Advances in Molecular Genetics Enabling Studies of Highly Pathogenic RNA Viruses
Abstract
:1. Introduction
2. EARLY CASE: Molecular Genetics for HIV
2.1. Viral Load Diagnostics for HIV
2.2. The Swiss Statement on Transmission
2.3. Testing Therapy-Resistance of HIV
2.4. Structured Treatment Interruption
2.5. Therapy Simplification
2.6. Approaches to Eliminate/Cure HIV
2.7. International Development Work for HIV Therapy and Diagnostics
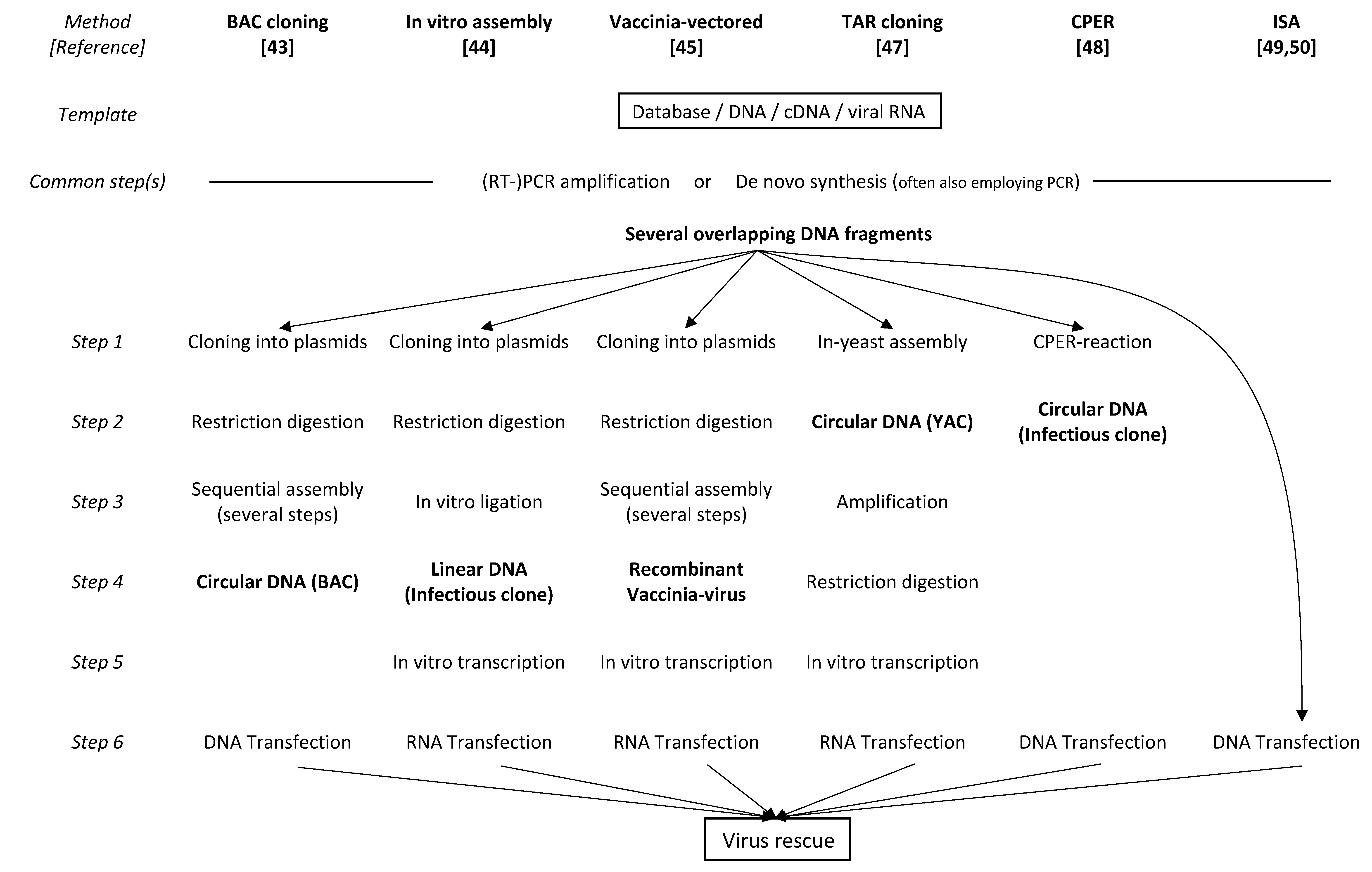
3. LATEST CASE: Reverse Genetics for Coronaviruses
3.1. BAC-Cloning
3.2. In Vitro Assembly and Vaccinia-Vectored Approaches
3.3. TAR Cloning and CPER
3.4. ISA
3.5. Role of N Protein in Virus Recovery
3.6. Role of the Polybasic S1/S2 Cleavage Site in the S Protein
3.7. Cell and Animal Models for SARS-CoV-2 Infection
3.8. Perspectives for Next-Generation Vaccines
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Taniguchi, T.; Palmieri, M.; Weissmann, C. QB DNA-containing hybrid plasmids giving rise to QB phage formation in the bacterial host. Nature 1978, 274, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Racaniello, V.R.; Baltimore, D. Cloned poliovirus complementary DNA is infectious in mammalian cells. Science 1981, 214, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Boyer, J.C.; Haenni, A.L. Infectious transcripts and cDNA clones of RNA viruses. Virology 1994, 198, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, G.; Lubinski, J.; Dasgupta, A.; Racaniello, V.R. In vitro synthesis of infectious poliovirus RNA. Proc. Natl. Acad. Sci. USA 1985, 82, 8424–8428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adachi, A.; Gendelman, H.E.; Koenig, S.; Folks, T.; Willey, R.; Rabson, A.; Martin, M.A. Production of acquired immunodeficiency syndrome-associated retrovirus in human and nonhuman cells transfected with an infectious molecular clone. J. Virol. 1986, 59, 284–291. [Google Scholar] [CrossRef] [Green Version]
