Zika Virus Immunoglobulin G Seroprevalence among Young Adults Living with HIV or without HIV in Thailand from 1997 to 2017
Abstract
:1. Introduction
2. Materials and Methods
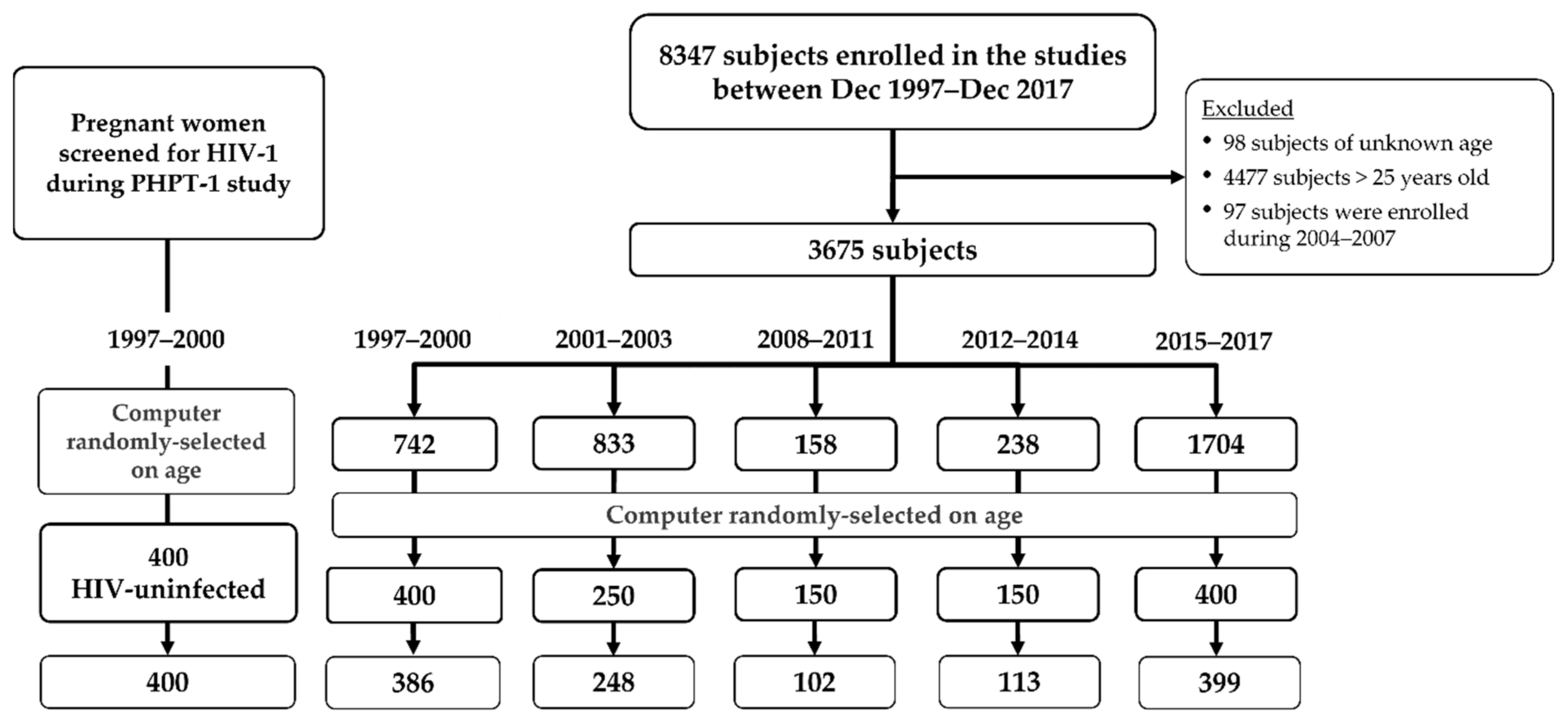
2.1. Study Population
2.2. Laboratory Testing
2.3. Statistical Considerations
3. Results
3.1. Study Population Characteristics
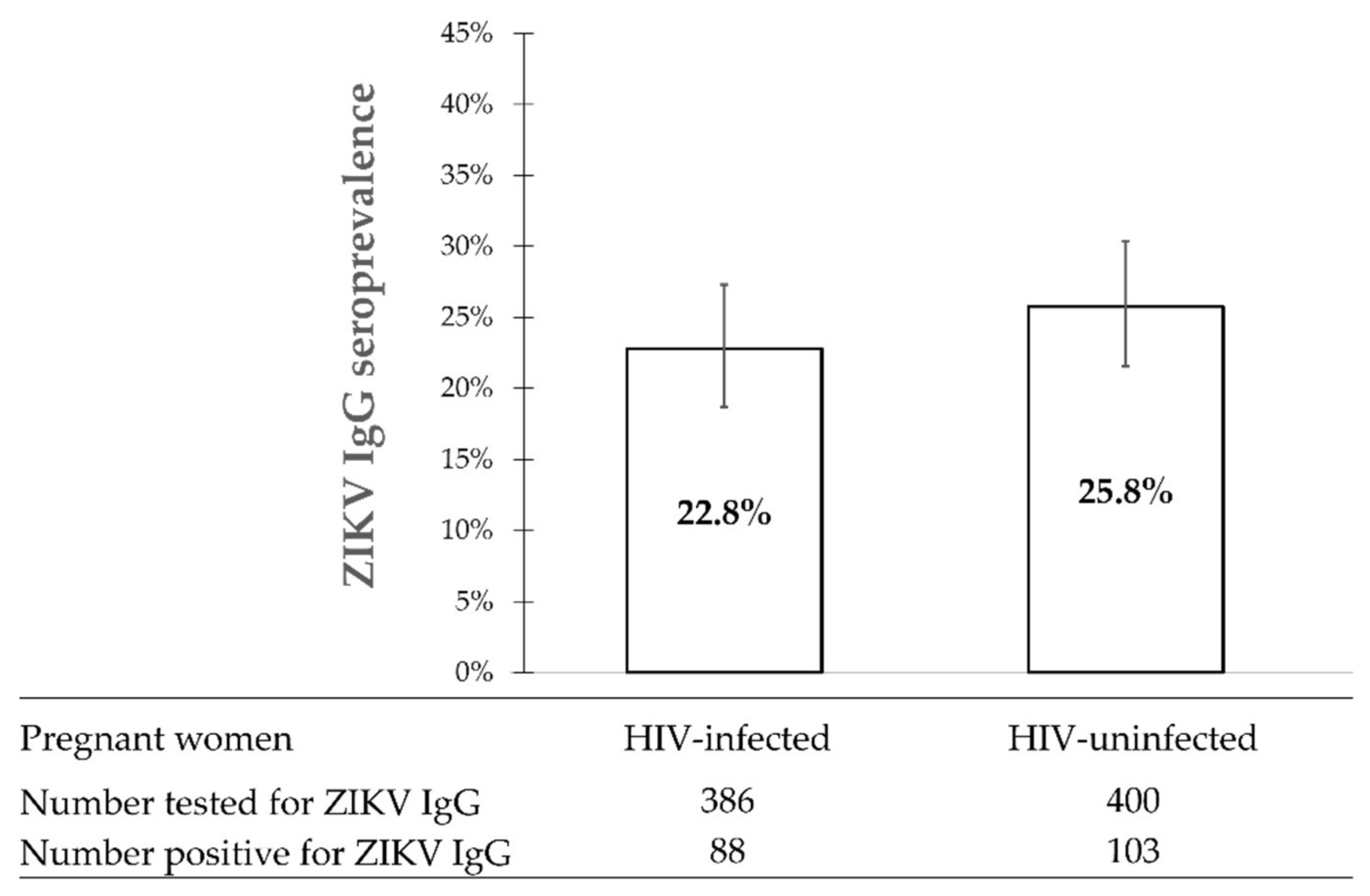
3.2. ZIKV IgG Seroprevalence in HIV-Infected versus HIV-Uninfected Pregnant Women during 1997–2000
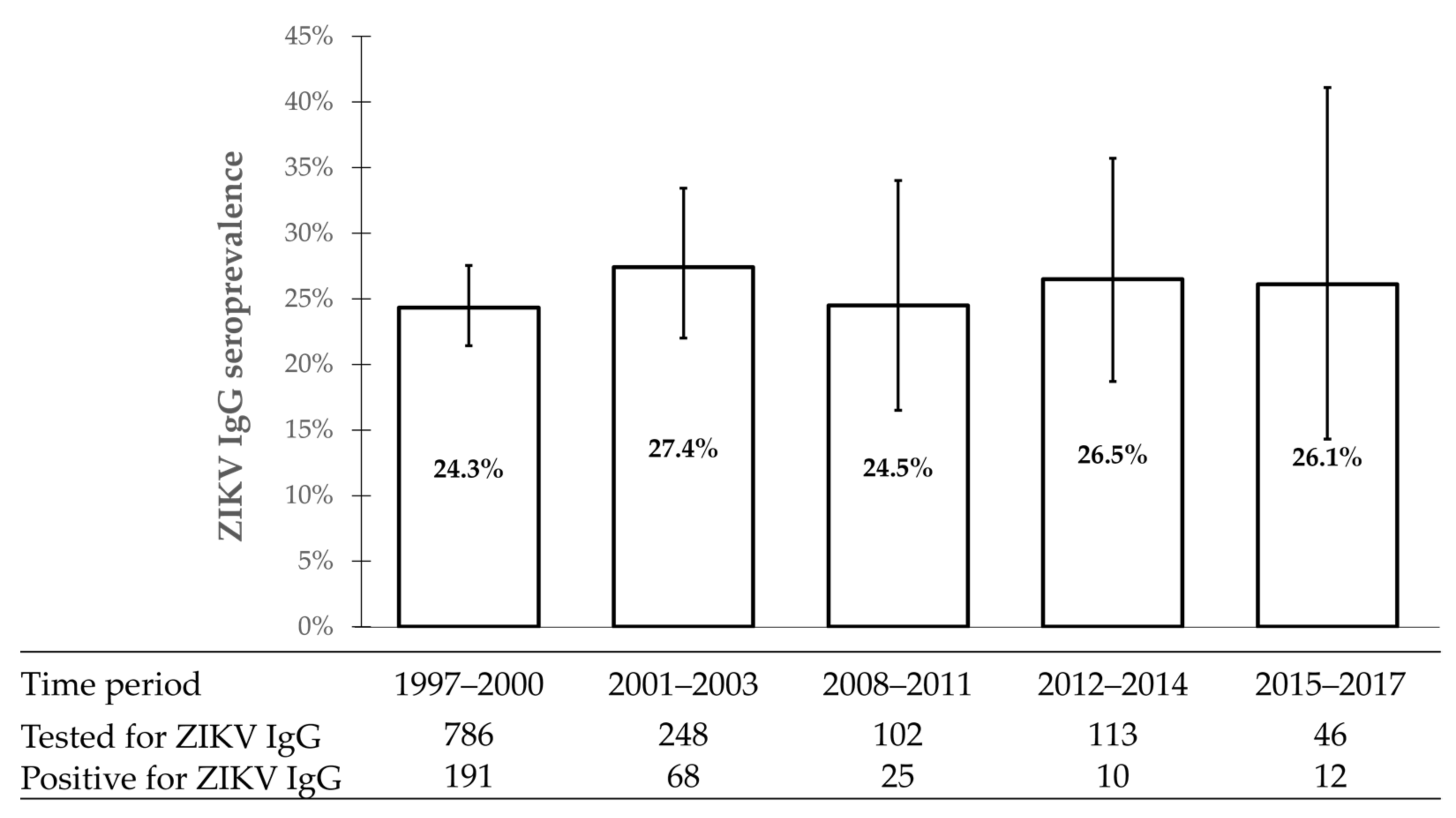
3.3. The Evolution of ZIKV IgG Seroprevalence during 1997–2017
3.4. Factors Associated with ZIKV IgG Seropositivity among Pregnant Women
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sirohi, D.; Kuhn, R.J. Zika Virus Structure, Maturation, and Receptors. J. Infect. Dis. 2017, 216 (Suppl. 10), S935–S944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musso, D.; Gubler, D.J. Zika Virus. Clin. Microbiol. Rev. 2016, 29, 487–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petersen, L.R.; Jamieson, D.J.; Powers, A.M.; Honein, M.A. Zika Virus. N. Engl. J. Med. 2016, 374, 1552–1563. [Google Scholar] [CrossRef] [PubMed]
