Association between Maternal Non-Coding Interferon-λ Polymorphisms and Congenital Zika Syndrome in a Cohort from Brazilian Northeast
Abstract
:1. Introduction
2. Materials and Methods
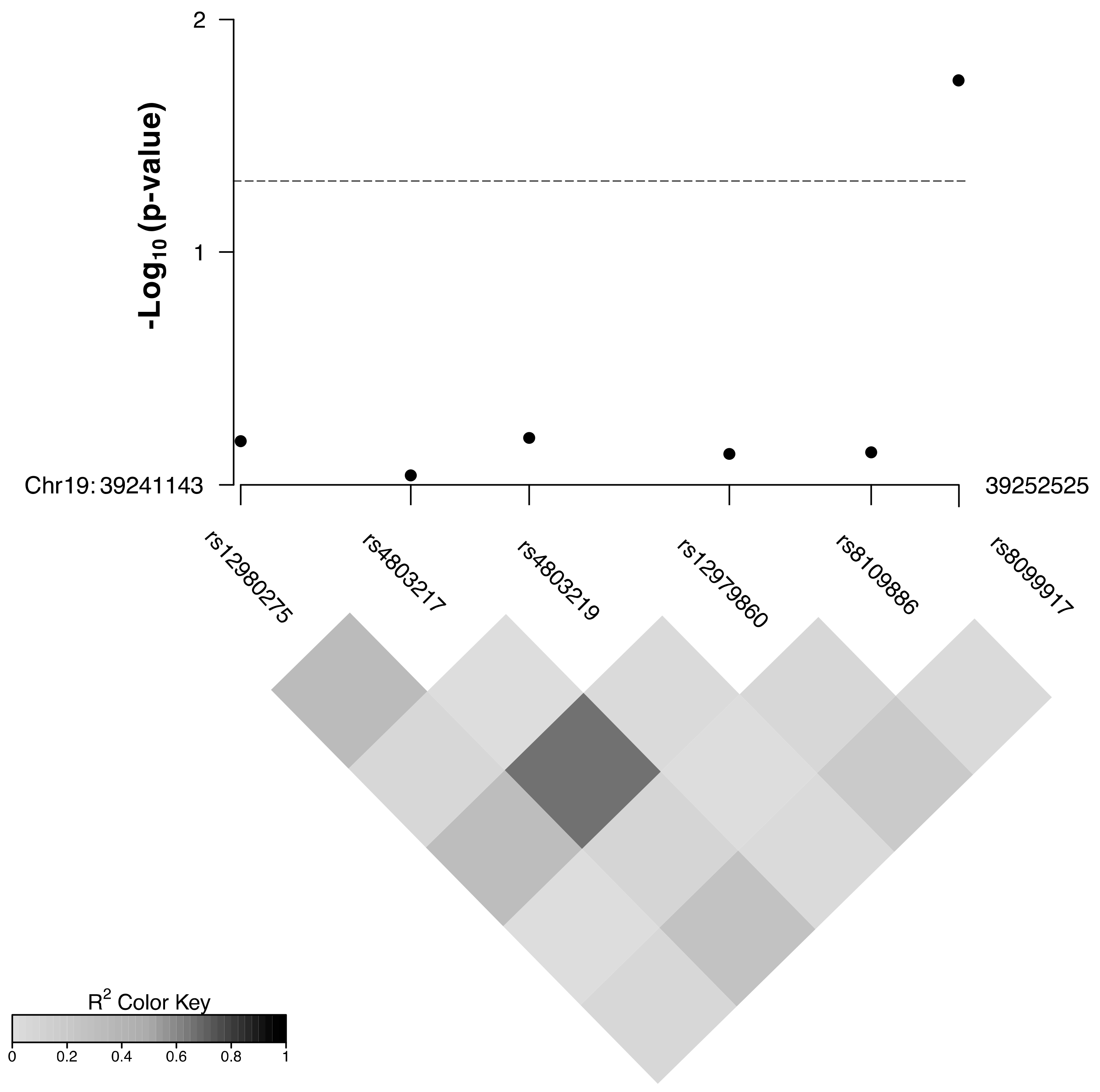
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hołda, M.K.; Klimek-Piotrowska, W.; Hołda, J.; Providência, R.; Lambiase, P.D.; Marijon, E.; Zipursky, J.S.; Shadowitz, S.; Kuck, K.; Brugada, J.; et al. Cryoballoon or Radiofrequency Ablation for Atrial Fibrillation. N. Engl. J. Med. 2016, 375, 1099–1101. [Google Scholar] [CrossRef] [Green Version]
- Brasil, P.; Pereira, J.P.; Moreira, M.E.; Nogueira, R.M.R.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.-A.; Salles, T.S.; et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N. Engl. J. Med. 2016, 375, 2321–2334. [Google Scholar] [CrossRef] [PubMed]
- Cao-Lormeau, V.-M.; Blake, A.; Mons, S.; Lastère, S.; Roche, C.; Vanhomwegen, J.; Dub, T.; Baudouin, L.; Teissier, A.; Larre, P.; et al. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: A case-control study. Lancet 2016, 387, 1531–1539. [Google Scholar] [CrossRef] [Green Version]
- Melo, A.S.D.O.; Aguiar, R.; Amorim, M.; Arruda, M.B.; Melo, F.D.O.; Ribeiro, S.T.C.; Batista, A.G.M.; Ferreira, T.; Dos Santos, M.P.; Sampaio, V.V.; et al. Congenital Zika Virus Infection. JAMA Neurol. 2016, 73, 1407–1416. [Google Scholar] [CrossRef] [PubMed]
- Junior, H.V.D.L.; Goulart, E.; Melo, U.S.; Araujo, B.H.S.; Alvizi, L.; Schanoski, A.S.; De Oliveira, D.F.; Kobayashi, G.; Griesi-Oliveira, K.; Musso, C.M.; et al. Discordant congenital Zika syndrome twins show differential in vitro viral susceptibility of neural progenitor cells. Nat. Commun. 2018, 9, 475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi, A.D.; Faucz, F.R.; Melo, A.; Pezzuto, P.; de Azevedo, G.S.; Schamber-Reis, B.L.F.; Tavares, J.S.; Mattapallil, J.J.; Tanuri, A.; Aguiar, R.; et al. Variations in maternal adenylate cyclase genes are associated with congenital Zika syndrome in a cohort from Northeast, Brazil. J. Intern. Med. 2018, 285, 215–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, C.N.; Ribeiro, D.R.; Alves, J.C.; Cazzaniga, R.; Magalhães, L.S.; De Souza, M.S.F.; Fonseca, A.B.L.; Bispo, A.J.B.; Porto, R.L.S.; Dos Santos, C.A.; et al. Association Between Zika Virus Microcephaly in Newborns With the rs3775291 Variant in Toll-Like Receptor 3 and rs1799964 Variant at Tumor Necrosis Factor-α Gene. J. Infect. Dis. 2019, 220, 1797–1801. [Google Scholar] [CrossRef] [PubMed]