- Ruggli, N.; Tratschin, J.D.; Mittelholzer, C.; Hofmann, M.A. Nucleotide sequence of classical swine fever virus strain Alfort/187 and transcription of infectious RNA from stably cloned full-length cDNA. J. Virol. 1996, 70, 3478–3487. [Google Scholar] [CrossRef] [Green Version]
- Sturmer, M.; Reinheimer, C. Description of two commercially available assays for genotyping of HIV-1. Intervirology 2012, 55, 134–137. [Google Scholar] [CrossRef]
- Merel, P.; Pellegrin, I.; Garrigue, I.; Caumont, A.; Schrive, M.H.; Birac, V.; Bonot, P.; Fleury, H. Comparison of capillary electrophoresis sequencing with the new CEQ 2000 DNA Analysis System to conventional gel based systems for HIV drug resistance analysis. J. Virol. Methods 2001, 98, 9–16. [Google Scholar] [CrossRef]
- Gall, A.; Ferns, B.; Morris, C.; Watson, S.; Cotten, M.; Robinson, M.; Berry, N.; Pillay, D.; Kellam, P. Universal amplification, next-generation sequencing, and assembly of HIV-1 genomes. J. Clin. Microbiol. 2012, 50, 3838–3844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henn, M.R.; Boutwell, C.L.; Charlebois, P.; Lennon, N.J.; Power, K.A.; Macalalad, A.R.; Berlin, A.M.; Malboeuf, C.M.; Ryan, E.M.; Gnerre, S.; et al. Whole genome deep sequencing of HIV-1 reveals the impact of early minor variants upon immune recognition during acute infection. PLoS Pathog. 2012, 8, e1002529. [Google Scholar] [CrossRef]
- Provisional Public Health Service inter-agency recommendations for screening donated blood and plasma for antibody to the virus causing acquired immunodeficiency syndrome. MMWR Morb. Mortal. Wkly Rep. 1985, 34, 1–5.
