Hemagglutinin Stability and Its Impact on Influenza A Virus Infectivity, Pathogenicity, and Transmissibility in Avians, Mice, Swine, Seals, Ferrets, and Humans
Abstract
:1. Influenza Virology
2. Molecular Properties Contributing to In Vivo Phenotypes of IAVs
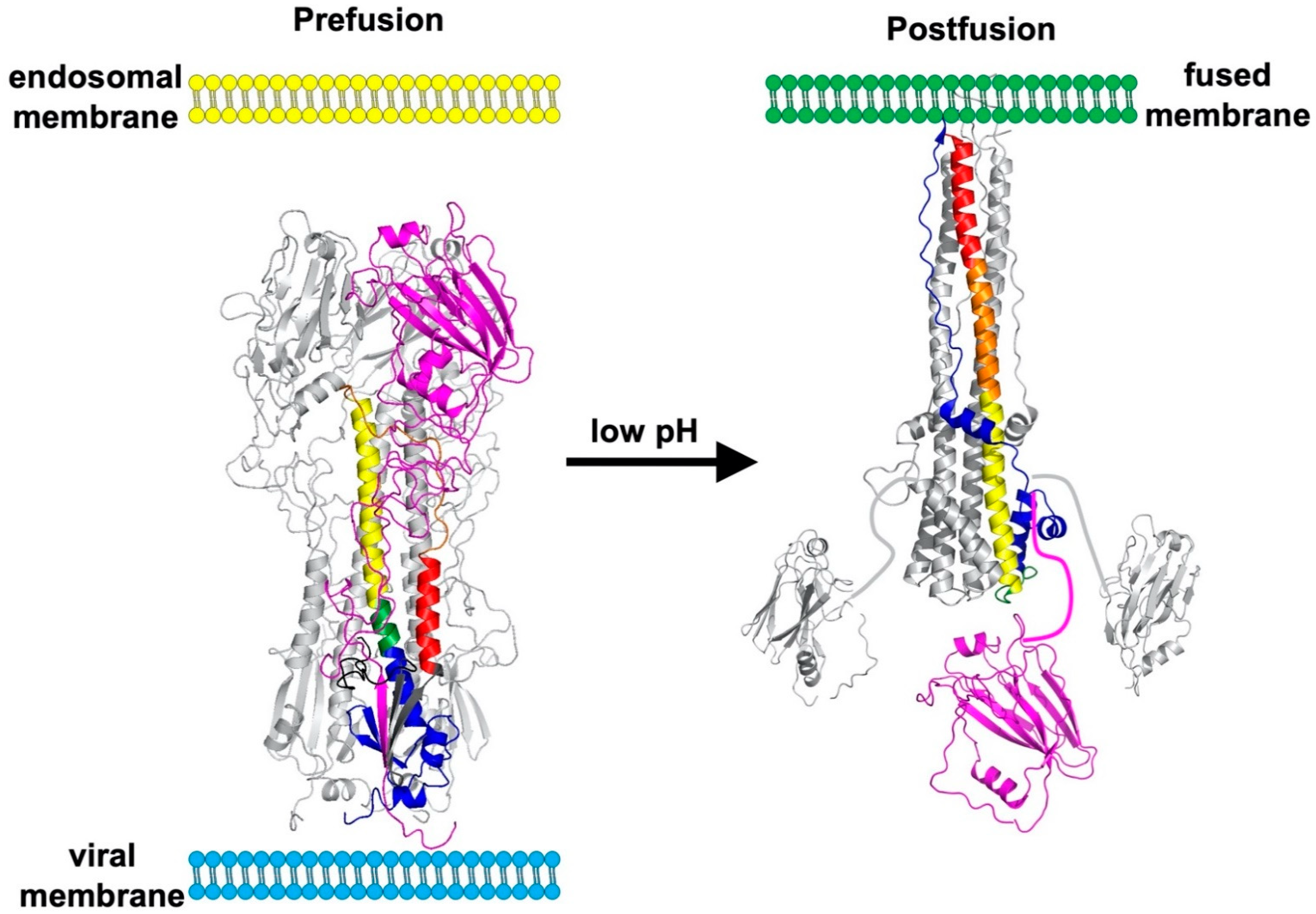
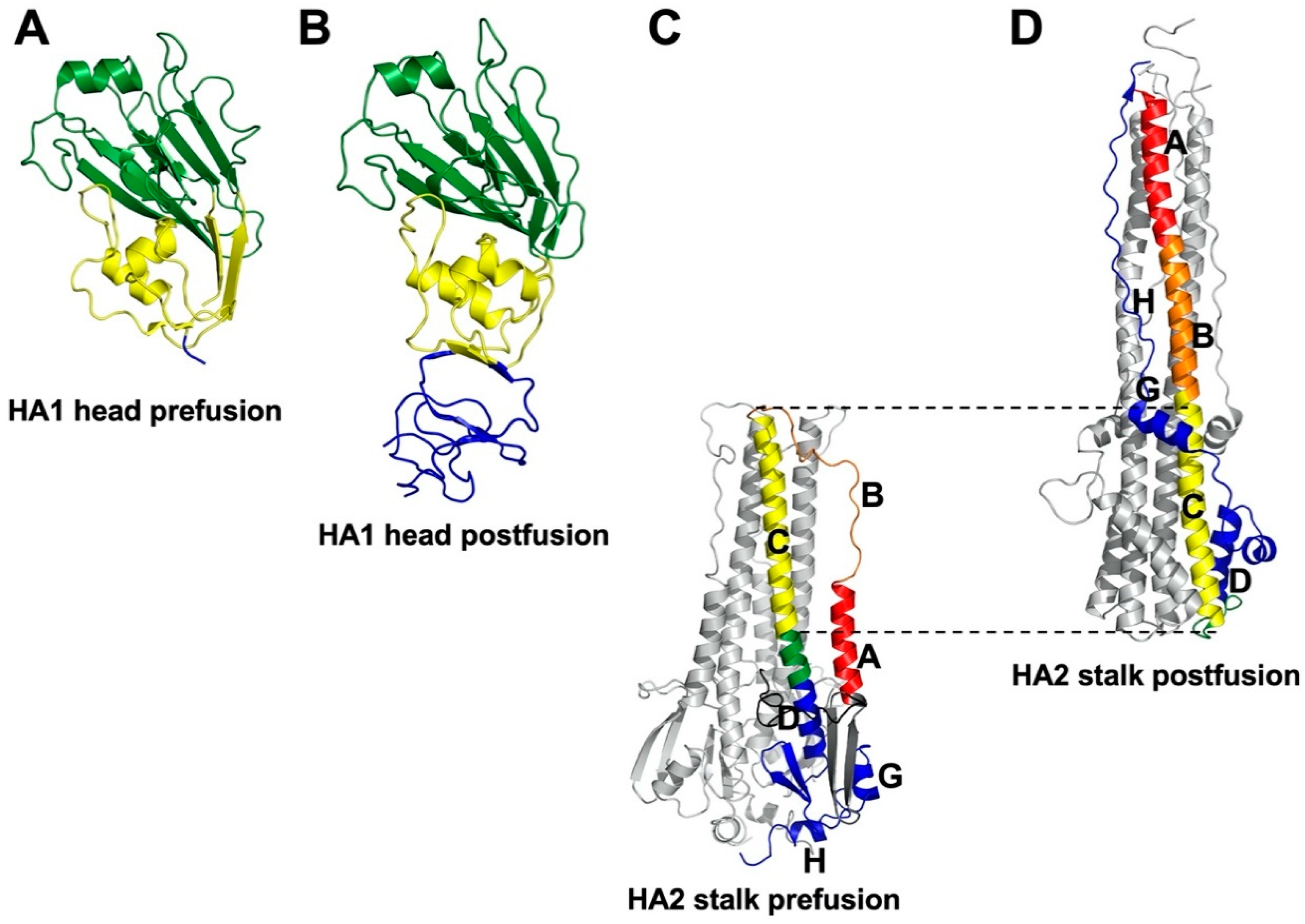
3. Molecular Basis of HA Stability
4. Trends in HA Stability for Viruses Isolated from Different Species
5. Animal Models
6. H1N1
6.1. Seasonal H1N1
6.2. Pandemic pH1N1
6.3. Swine and Avian H1
7. H2N2 and H2N3
8. H3N2
9. H5N1
10. H5Nx
11. H7Nx
12. H7N9
13. H9N2
14. H10N7
Funding
Conflicts of Interest
References
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Primers 2018, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Donatelli, I.; Castrucci, M.R.; De Marco, M.A.; Delogu, M.; Webster, R.G. Human–Animal Interface: The Case for Influenza Interspecies Transmission. Adv. Exp. Med. Biol. 2016, 972, 17–33. [Google Scholar] [CrossRef]
- Osterhaus, A.D.; Rimmelzwaan, G.F.; Martina, B.E.; Bestebroer, T.M.; Fouchier, R.A. Influenza B virus in seals. Science 2000, 288, 1051–1053. [Google Scholar] [CrossRef]
- Hause, B.M.; Ducatez, M.; Collin, E.A.; Ran, Z.; Liu, R.; Sheng, Z.; Armien, A.; Kaplan, B.; Chakravarty, S.; Hoppe, A.D.; et al. Isolation of a Novel Swine Influenza Virus from Oklahoma in 2011 Which Is Distantly Related to Human Influenza C Viruses. PLoS Pathog. 2013, 9, e1003176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuzaki, Y.; Sugawara, K.; Mizuta, K.; Tsuchiya, E.; Muraki, Y.; Hongo, S.; Suzuki, H.; Nakamura, K. Antigenic and Genetic Characterization of Influenza C Viruses Which Caused Two Outbreaks in Yamagata City, Japan, in 1996 and 1998. J. Clin. Microbiol. 2002, 40, 422–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, M.L.; Palese, P. Orthomyxoviridae. In Fields Virology, 6th ed.; Knipe, D.M., Howley, P.M., Eds.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2013; pp. 1151–1185. [Google Scholar]
- Krauss, S.; Webster, R.G. Avian influenza virus surveillance and wild birds: Past and present. Avian Dis. 2010, 54, 394–398. [Google Scholar] [CrossRef]
- Tong, S.; Li, Y.; Rivailler, P.; Conrardy, C.; Castillo, D.A.A.; Chen, L.-M.; Recuenco, S.; Ellison, J.A.; Davis, C.T.; York, I.A.; et al. A distinct lineage of influenza A virus from bats. Proc. Natl. Acad. Sci. USA 2012, 109, 4269–4274. [Google Scholar] [CrossRef] [Green Version]
- Tong, S.; Zhu, X.; Li, Y.; Shi, M.; Zhang, J.; Bourgeois, M.; Yang, H.; Chen, X.; Recuenco, S.; Gomez, J.; et al. New World Bats Harbor Diverse Influenza A Viruses. PLoS Pathog. 2013, 9, e1003657. [Google Scholar] [CrossRef] [Green Version]
- Kandeil, A.; Gomaa, M.R.; Shehata, M.M.; El Taweel, A.N.; Mahmoud, S.H.; Bagato, O.; Moatasim, Y.; Kutkat, O.; Kayed, A.S.; Dawson, P.; et al. Isolation and Characterization of a Distinct Influenza A Virus from Egyptian Bats. J. Virol. 2018, 93, e01059-18. [Google Scholar] [CrossRef] [Green Version]
- Gao, S.; Anderson, T.K.; Walia, R.R.; Dorman, K.S.; Janas-Martindale, A.; Vincent, A.L. The genomic evolution of H1 influenza A viruses from swine detected in the United States between 2009 and 2016. J. Gen. Virol. 2017, 98, 2001–2010. [Google Scholar] [CrossRef]
- Anderson, T.K.; Macken, C.A.; Lewis, N.S.; Scheuermann, R.H.; Van Reeth, K.; Brown, I.H.; Swenson, S.L.; Simon, G.; Saito, T.; Berhane, Y.; et al. A Phylogeny-Based Global Nomenclature System and Automated Annotation Tool for H1 Hemagglutinin Genes from Swine Influenza A Viruses. mSphere 2016, 1, e00275-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Webster, R.G.; Webby, R.J. Influenza Virus: Dealing with a Drifting and Shifting Pathogen. Viral Immunol. 2018, 31, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Cauldwell, A.V.; Long, J.S.; Moncorge, O.; Barclay, W.W. Viral determinants of influenza A virus host range. J. Gen. Virol. 2014, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bottcher-Friebertshauser, E.; Garten, W.; Matrosovich, M.; Klenk, H.D. The Hemagglutinin: A Determinant of Pathogenicity. In Influenza Pathogenesis and Control—Vol I; Compans, R.W., Oldstone, M.B.A., Eds.; Springer International Publishing Ag: Cham, Switzerland, 2014; Volume 385, pp. 3–34. [Google Scholar]
- de Graaf, M.; Fouchier, R.A. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J. 2014, 33, 823–841. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiong, X.L.; McCauley, J.W.; Steinhauer, D.A. Receptor binding properties of the influenza virus hemagglutinin as a determinant of host range. Curr. Top. Microbiol. Immunol. 2014, 385, 63–91. [Google Scholar] [PubMed]
- Tumpey, T.M.; Maines, T.R.; Van Hoeven, N.; Glaser, L.; Solórzano, A.; Pappas, C.; Cox, N.J.; Swayne, D.E.; Palese, P.; Katz, J.M.; et al. A Two-Amino Acid Change in the Hemagglutinin of the 1918 Influenza Virus Abolishes Transmission. Science 2007, 315, 655–659. [Google Scholar] [CrossRef]
- Yoon, S.-W.; Chen, N.; Ducatez, M.F.; McBride, R.; Barman, S.; Fabrizio, T.P.; Webster, R.G.; Haliloglu, T.; Paulson, J.C.; Russell, C.J.; et al. Changes to the dynamic nature of hemagglutinin and the emergence of the 2009 pandemic H1N1 influenza virus. Sci. Rep. 2015, 5, 12828. [Google Scholar] [CrossRef] [Green Version]
- Rogers, G.N.; Paulson, J.C. Receptor determinants of human and animal influenza virus isolates: Differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 1983, 127, 361–373. [Google Scholar] [CrossRef]
- Long, J.S.; Mistry, B.; Haslam, S.M.; Barclay, W.S. Host and viral determinants of influenza A virus species specificity. Nat. Rev. Microbiol. 2019, 17, 67–81. [Google Scholar] [CrossRef]
- Varki, A. Colloquium paper: Uniquely human evolution of sialic acid genetics and biology. Proc. Natl. Acad. Sci. USA 2010, 107, 8939–8946. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, Y.; Ito, T.; Suzuki, T.; Holland, R.E.; Chambers, T.M.; Kiso, M.; Ishida, H.; Kawaoka, Y. Sialic Acid Species as a Determinant of the Host Range of Influenza A Viruses. J. Virol. 2000, 74, 11825–11831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neumann, G.; Kawaoka, Y. Transmission of influenza A viruses. Virology 2015, 479–480, 234–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradley, K.C.; Jones, C.A.; Tompkins, S.M.; Tripp, R.A.; Russell, R.J.; Gramer, M.R.; Heimburg-Molinaro, J.; Smith, D.F.; Cummings, R.D.; Steinhauer, D.A. Comparison of the receptor binding properties of contemporary swine isolates and early human pandemic H1N1 isolates (Novel 2009 H1N1). Virology 2011, 413, 169–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byrd-Leotis, L.; Cummings, R.D.; Steinhauer, D.A. The Interplay between the Host Receptor and Influenza Virus Hemagglutinin and Neuraminidase. Int. J. Mol. Sci. 2017, 18, 1541. [Google Scholar] [CrossRef] [Green Version]
- Byrd-Leotis, L.; Jia, N.; Dutta, S.; Trost, J.F.; Gao, C.; Cummings, S.F.; Braulke, T.; Müller-Loennies, S.; Heimburg-Molinaro, J.; Steinhauer, D.A.; et al. Influenza binds phosphorylated glycans from human lung. Sci. Adv. 2019, 5, eaav2554. [Google Scholar] [CrossRef] [Green Version]
- Xu, R.; Zhu, X.; McBride, R.; Nycholat, C.M.; Yu, W.; Paulson, J.C.; Wilson, I.A. Functional Balance of the Hemagglutinin and Neuraminidase Activities Accompanies the Emergence of the 2009 H1N1 Influenza Pandemic. J. Virol. 2012, 86, 9221–9232. [Google Scholar] [CrossRef] [Green Version]
- Gaymard, A.; Le Briand, N.; Frobert, E.; Lina, B.; Escuret, V. Functional balance between neuraminidase and haemagglutinin in influenza viruses. Clin. Microbiol. Infect. 2016, 22, 975–983. [Google Scholar] [CrossRef]
- Yen, H.-L.; Liang, C.-H.; Wu, C.-Y.; Forrest, H.L.; Ferguson, A.; Choy, K.-T.; Jones, J.; Wong, D.D.-Y.; Cheung, P.P.-H.; Hsu, C.-H.; et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc. Natl. Acad. Sci. USA 2011, 108, 14264–14269. [Google Scholar] [CrossRef] [Green Version]
- Gambaryan, A.S.; Matrosovich, M.N. What adaptive changes in hemagglutinin and neuraminidase are necessary for emergence of pandemic influenza virus from its avian precursor? Biochemistry 2015, 80, 872–880. [Google Scholar] [CrossRef]
- Russell, C.J. Acid-Induced Membrane Fusion by the Hemagglutinin Protein and Its Role in Influenza Virus Biology. Curr. Top. Microbiol. Immunol. 2014, 385, 93–116. [Google Scholar] [CrossRef]
