COVID-19 in Infants Less than 3 Months: Severe or Not Severe Disease?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Evaluation of COVID-19 Outcomes and Severity Scores Assessment
- -
- SCORE 1—clinical and/or radiological diagnosis of pneumonia with normal oxygen levels or mild specific involvement of a single organ/apparatus without specific pharmacological support, requiring hospitalization without ICU admission.
- -
- SCORE 2—acute respiratory distress syndrome requiring low or high flow (HFNC) oxygen therapy without ICU admission, or moderate specific involvement of a single organ/apparatus with the need of specific pharmacological support, requiring hospitalization without ICU admission.
- -
- SCORE 3—severe acute respiratory illness (SARI) (SpO2 < 92% associated with tachypnea and other signs of respiratory failure requiring non-invasive or invasive mechanical ventilation, or critical involvement of a single organ/apparatus with the need of specific pharmacological support with ICU admission.
- -
- SCORE 4—Death
2.3. Statistical Analyses
3. Results
3.1. Patient Characteristics
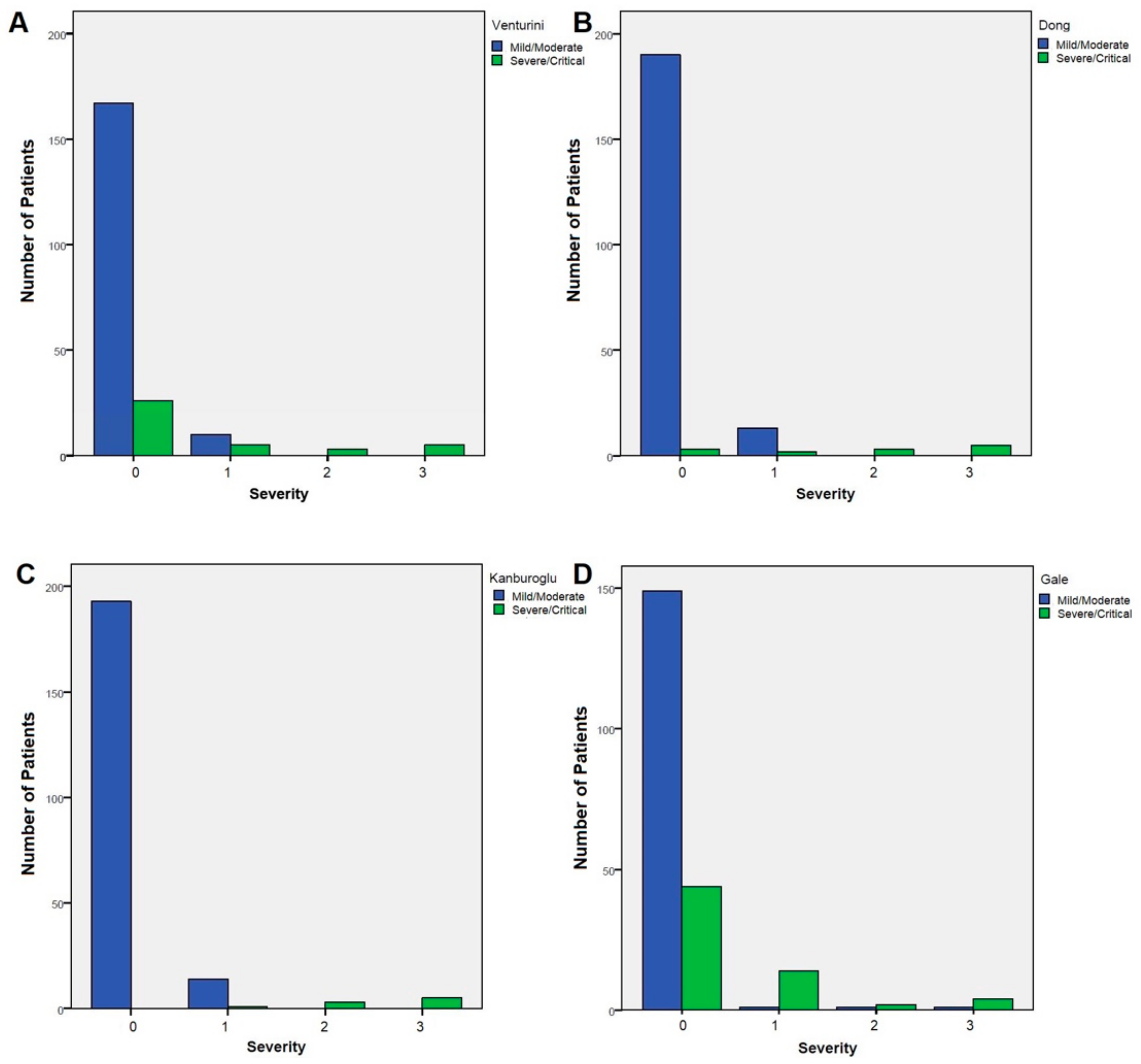
3.2. Correlation between Different Severity Scores and Our Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard, Updated to 10 June 2022. Available online: https://covid19.who.int/ (accessed on 26 July 2022).
