syndrome virus. J. Virol. 2015, 89, 3026–3037. [Google Scholar] [CrossRef] [Green Version]
- Tani, H.; Fukuma, A.; Fukushi, S.; Taniguchi, S.; Yoshikawa, T.; Iwata-Yoshikawa, N.; Sato, Y.; Suzuki, T.; Nagata, N.; Hasegawa, H.; et al. Efficacy of T-705 (favipiravir) in the treatment of infections with lethal severe fever with thrombocytopenia syndrome virus. mSphere 2016, 1, e00061-15. [Google Scholar] [CrossRef] [Green Version]





| Taxonomy | Larvae | Nymph | Adults | Total | |
|---|---|---|---|---|---|
| Asian longhorned ticks (Haemaphysalis longicornis Neumann, 1901) | 4776 | 8214 | 57 | 13,047 | |
| Haemaphysalis flava Neumann, 1897 | 68 | 250 | 78 | 396 | |
| Ixodes nipponensis Kitaoka and Saito, 1967 | 0 | 10 | 130 | 140 | |
| Haemaphysalis phasiana Saito, Hoogstraal and Wassef, 1974 | 17 | 35 | 0 | 52 | |
| Brown dog tick (Rhipicephalus sanguineus (Latreille, 1806)) | 0 | 0 | 1 | 1 | |
| Total specimens | 4861 | 8509 | 266 | 13,636 | |
| Pools | 186 | 445 | 95 | 726 |
| Genome Segment | Primer | Primer/Probe Sequence 5′-3′ |
|---|---|---|
| L | L-F-3-mod | AGTCTAGGTCATCTGAYCCGTTYAG |
| L-R-3 | TGTAAGTTCGCCCTTTGTCCAT | |
| L-Probe-3-mod | [HEX] CAATGACAGAYGCCTTCCATGGTAATAGGG [BHQ1] | |
| M | M-F-3-mod | AAG AAR TGG YTG TTC ATC ATT ATT G |
| M-R-3-mod | GCC TTR AGR ACA TTG GTG AGY A | |
| M-Probe-3-mod | [FAM] TCA TCC TCC TTG GRT ATG CAG GCC TCA [BHQ1] | |
| S | S-F-3-mod | GGRTCCCTGAAGGAGTTRTAAA |
| S-R-3-mod | TGCCTTCACCAAGACYATCAATGT | |
| S-Probe-3-mod | [TexasRed] YTCTGTCTTGCTRGCTCCRCGC [BHQ-2] |
| Strains | AMFC 17-1 | USAMRIID-HLP23 | USAMRIID-HLP23_VE6 | |
|---|---|---|---|---|
| L segment | AMFC 17-1 | - | 99.89 (7) | 99.92 (5) |
| USAMRIID-HLP23 | 99.9 (2) | - | 99.97 (2) | |
| USAMRIID-HLP23_VE6 | 99.95 (1) | 99.95 (1) | - | |
| M segment | AMFC 17-1 | - | 99.79 (7) | 99.79 (7) |
| USAMRIID-HLP23 | 99.72 (3) | - | 100 | |
| USAMRIID-HLP23_VE6 | 99.72 (3) | 100 | - | |
| S segment | AMFC 17-1 | - | 99.77 (4) | 99.83 (3) |
| USAMRIID-HLP23 | 99.81 (1) | - | 99.94 (1) | |
| USAMRIID-HLP23_VE6 | 99.81 (1) | 100 | - |
| Consensus Changes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Position nt | Segment | Position aa | Protein | Tick | Vero E6 | Human | ||||||
| Base | Freq. | Codon | Base | Freq. | Codon | Base | Freq. | Codon | ||||
| 1287 | L | 424 | L | T | 97.4 | F (TTT) | C | 98.6 | S (TCT) | C | 99.7 | S (TCT) |
| 2329 | 771 | T | 100 | Y (TAT) | T | 99.9 | Y (TAT) | C | 99.8 | Y (TAC) | ||
| 3070 | 1018 | A | 100 | I (ATA) | A | 99.9 | I (ATA) | T | 99.9 | I (ATT) | ||
| 3574 | 1186 | C * | 100 * | H (CAC) | C | 99.9 | H (CAC) | T | 99.9 | H (CAT) | ||
| 4170 | 1385 | G | 92.7 | R (AGA) | G | 88.8 | R (AGA) | A | 99.9 | K (AAA) | ||
| 6088 | 2024 | A | 100 | A (GCA) | A | 99.9 | A (GCA) | G | 99.6 | A (GCG) | ||
| 6275 | NC | NC | A | 98.1 | NC | T | 99.8 | NC | T | 99.9 | NC | |
| 40 | M | 8 | GP | A * | 100 * | T (ACC) | A | 99.9 | T (ACC) | T | 100 | S (TCC) |
| 63 | 15 | T | 100 | I (ATT) | T | 99.9 | I (ATT) | C | 100 | I (ATC) | ||
| 564 | 182 | T | 100 | P (CCT) | T | 99.9 | P (CCT) | C | 99.6 | P (CCC) | ||
| 573 | 185 | T | 100 | P (CCT) | T | 99.9 | P (CCT) | C | 97.8 | P (CCC) | ||
| 1291 | 425 | T | 66.4 | L (TTG) | T | 88.4 | L (TTG) | A | 99.9 | M (ATG) | ||
| 1951 | 645 | G * | 100 * | A (GCA) | G | 99.9 | A (GCA) | A | 99.9 | T (ACA) | ||
| 3237 | 1073 | A | 100 | A (GCA) | A | 99.9 | A (GCA) | T | 99.9 | A (GCT) | ||
| 280 | S | 84 | NS | G | 97.1 | C (TGC) | G | 88.4 | C (TGC) | A | 99.9 | Y (TAC) |
| 716 | 229 | T | 100 | D (GAT) | T | 99.9 | D (GAT) | C | 99.9 | D (GAC) | ||
| 860 | 277 | C | 100 | T (ACC) | C | 99.9 | T (ACC) | A | 100 | T (ACA) | ||
| 1455 | 83 | NP | T | 80.1 | L (TTA) | C | 99.9 | L (TTG) | C | 99.8 | L (TTG) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perez-Sautu, U.; Gu, S.H.; Caviness, K.; Song, D.H.; Kim, Y.-J.; Paola, N.D.; Lee, D.; Klein, T.A.; Chitty, J.A.; Nagle, E.; et al. A Model for the Production of Regulatory Grade Viral Hemorrhagic Fever Exposure Stocks: From Field Surveillance to Advanced Characterization of SFTSV. Viruses 2020, 12, 958. https://doi.org/10.3390/v12090958
Perez-Sautu U, Gu SH, Caviness K, Song DH, Kim Y-J, Paola ND, Lee D, Klein TA, Chitty JA, Nagle E, et al. A Model for the Production of Regulatory Grade Viral Hemorrhagic Fever Exposure Stocks: From Field Surveillance to Advanced Characterization of SFTSV. Viruses. 2020; 12(9):958. https://doi.org/10.3390/v12090958
Chicago/Turabian StylePerez-Sautu, Unai, Se Hun Gu, Katie Caviness, Dong Hyun Song, Yu-Jin Kim, Nicholas Di Paola, Daesang Lee, Terry A. Klein, Joseph A. Chitty, Elyse Nagle, and et al. 2020. "A Model for the Production of Regulatory Grade Viral Hemorrhagic Fever Exposure Stocks: From Field Surveillance to Advanced Characterization of SFTSV" Viruses 12, no. 9: 958. https://doi.org/10.3390/v12090958