- Russell, C.J.; Hu, M.; Okda, F.A. Influenza Hemagglutinin Protein Stability, Activation, and Pandemic Risk. Trends Microbiol. 2018, 26, 841–853. [Google Scholar] [CrossRef]
- Scholtissek, C. Stability of infectious influenza A viruses at low pH and at elevated temperature. Vaccine 1985, 3, 215–218. [Google Scholar] [CrossRef]
- Skehel, J.J.; Wiley, D.C. Receptor Binding and Membrane Fusion in Virus Entry: The Influenza Hemagglutinin. Annu. Rev. Biochem. 2000, 69, 531–569. [Google Scholar] [CrossRef]
- Wu, N.C.; Wilson, I.A. Influenza Hemagglutinin Structures and Antibody Recognition. Cold Spring Harb. Perspect. Med. 2019, 10, a038778. [Google Scholar] [CrossRef] [Green Version]
- Mair, C.M.; Ludwig, K.; Herrmann, A.; Sieben, C. Receptor binding and pH stability—How influenza A virus hemagglutinin affects host-specific virus infection. Biochim. et Biophys. Acta (BBA) Biomembr. 2014, 1838, 1153–1168. [Google Scholar] [CrossRef] [Green Version]
- Belser, J.A.; Pulit-Penaloza, J.A.; Maines, T.R. Ferreting Out Influenza Virus Pathogenicity and Transmissibility: Past and Future Risk Assessments in the Ferret Model. Cold Spring Harb. Perspect. Med. 2019, 10, a038323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herfst, S.; Böhringer, M.; Karo, B.; Lawrence, P.; Lewis, N.S.; Mina, M.J.; Russell, C.; Charles, J.; Steel, J.; De Swart, R.L.; et al. Drivers of airborne human-to-human pathogen transmission. Curr. Opin. Virol. 2017, 22, 22–29. [Google Scholar] [CrossRef]
- Joseph, U.; Su, Y.C.F.; Vijaykrishna, D.; Smith, G.J.D. The ecology and adaptive evolution of influenza A interspecies transmission. Influ. Other Respir. Viruses 2016, 11, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Lipsitch, M.; Barclay, W.; Raman, R.; Russell, C.J.; Belser, J.A.; Cobey, S.; Kasson, P.M.; Lloyd-Smith, J.O.; Maurer-Stroh, S.; Riley, S.; et al. Viral factors in influenza pandemic risk assessment. eLife 2016, 5, e18491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, M.L.; Stertz, S. Role of Host Genes in Influenza Virus Replication. Curr. Top. Microbiol. Immunol. 2017, 419, 151–189. [Google Scholar] [CrossRef]
- Edinger, T.O.; Pohl, M.O.; Stertz, S. Entry of influenza A virus: Host factors and antiviral targets. J. Gen. Virol. 2014, 95, 263–277. [Google Scholar] [CrossRef]
- Flatt, J.W.; Greber, U.F. Misdelivery at the Nuclear Pore Complex—Stopping a Virus Dead in Its Tracks. Cells 2015, 4, 277–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehwinkel, J.; Tan, C.P.; Goubau, D.; Schulz, O.; Pichlmair, A.; Bier, K.; Robb, N.; Vreede, F.; Barclay, W.; Fodor, E.; et al. RIG-I Detects Viral Genomic RNA during Negative-Strand RNA Virus Infection. Cell 2010, 140, 397–408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subbarao, E.K.; London, W.; Murphy, B.R. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 1993, 67, 1761–1764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Te Velthuis, A.J.W.; Grimes, J.M.; Fodor, E. Structural insights into RNA polymerases of negative-sense RNA viruses. Nat. Rev. Microbiol. 2021, 19, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Krischuns, T.; Lukarska, M.; Naffakh, N.; Cusack, S. Influenza Virus RNA-Dependent RNA Polymerase and the Host Transcriptional Apparatus. Annu. Rev. Biochem. 2021, 90. [Google Scholar] [CrossRef]
- Long, J.S.; Giotis, E.S.; Moncorgé, O.; Frise, R.; Mistry, B.; James, J.; Morisson, M.; Iqbal, M.; Vignal, A.; Skinner, M.A.; et al. Species difference in ANP32A underlies influenza A virus polymerase host restriction. Nature 2016, 529, 101–104. [Google Scholar] [CrossRef] [Green Version]
- Lakdawala, S.S.; Lamirande, E.W.; Suguitan, A.L.; Wang, W.; Santos, C.P.; Vogel, L.; Matsuoka, Y.; Lindsley, W.G.; Jin, H.; Subbarao, K. Eurasian-Origin Gene Segments Contribute to the Transmissibility, Aerosol Release, and Morphology of the 2009 Pandemic H1N1 Influenza Virus. PLoS Pathog. 2011, 7, e1002443. [Google Scholar] [CrossRef] [Green Version]
- Herfst, S.; Schrauwen, E.J.; Linster, M.; Chutinimitkul, S.; de Wit, E.; Munster, V.J.; Sorrell, E.M.; Bestebroer, T.M.; Burke, D.F.; Smith, D.J.; et al. Airborne Transmission of Influenza A/H5N1 Virus Between Ferrets. Science 2012, 336, 1534–1541. [Google Scholar] [CrossRef] [Green Version]
- Imai, M.; Watanabe, T.; Hatta, M.; Das, S.C.; Ozawa, M.; Shinya, K.; Zhong, G.; Hanson, A.; Katsura, H.; Watanabe, S.; et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 2012, 486, 420–428. [Google Scholar] [CrossRef] [Green Version]
- Linster, M.; Van Boheemen, S.; De Graaf, M.; Schrauwen, E.J.A.; Lexmond, P.; Mänz, B.; Bestebroer, T.M.; Baumann, J.; Van Riel, D.; Rimmelzwaan, G.F.; et al. Identification, Characterization, and Natural Selection of Mutations Driving Airborne Transmission of A/H5N1 Virus. Cell 2014, 157, 329–339. [Google Scholar] [CrossRef] [Green Version]
- Copeland, C.S.; Zimmer, K.-P.; Wagner, K.R.; Healey, G.A.; Mellman, I.; Helenius, A. Folding, trimerization, and transport are sequential events in the biogenesis of influenza virus hemagglutinin. Cell 1988, 53, 197–209. [Google Scholar] [CrossRef]
- Hebert, D.N.; Foellmer, B.; Helenius, A. Glucose trimming and reglucosylation determine glycoprotein association with calnexin in the endoplasmic reticulum. Cell 1995, 81, 425–433. [Google Scholar] [CrossRef] [Green Version]
- Naeve, C.W.; Williams, D. Fatty-Acids on the a-Japan-305-57 Influenza-Virus Hemagglutinin Have a Role in Membrane-Fusion. Embo J. 1990, 9, 3857–3866. [Google Scholar] [CrossRef] [PubMed]
- Veit, M.; Kretzschmar, E.; Kuroda, K.; Garten, W.; Schmidt, M.F.G.; Klenk, H.D.; Rott, R. Site-Specific Mutagenesis Identifies 3 Cysteine Residues in the Cytoplasmic Tail as Acylation Sites of Influenza-Virus Hemagglutinin. J. Virol. 1991, 65, 2491–2500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinhauer, D.A.; Wharton, S.A.; Wiley, D.C.; Skehel, J.J. Deacylation of the Hemagglutinin of Influenza-a/Aichi/2/68 Has No Effect on Membrane-Fusion Properties. Virology 1991, 184, 445–448. [Google Scholar] [CrossRef]
- Steinhauer, D.A. Role of Hemagglutinin Cleavage for the Pathogenicity of Influenza Virus. Virology 1999, 258, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Garten, W.; Braden, C.; Arendt, A.; Peitsch, C.; Baron, J.; Lu, Y.; Pawletko, K.; Hardes, K.; Steinmetzer, T.; Böttcher-Friebertshäuser, E. Influenza virus activating host proteases: Identification, localization and inhibitors as potential therapeutics. Eur. J. Cell Biol. 2015, 94, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Garten, W.; Bosch, F.X.; Linder, D.; Rott, R.; Klenk, H.-D. Proteolytic activation of the influenza virus hemagglutinin: The structure of the cleavage site and the enzymes involved in cleavage. Virology 1981, 115, 361–374. [Google Scholar] [CrossRef]
- Webster, R.G.; Rott, R. Influenza virus a pathogenicity: The pivotal role of hemagglutinin. Cell 1987, 50, 665–666. [Google Scholar] [CrossRef]
- Stienekegrober, A.; Vey, M.; Angliker, H.; Shaw, E.; Thomas, G.; Roberts, C.; Klenk, H.D.; Garten, W. Influenza-Virus Hemagglutinin with Multibasic Cleavage Site Is Activated by Furin, a Subtilisin-Like Endoprotease. Embo J. 1992, 11, 2407–2414. [Google Scholar] [CrossRef]
- Kido, H.; Yokogoshi, Y.; Sakai, K.; Tashiro, M.; Kishino, Y.; Fukutomi, A.; Katunuma, N. Isolation and Characterization of a Novel Trypsin-Like Protease Found in Rat Bronchiolar Epithelial Clara Cells—A Possible Activator of the Viral Fusion Glycoprotein. J. Biol. Chem. 1992, 267, 13573–13579. [Google Scholar] [CrossRef]
- Murakami, M.; Towatari, T.; Ohuchi, M.; Shiota, M.; Akao, M.; Okumura, Y.; Parry, M.A.A.; Kido, H. Mini-plasmin found in the epithelial cells of bronchioles triggers infection by broad-spectrum influenza A viruses and Sendai virus. JBIC J. Biol. Inorg. Chem. 2001, 268, 2847–2855. [Google Scholar] [CrossRef] [PubMed]
- Towatari, T.; Ide, M.; Ohba, K.; Chiba, Y.; Murakami, M.; Shiota, M.; Kawachi, M.; Yamada, H.; Kido, H. Identification of ectopic anionic trypsin I in rat lungs potentiating pneumotropic virus infectivity and increased enzyme level after virus infection. JBIC J. Biol. Inorg. Chem. 2002, 269, 2613–2621. [Google Scholar] [CrossRef] [PubMed]