- Schneider, W.M.; Chevillotte, M.D.; Rice, C.M. Interferon-Stimulated Genes: A Complex Web of Host Defenses. Annu. Rev. Immunol. 2014, 32, 513–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jagger, B.W.; Miner, J.J.; Cao, B.; Arora, N.; Smith, A.M.; Kovacs, A.; Mysorekar, I.U.; Coyne, C.B.; Diamond, M.S. Gestational Stage and IFN-λ Signaling Regulate ZIKV Infection In Utero. Cell Host Microbe 2017, 22, 366–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, Y.; Nishida, N.; Sugiyama, M.; Kurosaki, M.; Matsuura, K.; Sakamoto, N.; Nakagawa, M.; Korenaga, M.; Hino, K.; Hige, S.; et al. Genome-wide association of IL28B with response to pegylated interferon-α and ribavirin therapy for chronic hepatitis C. Nat. Genet. 2009, 41, 1105–1109. [Google Scholar] [CrossRef] [PubMed]
- Sakhaee, F.; Ghazanfari, M.; Vaziri, F.; Jamnani, F.R.; Davari, M.; Gharibzadeh, S.; Fateh, R.; Abdolrahimi, F.; Dizaji, S.P.; Fateh, A.; et al. The impact of genetic variation in IL28B, IFNL4 and HLA genes on treatment responses against chronic hepatitis C virus infection. Infect. Genet. Evol. 2017, 54, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, S.J.; Koegl, M.; Boutell, C.; Zenner, H.L.; Crump, C.; Pica, F.; Gonzalez, O.; Friedel, C.C.; Barry, G.; Martin, K.; et al. A Systematic Analysis of Host Factors Reveals a Med23-Interferon-λ Regulatory Axis against Herpes Simplex Virus Type 1 Replication. PLOS Pathog. 2013, 9, e1003514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manuel, O.; Wojtowicz, A.; Bibert, S.; Mueller, N.J.; Van Delden, C.; Hirsch, H.H.; Steiger, J.; Stern, M.; Egli, A.; Garzoni, C.; et al. Influence of IFNL3/4 Polymorphisms on the Incidence of Cytomegalovirus Infection After Solid-Organ Transplantation. J. Infect. Dis. 2014, 211, 906–914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manta, F.S.D.N.; Pereira, R.; Vianna, R.; De Araújo, A.R.B.; Gitaí, D.; Silva, D.; Wolfgramm, E.D.V.; Pontes, I.D.M.; Aguiar, J.I.; Moraes, M.O.; et al. Revisiting the Genetic Ancestry of Brazilians Using Autosomal AIM-Indels. PLoS ONE 2013, 8, e75145. [Google Scholar] [CrossRef]
- Pool, K.-L.; Adachi, K.; Karnezis, S.; Salamon, N.; Romero, T.; Nielsen-Saines, K.; Pone, S.M.; Boechat, M.; Aibe, M.; Da Silva, T.G.; et al. Association between Neonatal Neuroimaging and Clinical Outcomes in Zika-Exposed Infants From Rio de Janeiro, Brazil. JAMA Netw. Open 2019, 2, e198124. [Google Scholar] [CrossRef] [PubMed]
- Lazear, H.; Nice, T.; Diamond, M.S. Interferon-λ: Immune Functions at Barrier Surfaces and Beyond. Immunity 2015, 43, 15–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.-H.; Yang, H.-I.; Lu, S.-N.; Lin, Y.-J.; Jen, C.-L.; Wong, K.-H.; Chan, S.-Y.; Chen, L.-C.; Wang, L.-Y.; L’Italien, G.; et al. Polymorphisms near the IFNL3 Gene Associated with HCV RNA Spontaneous Clearance and Hepatocellular Carcinoma Risk. Sci. Rep. 2015, 5, 17030. [Google Scholar] [CrossRef] [PubMed]