- Saag, M.S.; Holodniy, M.; Kuritzkes, D.R.; O’Brien, W.A.; Coombs, R.; Poscher, M.E.; Jacobsen, D.M.; Shaw, G.M.; Richman, D.D.; Volberding, P.A. HIV viral load markers in clinical practice. Nat. Med. 1996, 2, 625–629. [Google Scholar] [CrossRef] [PubMed]
- CDC information. Post-Exposure Prophylaxis (PEP) | HIV Risk and Prevention. Available online: https://www.cdc.gov/hiv/risk/pep/index.html (accessed on 29 November 2022).
- Recommendations for the Use of Antiretroviral Drugs During Pregnancy and Interventions to Reduce Perinatal HIV Transmission in the United States. Available online: https://clinicalinfo.hiv.gov/en/guidelines/perinatal/intrapartum-care-for-people-with-hiv?view=full (accessed on 29 November 2022).
- Lee, B.E.; Plitt, S.S.; Jayaraman, G.C.; Chui, L.; Singh, A.E.; Preiksaitis, J.K. Use of quantitative HIV RNA detection for early diagnosis of HIV infection in infants and acute HIV infections in Alberta, Canada. J. Clin. Microbiol. 2012, 50, 502–505. [Google Scholar] [CrossRef] [Green Version]
- Ledergerber, B.; von Overbeck, J.; Egger, M.; Luthy, R. The Swiss HIV Cohort Study: Rationale, organization and selected baseline characteristics. Soz. Praventivmed. 1994, 39, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Swiss HIV Cohort Study Information. Available online: https://www.shcs.ch/157-about-shcs (accessed on 29 November 2022).
- Swiss Statement on Transmission. Available online: https://saez.ch/journalfile/view/article/ezm_saez/fr/bms.2008.13252/ceec6bc5af6bc91092a76b506e46e296f6dfc5f7/bms_2008_13252.pdf/rsrc/jf (accessed on 29 November 2022).
- Lorenzi, P.; Yerly, S.; Abderrakim, K.; Fathi, M.; Rutschmann, O.T.; von Overbeck, J.; Leduc, D.; Perrin, L.; Hirschel, B. Toxicity, efficacy, plasma drug concentrations and protease mutations in patients with advanced HIV infection treated with ritonavir plus saquinavir. Swiss HIV Cohort Study. AIDS 1997, 11, F95–F99. [Google Scholar] [CrossRef]
- Lorenzi, P.; Opravil, M.; Hirschel, B.; Chave, J.P.; Furrer, H.J.; Sax, H.; Perneger, T.V.; Perrin, L.; Kaiser, L.; Yerly, S. Impact of drug resistance mutations on virologic response to salvage therapy. Swiss HIV Cohort Study. AIDS 1999, 13, F17–F21. [Google Scholar] [CrossRef]
- von Wyl, V.; Klimkait, T.; Yerly, S.; Nicca, D.; Furrer, H.; Cavassini, M.; Calmy, A.; Bernasconi, E.; Boni, J.; Aubert, V.; et al. Adherence as a predictor of the development of class-specific resistance mutations: The Swiss HIV Cohort Study. PLoS ONE 2013, 8, e77691. [Google Scholar] [CrossRef]
- Hauser, A.; Goldstein, F.; Reichmuth, M.L.; Kouyos, R.D.; Wandeler, G.; Egger, M.; Riou, J. Acquired HIV drug resistance mutations on first-line antiretroviral therapy in Southern Africa: Systematic review and Bayesian evidence synthesis. J. Clin. Epidemiol. 2022, 148, 135–145. [Google Scholar] [CrossRef]
- Tang, M.W.; Liu, T.F.; Shafer, R.W. The HIVdb system for HIV-1 genotypic resistance interpretation. Intervirology 2012, 55, 98–101. [Google Scholar] [CrossRef]
- Euresist Network. A European Multidisciplinary Network for the Fight against HIV Drug Resistance. Available online: https://www.euresist.org (accessed on 29 November 2022).