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Qu, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Hernández, J.L.J.; Orozco, I.F. COVID-19 in Children: Respiratory Involvement and Some Differences With the Adults. Front. Pediatr. 2021, 9, 622240. [Google Scholar] [CrossRef] [PubMed]
- Girona-Alarcon, M.; Bobillo-Perez, S.; Sole-Ribalta, A.; Hernandez, L.; Guitart, C.; Suarez, R.; Balaguer, M.; Cambra, F.-J.; Jordan, I.; Platform, K.C. The different manifestations of COVID-19 in adults and children: A cohort study in an intensive care unit. BMC Infect. Dis. 2021, 21, 87. [Google Scholar] [CrossRef] [PubMed]
- Ludvigsson, J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020, 109, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiology of COVID-19 Among Children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Zhang, L.; Du, H.; Zhang, J.; Li, Y.Y.; Qu, J.; Zhang, W.; Wang, Y.; Bao, S.; Li, Y.; et al. SARS-CoV-2 Infection in Children. N. Engl. J. Med. 2020, 382, 1663–1665. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Xing, Y.; Wong, G.W.-K. COVID-19: Lessons to date from China. Arch. Dis. Child. 2020, 105, 1146–1150. [Google Scholar] [CrossRef]
- Zimmermann, P.; Curtis, N. Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections. Arch. Dis. Child. 2021, 106, 429–439. [Google Scholar] [CrossRef]
- Gale, C.; A Quigley, M.; Placzek, A.; Knight, M.; Ladhani, S.; Draper, E.S.; Sharkey, D.; Doherty, C.; Mactier, H.; Kurinczuk, J.J. Characteristics and outcomes of neonatal SARS-CoV-2 infection in the UK: A prospective national cohort study using active surveillance. Lancet Child Adolesc. Health 2021, 5, 113–121. [Google Scholar] [CrossRef]
- Walker, K.F.; O’Donoghue, K.; Grace, N.; Dorling, J.; Comeau, J.L.; Li, W.; Thornton, J.G. Maternal transmission of SARS-COV-2 to the neonate, and possible routes for such transmission: A systematic review and critical analysis. BJOG: Int. J. Obstet. Gynaecol. 2020, 127, 1324–1336. [Google Scholar] [CrossRef] [PubMed]
- Raschetti, R.; Vivanti, A.J.; Vauloup-Fellous, C.; Loi, B.; Benachi, A.; De Luca, D. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat. Commun. 2020, 11, 5164. [Google Scholar] [CrossRef] [PubMed]
- Götzinger, F.; Santiago-Garcia, B.; Fumadó-Pérez, V.; Brinkmann, F.; Tebruegge, M. The ability of the neonatal immune response to handle SARS-CoV-2 infection. Lancet Child Adolesc. Health 2021, 5, e6–e7. [Google Scholar] [CrossRef]
- Venturini, E.; Montagnani, C.; Garazzino, S.; Donà, D.; Pierantoni, L.; Vecchio, A.L.; Nicolini, G.; Bianchini, S.; Krzysztofiak, A.; Galli, L.; et al. Treatment of children with COVID-19: Position paper of the Italian Society of Pediatric Infectious Disease. Ital. J. Pediatr. 2020, 46, 139. [Google Scholar] [CrossRef] [PubMed]
- Kanburoglu, M.K.; Tayman, C.; Oncel, M.Y.; Akin, I.M.; Can, E.; Demir, N.; Arayici, S.; Baser, D.O.; Caner, I.; Memisoglu, A.; et al. A Multicentered Study on Epidemiologic and Clinical Characteristics of 37 Neonates With Community-acquired COVID-19. Pediatr. Infect. Dis. J. 2020, 39, e297–e302. [Google Scholar] [CrossRef] [PubMed]
- Garazzino, S.; Vecchio, A.L.; Pierantoni, L.; Carducci, F.I.C.; Marchetti, F.; Meini, A.; Castagnola, E.; Vergine, G.; Donà, D.; Bosis, S.; et al. Epidemiology, Clinical Features and Prognostic Factors of Pediatric SARS-CoV-2 Infection: Results From an Italian Multicenter Study. Front. Pediatr. 2021, 9, 649358. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Emergency Preparedness and Response: Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). 2020. Available online: https://emergency.cdc.gov/han/2020/han00432.asp (accessed on 27 March 2020).