- Bottcher, E.; Matrosovich, T.; Beyerle, M.; Klenk, H.-D.; Garten, W.; Matrosovich, M. Proteolytic Activation of Influenza Viruses by Serine Proteases TMPRSS2 and HAT from Human Airway Epithelium. J. Virol. 2006, 80, 9896–9898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okumura, Y.; Takahashi, E.; Yano, M.; Ohuchi, M.; Daidoji, T.; Nakaya, T.; Boöttcher, E.; Garten, W.; Klenk, H.-D.; Kido, H. Novel Type II Transmembrane Serine Proteases, MSPL and TMPRSS13, Proteolytically Activate Membrane Fusion Activity of the Hemagglutinin of Highly Pathogenic Avian Influenza Viruses and Induce Their Multicycle Replication. J. Virol. 2010, 84, 5089–5096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Lee, K.H.; Steinhauer, D.A.; Stevens, D.J.; Skehel, J.J.; Wiley, D.C. Structure of the Hemagglutinin Precursor Cleavage Site, a Determinant of Influenza Pathogenicity and the Origin of the Labile Conformation. Cell 1998, 95, 409–417. [Google Scholar] [CrossRef] [Green Version]
- Wilson, I.A.; Skehel, J.J.; Wiley, D.C. Structure of the Hemagglutinin Membrane Glycoprotein of Influenza-Virus at 3-a Resolution. Nature 1981, 289, 366–373. [Google Scholar] [CrossRef]
- Xu, R.; Wilson, I.A. Structural Characterization of an Early Fusion Intermediate of Influenza Virus Hemagglutinin. J. Virol. 2011, 85, 5172–5182. [Google Scholar] [CrossRef] [Green Version]
- Bullough, P.A.; Hughson, F.M.; Skehel, J.J.; Wiley, D.C. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature 1994, 371, 37–43. [Google Scholar] [CrossRef]
- Chen, J.; Skehel, J.J.; Wiley, D.C. N- and C-terminal residues combine in the fusion-pH influenza hemagglutinin HA(2) subunit to form an N cap that terminates the triple-stranded coiled coil. Proc. Natl. Acad. Sci. USA 1999, 96, 8967–8972. [Google Scholar] [CrossRef] [Green Version]
- Yewdell, J.W.; Gerhard, W.; Bachi, T. Monoclonal anti-hemagglutinin antibodies detect irreversible antigenic alterations that coincide with the acid activation of influenza virus A/PR/834-mediated hemolysis. J. Virol. 1983, 48, 239–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruigrok, R.; Martin, S.; Wharton, S.; Skehel, J.; Bayley, P.; Wiley, D. Conformational changes in the hemagglutinin of influenza virus which accompany heat-induced fusion of virus with liposomes. Virology 1986, 155, 484–497. [Google Scholar] [CrossRef]
- Carr, C.M.; Chaudhry, C.; Kim, P.S. Influenza hemagglutinin is spring-loaded by a metastable native conformation. Proc. Natl. Acad. Sci. USA 1997, 94, 14306–14313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubois, R.M.; Aguilar-Yañez, J.M.; Mendoza-Ochoa, G.I.; Oropeza-Almazán, Y.; Schultz-Cherry, S.; Alvarez, M.M.; White, S.W.; Russell, C.J. The Receptor-Binding Domain of Influenza Virus Hemagglutinin Produced in Escherichia coli Folds into Its Native, Immunogenic Structure. J. Virol. 2010, 85, 865–872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bizebard, T.; Gigant, B.; Rigolet, P.; Rasmussen, B.; Diat, O.; Bãseckei, P.; Wharton, S.A.; Skehel, J.J.; Knossow, M. Structure of influenza virus haemagglutinin complexed with a neutralizing antibody. Nature 1995, 376, 92–94. [Google Scholar] [CrossRef] [PubMed]
- White, J.M.; Whittaker, G.R. Fusion of Enveloped Viruses in Endosomes. Traffic 2016, 17, 593–614. [Google Scholar] [CrossRef] [Green Version]
- Gruenke, J.A.; Armstrong, R.T.; Newcomb, W.W.; Brown, J.C.; White, J.M. New Insights into the Spring-Loaded Conformational Change of Influenza Virus Hemagglutinin. J. Virol. 2002, 76, 4456–4466. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, P.B.; Zhang, X.; Formanowski, F.; Fitz, W.; Wong, C.-H.; Meier-Ewert, H.; Skehel, J.J.; Wiley, D.C. Structure of the haemagglutinin-esterase-fusion glycoprotein of influenza C virus. Nature 1998, 396, 92–96. [Google Scholar] [CrossRef]
- Xu, R.; McBride, R.; Nycholat, C.M.; Paulson, J.C.; Wilson, I.A. Structural Characterization of the Hemagglutinin Receptor Specificity from the 2009 H1N1 Influenza Pandemic. J. Virol. 2011, 86, 982–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daniels, R.; Downie, J.; Hay, A.; Knossow, M.; Skehel, J.; Wang, M.; Wiley, D. Fusion mutants of the influenza virus hemagglutinin glycoprotein. Cell 1985, 40, 431–439. [Google Scholar] [CrossRef]
- Gething, M.-J.; Doms, R.W.; York, D.; White, J. Studies on the mechanism of membrane fusion: Site-specific mutagenesis of the hemagglutinin of influenza virus. J. Cell Biol. 1986, 102, 11–23. [Google Scholar] [CrossRef]
- Steinhauer, D.A.; Wharton, S.A.; Skehel, J.J.; Wiley, D.C. Studies of the membrane fusion activities of fusion peptide mutants of influenza virus hemagglutinin. J. Virol. 1995, 69, 6643–6651. [Google Scholar] [CrossRef] [Green Version]
- Steinhauer, D.A.; Martin, J.; Lin, Y.P.; Wharton, S.A.; Oldstone, M.B.A.; Skehel, J.J.; Wiley, D.C. Studies using double mutants of the conformational transitions in influenza hemagglutinin required for its membrane fusion activity. Proc. Natl. Acad. Sci. USA 1996, 93, 12873–12878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thoennes, S.; Li, Z.-N.; Lee, B.-J.; Langley, W.A.; Skehel, J.J.; Russell, R.J.; Steinhauer, D.A. Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology 2008, 370, 403–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanson, A.; Imai, M.; Hatta, M.; McBride, R.; Imai, H.; Taft, A.; Zhong, G.; Watanabe, T.; Suzuki, Y.; Neumann, G.; et al. Identification of Stabilizing Mutations in an H5 Hemagglutinin Influenza Virus Protein. J. Virol. 2015, 90, 2981–2992. [Google Scholar] [CrossRef] [Green Version]
- Byrd-Leotis, L.; Galloway, S.E.; Agbogu, E.; Steinhauer, D.A. Influenza Hemagglutinin (HA) Stem Region Mutations That Stabilize or Destabilize the Structure of Multiple HA Subtypes. J. Virol. 2015, 89, 4504–4516. [Google Scholar] [CrossRef] [Green Version]
- Antanasijevic, A.; Durst, M.A.; Lavie, A.; Caffrey, M. Identification of a pH sensor in Influenza hemagglutinin using X-ray crystallography. J. Struct. Biol. 2020, 209, 107412. [Google Scholar] [CrossRef]
- Weis, W.I.; Cusack, S.C.; Brown, J.H.; Daniels, R.S.; Skehel, J.J.; Wiley, D.C. The Structure of a Membrane-Fusion Mutant of the Influenza-Virus Hemagglutinin. EMBO J. 1990, 9, 17–24. [Google Scholar] [CrossRef]
- Dubois, R.M.; Zaraket, H.; Reddivari, M.; Heath, R.J.; White, S.W.; Russell, C.J. Acid Stability of the Hemagglutinin Protein Regulates H5N1 Influenza Virus Pathogenicity. PLoS Pathog. 2011, 7, e1002398. [Google Scholar] [CrossRef] [Green Version]
- Xiong, X.; Coombs, P.J.; Martin, S.R.; Liu, J.; Xiao, H.; McCauley, J.W.; Locher, K.; Walker, P.A.; Collins, P.J.; Kawaoka, Y.; et al. Receptor binding by a ferret-transmissible H5 avian influenza virus. Nature 2013, 497, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Shi, Y.; Zhang, W.; Zhang, Y.; Qi, J.; Gao, G.F. Structure and receptor-binding properties of an airborne transmissible avian influenza A virus hemagglutinin H5 (VN1203mut). Protein Cell 2013, 4, 502–511. [Google Scholar] [CrossRef] [Green Version]
- De Vries, R.P.; Zhu, X.; McBride, R.; Rigter, A.; Hanson, A.; Zhong, G.; Hatta, M.; Xu, R.; Yu, W.; Kawaoka, Y.; et al. Hemagglutinin Receptor Specificity and Structural Analyses of Respiratory Droplet-Transmissible H5N1 Viruses. J. Virol. 2013, 88, 768–773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rachakonda, P.S.; Veit, M.; Korte, T.; Ludwig, K.; Böttcher, C.; Huang, Q.; Schmidt, M.F.G.; Herrmann, A. The relevance of salt bridges for the stability of the influenza virus hemagglutinin. FASEB J. 2007, 21, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Ohuchi, M.; Asaoka, N.; Sakai, T.; Ohuchi, R. Roles of neuraminidase in the initial stage of influenza virus infection. Microbes Infect. 2006, 8, 1287–1293. [Google Scholar] [CrossRef]
- Matrosovich, M.N.; Matrosovich, T.Y.; Gray, T.; Roberts, N.A.; Klenk, H.-D. Neuraminidase Is Important for the Initiation of Influenza Virus Infection in Human Airway Epithelium. J. Virol. 2004, 78, 12665–12667. [Google Scholar] [CrossRef] [Green Version]
- Reed, M.L.; Bridges, O.A.; Seiler, P.; Kim, J.-K.; Yen, H.-L.; Salomon, R.; Govorkova, E.A.; Webster, R.G.; Russell, C.J. The pH of Activation of the Hemagglutinin Protein Regulates H5N1 Influenza Virus Pathogenicity and Transmissibility in Ducks. J. Virol. 2009, 84, 1527–1535. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, C.D.; Vogel, L.; Matsuoka, Y.; Jin, H.; Subbarao, K. The Matrix Gene Segment Destabilizes the Acid and Thermal Stability of the Hemagglutinin of Pandemic Live Attenuated Influenza Virus Vaccines. J. Virol. 2014, 88, 12374–12384. [Google Scholar] [CrossRef] [Green Version]