- EACS (European AIDS Clinical Society) Guidelines. Available online: https://www.eacsociety.org/guidelines/eacs-guidelines/ (accessed on 29 November 2022).
- HIV Databases at Los Alamos National Laboratory. Available online: https://www.hiv.lanl.gov/content/index (accessed on 29 November 2022).
- Papasavvas, E.; Kostman, J.R.; Mounzer, K.; Grant, R.M.; Gross, R.; Gallo, C.; Azzoni, L.; Foulkes, A.; Thiel, B.; Pistilli, M.; et al. Randomized, controlled trial of therapy interruption in chronic HIV-1 infection. PLoS Med. 2004, 1, e64. [Google Scholar] [CrossRef]
- Oxenius, A.; Hirschel, B. Structured treatment interruptions in HIV infection: Benefit or disappointment? Expert Rev. Anti. Infect Ther. 2003, 1, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Yerly, S.; Fagard, C.; Günthard, H.F.; Hirschel, B.; Perrin, L. Drug resistance mutations during structured treatment interruptions. Antivir. Ther. 2003, 8, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Vernazza, P.; Daneel, S.; Schiffer, V.; Decosterd, L.; Fierz, W.; Klimkait, T.; Hoffmann, M.; Hirschel, B. The role of compartment penetration in PI-monotherapy: The Atazanavir-Ritonavir Monomaintenance (ATARITMO) Trial. AIDS 2007, 21, 1309–1315. [Google Scholar] [CrossRef]
- Hutter, G.; Nowak, D.; Mossner, M.; Ganepola, S.; Mussig, A.; Allers, K.; Schneider, T.; Hofmann, J.; Kucherer, C.; Blau, O.; et al. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. N. Engl. J. Med. 2009, 360, 692–698. [Google Scholar] [CrossRef] [Green Version]
- Hartley, O.; Martins, E.; Scurci, I. Preventing HIV transmission through blockade of CCR5: Rationale, progress and perspectives. Swiss. Med. Wkly 2018, 148, w14580. [Google Scholar] [CrossRef] [Green Version]
- Klinnert, S.; Chemnitzer, A.; Rusert, P.; Metzner, K.J. Systematic HIV-1 promoter targeting with CRISPR/dCas9-VPR reveals optimal region for activation of the latent provirus. J. Gen. Virol. 2022, 103, 1–13. [Google Scholar] [CrossRef]
- Rusert, P.; Kouyos, R.D.; Kadelka, C.; Ebner, H.; Schanz, M.; Huber, M.; Braun, D.L.; Hozé, N.; Scherrer, A.; Magnus, C.; et al. Determinants of HIV-1 broadly neutralizing antibody induction. Nat. Med. 2016, 22, 1260–1267. [Google Scholar] [CrossRef] [Green Version]
- Kouyos, R.D.; Rusert, P.; Kadelka, C.; Huber, M.; Marzel, A.; Ebner, H.; Schanz, M.; Liechti, T.; Friedrich, N.; Braun, D.L.; et al. Tracing HIV-1 strains that imprint broadly neutralizing antibody responses. Nature 2018, 561, 406–410. [Google Scholar] [CrossRef]
- Perreau, M.; Banga, R.; Pantaleo, G. Targeted Immune Interventions for an HIV-1 Cure. Trends Mol. Med. 2017, 23, 945–961. [Google Scholar] [CrossRef]
- Report on the Global HIV/AIDS Epidemic. Available online: https://data.unaids.org/pub/report/1998/19981125_global_epidemic_report_en.pdf (accessed on 29 November 2022).
