Serological Evidence of Filovirus Infection in Nonhuman Primates in Zambia
Abstract
:1. Introduction
2. Materials and Methods
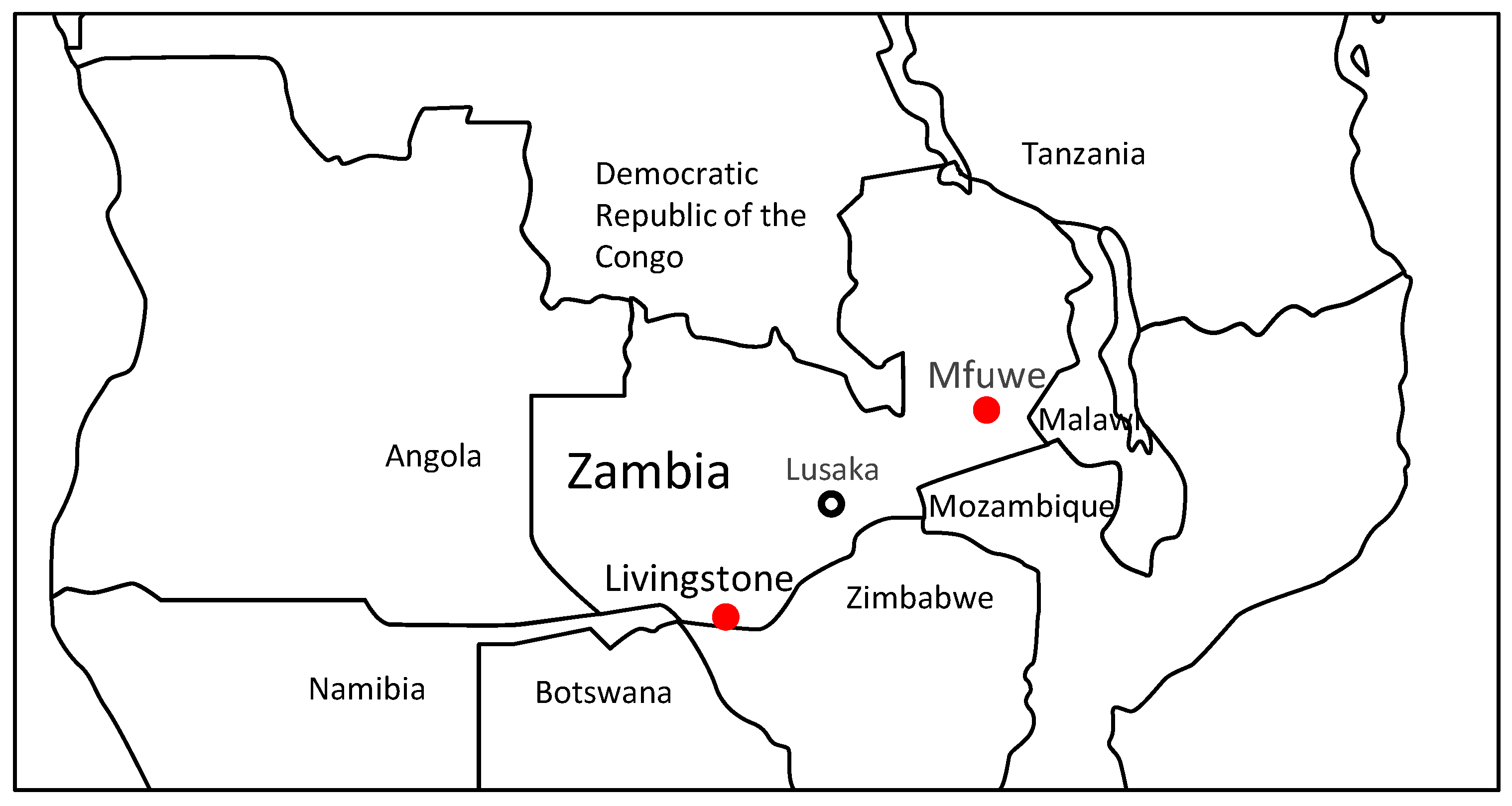
2.1. Animals and Serum Samples
2.2. Enzyme-Linked Immunosorbent Assay (ELISA)
2.3. Reverse Transcription Polymerase Chain Reaction (RT-PCR)
2.4. Statistics
3. Results and Discussion
3.1. Serological and Genetic Screening of NHPs for Filoviruses
3.2. Filoviruses-Species Specificity of Serum IgG Antibodies Detected in NHPs
3.3. Difference in the Seropositivity for MARV between Baboons and Vervet Monkeys
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kuhn, J.H.; Adkins, S.; Alioto, D.; Alkhovsky, S.V.; Amarasinghe, G.K.; Anthony, S.J.; Avšič-Županc, T.; Ayllón, M.A.; Bahl, J.; Balkema-Buschmann, A.; et al. 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales. Arch. Virol. 2020, 165, 3023–3072. [Google Scholar] [CrossRef]
- Feldmann, H.; Sanchez, A.; Geisbert, T.W. Filoviridae: Marburg and Ebola viruses. In Fields Virology, 6th ed.; Knipe, D.M., Howley, P.M., Cohen, J.I., Griffin, D.E., Lamb, R.A., Martin, M.A., Racaniello, V.R., Roizman, B., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; Volume 1, pp. 923–956. [Google Scholar]
- Barrette, R.W.; Metwally, S.A.; Rowland, J.M.; Xu, L.; Zaki, S.R.; Nichol, S.T.; Rollin, P.E.; Towner, J.S.; Shieh, W.J.; Batten, B.; et al. Discovery of swine as a host for the Reston ebolavirus. Science 2009, 325, 204–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jahrling, P.B.; Geisbert, T.W.; Dalgard, D.W.; Johnson, E.D.; Ksiazek, T.G.; Hall, W.C.; Peters, C.J. Preliminary report: Isolation of Ebola virus from monkeys imported to USA. Lancet 1990, 335, 502–505. [Google Scholar] [CrossRef]
- Formenty, P.; Boesch, C.; Wyers, M.; Steiner, C.; Donati, F.; Dind, F.; Walker, F.; Le, G.B. Ebola virus outbreak among wild chimpanzees living in a rain forest of Cote d’Ivoire. J. Infect. Dis. 1999, 179 (Suppl. 1), S120–S126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pourrut, X.; Kumulungui, B.; Wittmann, T.; Moussavou, G.; Delicat, A.; Yaba, P.; Nkoghe, D.; Gonzalez, J.P.; Leroy, E.M. The natural history of Ebola virus in Africa. Microbes. Infect. 2005, 7, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Leroy, E.M.; Rouquet, P.; Formenty, P.; Souquiere, S.; Kilbourne, A.; Froment, J.M.; Bermejo, M.; Smit, S.; Karesh, W.; Swanepoel, R.; et al. Multiple Ebola virus transmission events and rapid decline of central African wildlife. Science 2004, 303, 387–390. [Google Scholar] [CrossRef] [Green Version]