- Sauter, N.K.; Hanson, J.E.; Glick, G.D.; Brown, J.H.; Crowther, R.L.; Park, S.J.; Skehel, J.J.; Wiley, D.C. Binding of influenza virus hemagglutinin to analogs of its cell-surface receptor, sialic acid: Analysis by proton nuclear magnetic resonance spectroscopy and x-ray crystallography. Biochemistry 1992, 31, 9609–9621. [Google Scholar] [CrossRef]
- Ha, Y.; Stevens, D.J.; Skehel, J.J.; Wiley, D.C. H5 avian and H9 swine influenza virus haemagglutinin structures: Possible origin of influenza subtypes. EMBO J. 2002, 21, 865–875. [Google Scholar] [CrossRef] [Green Version]
- Burke, D.F.; Smith, D.J. A Recommended Numbering Scheme for Influenza A HA Subtypes. PLoS ONE 2014, 9, e112302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- HA Subtype Numbering Conversion (Beta). Available online: https://www.fludb.org/brc/haNumbering.spg?method=ShowCleanInputPage&decorator=influenza (accessed on 1 April 2021).
- Blijleven, J.S.; Boonstra, S.; Onck, P.R.; van der Giessen, E.; van Oijen, A.M. Mechanisms of influenza viral membrane fusion. Semin. Cell Dev. Biol. 2016, 60, 78–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, B.S.; Whittaker, G.R.; Daniel, S. Influenza Virus-Mediated Membrane Fusion: Determinants of Hemagglutinin Fusogenic Activity and Experimental Approaches for Assessing Virus Fusion. Viruses 2012, 4, 1144–1168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costello, D.A.; Whittaker, G.R.; Daniel, S. Variations in pH Sensitivity, Acid Stability, and Fusogenicity of Three Influenza Virus H3 Subtypes. J. Virol. 2014, 89, 350–360. [Google Scholar] [CrossRef] [Green Version]
- Hsu, H.-L.; Millet, J.K.; Costello, D.A.; Whittaker, G.R.; Daniel, S. Viral fusion efficacy of specific H3N2 influenza virus reassortant combinations at single-particle level. Sci. Rep. 2016, 6, 35537. [Google Scholar] [CrossRef]
- Galloway, S.E.; Reed, M.L.; Russell, C.J.; Steinhauer, D.A. Influenza HA Subtypes Demonstrate Divergent Phenotypes for Cleavage Activation and pH of Fusion: Implications for Host Range and Adaptation. PLoS Pathog. 2013, 9, e1003151. [Google Scholar] [CrossRef] [Green Version]
- Okamatsu, M.; Motohashi, Y.; Hiono, T.; Tamura, T.; Nagaya, K.; Matsuno, K.; Sakoda, Y.; Kida, H. Is the optimal pH for membrane fusion in host cells by avian influenza viruses related to host range and pathogenicity? Arch. Virol. 2016, 161, 2235–2242. [Google Scholar] [CrossRef]
- Brown, J.D.; Goekjian, G.; Poulson, R.; Valeika, S.; Stallknecht, D.E. Avian influenza virus in water: Infectivity is dependent on pH, salinity and temperature. Vet. Microbiol. 2009, 136, 20–26. [Google Scholar] [CrossRef]
- Poulson, R.L.; Tompkins, S.M.; Berghaus, R.D.; Brown, J.D.; Stallknecht, D.E. Environmental Stability of Swine and Human Pandemic Influenza Viruses in Water under Variable Conditions of Temperature, Salinity, and pH. Appl. Environ. Microbiol. 2016, 82, 3721–3726. [Google Scholar] [CrossRef] [Green Version]
- Thompson, K.-A.; Bennett, A. Persistence of influenza on surfaces. J. Hosp. Infect. 2017, 95, 194–199. [Google Scholar] [CrossRef]
- Munster, V.; Baas, C.; Lexmond, P.; Waldenström, J.; Wallensten, A.; Fransson, T.; Rimmelzwaan, G.; Beyer, W.; Schutten, M.; Olsen, B.; et al. Spatial, Temporal, and Species Variation in Prevalence of Influenza A Viruses in Wild Migratory Birds. PLoS Pathog. 2007, 3, e61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krauss, S.; Walker, D.; Pryor, S.P.; Niles, L.; Chenghong, L.; Hinshaw, V.S.; Webster, R.G. Influenza A viruses of migrating wild aquatic birds in North America. Vector Borne Zoonotic Dis. 2004, 4, 177–189. [Google Scholar] [CrossRef]
- Honce, R.; Schultz-Cherry, S. Recipe for Zoonosis: How Influenza Virus Leaps into Human Circulation. Cell Host Microbe 2020, 28, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Peiris, M.; Yen, H.-L. Animal and human influenzas. Rev. Sci. et Tech. de l’OIE 2014, 33, 539–553. [Google Scholar] [CrossRef] [PubMed]
- Hinshaw, V.S.; Bean, W.J.; Geraci, J.; Fiorelli, P.; Early, G.; Webster, R.G. Characterization of two influenza A viruses from a pilot whale. J. Virol. 1986, 58, 655–656. [Google Scholar] [CrossRef] [Green Version]
- Gulyaeva, M.; Sobolev, I.; Sharshov, K.; Kurskaya, O.; Alekseev, A.; Shestopalova, L.; Kovner, A.; Bi, Y.; Shi, W.; Shchelkanov, M.; et al. Characterization of Avian-like Influenza A (H4N6) Virus Isolated from Caspian Seal in 2012. Virol. Sin. 2018, 33, 449–452. [Google Scholar] [CrossRef]
- Karasin, A.I.; Brown, I.H.; Carman, S.; Olsen, C.W. Isolation and Characterization of H4N6 Avian Influenza Viruses from Pigs with Pneumonia in Canada. J. Virol. 2000, 74, 9322–9327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olivier, A.J. Ecology and epidemiology of avian influenza in ostriches. Dev. Boil. 2006, 124, 51–57. [Google Scholar]
- Xie, T.; Anderson, B.D.; Daramragchaa, U.; Chuluunbaatar, M.; Gray, G.C. A Review of Evidence that Equine Influenza Viruses Are Zoonotic. Pathogens 2016, 5, 50. [Google Scholar] [CrossRef] [Green Version]
- Hayward, J.J.; Dubovi, E.J.; Scarlett, J.M.; Janeczko, S.; Holmes, E.C.; Parrish, C.R. Microevolution of Canine Influenza Virus in Shelters and Its Molecular Epidemiology in the United States. J. Virol. 2010, 84, 12636–12645. [Google Scholar] [CrossRef] [Green Version]
- Romváry, J.; Rózsa, J.; Farkas, E. Infection of dogs and cats with the Hong Kong influenza A (H3N2) virus during an epidemic period in Hungary. Acta Vet. Acad. Sci. Hung. 1975, 25, 255–259. [Google Scholar]
- Borland, S.; Gracieux, P.; Jones, M.; Mallet, F.; Yugueros-Marcos, J. Influenza A Virus Infection in Cats and Dogs: A Literature Review in the Light of the “One Health” Concept. Front. Public Health 2020, 8, 83. [Google Scholar] [CrossRef]
- O’Donnell, C.D.; Subbarao, K. The contribution of animal models to the understanding of the host range and virulence of influenza A viruses. Microbes Infect. 2011, 13, 502–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belser, J.A.; Eckert, A.M.; Tumpey, T.M.; Maines, T.R. Complexities in Ferret Influenza Virus Pathogenesis and Transmission Models. Microbiol. Mol. Biol. Rev. 2016, 80, 733–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouvier, N.M. Animal models for influenza virus transmission studies: A historical perspective. Curr. Opin. Virol. 2015, 13, 101–108. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.K.; Negovetich, N.J.; Forrest, H.L.; Webster, R.G. Ducks: The “Trojan horses” of H5N1 influenza. Influenza Other Respir. Viruses 2009, 3, 121–128. [Google Scholar]
- Fouchier, R.A.; Munster, V.J. Epidemiology of low pathogenic avian influenza viruses in wild birds. Rev. Sci. Tech. 2009, 28, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Kawaoka, Y.; Webster, R.G. Molecular mechanism of acquisition of virulence in influenza virus in nature. Microb. Pathog. 1988, 5, 311–318. [Google Scholar] [CrossRef]
- Kamal, R.P.; Katz, J.M.; York, I.A. Molecular Determinants of Influenza Virus Pathogenesis in Mice. Curr. Top. Microbiol. Immunol. 2014, 385, 243–274. [Google Scholar] [PubMed] [Green Version]
- Samet, S.J.; Tompkins, S.M. Influenza Pathogenesis in Genetically Defined Resistant and Susceptible Murine Strains. Yale J. Boil. Med. 2017, 90, 471–479. [Google Scholar]
- Rajao, D.S.; Vincent, A.L. Swine as a Model for Influenza A Virus Infection and Immunity. ILAR J. 2015, 56, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Bouvier, N.M.; Steel, J. Transmission in the Guinea Pig Model. Curr. Top. Microbiol. Immunol. 2014, 385, 157–183. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, R.A.; Liu, W.-C.; Sant, A.J.; Tompkins, S.M.; Pekosz, A.; Meliopoulos, V.; Cherry, S.; Thomas, P.G.; Schultz-Cherry, S. Moving Forward: Recent Developments for the Ferret Biomedical Research Model. mBio 2018, 9, e01113-18. [Google Scholar] [CrossRef] [Green Version]
- Belser, J.A.; Barclay, W.; Barr, I.; Fouchier, R.A.; Matsuyama, R.; Nishiura, H.; Peiris, M.; Russell, C.J.; Subbarao, K.; Zhu, H.; et al. Ferrets as Models for Influenza Virus Transmission Studies and Pandemic Risk Assessments. Emerg. Infect. Dis. 2018, 24, 965–971. [Google Scholar] [CrossRef] [Green Version]