- Masimba, P.; Kituma, E.; Klimkait, T.; Horvath, E.; Stoeckle, M.; Hatz, C.; Mossdorf, E.; Mwaigomole, E.; Khamis, S.; Jullu, B.; et al. Prevalence of drug resistance mutations and HIV type 1 subtypes in an HIV type 1-infected cohort in rural Tanzania. AIDS Res. Hum. Retrovir. 2013, 29, 1229–1236. [Google Scholar] [CrossRef] [Green Version]
- Muri, L.; Gamell, A.; Ntamatungiro, A.J.; Glass, T.R.; Luwanda, L.B.; Battegay, M.; Furrer, H.; Hatz, C.; Tanner, M.; Felger, I.; et al. Development of HIV drug resistance and therapeutic failure in children and adolescents in rural Tanzania: An emerging public health concern. AIDS 2017, 31, 61–70. [Google Scholar] [CrossRef] [PubMed]
- von Braun, A.; Sekaggya-Wiltshire, C.; Bachmann, N.; Ssemwanga, D.; Scherrer, A.U.; Nanyonjo, M.; Kapaata, A.; Kaleebu, P.; Gunthard, H.F.; Castelnuovo, B.; et al. HIV-1 Drug Resistance Among Ugandan Adults Attending an Urban Out-Patient Clinic. J. Acquir. Immune Defic. Syndr. 2018, 78, 566–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amstutz, A.; Brown, J.A.; Ringera, I.; Muhairwe, J.; Lejone, T.I.; Klimkait, T.; Glass, T.R.; Labhardt, N.D. Engagement in Care, Viral Suppression, Drug Resistance, and Reasons for Nonengagement After Home-Based Same-Day Antiretroviral Therapy Initiation in Lesotho: A Two-Year Follow-up of the CASCADE Trial. Clin. Infect. Dis. 2020, 71, 2608–2614. [Google Scholar] [CrossRef] [Green Version]
- Labhardt, N.D.; Ringera, I.; Lejone, T.I.; Klimkait, T.; Muhairwe, J.; Amstutz, A.; Glass, T.R. Effect of Offering Same-Day ART vs Usual Health Facility Referral During Home-Based HIV Testing on Linkage to Care and Viral Suppression Among Adults With HIV in Lesotho: The CASCADE Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2018, 319, 1103–1112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almazan, F.; Gonzalez, J.M.; Penzes, Z.; Izeta, A.; Calvo, E.; Plana-Duran, J.; Enjuanes, L. Engineering the largest RNA virus genome as an infectious bacterial artificial chromosome. Proc. Natl. Acad. Sci. USA 2000, 97, 5516–5521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yount, B.; Curtis, K.M.; Baric, R.S. Strategy for systematic assembly of large RNA and DNA genomes: Transmissible gastroenteritis virus model. J. Virol. 2000, 74, 10600–10611. [Google Scholar] [CrossRef] [Green Version]
- Thiel, V.; Herold, J.; Schelle, B.; Siddell, S.G. Infectious RNA transcribed in vitro from a cDNA copy of the human coronavirus genome cloned in vaccinia virus. J. Gen. Virol. 2001, 82 Pt 6, 1273–1281. [Google Scholar] [CrossRef]
- Almazan, F.; Sola, I.; Zuniga, S.; Marquez-Jurado, S.; Morales, L.; Becares, M.; Enjuanes, L. Coronavirus reverse genetic systems: Infectious clones and replicons. Virus Res. 2014, 189, 262–270. [Google Scholar] [CrossRef]
- Thi Nhu Thao, T.; Labroussaa, F.; Ebert, N.; V’Kovski, P.; Stalder, H.; Portmann, J.; Kelly, J.; Steiner, S.; Holwerda, M.; Kratzel, A.; et al. Rapid reconstruction of SARS-CoV-2 using a synthetic genomics platform. Nature 2020, 582, 561–565. [Google Scholar] [CrossRef]