- Bermejo, M.; Rodriguez-Teijeiro, J.D.; Illera, G.; Barroso, A.; Vila, C.; Walsh, P.D. Ebola outbreak killed 5000 gorillas. Science 2006, 314, 1564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Guenno, B.; Formenty, P.; Wyers, M.; Gounon, P.; Walker, F.; Boesch, C. Isolation and partial characterisation of a new strain of Ebola virus. Lancet 1995, 345, 1271–1274. [Google Scholar] [CrossRef]
- Slenczka, W. Filovirus Research: How it Began. Curr. Top Microbiol. Immunol. 2017, 411, 3–21. [Google Scholar] [CrossRef]
- Leroy, E.M.; Telfer, P.; Kumulungui, B.; Yaba, P.; Rouquet, P.; Roques, P.; Gonzalez, J.P.; Ksiazek, T.G.; Rollin, P.E.; Nerrienet, E. A serological survey of Ebola virus infection in central African nonhuman primates. J. Infect. Dis. 2004, 190, 1895–1899. [Google Scholar] [CrossRef] [Green Version]
- Johnson, B.K.; Gitau, L.G.; Gichogo, A.; Tukei, P.M.; Else, J.G.; Suleman, M.A.; Kimani, R.; Sayer, P.D. Marburg, Ebola and Rift Valley Fever virus antibodies in East African primates. Trans. R. Soc. Trop. Med. Hyg. 1982, 76, 307–310. [Google Scholar] [CrossRef]
- Reed, P.E.; Mulangu, S.; Cameron, K.N.; Ondzie, A.U.; Joly, D.; Bermejo, M.; Rouquet, P.; Fabozzi, G.; Bailey, M.; Shen, Z.; et al. A new approach for monitoring ebolavirus in wild great apes. PLoS Negl. Trop. Dis. 2014, 8, e3143. [Google Scholar] [CrossRef] [PubMed]
- Ayouba, A.; Ahuka-Mundeke, S.; Butel, C.; Mbala, K.P.; Loul, S.; Tagg, N.; Villabona-Arenas, C.J.; Lacroix, A.; Ndimbo-Kumugo, S.P.; Keita, A.K.; et al. Extensive serological survey of multiple African nonhuman primate species reveals low prevalence of immunoglobulin G antibodies to 4 Ebola virus species. J. Infect. Dis. 2019, 220, 1599–1608. [Google Scholar] [CrossRef]
- Ogunro, B.N.; Olugasa, B.O.; Verschoor, E.J.; Olarinmoye, A.O.; Theyse, I.; Niphuis, H. Serological detection of Ebola virus exposures in native non-human primates of southern Nigeria. J. Epidemiol. Glob. Health 2018, 8, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Nidom, C.A.; Nakayama, E.; Nidom, R.V.; Alamudi, M.Y.; Daulay, S.; Dharmayanti, I.N.; Dachlan, Y.P.; Amin, M.; Igarashi, M.; Miyamoto, H.; et al. Serological evidence of Ebola virus infection in Indonesian orangutans. PLoS ONE 2012, 7, e40740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sasaki, M.; Ishii, A.; Orba, Y.; Thomas, Y.; Hang’ombe, B.M.; Moonga, L.; Mweene, A.S.; Ogawa, H.; Nakamura, I.; Kimura, T.; et al. Human parainfluenza virus type 3 in wild nonhuman primates, Zambia. Emerg. Infect. Dis. 2013, 19, 1500–1503. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Kobayashi, S.; Ishii, A.; Ogawa, H.; Nakamura, I.; Moonga, L.; Hang’ombe, B.M.; Mweene, A.S.; Thomas, Y.; Kimura, T.; et al. Identification of a novel polyomavirus from vervet monkeys in Zambia. J. Gen. Virol. 2013, 94 Pt 6, 1357–1364. [Google Scholar] [CrossRef]
- Nakayima, J.; Hayashida, K.; Nakao, R.; Ishii, A.; Ogawa, H.; Nakamura, I.; Moonga, L.; Hang’ombe, B.M.; Mweene, A.S.; Thomas, Y.; et al. Detection and characterization of zoonotic pathogens of free-ranging non-human primates from Zambia. Parasit. Vectors 2014, 7, 490. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, E.; Yokoyama, A.; Miyamoto, H.; Igarashi, M.; Kishida, N.; Matsuno, K.; Marzi, A.; Feldmann, H.; Ito, K.; Saijo, M.; et al. Enzyme-linked immunosorbent assay for detection of filovirus species-specific antibodies. Clin. Vaccine Immunol. 2010, 17, 1723–1728. [Google Scholar] [CrossRef] [Green Version]
- Ogawa, H.; Miyamoto, H.; Nakayama, E.; Yoshida, R.; Nakamura, I.; Sawa, H.; Ishii, A.; Thomas, Y.; Nakagawa, E.; Matsuno, K.; et al. Seroepidemiological prevalence of multiple species of filoviruses in fruit bats (Eidolon helvum) migrating in Africa. J. Infect. Dis. 2015, 212 (Suppl. 2), S101–S108. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Miyamoto, H.; Ebihara, H.; Ito, K.; Morikawa, S.; Feldmann, H.; Takada, A. Detection of all known filovirus species by reverse transcription-polymerase chain reaction using a primer set specific for the viral nucleoprotein gene. J. Virol. Methods 2011, 171, 310–313. [Google Scholar] [CrossRef] [Green Version]
- Broadhurst, M.J.; Brooks, T.J.; Pollock, N.R. Diagnosis of Ebola virus disease: Past, present, and future. Clin. Microbiol. Rev. 2016, 29, 773–793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher-Hoch, S.P.; Perez-Oronoz, G.I.; Jackson, E.L.; Hermann, L.M.; Brown, B.G. Filovirus clearance in non-human primates. Lancet 1992, 340, 451–453. [Google Scholar] [CrossRef]
- CDC. Chronology of Marburg Hemorrhagic Fever Outbreaks. Available online: http://www.cdc.gov/vhf/marburg/resources/outbreak-table.html (accessed on 18 April 2021).
- CDC. Chronology of Ebola Hemorrhagic Fever Outbreaks. Available online: http://www.cdc.gov/vhf/ebola/resources/outbreak-table.html (accessed on 18 April 2021).