- Dhir, S.K.; Kumar, J.; Meena, J.; Kumar, P. Clinical features and outcome of SARS-CoV-2 infection in neonates: A systematic review. J. Trop. Pediatr. 2020, 67, fmaa059. [Google Scholar] [CrossRef] [PubMed]
- Liguoro, I.; Pilotto, C.; Bonanni, M.; Ferrari, M.E.; Pusiol, A.; Nocerino, A.; Vidal, E.; Cogo, P. SARS-COV-2 infection in children and newborns: A systematic review. Eur. J. Pediatr. 2020, 179, 1029–1046, Erratum in Eur. J. Pediatr. 2021, 180, 2343. [Google Scholar] [CrossRef]
- Bhuiyan, M.U.; Stiboy, E.; Hassan, M.Z.; Chan, M.; Islam, M.S.; Haider, N.; Jaffe, A.; Homaira, N. Epidemiology of COVID-19 infection in young children under five years: A systematic review and meta-analysis. Vaccine 2021, 39, 667–677. [Google Scholar] [CrossRef]
- Mithal, L.B.; Machut, K.Z.; Muller, W.J.; Kociolek, L.K. SARS-CoV-2 Infection in Infants Less than 90 Days Old. J. Pediatr. 2020, 224, 150–152. [Google Scholar] [CrossRef]
- Olivini, N.; Carducci, F.I.C.; Santilli, V.; De Ioris, M.A.; Scarselli, A.; Alario, D.; Geremia, C.; Lombardi, M.H.; Marabotto, C.; Mariani, R.; et al. A neonatal cluster of novel coronavirus disease 2019: Clinical management and considerations. Ital. J. Pediatr. 2020, 46, 180. [Google Scholar] [CrossRef]
- Sankaran, D.; Nakra, N.; Cheema, R.; Blumberg, D.; Lakshminrusimha, S. Perinatal SARS-CoV-2 Infection and Neonatal COVID-19: A 2021 Update. NeoReviews 2021, 22, e284–e295. [Google Scholar] [CrossRef]
- Shah, P.S.; Diambomba, Y.; Acharya, G.; Morris, S.K.; Bitnun, A. Classification system and case definition for SARS-CoV-2 infection in pregnant women, fetuses, and neonates. Acta Obstet. Gynecol. Scand. 2020, 99, 565–568. [Google Scholar] [CrossRef]
- De Luca, D. Managing neonates with respiratory failure due to SARS-CoV-2. Lancet Child Adolesc. Health 2020, 4, e8. [Google Scholar] [CrossRef]
- Wolter, N.; Jassat, W.; Walaza, S.; Welch, R.; Moultrie, H.; Groome, M.; Amoako, D.G.; Everatt, J.; Bhiman, J.N.; Scheepers, C.; et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: A data linkage study. Lancet 2022, 399, 437–446. [Google Scholar] [CrossRef]
- Tagarro, A.; Coya, O.-N.; Pérez-Villena, A.; Iglesias, B.; Navas, A.; Aguilera-Alonso, D.; Moraleda, C. Features of COVID-19 in Children During the Omicron Wave Compared With Previous Waves in Madrid, Spain. Pediatr. Infect. Dis. J. 2022, 41, e249–e251. [Google Scholar] [CrossRef]

| Dong et al. [7] | Gale et al. [11] | Venturini et al. [15] | Kanburoglu et al. [16] | |
|---|---|---|---|---|
| Mild | Symptoms of acute upper respiratory tract infection or digestive symptoms | Fever and/or fatigue and/or upper airways symptoms without radiological/ultrasound findings | Upper respiratory tract infection or fever, no feeding difficulty and no obvious hypoxemia, and no risk of late neonatal sepsis | |