- Torii, S.; Ono, C.; Suzuki, R.; Morioka, Y.; Anzai, I.; Fauzyah, Y.; Maeda, Y.; Kamitani, W.; Fukuhara, T.; Matsuura, Y. Establishment of a reverse genetics system for SARS-CoV-2 using circular polymerase extension reaction. Cell Rep. 2021, 35, 109014. [Google Scholar] [CrossRef]
- Aubry, F.; Nougairède, A.; de Fabritus, L.; Querat, G.; Gould, E.A.; de Lamballerie, X. Single-stranded positive-sense RNA viruses generated in days using infectious subgenomic amplicons. J. Gen. Virol. 2014, 95 Pt 11, 2462–2467. [Google Scholar] [CrossRef]
- Melade, J.; Piorkowski, G.; Touret, F.; Fourie, T.; Driouich, J.S.; Cochin, M.; Bouzidi, H.S.; Coutard, B.; Nougairede, A.; de Lamballerie, X. A simple reverse genetics method to generate recombinant coronaviruses. EMBO Rep. 2022, 23, e53820. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Muruato, A.; Lokugamage, K.G.; Narayanan, K.; Zhang, X.; Zou, J.; Liu, J.; Schindewolf, C.; Bopp, N.E.; Aguilar, P.V.; et al. An Infectious cDNA Clone of SARS-CoV-2. Cell Host Microbe 2020, 27, 841–848.e3. [Google Scholar] [CrossRef] [PubMed]
- Casais, R.; Thiel, V.; Siddell, S.G.; Cavanagh, D.; Britton, P. Reverse genetics system for the avian coronavirus infectious bronchitis virus. J. Virol. 2001, 75, 12359–12369. [Google Scholar] [CrossRef] [Green Version]
- Yount, B.; Denison, M.R.; Weiss, S.R.; Baric, R.S. Systematic assembly of a full-length infectious cDNA of mouse hepatitis virus strain A59. J. Virol. 2002, 76, 11065–11078. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yount, B.; Curtis, K.M.; Fritz, E.A.; Hensley, L.E.; Jahrling, P.B.; Prentice, E.; Denison, M.R.; Geisbert, T.W.; Baric, R.S. Reverse genetics with a full-length infectious cDNA of severe acute respiratory syndrome coronavirus. Proc. Natl. Acad. Sci. USA 2003, 100, 12995–13000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peacock, T.P.; Goldhill, D.H.; Zhou, J.; Baillon, L.; Frise, R.; Swann, O.C.; Kugathasan, R.; Penn, R.; Brown, J.C.; Sanchez-David, R.Y.; et al. The furin cleavage site in the SARS-CoV-2 spike protein is required for transmission in ferrets. Nat. Microbiol. 2021, 6, 899–909. [Google Scholar] [CrossRef]
- Johnson, B.A.; Xie, X.; Bailey, A.L.; Kalveram, B.; Lokugamage, K.G.; Muruato, A.; Zou, J.; Zhang, X.; Juelich, T.; Smith, J.K.; et al. Loss of furin cleavage site attenuates SARS-CoV-2 pathogenesis. Nature 2021, 591, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.G.; Tang, Y.D.; Akter, S.; Zheng, C. Roles of the polybasic furin cleavage site of spike protein in SARS-CoV-2 replication, pathogenesis, and host immune responses and vaccination. J. Med. Virol. 2022, 94, 1815–1820. [Google Scholar] [CrossRef]
- Matsuyama, S.; Nagata, N.; Shirato, K.; Kawase, M.; Takeda, M.; Taguchi, F. Efficient activation of the severe acute respiratory syndrome coronavirus spike protein by the transmembrane protease TMPRSS2. J. Virol. 2010, 84, 12658–12664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuyama, S.; Nao, N.; Shirato, K.; Kawase, M.; Saito, S.; Takayama, I.; Nagata, N.; Sekizuka, T.; Katoh, H.; Kato, F.; et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl. Acad Sci. USA 2020, 117, 7001–7003. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, X.; Liu, J.; Xia, H.; Zou, J.; Muruato, A.E.; Periasamy, S.; Kurhade, C.; Plante, J.A.; Bopp, N.E.; et al. A live-attenuated SARS-CoV-2 vaccine candidate with accessory protein deletions. Nat. Commun. 2022, 13, 4337. [Google Scholar] [CrossRef] [PubMed]