- Carroll, S.A.; Towner, J.S.; Sealy, T.K.; McMullan, L.K.; Khristova, M.L.; Burt, F.J.; Swanepoel, R.; Rollin, P.E.; Nichol, S.T. Molecular evolution of viruses of the family Filoviridae based on 97 whole-genome sequences. J. Virol. 2013, 87, 2608–2616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Changula, K.; Kajihara, M.; Mori-Kajihara, A.; Eto, Y.; Miyamoto, H.; Yoshida, R.; Shigeno, A.; Hang’ombe, B.; Qiu, Y.; Mwizabi, D.; et al. Seroprevalence of filovirus infection of Rousettus aegyptiacus bats in Zambia. J. Infect. Dis. 2018, 218 (Suppl. 5), S312–S317. [Google Scholar] [CrossRef] [PubMed]
- Fisher-Hoch, S.P.; Brammer, T.L.; Trappier, S.G.; Hutwagner, L.C.; Farrar, B.B.; Ruo, S.L.; Brown, B.G.; Hermann, L.M.; Perez-Oronoz, G.I.; Goldsmith, C.S. Pathogenic potential of filoviruses: Role of geographic origin of primate host and virus strain. J. Infect. Dis. 1992, 166, 753–763. [Google Scholar] [CrossRef]
- Saj, T.L.; Sicotte, P.; Paterson, J.D. The conflict between vervet monkeys and farmers at the forest edge in Entebbe, Uganda. Afr. J. Ecol. 2001, 39, 159–199. [Google Scholar] [CrossRef]
- Healy, A.; Nijman, V. Pets and pests: Vervet monkey intake at a specialist South African rehabilitation centre. Anim. Welf. 2014, 23, 353–360. [Google Scholar] [CrossRef]
- Findlay, L.H.; Hill, R.A. Baboon and vervet monkey crop-foraging behaviors on a commercial South African farm: Preliminary implications for damage mitigation. Hum-Wildl. Interact. 2020, 14, 505–518. [Google Scholar] [CrossRef]
- Chomba, C.; Senzota, R.; Chabwela, H.; Mwitwa, J.; Nyirenda, V. Patterns of human-wildlife conflicts in Zambia, causes, consequences and management responses. J. Ecol. Nat. Environ. 2012, 4, 303–313. [Google Scholar] [CrossRef] [Green Version]
- Grobler, P.; Jacquier, M.; deNys, H.; Blair, M.; Whitten, P.L.; Turner, T.R. Primate sanctuaries, taxonomy and survival: A case study from South Africa. Ecol. Envir. Anthropol. 2006, 2, 12–15. [Google Scholar]
- Mulangu, S.; Alfonso, V.H.; Hoff, N.A.; Doshi, R.H.; Mulembakani, P.; Kisalu, N.K.; Okitolonda-Wemakoy, E.; Kebela, B.I.; Marcus, H.; Shiloach, J.; et al. Serologic evidence of ebolavirus infection in a population with no history of outbreaks in the Democratic Republic of the Congo. J. Infect. Dis. 2018, 217, 529–537. [Google Scholar] [CrossRef]