- Dick, G.W.; Kitchen, S.F.; Haddow, A.J. Zika virus. I. Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 1952, 46, 509–520. [Google Scholar] [CrossRef]
- Duffy, M.R.; Chen, T.H.; Hancock, W.T.; Powers, A.M.; Kool, J.L.; Lanciotti, R.S.; Pretrick, M.; Marfel, M.; Holzbauer, S.; Dubray, C.; et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N. Engl. J. Med. 2009, 360, 2536–2543. [Google Scholar] [CrossRef] [PubMed]
- Musso, D.; Nilles, E.J.; Cao-Lormeau, V.M. Rapid spread of emerging Zika virus in the Pacific area. Clin. Microbiol. Infect. 2014, 20, O595–O596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cauchemez, S.; Besnard, M.; Bompard, P.; Dub, T.; Guillemette-Artur, P.; Eyrolle-Guignot, D.; Salje, H.; Van Kerkhove, M.D.; Abadie, V.; Garel, C.; et al. Association between Zika virus and microcephaly in French Polynesia, 2013–2015: A retrospective study. Lancet 2016, 387, 2125–2132. [Google Scholar] [CrossRef] [Green Version]
- Hennessey, M.; Fischer, M.; Staples, J.E. Zika Virus Spreads to New Areas—Region of the Americas, May 2015–January 2016. MMWR 2016, 65, 55–58. [Google Scholar]
- Araujo, L.M.; Ferreira, M.L.; Nascimento, O.J. Guillain-Barré syndrome associated with the Zika virus outbreak in Brazil. Arq. De Neuro-Psiquiatr. 2016, 74, 253–255. [Google Scholar] [CrossRef] [Green Version]
- Baud, D.; Gubler, D.J.; Schaub, B.; Lanteri, M.C.; Musso, D. An update on Zika virus infection. Lancet 2017, 390, 2099–2109. [Google Scholar] [CrossRef] [Green Version]
- WHO. WHO Statement on the 2nd Meeting of IHR Emergency Committee on Zika Virus and Observed Increase in Neurological Disorders and Neonatal Malformations [Online] 2016. Available online: https://www.who.int/news/item/08-03-2016-who-statement-on-the-2nd-meeting-of-ihr-emergency-committee-on-zika-virus-and-observed-increase-in-neurological-disorders-and-neonatal-malformations (accessed on 4 December 2021).