- Amarilla, A.A.; Sng, J.D.J.; Parry, R.; Deerain, J.M.; Potter, J.R.; Setoh, Y.X.; Rawle, D.J.; Le, T.T.; Modhiran, N.; Wang, X.; et al. A versatile reverse genetics platform for SARS-CoV-2 and other positive-strand RNA viruses. Nat. Commun. 2021, 12, 3431. [Google Scholar] [CrossRef] [PubMed]
- Piplani, S.; Singh, P.K.; Winkler, D.A.; Petrovsky, N. In silico comparison of SARS-CoV-2 spike protein-ACE2 binding affinities across species and implications for virus origin. Sci. Rep. 2021, 11, 13063. [Google Scholar] [CrossRef]
- Ma, C.; Gong, C. ACE2 models of frequently contacted animals provide clues of their SARS-CoV-2 S protein affinity and viral susceptibility. J. Med. Virol. 2021, 93, 4469–4479. [Google Scholar] [CrossRef] [PubMed]
- Funnell, S.G.P.; Afrough, B.; Baczenas, J.J.; Berry, N.; Bewley, K.R.; Bradford, R.; Florence, C.; Duff, Y.L.; Lewis, M.; Moriarty, R.V.; et al. A cautionary perspective regarding the isolation and serial propagation of SARS-CoV-2 in Vero cells. NPJ Vaccines 2021, 6, 83. [Google Scholar] [CrossRef]
- Dedoni, S.; Avdoshina, V.; Camoglio, C.; Siddi, C.; Fratta, W.; Scherma, M.; Fadda, P. K18- and CAG-hACE2 Transgenic Mouse Models and SARS-CoV-2: Implications for Neurodegeneration Research. Molecules 2022, 27, 4142. [Google Scholar] [CrossRef] [PubMed]
- DeDiego, M.L.; Alvarez, E.; Almazan, F.; Rejas, M.T.; Lamirande, E.; Roberts, A.; Shieh, W.J.; Zaki, S.R.; Subbarao, K.; Enjuanes, L. A severe acute respiratory syndrome coronavirus that lacks the E gene is attenuated in vitro and in vivo. J. Virol. 2007, 81, 1701–1713. [Google Scholar] [CrossRef] [Green Version]
- Dediego, M.L.; Pewe, L.; Alvarez, E.; Rejas, M.T.; Perlman, S.; Enjuanes, L. Pathogenicity of severe acute respiratory coronavirus deletion mutants in hACE-2 transgenic mice. Virology 2008, 376, 379–389. [Google Scholar] [CrossRef] [Green Version]
- Lamirande, E.W.; DeDiego, M.L.; Roberts, A.; Jackson, J.P.; Alvarez, E.; Sheahan, T.; Shieh, W.J.; Zaki, S.R.; Baric, R.; Enjuanes, L.; et al. A live attenuated severe acute respiratory syndrome coronavirus is immunogenic and efficacious in golden Syrian hamsters. J. Virol. 2008, 82, 7721–7724. [Google Scholar] [CrossRef] [Green Version]
- Netland, J.; DeDiego, M.L.; Zhao, J.; Fett, C.; Alvarez, E.; Nieto-Torres, J.L.; Enjuanes, L.; Perlman, S. Immunization with an attenuated severe acute respiratory syndrome coronavirus deleted in E protein protects against lethal respiratory disease. Virology 2010, 399, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Fett, C.; DeDiego, M.L.; Regla-Nava, J.A.; Enjuanes, L.; Perlman, S. Complete protection against severe acute respiratory syndrome coronavirus-mediated lethal respiratory disease in aged mice by immunization with a mouse-adapted virus lacking E protein. J. Virol. 2013, 87, 6551–6559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jimenez-Guardeno, J.M.; Regla-Nava, J.A.; Nieto-Torres, J.L.; DeDiego, M.L.; Castano-Rodriguez, C.; Fernandez-Delgado, R.; Perlman, S.; Enjuanes, L. Identification of the Mechanisms Causing Reversion to Virulence in an Attenuated SARS-CoV for the Design of a Genetically Stable Vaccine. PLoS Pathog. 