- Belser, J.A.; Eckert, A.M.; Huynh, T.; Gary, J.M.; Ritter, J.M.; Tumpey, T.M.; Maines, T.R. A Guide for the Use of the Ferret Model for Influenza Virus Infection. Am. J. Pathol. 2020, 190, 11–24. [Google Scholar] [CrossRef] [Green Version]
- Varble, A.; Albrecht, R.A.; Backes, S.; Crumiller, M.; Bouvier, N.M.; Sachs, D.; García-Sastre, A.; Tenoever, B.R. Influenza A Virus Transmission Bottlenecks Are Defined by Infection Route and Recipient Host. Cell Host Microbe 2014, 16, 691–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richard, M.; Brand, J.M.A.V.D.; Bestebroer, T.M.; Lexmond, P.; De Meulder, D.; Fouchier, R.A.M.; Lowen, A.C.; Herfst, S. Influenza A viruses are transmitted via the air from the nasal respiratory epithelium of ferrets. Nat. Commun. 2020, 11, 1–11. [Google Scholar] [CrossRef]
- Lakdawala, S.S.; Jayaraman, A.; Halpin, R.A.; Lamirande, E.W.; Shih, A.R.; Stockwell, T.B.; Lin, X.; Simenauer, A.; Hanson, C.T.; Vogel, L.; et al. The soft palate is an important site of adaptation for transmissible influenza viruses. Nature 2015, 526, 122–125. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, T.; Zhong, G.; Russell, C.A.; Nakajima, N.; Hatta, M.; Hanson, A.; McBride, R.; Burke, D.F.; Takahashi, K.; Fukuyama, S.; et al. Circulating Avian Influenza Viruses Closely Related to the 1918 Virus Have Pandemic Potential. Cell Host Microbe 2014, 15, 692–705. [Google Scholar] [CrossRef] [Green Version]
- Murakami, S.; Horimoto, T.; Ito, M.; Takano, R.; Katsura, H.; Shimojima, M.; Kawaoka, Y. Enhanced Growth of Influenza Vaccine Seed Viruses in Vero Cells Mediated by Broadening the Optimal pH Range for Virus Membrane Fusion. J. Virol. 2011, 86, 1405–1410. [Google Scholar] [CrossRef] [Green Version]
- Koerner, I.; Matrosovich, M.N.; Haller, O.; Staeheli, P.; Kochs, G. Altered receptor specificity and fusion activity of the haemagglutinin contribute to high virulence of a mouse-adapted influenza A virus. J. Gen. Virol. 2012, 93, 970–979. [Google Scholar] [CrossRef]
- Wörmann, X.; Lesch, M.; Welke, R.-W.; Okonechnikov, K.; Abdurishid, M.; Sieben, C.; Geissner, A.; Brinkmann, V.; Kästner, M.; Karner, A.; et al. Genetic characterization of an adapted pandemic 2009 H1N1 influenza virus that reveals improved replication rates in human lung epithelial cells. Virology 2016, 492, 118–129. [Google Scholar] [CrossRef] [Green Version]
- Cotter, C.R.; Jin, H.; Chen, Z. A Single Amino Acid in the Stalk Region of the H1N1pdm Influenza Virus HA Protein Affects Viral Fusion, Stability and Infectivity. PLoS Pathog. 2014, 10, e1003831. [Google Scholar] [CrossRef] [PubMed]
- Smeenk, C.A.; Wright, K.E.; Burns, B.F.; Thaker, A.J.; Brown, E.G. Mutations in the hemagglutinin and matrix genes of a virulent influenza virus variant, A/FM/1/47-MA, control different stages in pathogenesis. Virus Res. 1996, 44, 79–95. [Google Scholar] [CrossRef]
- Jakubcová, L.; Vozárová, M.; Hollý, J.; Tomčíková, K.; Fogelová, M.; Polčicová, K.; Kostolanský, F.; Fodor, E.; Varečková, E. Biological properties of influenza A virus mutants with amino acid substitutions in the HA2 glycoprotein of the HA1/HA2 interaction region. J. Gen. Virol. 2019, 100, 1282–1292. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.J.D.; Vijaykrishna, D.; Bahl, J.; Lycett, S.J.; Worobey, M.; Pybus, O.G.; Ma, S.K.; Cheung, C.L.; Raghwani, J.; Bhatt, S.; et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 2009, 459, 1122–1125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mena, I.; Nelson, M.I.; Quezada-Monroy, F.; Dutta, J.; Cortes-Fernández, R.; Lara-Puente, J.H.; Castro-Peralta, F.; Cunha, L.F.; Trovão, N.S.; Lozano-Dubernard, B.; et al. Origins of the 2009 H1N1 influenza pandemic in swine in Mexico. eLife 2016, 5, 5. [Google Scholar] [CrossRef]
- Neumann, G.; Noda, T.; Kawaoka, Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 2009, 459, 931–939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russier, M.; Yang, G.; Rehg, J.E.; Wong, S.-S.; Mostafa, H.H.; Fabrizio, T.P.; Barman, S.; Krauss, S.; Webster, R.G.; Webby, R.J.; et al. Molecular requirements for a pandemic influenza virus: An acid-stable hemagglutinin protein. Proc. Natl. Acad. Sci. USA 2016, 113, 1636–1641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singanayagam, A.; Zambon, M.; Barclay, W.S. Influenza Virus with Increased pH of Hemagglutinin Activation Has Improved Replication in Cell Culture but at the Cost of Infectivity in Human Airway Epithelium. J. Virol. 2019, 93, e00058-19. [Google Scholar] [CrossRef] [Green Version]
- Russier, M.; Yang, G.; Briard, B.; Meliopoulos, V.; Cherry, S.; Kanneganti, T.D.; Schultz-Cherry, S.; Vogel, P.; Russell, C.J. HA stability regulates H1N1 influenza virus replication and pathogenicity in mice by modulating type I interferon responses in dendritic cells. J. Virol. 2019. [Google Scholar] [CrossRef]
- Cho, K.J.; Lee, J.-H.; Hong, K.W.; Kim, S.-H.; Park, Y.; Lee, J.Y.; Kang, S.; Kim, S.; Yang, J.H.; Kim, E.-K.; et al. Insight into structural diversity of influenza virus haemagglutinin. J. Gen. Virol. 2013, 94, 1712–1722. [Google Scholar] [CrossRef]
- Yang, H.; Chang, J.C.; Guo, Z.; Carney, P.J.; Shore, D.A.; Donis, R.O.; Cox, N.J.; Villanueva, J.M.; Klimov, A.I.; Stevens, J. Structural Stability of Influenza A(H1N1)pdm09 Virus Hemagglutinins. J. Virol. 2014, 88, 4828–4838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seok, J.H.; Kim, J.; Lee, D.B.; Cho, K.J.; Lee, J.-H.; Bae, G.; Chung, M.S.; Kim, K.H. Conformational modulation of influenza virus hemagglutinin: Characterization and in vivo efficacy of monomeric form. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Jiménez-Alberto, A.; Alvarado-Facundo, E.; Ribas-Aparicio, R.M.; Castelán-Vega, J.A. Analysis of Adaptation Mutants in the Hemagglutinin of the Influenza A(H1N1)pdm09 Virus. PLoS ONE 2013, 8, e70005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maurer-Stroh, S.; Lee, R.T.C.; Eisenhaber, F.; Cui, L.; Phuah, S.P.; Lin, R.T. A new common mutation in the hemagglutinin of the 2009 (H1N1) influenza A virus. PLoS Curr. 2010, 2, RRN1162. [Google Scholar] [CrossRef]
- Ribas-Aparicio, R.M.; Castelan-Vega, J.A.; Jiménez-Alberto, A.; Magaña-Hernández, A. The hemagglutinin of the influenza A(H1N1)pdm09 is mutating towards stability. Adv. Appl. Bioinform. Chem. 2014, 7, 37–44. [Google Scholar] [CrossRef] [Green Version]
- Klein, E.Y.; Blumenkrantz, D.; Serohijos, A.; Shakhnovich, E.; Choi, J.-M.; Rodrigues, J.V.; Smith, B.D.; Lane, A.P.; Feldman, A.; Pekosz, A. Stability of the Influenza Virus Hemagglutinin Protein Correlates with Evolutionary Dynamics. mSphere 2018, 3, e00554-17. [Google Scholar] [CrossRef] [Green Version]
- Nieto, A.; Vasilijevic, J.; Santos, N.B.; Zamarreño, N.; López, P.; Amorim, M.J.; Falcon, A. Mutation S110L of H1N1 Influenza Virus Hemagglutinin: A Potent Determinant of Attenuation in the Mouse Model. Front. Immunol. 2019, 10, 132. [Google Scholar] [CrossRef] [Green Version]
- Parker, L.; Ritter, L.; Wu, W.; Maeso, R.; Bright, H.; Dibben, O. Haemagglutinin stability was not the primary cause of the reduced effectiveness of live attenuated influenza vaccine against A/H1N1pdm09 viruses in the 2013–2014 and 2015–2016 seasons. Vaccine 2019, 37, 4543–4550. [Google Scholar] [CrossRef]
- Cline, T.D.; Beck, D.; Bianchini, E. Influenza virus replication in macrophages: Balancing protection and pathogenesis. J. Gen. Virol. 2017, 98, 2401–2412. [Google Scholar] [CrossRef] [PubMed]
- Cline, T.D.; Karlsson, E.A.; Seufzer, B.J.; Schultz-Cherry, S. The Hemagglutinin Protein of Highly Pathogenic H5N1 Influenza Viruses Overcomes an Early Block in the Replication Cycle To Promote Productive Replication in Macrophages. J. Virol. 2012, 87, 1411–1419. [Google Scholar] [CrossRef] [Green Version]
- Marvin, S.A.; Russier, M.; Huerta, C.T.; Russell, C.J.; Schultz-Cherry, S. Influenza Virus Overcomes Cellular Blocks To Productively Replicate, Impacting Macrophage Function. J. Virol. 2016, 91, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dash, P.; Thomas, P.G. Host Detection and the Stealthy Phenotype in Influenza Virus Infection. In Influenza Pathogenesis and Control—Vol Ii; Oldstone, M.B.A., Compans, R.W., Eds.; Springer: Berlin, Germany, 2015; Volume 386, pp. 121–147. [Google Scholar]