- Pond, W.L. Arthropod-borne virus antibody in sera from residents of South-East Asia. Trans. R. Soc. Trop. Med. Hyg. 1963, 57, 364–371. [Google Scholar] [CrossRef]
- Fonseca, K.; Meatherall, B.; Zarra, D.; Drebot, M.; MacDonald, J.; Pabbaraju, K.; Wong, S.; Webster, P.; Lindsay, R.; Tellier, R. First case of Zika virus infection in a returning Canadian traveler. Am. J. Trop. Med. Hyg. 2014, 91, 1035–1038. [Google Scholar] [CrossRef] [PubMed]
- Buathong, R.; Hermann, L.; Thaisomboonsuk, B.; Rutvisuttinunt, W.; Klungthong, C.; Chinnawirotpisan, P.; Manasatienkij, W.; Nisalak, A.; Fernandez, S.; Yoon, I.K.; et al. Detection of Zika Virus Infection in Thailand, 2012–2014. Am. J. Trop. Med. Hyg. 2015, 93, 380–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lallemant, M.; Jourdain, G.; Le Coeur, S.; Kim, S.; Koetsawang, S.; Comeau, A.M.; Phoolcharoen, W.; Essex, M.; McIntosh, K.; Vithayasai, V. A trial of shortened zidovudine regimens to prevent mother-to-child transmission of human immunodeficiency virus type 1. Perinatal HIV Prevention Trial (Thailand) Investigators. N. Engl. J. Med. 2000, 343, 982–991. [Google Scholar] [CrossRef]
- Lallemant, M.; Jourdain, G.; Le Coeur, S.; Mary, J.Y.; Ngo-Giang-Huong, N.; Koetsawang, S.; Kanshana, S.; McIntosh, K.; Thaineua, V. Single-dose perinatal nevirapine plus standard zidovudine to prevent mother-to-child transmission of HIV-1 in Thailand. N. Engl. J. Med. 2004, 351, 217–228. [Google Scholar] [CrossRef] [Green Version]
- Lallemant, M.; Ngo-Giang-Huong, N.; Jourdain, G.; Traisaithit, P.; Cressey, T.R.; Collins, I.J.; Jarupanich, T.; Sukhumanant, T.; Achalapong, J.; Sabsanong, P.; et al. Efficacy and safety of 1-month postpartum zidovudine-didanosine to prevent HIV-resistance mutations after intrapartum single-dose nevirapine. Clin. Infect. Dis. 2010, 50, 898–908. [Google Scholar] [CrossRef]
- Lallemant, M.; Le Coeur, S.; Sirirungsi, W.; Cressey, T.R.; Ngo-Giang-Huong, N.; Traisathit, P.; Klinbuayaem, V.; Sabsanong, P.; Kanjanavikai, P.; Jourdain, G.; et al. Randomized noninferiority trial of two maternal single-dose nevirapine-sparing regimens to prevent perinatal HIV in Thailand. AIDS 2015, 29, 2497–2507. [Google Scholar] [CrossRef] [Green Version]
- Lallemant, M.; Amzal, B.; Sripan, P.; Urien, S.; Cressey, T.R.; Ngo-Giang-Huong, N.; Klinbuayaem, V.; Rawangban, B.; Sabsanong, P.; Siriwachirachai, T.; et al. Perinatal Antiretroviral Intensification to Prevent Intrapartum HIV Transmission When Antenatal Antiretroviral Therapy Is Initiated Less Than 8 Weeks Before Delivery. J. Acquir. Immune. Defic. Syndr. 2020, 84, 313–322. [Google Scholar] [CrossRef]
- Jourdain, G.; Ngo-Giang-Huong, N.; Harrison, L.; Decker, L.; Khamduang, W.; Tierney, C.; Salvadori, N.; Cressey, T.R.; Sirirungsi, W.; Achalapong, J.; et al. Tenofovir versus Placebo to Prevent Perinatal Transmission of Hepatitis, B. N. Engl. J. Med. 2018, 378, 911–923. [Google Scholar] [CrossRef]
- Salvadori, N.; Decker, L.; Ngo-Giang-Huong, N.; Mary, J.Y.; Chevret, S.; Arunothong, S.; Adam, P.; Khamduang, W.; Samleerat, T.; Luangsook, P.; et al. Impact of Counseling Methods on HIV Retesting Uptake in At-Risk Individuals: A Randomized Controlled Study. AIDS Behav. 2020, 24, 1505–1516. [Google Scholar] [CrossRef]