- Steffen, I.; Lu, K.; Yamamoto, L.K.; Hoff, N.A.; Mulembakani, P.; Wemakoy, E.O.; Muyembe-Tamfum, J.J.; Ndembi, N.; Brennan, C.A.; Hackett, J., Jr.; et al. Serologic prevalence of Ebola virus in Equatorial Africa. Emerg. Infect. Dis. 2019, 25, 911–918. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steffen, I.; Lu, K.; Hoff, N.A.; Mulembakani, P.; Okitolonda, W.E.; Muyembe-Tamfum, J.J.; Ndembi, N.; Brennan, C.A.; Hackett, J., Jr.; Switzer, W.M.; et al. Seroreactivity against Marburg or related filoviruses in West and Central Africa. Emerg. Microbes. Infect. 2020, 9, 124–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, V.; Charlett, A.; Brown, C.S. Meta-analysis of predictive symptoms for Ebola virus disease. PLoS Negl. Trop. Dis. 2020, 23, e0008799. [Google Scholar] [CrossRef]
- Kortepeter, M.G.; Dierberg, K.; Shenoy, E.S.; Cieslak, T.J. Medical Countermeasures Working Group of the National Ebola Training and Education Center’s (NETEC) Special Pathogens Research Network (SPRN). Marburg virus disease: A summary for clinicians. Int. J. Infect Dis. 2020, 99, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, K.E.; Isbell, L.A. Changes in ranging and agonistic behavior of vervet monkeys (Cercopithecus aethiops) after predator-induced group fusion. Am. J. Primatol. 2010, 72, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.; Piel, A.K.; Forman, D.; Stewart, F.A.; King, A.J. The ecological determinants of baboon troop movements at local and continental scales. Mov. Ecol. 2015, 3, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kajihara, M.; Hang’ombe, B.M.; Changula, K.; Harima, H.; Isono, M.; Okuya, K.; Yoshida, R.; Mori-Kajihara, A.; Eto, Y.; Orba, Y.; et al. Marburgvirus in Egyptian fruit bats, Zambia. Emerg. Infect. Dis. 2019, 25, 1577–1580. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, W.J., III. Baboon sleeping site preferences and relationships to primate grouping patterns. Am. J. Primatol. 1982, 3, 41–53. [Google Scholar] [CrossRef]
- Randhawa, N.; Bird, B.H.; VanWormer, E.; Sijali, Z.; Kilonzo, C.; Msigwa, A.; Ekiri, A.B.; Samson, A.; Epstein, J.H.; Wolking, D.J.; et al. Fruit bats in flight: A look into the movements of the ecologically important Eidolon helvum in Tanzania. One Health Outlook 2020, 2, 16. [Google Scholar] [CrossRef] [PubMed]
- Tapanes, E.; Detwiler, K.M.; Cords, M. Bat predation by cercopithecus monkeys: Implications for zoonotic disease transmission. Ecohealth 2016, 13, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Monadjem, A.; Taylor, P.J.; Cotterill, F.P.D.; Schoeman, M.C. Bats of Southern and Central Africa. A Biogeographic and Taxonomic Synthesis, 1st ed.; Wits University Press: Johannesburg, South Africa, 2010; pp. 132–135. [Google Scholar]


| Year | % (Positive/Total) for Each Filovirus 1 | ||||||
|---|---|---|---|---|---|---|---|