- Labadie, T.; Batéjat, C.; Manuguerra, J.-C.; Leclercq, I. Influenza Virus Segment Composition Influences Viral Stability in the Environment. Front. Microbiol. 2018, 9, 1496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singanayagam, A.; Zhou, J.; Elderfield, R.A.; Frise, R.; Ashcroft, J.; Galiano, M.; Miah, S.; Nicolaou, L.; Barclay, W.S. Characterising viable virus from air exhaled by H1N1 influenza-infected ferrets reveals the importance of haemagglutinin stability for airborne infectivity. PLoS Pathog. 2020, 16, e1008362. [Google Scholar] [CrossRef]
- Kormuth, K.A.; Lin, K.; Prussin, A.J., II; Vejerano, E.P.; Tiwari, A.J.; Cox, S.S.; Myerburg, M.M.; Lakdawala, S.S.; Marr, L.C. Influenza Virus Infectivity Is Retained in Aerosols and Droplets Independent of Relative Humidity. J. Infect. Dis. 2018, 218, 739–747. [Google Scholar] [CrossRef]
- Kormuth, K.A.; Lin, K.; Qian, Z.; Myerburg, M.M.; Marr, L.C.; Lakdawala, S.S. Environmental Persistence of Influenza Viruses Is Dependent upon Virus Type and Host Origin. mSphere 2019, 4, e00552-19. [Google Scholar] [CrossRef] [Green Version]
- Marr, L.C.; Tang, J.W.; Van Mullekom, J.; Lakdawala, S.S. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface 2019, 16, 20180298. [Google Scholar] [CrossRef]
- Russier, M.; Yang, G.; Marinova-Petkova, A.; Vogel, P.; Kaplan, B.S.; Webby, R.J.; Russell, C.J. H1N1 influenza viruses varying widely in hemagglutinin stability transmit efficiently from swine to swine and to ferrets. PLoS Pathog. 2017, 13, e1006276. [Google Scholar] [CrossRef] [Green Version]
- Pulit-Penaloza, J.A.; Pappas, C.; Belser, J.A.; Sun, X.; Brock, N.; Zeng, H.; Tumpey, T.M.; Maines, T.R. Comparative In Vitro and In Vivo Analysis of H1N1 and H1N2 Variant Influenza Viruses Isolated from Humans between 2011 and 2016. J. Virol. 2018, 92, e01444-18. [Google Scholar] [CrossRef] [Green Version]
- Pulit-Penaloza, J.A.; Belser, J.A.; Tumpey, T.M.; Maines, T.R. Swine-Origin H1 Influenza Viruses Isolated from Humans Exhibit Sustained Infectivity in an Aerosol State. Appl. Environ. Microbiol. 2019, 85, 10. [Google Scholar] [CrossRef]
- Hu, M.; Yang, G.; DeBeauchamp, J.; Crumpton, J.C.; Kim, H.; Li, L.; Wan, X.F.; Kercher, L.; Bowman, A.S.; Webster, R.G.; et al. HA stabilization promotes replication and transmission of swine H1N1 gamma influenza viruses in ferrets. Elife 2020, 9, e56236. [Google Scholar] [CrossRef]
- Baumann, J.; Kouassi, N.M.; Foni, E.; Klenk, H.-D.; Matrosovich, M. H1N1 Swine Influenza Viruses Differ from Avian Precursors by a Higher pH Optimum of Membrane Fusion. J. Virol. 2015, 90, 1569–1577. [Google Scholar] [CrossRef] [Green Version]
- Koçer, Z.A.; Obenauer, J.; Zaraket, H.; Zhang, J.; Rehg, J.E.; Russell, C.J.; Webster, R.G. Fecal Influenza in Mammals: Selection of Novel Variants. J. Virol. 2013, 87, 11476–11486. [Google Scholar] [CrossRef] [Green Version]
- Bourret, V.; Lyall, J.; Frost, S.D.W.; Teillaud, A.; Smith, C.A.; LeClaire, S.; Fu, J.; Gandon, S.; Guérin, J.-L.; Tiley, L.S. Adaptation of avian influenza virus to a swine host. Virus Evol. 2017, 3, vex007. [Google Scholar] [CrossRef] [PubMed]
- Shelton, H.; Roberts, K.L.; Molesti, E.; Temperton, N.; Barclay, W.S. Mutations in haemagglutinin that affect receptor binding and pH stability increase replication of a PR8 influenza virus with H5 HA in the upper respiratory tract of ferrets and may contribute to transmissibility. J. Gen. Virol. 2013, 94, 1220–1229. [Google Scholar] [CrossRef]
- Zaraket, H.; Bridges, O.A.; Duan, S.; Baranovich, T.; Yoon, S.-W.; Reed, M.L.; Salomon, R.; Webby, R.J.; Webster, R.G.; Russell, C.J. Increased Acid Stability of the Hemagglutinin Protein Enhances H5N1 Influenza Virus Growth in the Upper Respiratory Tract but Is Insufficient for Transmission in Ferrets. J. Virol. 2013, 87, 9911–9922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negovetich, N.J.; Webster, R.G. Thermostability of Subpopulations of H2N3 Influenza Virus Isolates from Mallard Ducks. J. Virol. 2010, 84, 9369–9376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez-Sobrido, L.; Blanco-Lobo, P.; Rodriguez, L.; Fitzgerald, T.; Zhang, H.; Nguyen, P.; Anderson, C.S.; Holden-Wiltse, J.; Bandyopadhyay, S.; Nogales, A.; et al. Characterizing Emerging Canine H3 Influenza Viruses. PLoS Pathog. 2020, 16, e1008409. [Google Scholar] [CrossRef]
- Lin, Y.P.; Wharton, S.A.; Martín, J.; Skehel, J.J.; Wiley, D.C.; Steinhauer, D.A. Adaptation of Egg-Grown and Transfectant Influenza Viruses for Growth in Mammalian Cells: Selection of Hemagglutinin Mutants with Elevated pH of Membrane Fusion. Virology 1997, 233, 402–410. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.M.; Huddleston, J.; Doud, M.B.; Hooper, K.A.; Wu, N.C.; Bedford, T.; Bloom, J.D. Deep mutational scanning of hemagglutinin helps predict evolutionary fates of human H3N2 influenza variants. Proc. Natl. Acad. Sci. USA 2018, 115, E8276–E8285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Sage, V.; Kormuth, K.A.; Nturibi, E.; Lee, J.M.; Frizzell, S.A.; M’yerburg, M.M.; Bloom, J.D.; Lakdawala, S.S. Cell-culture adaptation of H3N2 influenza virus impacts acid stability and reduces airborne transmission in ferret model. Viruses 2021, 13, 719. [Google Scholar] [CrossRef]
- Sun, X.; Pulit-Penaloza, J.A.; Belser, J.A.; Pappas, C.; Pearce, M.B.; Brock, N.; Zeng, H.; Creager, H.M.; Zanders, N.; Jang, Y.; et al. Pathogenesis and Transmission of Genetically Diverse Swine-Origin H3N2 Variant Influenza A Viruses from Multiple Lineages Isolated in the United States, 2011–2016. J. Virol. 2018, 92, e00665-18. [Google Scholar] [CrossRef] [Green Version]
- Belser, J.A.; Tumpey, T.M. H5N1 pathogenesis studies in mammalian models. Virus Res. 2013, 178, 168–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, R.; Martin, A.C.R.; Zambon, M.; Barclay, W.S. Restrictions to the Adaptation of Influenza A Virus H5 Hemagglutinin to the Human Host. J. Virol. 2004, 78, 502–507. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, Y.; Arai, Y.; Daidoji, T.; Kawashita, N.; Ibrahim, M.S.; El-Gendy, E.E.-D.M.; Hiramatsu, H.; Kubota-Koketsu, R.; Takagi, T.; Murata, T.; et al. Characterization of H5N1 Influenza Virus Variants with Hemagglutinin Mutations Isolated from Patients. mBio 2015, 6, e00081-15. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, Y.; Arai, Y.; Kawashita, N.; Ibrahim, M.S.; Elgendy, E.M.; Daidoji, T.; Kajikawa, J.; Hiramatsu, H.; Sriwilaijaroen, N.; Ono, T.; et al. Characterization of H5N1 Influenza Virus Quasispecies with Adaptive Hemagglutinin Mutations from Single-Virus Infections of Human Airway Cells. J. Virol. 2018, 92, e02004-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hulse, D.J.; Webster, R.G.; Russell, R.J.; Perez, D.R. Molecular Determinants within the Surface Proteins Involved in the Pathogenicity of H5N1 Influenza Viruses in Chickens. J. Virol. 2004, 78, 9954–9964. [Google Scholar] [CrossRef] [Green Version]
- Reed, M.L.; Yen, H.-L.; Dubois, R.M.; Bridges, O.A.; Salomon, R.; Webster, R.G.; Russell, C.J. Amino Acid Residues in the Fusion Peptide Pocket Regulate the pH of Activation of the H5N1 Influenza Virus Hemagglutinin Protein. J. Virol. 2009, 83, 3568–3580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaraket, H.; Baranovich, T.; Kaplan, B.S.; Carter, R.; Song, M.-S.; Paulson, J.C.; Rehg, J.E.; Bahl, J.; Crumpton, J.C.; Seiler, J.; et al. Mammalian adaptation of influenza A(H7N9) virus is limited by a narrow genetic bottleneck. Nat. Commun. 2015, 6, 6553. [Google Scholar] [CrossRef] [PubMed]
- Zaraket, H.; Bridges, O.A.; Russell, C.J. The pH of Activation of the Hemagglutinin Protein Regulates H5N1 Influenza Virus Replication and Pathogenesis in Mice. J. Virol. 2013, 87, 4826–4834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krenn, B.M.; Egorov, A.; Romanovskaya-Romanko, E.; Wolschek, M.; Nakowitsch, S.; Ruthsatz, T.; Kiefmann, B.; Morokutti, A.; Humer, J.; Geiler, J.; et al. Single HA2 Mutation Increases the Infectivity and Immunogenicity of a Live Attenuated H5N1 Intranasal Influenza Vaccine Candidate Lacking NS1. PLoS ONE 2011, 6, e18577. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.; Herfst, S.; Brand, J.M.A.V.D.; De Meulder, D.; Lexmond, P.; Bestebroer, T.M.; Fouchier, R.A.M. Mutations Driving Airborne Transmission of A/H5N1 Virus in Mammals Cause Substantial Attenuation in Chickens only when combined. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Daidoji, T.; Watanabe, Y.; Ibrahim, M.S.; Yasugi, M.; Maruyama, H.; Masuda, T.; Arai, F.; Ohba, T.; Honda, A.; Ikuta, K.; et al. Avian Influenza Virus Infection of Immortalized Human Respiratory Epithelial Cells Depends upon a Delicate Balance between Hemagglutinin Acid Stability and Endosomal pH. J. Biol. Chem. 2015, 290, 10627–10642. [Google Scholar] [CrossRef] [Green Version]