- Steinhagen, K.; Probst, C.; Radzimski, C.; Schmidt-Chanasit, J.; Emmerich, P.; van Esbroeck, M.; Schinkel, J.; Grobusch, M.P.; Goorhuis, A.; Warnecke, J.M.; et al. Serodiagnosis of Zika virus (ZIKV) infections by a novel NS1-based ELISA devoid of cross-reactivity with dengue virus antibodies: A multicohort study of assay performance, 2015 to 2016. Euro. Surveill. 2016, 21, 30426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ngo-Giang-Huong, N.; Leroi, C.; Fusco, D.; Cressey, T.R.; Wangsaeng, N.; Salvadori, N.; Kongyai, N.; Sirirungsi, W.; Lallemant, M.; Auewarakul, P.; et al. Lack of Association between Adverse Pregnancy Outcomes and Zika Antibodies among Pregnant Women in Thailand between 1997 and 2015. Viruses 2021, 13, 1423. [Google Scholar] [CrossRef] [PubMed]
- Ruchusatsawat, K.; Wongjaroen, P.; Posanacharoen, A.; Rodriguez-Barraquer, I.; Sangkitporn, S.; Cummings, D.A.T.; Salje, H. Long-term circulation of Zika virus in Thailand: An observational study. Lancet Infect. Dis. 2019, 19, 439–446. [Google Scholar] [CrossRef] [Green Version]
- Thongsripong, P.; Green, A.; Kittayapong, P.; Kapan, D.; Wilcox, B.; Bennett, S. Mosquito vector diversity across habitats in central Thailand endemic for dengue and other arthropod-borne diseases. PLoS Negl. Trop. Dis. 2013, 7, e2507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinhold, J.M.; Lazzari, C.R.; Lahondère, C. Effects of the Environmental Temperature on Aedes aegypti and Aedes albopictus Mosquitoes: A Review. Insects 2018, 9, 158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chansang, C.; Krutbut, J.; Makruen, T.; Suebsaard, W.; Denchonchai, E.; Ninphanomchai, S.; Chansang, U. Dengue risk areas for Thailand from Aedes ovitrap survey and dengue cases analysis with Geographic Information System. Bull. Dept. Med. Sci. 2021, 63, 78–91. [Google Scholar]
- Sornjai, W.; Jaratsittisin, J.; Auewarakul, P.; Wikan, N.; Smith, D.R. Analysis of Zika virus neutralizing antibodies in normal healthy Thais. Sci. Rep. 2018, 8, 17193. [Google Scholar] [CrossRef]
| Characteristics | Overall (n = 1648) | HIV-Uninfected Pregnant Women 1997–2000 | Period 1997–2000 | Period 2001–2003 | Period 2008–2011 | Period 2012–2015 | Period 2015–2017 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n/N or n | Percentage or Median (IQR) | n/N or n | Percentage or Median (IQR) | n/N or n | Percentage or Median (IQR) | n/N or n | Percentage or Median (IQR) | n/N or n | Percentage or Median (IQR) | n/N or n | Percentage or Median (IQR) | n/N or n | Percentage or Median (IQR) | ||
| Sex | Female | 1464/1648 | 88.8 | 400/400 | 100.0 | 386/386 | 100.0 | 248/248 | 100.0 | 102/102 | 100.0 | 113/113 | 100.0 | 215/399 | 53.9 |
| Male | 174/1648 | 10.6 | 0/400 | 0.0 | 0/386 | 0.0 | 0/248 | 0.0 | 0/102 | 0.0 | 0/113 | 0.0 | 174/399 | 43.6 | |
| Other | 10/1648 | 0.6 | 0/400 | 0.0 | 0/386 | 0.0 | 0/248 | 0.0 | 0/102 | 0.0 | 0/113 | 0.0 | 10/399 | 2.5 | |
| Age (years old) | 1648 | 22.0 (20.0, 23.0) | 372 | 22.0 (20.0, 23.0) | 386 | 22.0 (20.1, 23.0) | 248 | 22.0 (20.0, 23.0) | 102 | 22.2 (20.2, 23.1) | 113 | 21.9 (19.9, 23.7) | 399 | 22.0 (20.0, 23.0) | |
| Pregnancy (denominator: females) | 1295/1464 | 88.5 | 400/400 | 100 | 386/386 | 100 | 248/248 | 100 | 102/102 | 100 | 113/113 | 100 | 46/215 | 21.4 | |
| Gestational age (weeks) | 1262 | 25.0 (16.7, 29.7) | 347 | 15.9 (11.3, 22.9) | 386 | 21.4 (16.9, 25.3) | 248 | 29.7 (28.0, 33.0) | 102 | 32.4 (32.0, 33.7) | 113 | 26.4 (20.6, 33.9) | 46 | 28.1 (28.0, 28.6) | |
| Region of birth | Central | 250/1522 | 16.4 | 19/354 | 5.4 | 46/339 | 13.6 | 60/244 | 24.6 | 35/102 | 34.3 | 24/107 | 22.4 | 66/376 | 17.6 |
| Northern | 757/1522 | 49.7 | 251/354 | 70.9 | 156/339 | 46.0 | 39/244 | 16 | 23/102 | 22.5 | 24/107 | 22.4 | 264/376 | 70.2 | |