| Moderate | Pneumonia without hypoxemia and shortness of breath Chest computed tomography abnormalities without clinical signs and symptoms | Fever and/or fatigue and/or upper airways symptoms (cough or mild respiratory distress) and/or poor feeding and/or pneumonia identified with chest X-ray or ultrasound | Hospitalization due to feeding difficulty or risk of late neonatal sepsis, but no obvious hypoxemia or no need for nasal continuous positive airway pressure | |
| Severe | Oxygen saturation is <92% with other hypoxia manifestations | At least two of the following: (1) any of hyperthermia, apnea, cough, tachypnoea, respiratory distress or recession, supplemental oxygen requirement, poor feeding or vomiting, or diarrhea; (2) any of low white blood cell count, low lymphocyte count, or raised C-reactive protein concentration; and (3) abnormal chest X-ray | Fever and cough, plus at least one of the following: (1) oxygen saturation on finger pulse <92% on room air; (2) severe respiratory distress, cyanosis, intermittent apnea; (3) fast breathing; (4) systemic symptoms: drowsiness, lethargy, seizures, dehydration | Oxygen saturation <92% or need for nasal continuous positive airway pressure |
| Critical | Acute respiratory distress syndrome, respiratory failure, shock, encephalopathy, myocardial injury or heart failure, coagulation dysfunction, and acute kidney injury | Pediatric acute respiratory distress syndrome, sepsis-associated organ dysfunction, septic shock, coma | Mechanical ventilation or disseminated intravascular coagulopathy or multiple organ dysfunction |
| Characteristics | Number (%) |
|---|---|
| Age at diagnosis | |
| <2 days | 3 (1.4) |
| 2–7 days | 6 (2.8) |
| 8–14 days | 11 (5.1) |
| 15–21 days | 21 (9.7) |
| 22–28 days | 18 (8.3) |
| >28 days | 157 (72.7) |
| Underlying disease | 18 (8.3) |
| Congenital heart disease | 10 (6.1) |
| Congenital hypothyroidism | 3 (1.4) |
| Other * | 5 (2.3) |
| Preterms | 17 (7.9) |
| <32 weeks | 1 (0.5) |
| 32–33 weeks | 1 (0.5) |
| 34–36 | 15 (6.9) |
| Underlying treatments | 4 (1.8) |
| Carnitine | 1 (0.5) |
| Levothyroxine | 3 (1.4) |
| Known SARS-CoV-2 contact | 138 (63.9) |
| Immediate family member | 127 (58.8) |
| Healthcare workers | 6 (2.8) |
| Other | 5 (2.3) |
| Characteristics | Number (%) |
|---|---|
| Clinical characteristics | |
| Fever | 172 (79.6) |
| Coryza | 58 (26.9) |
| Poor feeding | 51 (23.6) |
| Cough | 42 (19.4) |
| Diarrhea | 28 (13.0) |
| Vomiting | 15 (6.9) |
| Irritability | 10 (4.6) |
| Lethargy | 9 (4.2) |
| Respiratory distress | 7 (3.2) |
| Pharyngitis | 6 (2.8) |
| Conjunctivitis | 5 (2.3) |
| Apnea | 4 (1.8) |
| Febrile seizures | 2 (0.9) |
| Asymptomatic | 15 (6.9) |
| Laboratory findings (data available) | |
| Leukocytosis (210) | 21 (9.7) |
| Lymphocytopenia (210) | 10 (4.6) |
| Increased ESR (127) | 3 (1.4) |
| Increased CRP (210) | 34 (15.7) |
| Increased ALT (167) | 19 (8.8) |
| Increased LDH (141) | 35 (16.2) |
| Increased ferritin (141) | 30 (13.9) |
| Increased CK (134) | 6 (2.8) |
| Increased Troponin (124) | 21 (9.7) |
| Concomitant viral infection (98 tested) | 9 (9.2) |