- Daidoji, T.; Kajikawa, J.; Arai, Y.; Watanabe, Y.; Hirose, R.; Nakaya, T. Infection of Human Tracheal Epithelial Cells by H5 Avian Influenza Virus Is Regulated by the Acid Stability of Hemagglutinin and the pH of Target Cell Endosomes. Viruses 2020, 12, 82. [Google Scholar] [CrossRef] [Green Version]
- Imai, H.; Dinis, J.M.; Zhong, G.; Moncla, L.H.; Lopes, T.J.; McBride, R.; Thompson, A.J.; Peng, W.; Le, M.T.Q.; Hanson, A.; et al. Diversity of Influenza A(H5N1) Viruses in Infected Humans, Northern Vietnam, 2004–2010. Emerg. Infect. Dis. 2018, 24, 1128–1238. [Google Scholar] [CrossRef] [PubMed]
- Rudneva, I.A.; Timofeeva, T.A.; Ignatieva, A.V.; Shilov, A.A.; Krylov, P.S.; Ilyushina, N.A.; Kaverin, N.V. Pleiotropic effects of hemagglutinin amino acid substitutions of H5 influenza escape mutants. Virology 2013, 447, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Song, H.S.; Keller, P.W.; Alvarado-Facundo, E.; Vassell, R.; Weiss, C.D. Conformational Stability of the Hemagglutinin of H5N1 Influenza A Viruses Influences Susceptibility to Broadly Neutralizing Stem Antibodies. J. Virol. 2018, 92, e00247-18. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.-H.; Torchetti, M.K.; Winker, K.; Ip, H.S.; Song, C.-S.; Swayne, D.E. Intercontinental Spread of Asian-Origin H5N8 to North America through Beringia by Migratory Birds. J. Virol. 2015, 89, 6521–6524. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, B.S.; Russier, M.; Jeevan, T.; Marathe, B.; Govorkova, E.A.; Russell, C.J.; Kim-Torchetti, M.; Choi, Y.K.; Brown, I.; Saito, T.; et al. Novel Highly Pathogenic Avian A(H5N2) and A(H5N8) Influenza Viruses of Clade 2.3.4.4 from North America Have Limited Capacity for Replication and Transmission in Mammals. mSphere 2016, 1, e00003-16. [Google Scholar] [CrossRef] [Green Version]
- Yu, Z.; Cheng, K.; Sun, W.; Zhang, X.; Xia, X.; Gao, Y. PB2 and HA mutations increase the virulence of highly pathogenic H5N5 clade 2.3.4.4 avian influenza virus in mice. Arch. Virol. 2017, 163, 401–410. [Google Scholar] [CrossRef]
- Herfst, S.; Mok, C.K.P.; Brand, J.M.A.V.D.; Van Der Vliet, S.; Rosu, M.E.; Spronken, M.I.; Yang, Z.; De Meulder, D.; Lexmond, P.; Bestebroer, T.M.; et al. Human Clade 2.3.4.4 A/H5N6 Influenza Virus Lacks Mammalian Adaptation Markers and Does Not Transmit via the Airborne Route between Ferrets. mSphere 2018, 3, e00405-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohuchi, M.; Cramer, A.; Vey, M.; Ohuchi, R.; Garten, W.; Klenk, H.D. Rescue of vector-expressed fowl plague virus hemagglutinin in biologically active form by acidotropic agents and coexpressed M2 protein. J. Virol. 1994, 68, 920–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutton, T.C.; Finch, C.; Shao, H.; Angel, M.; Chen, H.; Capua, I.; Cattoli, G.; Monne, I.; Perez, D.R. Airborne Transmission of Highly Pathogenic H7N1 Influenza Virus in Ferrets. J. Virol. 2014, 88, 6623–6635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanton, L.; Mustaquim, D.; Alabi, N.; Kniss, K.; Kramer, N.; Budd, A.; Garg, S.; Cummings, C.N.; Fry, A.M.; Bresee, J.; et al. Update: Influenza Activity—United States, October 2, 2016-February 4, 2017. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 159–166. [Google Scholar] [CrossRef] [Green Version]
- Belser, J.A.; Pulit-Penaloza, J.A.; Sun, X.; Brock, N.; Pappas, C.; Creager, H.M.; Zeng, H.; Tumpey, T.M.; Maines, T.R. A Novel A(H7N2) Influenza Virus Isolated from a Veterinarian Caring for Cats in a New York City Animal Shelter Causes Mild Disease and Transmits Poorly in the Ferret Model. J. Virol. 2017, 91, e00672-17. [Google Scholar] [CrossRef] [Green Version]
- Gao, R.; Cao, B.; Hu, Y.; Feng, Z.; Wang, D.; Hu, W.; Chen, J.; Jie, Z.; Qiu, H.; Xu, K.; et al. Human Infection with a Novel Avian-Origin Influenza A (H7N9) Virus. N. Engl. J. Med. 2013, 368, 1888–1897. [Google Scholar] [CrossRef] [Green Version]
- Shi, J.; Deng, G.; Ma, S.; Zeng, X.; Yin, X.; Li, M.; Zhang, B.; Cui, P.; Chen, Y.; Yang, H.; et al. Rapid Evolution of H7N9 Highly Pathogenic Viruses that Emerged in China in 2017. Cell Host Microbe 2018, 24, 558–568.e7. [Google Scholar] [CrossRef] [Green Version]
- Gabbard, J.D.; Dlugolenski, D.; Van Riel, D.; Marshall, N.; Galloway, S.E.; Howerth, E.W.; Campbell, P.J.; Jones, C.; Johnson, S.; Byrd-Leotis, L.; et al. Novel H7N9 Influenza Virus Shows Low Infectious Dose, High Growth Rate, and Efficient Contact Transmission in the Guinea Pig Model. J. Virol. 2013, 88, 1502–1512. [Google Scholar] [CrossRef] [Green Version]
- Richard, M.; Schrauwen, E.J.A.; De Graaf, M.; Bestebroer, T.M.; Spronken, M.I.J.; Van Boheemen, S.; De Meulder, D.; Lexmond, P.; Linster, M.; Herfst, S.; et al. Limited airborne transmission of H7N9 influenza A virus between ferrets. Nature 2013, 501, 560–563. [Google Scholar] [CrossRef] [Green Version]
- Imai, M.; Watanabe, T.; Kiso, M.; Nakajima, N.; Yamayoshi, S.; Iwatsuki-Horimoto, K.; Hatta, M.; Yamada, S.; Ito, M.; Sakai-Tagawa, Y.; et al. A Highly Pathogenic Avian H7N9 Influenza Virus Isolated from A Human Is Lethal in Some Ferrets Infected via Respiratory Droplets. Cell Host Microbe 2017, 22, 615–626.e8. [Google Scholar] [CrossRef] [Green Version]
- Schrauwen, E.J.; Richard, M.; Burke, D.F.; Rimmelzwaan, G.F.; Herfst, S.; Fouchier, R.A. Amino acid substitutions that affect feceptor binding and stability of the hemagglutinin of influenza A/H7N9 virus. J. Virol. 2016, 90, 3794–3799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiong, X.; Martin, S.R.; Haire, L.F.; Wharton, S.A.; Daniels, R.S.; Bennett, M.S.; McCauley, J.W.; Collins, P.J.; Walker, P.A.; Skehel, J.J.; et al. Receptor binding by an H7N9 influenza virus from humans. Nature 2013, 499, 496–499. [Google Scholar] [CrossRef] [PubMed]
- Belser, J.A.; Creager, H.M.; Sun, X.; Gustin, K.M.; Jones, T.; Shieh, W.-J.; Maines, T.R.; Tumpey, T.M. Mammalian Pathogenesis and Transmission of H7N9 Influenza Viruses from Three Waves, 2013–2015. J. Virol. 2016, 90, 4647–4657. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, X.; Belser, J.A.; Pappas, C.; Pulit-Penaloza, J.A.; Brock, N.; Zeng, H.; Creager, H.M.; Le, S.; Wilson, M.; Lewis, A.; et al. Risk Assessment of Fifth-Wave H7N9 Influenza A Viruses in Mammalian Models. J. Virol. 2019, 93, e01740-18. [Google Scholar] [CrossRef] [Green Version]
- Chang, P.; Sealy, J.E.; Sadeyen, J.-R.; Bhat, S.; Lukosaityte, D.; Sun, Y.; Iqbal, M. Immune Escape Adaptive Mutations in the H7N9 Avian Influenza Hemagglutinin Protein Increase Virus Replication Fitness and Decrease Pandemic Potential. J. Virol. 2020, 94, 19. [Google Scholar] [CrossRef]
- Homme, P.J.; Easterday, B.C. Avian influenza virus infections. I. Characteristics of influenza A-turkey-Wisconsin-1966 virus. Avian Dis. 1970, 14, 66–74. [Google Scholar] [CrossRef]
- Jackwood, M.W.; Stallknecht, D.E. Molecular epidemiologic studies on North American H9 avian influenza virus isolates from waterfowl and shorebirds. Avian Dis. 2007, 51, 448–450. [Google Scholar] [CrossRef]
- Sharp, G.B.; Kawaoka, Y.; Jones, D.J.; Bean, W.J.; Pryor, S.P.; Hinshaw, V.; Webster, R.G. Coinfection of wild ducks by influenza A viruses: Distribution patterns and biological significance. J. Virol. 1997, 71, 6128–6135. [Google Scholar] [CrossRef] [Green Version]
- Cameron, K.; Gregory, V.; Banks, J.; Brown, I.; Alexander, D.; Hay, A.; Lin, Y. H9N2 Subtype Influenza A Viruses in Poultry in Pakistan Are Closely Related to the H9N2 Viruses Responsible for Human Infection in Hong Kong. Virology 2000, 278, 36–41. [Google Scholar] [CrossRef] [Green Version]
- Choi, Y.K.; Ozaki, H.; Webby, R.J.; Webster, R.G.; Peiris, J.S.; Poon, L.; Butt, C.; Leung, Y.H.C.; Guan, Y. Continuing Evolution of H9N2 Influenza Viruses in Southeastern China. J. Virol. 2004, 78, 8609–8614. [Google Scholar] [CrossRef] [Green Version]