| Northeastern | 173/1522 | 11.4 | 4/354 | 1.1 | 5/339 | 1.5 | 83/244 | 34 | 28/102 | 27.5 | 34/107 | 31.8 | 19/376 | 5.1 | |
| Eastern | 273/1522 | 17.9 | 78/354 | 22 | 125/339 | 36.9 | 46/244 | 18.9 | 6/102 | 5.9 | 13/107 | 12.1 | 5/376 | 1.3 | |
| Western | 25/1522 | 1.6 | 0/354 | 0.0 | 0/339 | 0.0 | 7/244 | 2.9 | 4/102 | 3.9 | 2/107 | 1.9 | 12/376 | 3.2 | |
| Southern | 38/1522 | 2.5 | 2/354 | 0.6 | 7/339 | 2.1 | 9/244 | 3.7 | 2/102 | 2.0 | 8/107 | 7.5 | 10/376 | 2.7 | |
| Foreign country | 6/1522 | 0.4 | 0/354 | 0.0 | 0/339 | 0.0 | 0/244 | 0 | 4/102 | 3.9 | 2/107 | 1.9 | 0/376 | 0.0 | |
| Region of enrollment | Central | 250/1644 | 15.2 | 19/398 | 4.8 | 58/386 | 15.0 | 73/242 | 30.2 | 41/102 | 40.2 | 30/114 | 26.3 | 29/396 | 7.3 |
| Northern | 868/1644 | 52.8 | 256/398 | 64.3 | 168/386 | 43.5 | 37/242 | 15.3 | 24/102 | 23.5 | 32/114 | 28.1 | 351/396 | 88.6 | |
| Northeastern | 70/1644 | 4.3 | 0/398 | 0.0 | 0/386 | 0.0 | 39/242 | 16.1 | 7/102 | 6.9 | 19/114 | 16.7 | 5/396 | 1.3 | |
| Eastern | 413/1644 | 25.1 | 121/398 | 30.4 | 152/386 | 39.4 | 81/242 | 33.5 | 27/102 | 26.5 | 22/114 | 19.3 | 10/396 | 2.5 | |
| Western | 7/1644 | 0.4 | 0/398 | 0.0 | 0/386 | 0.0 | 0/242 | 0.0 | 0/102 | 0.0 | 1/114 | 0.9 | 0/396 | 0.0 | |
| Southern | 36/1644 | 2.2 | 2/398 | 0.5 | 8/386 | 2.1 | 12/242 | 5.0 | 3/102 | 2.9 | 10/114 | 8.8 | 1/396 | 0.3 | |
| Education | Higher than bachelor’s degree | 5/1638 | 0.3 | 0/396 | 0.0 | 0/383 | 0.0 | 0/248 | 0.0 | 0/102 | 0.0 | 0/113 | 0.0 | 5/396 | 1.3 |
| College/University | 369/1638 | 22.5 | 21/396 | 5.3 | 25/383 | 6.5 | 25/248 | 10.1 | 14/102 | 13.7 | 16/113 | 14.2 | 268/396 | 67.7 | |
| High school | 188/1638 | 11.5 | 37/396 | 9.3 | 24/383 | 6.3 | 24/248 | 9.7 | 13/102 | 12.7 | 18/113 | 15.9 | 72/396 | 18.2 | |
| Secondary school/Vocational certificate | 394/1638 | 24.5 | 92/396 | 23.2 | 95/383 | 24.8 | 67/248 | 27.0 | 48/102 | 47.1 | 59/113 | 52.2 | 33/396 | 8.3 | |
| Primary school | 482/1638 | 29.4 | 179/396 | 45.2 | 164/383 | 42.8 | 88/248 | 35.5 | 24/102 | 23.5 | 15/113 | 13.3 | 12/396 | 3.0 | |
| Lower than primary school | 175/1638 | 10.7 | 55/396 | 13.9 | 75/383 | 19.6 | 36/248 | 14.5 | 3/102 | 2.9 | 5/113 | 4.4 | 1/396 | 0.3 | |
| Others | 25/1638 | 1.5 | 12/396 | 3.0 | 0/383 | 0.0 | 8/248 | 3.2 | 0/102 | 0.0 | 0/113 | 0.0 | 5/396 | 1.3 | |
| Marital status | Living with partner | 834/892 | 93.5 | n.a. 1 | n.a. 1 | 372/384 | 96.9 | 224/247 | 90.7 | 91/102 | 89.2 | 102/113 | 90.3 | 45/46 | 97.8 |
| Divorced/Not living with partner/Widowed/Single | 53/892 | 5.9 | n.a. 1 | n.a. 1 | 12/384 | 3.1 | 19/247 | 7.7 | 10/102 | 9.8 | 11/113 | 9.7 | 1/46 | 2.2 | |
| Others | 5/892 | 0.6 | n.a. 1 | n.a. 1 | 0/384 | 0.0 | 4/247 | 1.6 | 1/102 | 1.0 | 0/113 | 0.0 | 0/46 | 0.0 | |
| Number of household members | 1 (Living alone) | 101/611 | 16.5 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 3/102 | 2.9 | 0/112 | 0.0 | 98/397 | 24.7 |
| 2 people | 136/611 | 22.3 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 26/102 | 25.5 | 32/112 | 28.6 | 78/397 | 19.6 | |
| 3 people | 96/611 | 15.7 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 15/102 | 14.7 | 16/112 | 14.3 | 65/397 | 16.4 | |
| 4 people | 110/611 | 18 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 21/102 | 20.6 | 28/112 | 25 | 61/397 | 15.4 | |
| More than 4 people | 168/611 | 27.5 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 37/102 | 36.3 | 36/112 | 32.1 | 95/397 | 23.9 | |
| Multiple partner | 77/236 | 32.6 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 77/236 | 32.6 | |