| EBOV | SUDV | TAFV | BDBV | RESTV | MARV | Total | |
| 2008 | 3.2 | 2.1 | 1.1 | 4.3 | 0 | 2.1 | 12.8 |
| (3/94) | (2/94) | (1/94) | (4/94) | (0/94) | (2/94) | (12/94) | |
| 2009 | 8.1 | 4.0 | 0 | 1.0 | 1.0 | 1.0 | 15.2 |
| (8/99) | (4/99) | (0/99) | (1/99) | (1/99) | (1/99) | (15/99) | |
| 2010 | 6.0 | 0 | 4.0 | 2.0 | 2.0 | 10.0 | 24.0 |
| (3/50) | (0/50) | (2/50) | (1/50) | (1/50) | (5/50) | (12/50) | |
| Total | 5.8 | 2.5 | 1.2 | 2.5 | 0.8 | 3.3 | 16.0 |
| (14/243) | (6/243) | (3/243) | (6/243) | (2/243) | (8/243) | (39/243) | |
| Antigen | Antibody Titer 1 | Total | |||
|---|---|---|---|---|---|
| 400 | 1600 | 6400 | 25,600 | ||
| EBOV | 3 | 7 | 3 | 1 | 14 |
| SUDV | 2 | 4 | 0 | 0 | 6 |
| TAFV | 0 | 3 | 0 | 0 | 3 |
| BDBV | 1 | 3 | 1 | 1 | 6 |
| RESTV | 1 | 0 | 1 | 0 | 2 |
| MARV | 3 | 4 | 1 | 0 | 8 |
| NHP Species | % (Positive/Total) for Each Filovirus 1 | |||||
|---|---|---|---|---|---|---|
| EBOV | SUDV | TAFV | BDBV | RESTV | MARV 2 | |
| Baboon | 6.4 | 2.4 | 0.8 | 1.6 | 0.8 | 5.6 |
| (8/125) | (3/125) | (1/125) | (2/125) | (1/125) | (7/125) | |
| Vervet monkey | 5.1 | 2.5 | 1.7 | 3.4 | 0.8 | 0.81 |
| (6/118) | (3/118) | (2/118) | (4/118) | (1/118) | (1/118) | |
| Total | 5.8 | 2.5 | 1.2 | 2.5 | 0.8 | 3.3 |
| (14/243) | (6/243) | (3/243) | (6/243) | (2/243) | (8/243) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Changula, K.; Simulundu, E.; Lombe, B.P.; Nakayama, E.; Miyamoto, H.; Takahashi, Y.; Sawa, H.; Simukonda, C.; Hang’ombe, B.M.; Takada, A. Serological Evidence of Filovirus Infection in Nonhuman Primates in Zambia. Viruses 2021, 13, 1283. https://doi.org/10.3390/v13071283
Changula K, Simulundu E, Lombe BP, Nakayama E, Miyamoto H, Takahashi Y, Sawa H, Simukonda C, Hang’ombe BM, Takada A. Serological Evidence of Filovirus Infection in Nonhuman Primates in Zambia. Viruses. 2021; 13(7):1283. https://doi.org/10.3390/v13071283
Chicago/Turabian StyleChangula, Katendi, Edgar Simulundu, Boniface Pongombo Lombe, Eri Nakayama, Hiroko Miyamoto, Yuji Takahashi, Hirofumi Sawa, Chuma Simukonda, Bernard M. Hang’ombe, and Ayato Takada. 2021. "Serological Evidence of Filovirus Infection in Nonhuman Primates in Zambia" Viruses 13, no. 7: 1283. https://doi.org/10.3390/v13071283
APA StyleChangula, K., Simulundu, E., Lombe, B. P., Nakayama, E., Miyamoto, H., Takahashi, Y., Sawa, H., Simukonda, C., Hang’ombe, B. M., & Takada, A. (2021). Serological Evidence of Filovirus Infection in Nonhuman Primates in Zambia. Viruses, 13(7), 1283. https://doi.org/10.3390/v13071283