- Nili, H.; Asasi, K. Natural cases and an experimental study of H9N2 avian influenza in commercial broiler chickens of Iran. Avian Pathol. 2002, 31, 247–252. [Google Scholar] [CrossRef]
- Peiris, M.; Yuen, K.; Leung, C.; Chan, K.; Ip, P.; Lai, R.; Orr, W.; Shortridge, K. Human infection with influenza H9N2. Lancet 1999, 354, 916–917. [Google Scholar] [CrossRef]
- Sun, X.; Belser, J.A.; Maines, T.R. Adaptation of H9N2 Influenza Viruses to Mammalian Hosts: A Review of Molecular Markers. Viruses 2020, 12, 541. [Google Scholar] [CrossRef]
- Liu, S.; Zhuang, Q.; Wang, S.; Jiang, W.; Jin, J.; Peng, C.; Hou, G.; Li, J.; Yu, J.; Yu, X.; et al. Control of avian influenza in China: Strategies and lessons. Transbound. Emerg. Dis. 2020, 67, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- Group, S.H.W. Assessing the fitness of distinct clades of influenza A (H9N2) viruses. Emerg. Microbes Infect. 2013, 2, e75. [Google Scholar]
- Peacock, T.P.; Benton, D.J.; Sadeyen, J.R.; Chang, P.; Sealy, J.E.; Bryant, J.E.; Martin, S.R.; Shelton, H.; McCauley, J.W.; Barclay, W.S.; et al. Variability in H9N2 haemagglutinin receptor-binding preference and the pH of fusion. Emerg. Microbes Infect. 2017, 6, e11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belser, J.A.; Sun, X.; Brock, N.; Pappas, C.; Pulit-Penaloza, J.A.; Zeng, H.; Jang, Y.; Jones, J.; Carney, P.J.; Chang, J.; et al. Genetically and Antigenically Divergent Influenza A(H9N2) Viruses Exhibit Differential Replication and Transmission Phenotypes in Mammalian Models. J. Virol. 2020, 94, 17. [Google Scholar] [CrossRef] [PubMed]
- Sang, X.; Wang, A.; Ding, J.; Kong, H.; Gao, X.; Li, L.; Chai, T.; Li, Y.; Zhang, K.; Wang, C.; et al. Adaptation of H9N2 AIV in guinea pigs enables efficient transmission by direct contact and inefficient transmission by respiratory droplets. Sci. Rep. 2015, 5, 15928. [Google Scholar] [CrossRef] [Green Version]
- Zhong, L.; Wang, X.; Li, Q.; Liu, D.; Chen, H.; Zhao, M.; Gu, X.; He, L.; Liu, X.; Gu, M.; et al. Molecular Mechanism of the Airborne Transmissibility of H9N2 Avian Influenza A Viruses in Chickens. J. Virol. 2014, 88, 9568–9578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rudneva, I.A.; Timofeeva, T.A.; Ignatieva, A.V.; Shilov, A.A.; Ilyushina, N.A. Effects of hemagglutinin amino acid substitutions in H9 influenza A virus escape mutants. Arch. Virol. 2016, 161, 3515–3520. [Google Scholar] [CrossRef] [PubMed]
- Zohari, S.; Neimanis, A.; Härkönen, T.; Moraeus, C.; Valarcher, J.F. Avian influenza A(H10N7) virus involvement in mass mortality of harbour seals (Phoca vitulina) in Sweden, March through October 2014. Eurosurveillance 2014, 19, 20967. [Google Scholar] [CrossRef] [PubMed]
- Dittrich, A.; Scheibner, D.; Salaheldin, A.H.; Veits, J.; Gischke, M.; Mettenleiter, T.C.; Abdelwhab, E.M. Impact of Mutations in the Hemagglutinin of H10N7 Viruses Isolated from Seals on Virus Replication in Avian and Human Cells. Viruses 2018, 10, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herfst, S.; Zhang, J.; Richard, M.; McBride, R.; Lexmond, P.; Bestebroer, T.M.; Spronken, M.I.; De Meulder, D.; Brand, J.M.V.D.; Rosu, M.E.; et al. Hemagglutinin Traits Determine Transmission of Avian A/H10N7 Influenza Virus between Mammals. Cell Host Microbe 2020, 28, 602–613.e7. [Google Scholar] [CrossRef]

| Strain | Activation pH | Phenotype | Reference |
|---|---|---|---|
| A/Hamburg/04/2009 HA2-I91L | 5.9 | ↑ growth A549 | [145] |
| A/Hamburg/04/2009 WT | 5.7 | -- | |
| (A/Ann Arbor/6/60 ca) A/California/7/2009 HA WT | 5.5 | -- | [146] |
| (A/Ann Arbor/6/60 ca) A/California/7/2009 HA2-E47K | 5.3 | ↓ growth Vero, = growth MDCK | |
| (A/Ann Arbor/6/60 ca) A/Brisbane/10/2010 HA2-K47E | 5.5 | ↑ growth Vero, = growth MDCK | [146] |
| (A/Ann Arbor/6/60 ca) A/Brisbane/10/2010 HA WT | 5.3 | -- | |
| A/Puerto Rico/8/34 HA2-N117D | 5.4 | ↑ growth Vero, = growth MDCK | [143] |
| A/Puerto Rico/8/34 WT | 5.2 | -- |
| Strain | Activation pH | Phenotype | Reference |
|---|---|---|---|
| A/Tennessee/1-560/2009 HA1-Y17H | 6.0 | ↓↓ virulence in mice | [152,154] |
| A/Tennessee/1-560/2009 WT | 5.5 | -- | |
| A/Tennessee/1-560/2009 HA2-R106K | 5.3 | ↓ virulence in mice | |
| A/England/195/2009 HA1-Y17H | 5.9 | ↓↓ virulence in mice | [153] |
| A/England/195/2009 HA1-A19T | 5.8 | ↓ virulence in mice | |
| A/England/195/2009 WT | 5.5 | -- | |
| A/England/195/2009 HA1-E31K | 5.3 | ↓ virulence in mice | |
| A/FM/1/47 | 5.7 | -- | [147] |
| A/FM/1/47 HA2-W47G | 5.5 | ↑ virulence in mice | |
| A/Puerto Rico/8/34 HA1-P78L, HA2-H25Q | 5.5 | ↑ virulence in mice | [144] |
| A/Puerto Rico/8/34 | 5.3 | -- | |
| A/WSN/33 (H1N1) WT | 5.4 | -- | [148] |
| A/WSN/33 (H1N1) HA2-T64H, HA2-V66H | 5.2 | ↓ virulence in mice |
| Strain | Activation pH | Low-MOI Phenotype | High-MOI Phenotype | Reference |
|---|---|---|---|---|
| TN09 HA1-Y17H | 6.0 | ↓ growth mNEC, mTEC | ↑ growth MDCK, A549, RAW 264.7 | [152,154] |
| TN09 WT | 5.5 | -- | ||
| ENG09 HA1-Y17H | 5.9 | ↓↓ growth HAE | ↑ growth MDCK, A549 | [153] |
| ENG09 HA1-A19T | 5.8 | ↓ growth HAE | ↑ growth MDCK, A549 | |
| ENG09 WT | 5.5 | -- | -- | |
| ENG09 HA1-E31K | 5.3 | = growth HAE | = growth MDCK, A549 |
| Virus | Activation pH | Nasal Growth in Inoculated | Airborne Transmission | Variant Transmission | Transmitted Variant |
|---|---|---|---|---|---|
| TN09 HA1-Y17H | 6.0 | ↓ growth; delayed | 0/4 | 1/4 | HA1-H17Y/HA2-R106K (pH 5.3) |
| TN09 WT | 5.5 | -- | 4/4 | -- | -- |
| Virus | Activation pH | Nasal Growth in Inoculated Ferrets | Delay in Peak Shedding | Air-Emitted Virus Plaques | Variants in Donor Ferrets and in Emitted Virus Recovered |
|---|---|---|---|---|---|
| ENG09 HA1-Y17H | 5.9 | Similar A.U.C. | 1 day | 23 | HA1-H17Y, HA2-V55I, HA2-E47K, HA1-V29I |
| ENG09 HA1-E31K | 5.3 | Similar A.U.C. | -- | 184 | -- |
| Virus | Activation pH | Growth in Inoculated Swine | Contact Transmission to Swine | Airborne Transmission to Ferrets | Variants Transmitted to Ferrets | Transmitted Variants |
|---|---|---|---|---|---|---|
| TN09 HA1-Y17H | 6.0 | ↓ growth; delayed | 3/3; delayed | 0/3 | 3/3 | HA1-H17Y, HA2-V55I, HA2-R106K |
| TN09 WT | 5.5 | -- | 3/3 | 3/3 | -- | -- |
| TN09 HA2-R106K | 5.3 | WT-like | 3/3 | 3/3 | -- | -- |
| Virus | Activation pH | % of Inoculum | % 3d Post infection | Airborne Transmitted |
|---|---|---|---|---|
| A/sw/IL/2A-1213-G15/2013 HA1-N210 | 5.8 | ~85% | <10% | 0/3 |
| A/sw/IL/2A-1213-G15/2013 HA1-S210 | 5.5 | ~15% | >90% | 3/3 |
| Virus | Activation pH | Environmental Persistence, 28 °C | Growth, Morbidity, and Mortality in Mallards | Transmission in Mallards | Growth, Morbidity, and Mortality in Mice |
|---|---|---|---|---|---|
| CH58 HA1-Y17H | 6.3 | 61 d | ↓ | ↓ | ↓ |
| CH58 WT | 5.9 | 62 d | -- | -- | -- |
| CH58 HA1-H18Q | 5.6 | 77 d | WT-like | WT-like | WT-like |
| CH58 HA2-K58I | 5.4 | 79 d | ↓ | ↓ | ↑ |
| Virus | Activation pH | Receptor-Binding Specificity | Contact Transmission in Ferrets | Airborne Transmission in Ferrets | Transmitted Variants |
|---|---|---|---|---|---|
| WT | 5.6 | α2,3 | 0/3 | 0/3 | -- |
| N224K/Q226L | 5.8 | α2,6 | 0/3 | 0/3 | -- |
| N158D/N224K/Q226L | 5.8 | α2,6 | 5/6 | 0/6 | 2/6 (T318I) |
| N158D/N224K/Q226L/T318I | 5.4 | α2,6 | 5/6 | 4/6 | -- |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russell, C.J. Hemagglutinin Stability and Its Impact on Influenza A Virus Infectivity, Pathogenicity, and Transmissibility in Avians, Mice, Swine, Seals, Ferrets, and Humans. Viruses 2021, 13, 746. https://doi.org/10.3390/v13050746
Russell CJ. Hemagglutinin Stability and Its Impact on Influenza A Virus Infectivity, Pathogenicity, and Transmissibility in Avians, Mice, Swine, Seals, Ferrets, and Humans. Viruses. 2021; 13(5):746. https://doi.org/10.3390/v13050746
Chicago/Turabian StyleRussell, Charles J. 2021. "Hemagglutinin Stability and Its Impact on Influenza A Virus Infectivity, Pathogenicity, and Transmissibility in Avians, Mice, Swine, Seals, Ferrets, and Humans" Viruses 13, no. 5: 746. https://doi.org/10.3390/v13050746
APA StyleRussell, C. J. (2021). Hemagglutinin Stability and Its Impact on Influenza A Virus Infectivity, Pathogenicity, and Transmissibility in Avians, Mice, Swine, Seals, Ferrets, and Humans. Viruses, 13(5), 746. https://doi.org/10.3390/v13050746