| Occupation | Unemployed or Housewife | 487/1603 | 30.4 | 89/397 | 22.4 | 25/386 | 6.5 | 243/248 | 98.0 | 56/102 | 54.9 | 64/110 | 58.2 | 10/360 | 2.8 |
| Agriculturist/Fishery | 176/1603 | 11 | 106/397 | 26.7 | 63/386 | 16.3 | 2/248 | 0.8 | 3/102 | 2.9 | 2/110 | 1.8 | 0/360 | 0.0 | |
| Commercial/Private business/ Self-employed | 128/1603 | 8.0 | 34/397 | 8.6 | 42/386 | 10.9 | 1/248 | 0.4 | 22/102 | 21.6 | 21/110 | 19.1 | 8/360 | 2.2 | |
| Office man | 152/1603 | 9.5 | 27/397 | 6.8 | 124/386 | 32.1 | 0/248 | 0.0 | 1/102 | 1.0 | 0/110 | 0.0 | 0/360 | 0.0 | |
| Labor/Housekeeper | 292/1603 | 18.2 | 131/397 | 33 | 121/386 | 31.3 | 0/248 | 0.0 | 12/102 | 11.8 | 19/110 | 17.3 | 9/360 | 2.5 | |
| Student | 303/1603 | 18.9 | 3/397 | 0.8 | 2/386 | 0.5 | 0/248 | 0.0 | 3/102 | 2.9 | 3/110 | 2.7 | 292/360 | 81.1 | |
| Others | 65/1603 | 4.1 | 7/397 | 1.8 | 9/386 | 2.3 | 2/248 | 0.8 | 5/102 | 4.9 | 1/110 | 0.9 | 41/360 | 11.4 | |
| Risk behavior | Alcohol consumption | 290/404 | 71.8 | n.a. 1 | n.a. 1 | 24/24 | 100.0 | 16/16 | 100.0 | 7/7 | 100.0 | 9/9 | 100.0 | 234/348 | 67.2 |
| Smoking | 59/349 | 16.9 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 59/349 | 16.9 | |
| Drug use | 73/351 | 20.8 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 73/351 | 20.8 | |
| Any of these | 301/407 | 74 | n.a. 1 | n.a. 1 | 24/24 | 100.0 | 16/16 | 100.0 | 7/7 | 100.0 | 9/9 | 100.0 | 245/351 | 69.8 | |
| Infection status | Anti-HIV positive | 844/1645 | 51.2 | - 2 | - 2 | 386/386 | 100.0 | 247/248 | 99.6 | 101/101 | 100.0 | 106/112 | 94.6 | 4/398 | 1.0 |
| HIV RNA load (log10 copies/mL) | 838 | 3.88 (3.21, 4.46) | - 2 | - 2 | 386 | 3.92 (3.32, 4.40) | 246 | 4.0 (3.33, 4.70) | 102 | 3.57 (2.16, 4.19) | 99 | 3.81 (4.52, 3.04) | 5 | 4.88 (3.9, 5.01) | |
| HIV RNA load among pregnant women (log10 copies/mL) | 834 | 3.87 (3.21, 4.45) | - 2 | - 2 | 386 | 3.92 (3.32, 4.40) | 246 | 4.0 (3.33, 4.70) | 102 | 3.57 (2.16, 4.19) | 99 | 3.81 (4.52, 3.04) | - 2 | - 2 | |
| HBsAg positive | 111/1245 | 8.9 | n.a. 1 | n.a. 1 | 28/385 | 7.3 | 16/246 | 6.5 | 5/102 | 4.9 | 8/113 | 7.1 | 54/399 | 13.5 | |
| Anti-HCV positive | 22/1246 | 1.8 | n.a. 1 | n.a. 1 | 13/384 | 3.4 | 3/248 | 1.2 | 5/105 | 4.9 | 0/113 | 0.0 | 1/399 | 0.3 | |
| Syphilis positive | 3/353 | 0.8 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | n.a. 1 | 3/353 | 0.8 | |
| Blood chemistry testing | Fasting blood sugar (mg/dL) | 112 | 82 (73, 91) | n.a. 1 | n.a. 1 | 17 | 90 (85, 109) | 7 | 88.8 (83, 94) | 42 | 78.5 (71, 84) | 43 | 77 (71, 84) | 3 | 105 (68, 120) |
| Cholesterol (mg/dL) | 248 | 217 (180, 258.5) | n.a. 1 | n.a. 1 | 32 | 197 (160.5, 225) | 38 | 173.5 (152, 206) | 102 | 244 (217, 280) | 106 | 211.5 (182, 252) | 6 | 200 (179, 220) | |
| AST (IU/L) | 184 | 21.0 (17, 29.5) | n.a. 1 | n.a. 1 | 32 | 30.5 (21.5, 46) | 32 | 22(18, 34.5) | 40 | 20.5 (16.5, 31.5) | 34 | 20 (16, 24) | 46 | 19 (16, 22) | |
| ALT (IU/L) | 866 | 14.0 (10.0, 20.0) | n.a. 1 | n.a. 1 | 385 | 14 (10, 20) | 239 | 16(11,15) | 102 | 14 (10, 21) | 111 | 12 (9, 15) | 46 | 17.5 (12, 20) | |
| Hematological testing | Hemoglobin (g/dL) | 893 | 10.8 (11.6, 10) | n.a. 1 | n.a. 1 | 384 | 10.6 (9.9, 11.4) | 248 | 11 (10.1, 11.65) | 102 | 10.9 (10.2, 11.6) | 113 | 11 (10.2, 11.6) | 46 | 11.35 (10.7, 12.0) |
| Hematocrit (%) | 895 | 33.0 (35.0, 30.9) | n.a. 1 | n.a. 1 | 386 | 33.0 (30.9, 35.1) | 248 | 32.9 (30.55, 34.85) | 102 | 32.7 (31.0, 34.4) | 113 | 32.9 (30.8, 35.0) | 46 | 33.9 (32.0, 35.6) | |