| Adenovirus | 1 (1.0) |
| Rhinovirus | 4 (4.1) |
| Bocavirus | 1 (1.0) |
| RSV | 3 (3.1) |
| Influenza | 1 (1.0) |
| Enterovirus | 2 (2.0) |
| Chest X-ray performed | 78 (36.1) |
| Normal | 36 (46.2) |
| Parenchymal opacity | 8 (10.3) |
| Interstitial pattern | 20 (25.6) |
| Parenchymal and interstitial pattern | 14 (17.9) |
| Characteristics | Number (%) |
|---|---|
| Moderate/severe clinical presentation | 22 (10.2) |
| Pneumonia | 15 (6.9) |
| SARI | 7 (3.2) |
| Sepsis | 4 (1.8) |
| Multisystem inflammatory syndrome | 2 (0.9) |
| Myocarditis | 1 (0.5) |
| Coma | 1 (0.5) |
| Horner Syndrome | 1 (0.5) |
| Respiratory support | 10 (4.6) |
| Supplemental oxygen | 8 (3.7) |
| HFNC oxygen therapy | 1 (0.5) |
| Invasive ventilation | 1 (0.5) |
| Treatment | 33 (15.3) |
| Hydroxychloroquine | 1 (0.5) |
| Macrolides | 8 (3.7) |
| Other antibiotics | 20 (9.3) |
| Corticosteroids | 4 (1.9) |
| Severity score | |
| 0 | 193 (89.3) |
| 1 | 15 (6.9) |
| 2 | 3 (1.4) |
| 3 | 5 (2.3) |
| 4 | 0 (0.0) |
| ICU admission | 5 (2.3) |
| Sequelae | 3 (1.4) |
| Death | 0 (0.0) |
| Dong et al. [7] % (n) | Kanburoglu et al. [11] % (n) | Gale et al. [15] % (n) | Venturini et al. [16] % (n) | p | |
|---|---|---|---|---|---|
| All Infants (n 216) Severe Critical | |||||
| 5.1% (11) | 3.7% (8) | 29.6% (64) | 17.1% (37) | p < 0.001 | |
| 0.9% (2) | 0.5% (1) | 0.5% (2) | p= 0.764 | ||
| Newborns (n 59) Severe | |||||
| 6.8% (4) | 6.8% (4) | 28.8% (17) | 25.4% (15) | p < 0.001 | |
| Critical | 1.7% (1) | 1.7% (1) | 1.7% (1) | p = 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dona’, D.; Montagnani, C.; Di Chiara, C.; Venturini, E.; Galli, L.; Lo Vecchio, A.; Denina, M.; Olivini, N.; Bruzzese, E.; Campana, A.; et al. COVID-19 in Infants Less than 3 Months: Severe or Not Severe Disease? Viruses 2022, 14, 2256. https://doi.org/10.3390/v14102256
Dona’ D, Montagnani C, Di Chiara C, Venturini E, Galli L, Lo Vecchio A, Denina M, Olivini N, Bruzzese E, Campana A, et al. COVID-19 in Infants Less than 3 Months: Severe or Not Severe Disease? Viruses. 2022; 14(10):2256. https://doi.org/10.3390/v14102256
Chicago/Turabian StyleDona’, Daniele, Carlotta Montagnani, Costanza Di Chiara, Elisabetta Venturini, Luisa Galli, Andrea Lo Vecchio, Marco Denina, Nicole Olivini, Eugenia Bruzzese, Andrea Campana, and et al. 2022. "COVID-19 in Infants Less than 3 Months: Severe or Not Severe Disease?" Viruses 14, no. 10: 2256. https://doi.org/10.3390/v14102256
APA StyleDona’, D., Montagnani, C., Di Chiara, C., Venturini, E., Galli, L., Lo Vecchio, A., Denina, M., Olivini, N., Bruzzese, E., Campana, A., Giacchero, R., Salvini, F., Meini, A., Ponzoni, M., Trapani, S., Rossi, E., Lombardi, M. H., Badolato, R., Pierri, L., ... on behalf of The Italian SITIP-SIP Pediatric SARS-CoV-2 Infection Study Group. (2022). COVID-19 in Infants Less than 3 Months: Severe or Not Severe Disease? Viruses, 14(10), 2256. https://doi.org/10.3390/v14102256