| rs8099917 Genotype | Controls (%) | Cases (%) | OR (95% CI) | OR (95% CI) * |
|---|---|---|---|---|
| T/T | 16 (66.7) | 12 (42.9) | Reference | Reference |
| T/G | 7 (29.2) | 10 (35.7) | 1.90 (0.56–6.46) | 2.04 (0.57–7.38) |
| G/G | 1 (4.2) | 6 (21.4) | 8.00 (0.85–75.86) | 10.01 (1.0–100.47) |
| 24 | 28 | p = 0.09 | p = 0.06 | |
| T/T | 16 (66.7) | 12 (42.9) | Reference | Reference |
| T/G—G/G | 8 (33.3) | 16 (57.1) | 2.67 (0.86–8.27) | 2.98 (0.90–9.88) |
| 24 | 28 | p = 0.08 | p = 0.07 | |
| T/T—T/G | 23 (95.8) | 22 (78.6) | Reference | Reference |
| G/G | 1 (4.2) | 6 (21.4) | 6.27 (0.7–56.4) | 7.47 (0.80–70.24) |
| 24 | 28 | p = 0.05 | p = 0.06 | |
| log-additive (G) | 24 | 28 | 2.41 (1.02–5.71) | 2.80 (1.14–6.91) |
| p = 0.03 | p = 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, Á.D.; Faucz, F.R.; Melo, A.; de Azevedo, G.S.; Pezzuto, P.; Bezerra, O.C.d.L.; Manta, F.S.d.N.; Azamor, T.; Schamber-Reis, B.L.F.; Tanuri, A.; et al. Association between Maternal Non-Coding Interferon-λ Polymorphisms and Congenital Zika Syndrome in a Cohort from Brazilian Northeast. Viruses 2021, 13, 2253. https://doi.org/10.3390/v13112253
Rossi ÁD, Faucz FR, Melo A, de Azevedo GS, Pezzuto P, Bezerra OCdL, Manta FSdN, Azamor T, Schamber-Reis BLF, Tanuri A, et al. Association between Maternal Non-Coding Interferon-λ Polymorphisms and Congenital Zika Syndrome in a Cohort from Brazilian Northeast. Viruses. 2021; 13(11):2253. https://doi.org/10.3390/v13112253
Chicago/Turabian StyleRossi, Átila Duque, Fabio Rueda Faucz, Adriana Melo, Girlene Souza de Azevedo, Paula Pezzuto, Ohanna Cavalcanti de Lima Bezerra, Fernanda Saloum de Neves Manta, Tamiris Azamor, Bruno Luiz Fonseca Schamber-Reis, Amilcar Tanuri, and et al. 2021. "Association between Maternal Non-Coding Interferon-λ Polymorphisms and Congenital Zika Syndrome in a Cohort from Brazilian Northeast" Viruses 13, no. 11: 2253. https://doi.org/10.3390/v13112253
APA StyleRossi, Á. D., Faucz, F. R., Melo, A., de Azevedo, G. S., Pezzuto, P., Bezerra, O. C. d. L., Manta, F. S. d. N., Azamor, T., Schamber-Reis, B. L. F., Tanuri, A., Moraes, M. O., Aguiar, R. S., Stratakis, C. A., & Cardoso, C. C. (2021). Association between Maternal Non-Coding Interferon-λ Polymorphisms and Congenital Zika Syndrome in a Cohort from Brazilian Northeast. Viruses, 13(11), 2253. https://doi.org/10.3390/v13112253