2015, 11, e1005215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regla-Nava, J.A.; Nieto-Torres, J.L.; Jimenez-Guardeno, J.M.; Fernandez-Delgado, R.; Fett, C.; Castano-Rodriguez, C.; Perlman, S.; Enjuanes, L.; DeDiego, M.L. Severe acute respiratory syndrome coronaviruses with mutations in the E protein are attenuated and promising vaccine candidates. J. Virol. 2015, 89, 3870–3887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almazan, F.; DeDiego, M.L.; Sola, I.; Zuniga, S.; Nieto-Torres, J.L.; Marquez-Jurado, S.; Andres, G.; Enjuanes, L. Engineering a replication-competent, propagation-defective Middle East respiratory syndrome coronavirus as a vaccine candidate. mBio 2013, 4, e00650-13. [Google Scholar] [CrossRef] [Green Version]
- Gutierrez-Alvarez, J.; Honrubia, J.M.; Fernandez-Delgado, R.; Wang, L.; Castano-Rodriguez, C.; Zuniga, S.; Sola, I.; Enjuanes, L. Genetically Engineered Live-Attenuated Middle East Respiratory Syndrome Coronavirus Viruses Confer Full Protection against Lethal Infection. mBio 2021, 12, 1–19. [Google Scholar] [CrossRef]
- Gutierrez-Alvarez, J.; Honrubia, J.M.; Sanz-Bravo, A.; Gonzalez-Miranda, E.; Fernandez-Delgado, R.; Rejas, M.T.; Zuniga, S.; Sola, I.; Enjuanes, L. Middle East respiratory syndrome coronavirus vaccine based on a propagation-defective RNA replicon elicited sterilizing immunity in mice. Proc. Natl. Acad. Sci. USA 2021, 118, 1–11. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, Y.; Liu, J.; Bailey, A.L.; Plante, K.S.; Plante, J.A.; Zou, J.; Xia, H.; Bopp, N.E.; Aguilar, P.V.; et al. A trans-complementation system for SARS-CoV-2 recapitulates authentic viral replication without virulence. Cell 2021, 184, 2229–2238.e13. [Google Scholar] [CrossRef]
- Ju, X.; Zhu, Y.; Wang, Y.; Li, J.; Zhang, J.; Gong, M.; Ren, W.; Li, S.; Zhong, J.; Zhang, L.; et al. A novel cell culture system modeling the SARS-CoV-2 life cycle. PLoS Pathog. 2021, 17, e1009439. [Google Scholar] [CrossRef]
- Cheung, P.H.; Ye, Z.W.; Lui, W.Y.; Ong, C.P.; Chan, P.; Lee, T.T.; Tang, T.T.; Yuen, T.L.; Fung, S.Y.; Cheng, Y.; et al. Production of single-cycle infectious SARS-CoV-2 through a trans-complemented replicon. J. Med. Virol. 2022, 94, 6078–6090. [Google Scholar] [CrossRef]
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mittelholzer, C.; Klimkait, T. Advances in Molecular Genetics Enabling Studies of Highly Pathogenic RNA Viruses. Viruses 2022, 14, 2682. https://doi.org/10.3390/v14122682
Mittelholzer C, Klimkait T. Advances in Molecular Genetics Enabling Studies of Highly Pathogenic RNA Viruses. Viruses. 2022; 14(12):2682. https://doi.org/10.3390/v14122682
Chicago/Turabian StyleMittelholzer, Christian, and Thomas Klimkait. 2022. "Advances in Molecular Genetics Enabling Studies of Highly Pathogenic RNA Viruses" Viruses 14, no. 12: 2682. https://doi.org/10.3390/v14122682
APA StyleMittelholzer, C., & Klimkait, T. (2022). Advances in Molecular Genetics Enabling Studies of Highly Pathogenic RNA Viruses. Viruses, 14(12), 2682. https://doi.org/10.3390/v14122682