| RBC count (million cells/mL) | 516 | 4.0 (3.6, 4.4) | n.a. 1 | n.a. 1 | 129 | 3.97 (3.54, 4.40) | 127 | 4.33 (3.95, 4.72) | 102 | 3.71 (3.49, 3.95) | 112 | 3.94 (3.61, 4.26) | 46 | 4.15 (3.80, 4.47) | |
| Platelet count (thousand/mm3) | 596 | 78.5 (180.0, 258.5) | n.a. 1 | n.a. 1 | 87 | 241 (197, 286) | 248 | 271 (230.5, 318.5) | 102 | 271.5 (233, 328) | 113 | 255 (217, 298) | 46 | 254.5 (219, 283) | |
| WBC count (cells/mm3) | 877 | 8880 (10,600, 6400) | n.a. 1 | n.a. 1 | 386 | 8800 (7300, 10,700) | 248 | 8525 (7400, 10,700) | 102 | 8780 (7650, 10,490) | 113 | 9000(7700, 10,120) | 46 | 11,150 (9100, 12,710) | |
| Absolute CD4 T-cell (cells/mm3) | 814 | 410 (280, 550) | - 2 | - 2 | 358 | 378.5 (250, 540) | 248 | 405.5 (266.5, 541) | 102 | 518.5 (413, 654) | 102 | 394.5(292, 516) | 4 | 565 (417, 853) | |
| Absolute CD4 T-cell among pregnant women (cells/mm3) | 810 | 409.5 (280, 550) | - 2 | - 2 | 358 | 378.5 (250, 540) | 248 | 405.5 (266.5, 541) | 102 | 518.5 (413, 654) | 102 | 394.5(292, 516) | n.a. 1 | n.a. 1 | |
| Characteristics | n/N | % | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95%CI) | p | Adjusted Odds Ratio (95%CI) | p | ||||
| Period | 1997–2000 | 88/386 | 22.8 | 1 | |||
| 2001–2003 | 68/248 | 27.4 | 1.28 (0.89–1.85) | 0.19 | |||
| 2008–2011 | 25/102 | 24.5 | 1.10 (0.66–1.83) | 0.72 | |||
| 2012–2014 | 30/113 | 26.5 | 1.22 (0.76–1.98) | 0.41 | |||
| 2015–2017 | 12/46 | 26.1 | 1.20 (0.59–2.41) | 0.62 | |||
| Age | 18–20 years | 47/221 | 21.3 | 1 | 1 | ||
| >20–22 years | 51/226 | 22.6 | 1.08 (0.69–1.69) | 0.74 | 1.06 (0.65–1.73) | 0.81 | |
| >22–23 years | 55/216 | 25.5 | 1.26 (0.81–1.97) | 0.30 | 1.36 (0.85–2.20) | 0.20 | |
| >23–25 years | 70/232 | 30.2 | 1.60 (1.04–2.45) | 0.03 | 1.65 (1.03–2.63) | 0.04 | |
| Gestational age (N = 1262) | 1–13 weeks | 11/46 | 23.9 | 1 | |||
| >13–28 weeks | 111/466 | 23.8 | 0.99 (0.49–2.02) | 0.99 | |||
| >28 weeks | 101/383 | 26.4 | 1.14 (0.56–2.33) | 0.72 | |||
| Region of birth (N = 1177) | North | 44/254 | 17.3 | 1 | 1 | ||
| Other | 168/569 | 29.5 | 2.00 (1.38–2.90) | <0.001 | 1.95 (1.32–2.88) | <0.001 | |
| Region of enrollment (N = 1293) | North | 45/277 | 16.3 | 1 | |||
| Other | 178/618 | 28.8 | 2.09 (1.45–3.00) | <0.001 | - 1 | n.i. 2 | |
| Education (N = 1288) | Lower than secondary school | 99/421 | 23.5 | 1 | |||
| Secondary school/Vocational certificate | 76/283 | 26.9 | 1.19 (0.84–1.69) | 0.32 | |||
| Higher than secondary school | 46/177 | 26 | 1.14 (0.76–1.71) | 0.52 | |||
| Other | 2/11 | 18.2 | 0.72 (0.15–3.40) | 0.68 | |||
| Marital status (N = 892) | Divorced/Not living with partner/Widowed/Singer | 18/53 | 34 | 1.62 (0.90–2.92) | 0.11 | 1.45 (0.77–2.75) | n.s.3 |
| Living with partner | 201/834 | 24.1 | 1 | 1 | |||
| Other | 2/5 | 40 | 2.10 (0.35–12.65) | 0.42 | 1.98 (0.33–12.09) | n.s.3 | |
| HIV status (N = 1292) | HIV negative | 118/452 | 26.1 | 1.24 (0.67–2.30) | 0.50 | ||
| HIV positive | 207/840 | 24.6 | 1 | ||||
| HIV-1 RNA load (N = 834) | ≤3.88 log 10 copies/mL | 120/420 | 28.6 | 1.55 (1.13–2.13) | 0.01 | 1.46 (1.05–2.04) | 0.03 |
| >3.88 log 10 copies/mL | 85/414 | 20.5 | 1 | 1 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choyrum, S.; Wangsaeng, N.; Nechba, A.; Salvadori, N.; Saisom, R.; Achalapong, J.; Putiyanun, C.; Sabsanong, P.; Sangsawang, S.; Patamasingh Na Ayudhaya, O.; et al. Zika Virus Immunoglobulin G Seroprevalence among Young Adults Living with HIV or without HIV in Thailand from 1997 to 2017. Viruses 2022, 14, 368. https://doi.org/10.3390/v14020368
Choyrum S, Wangsaeng N, Nechba A, Salvadori N, Saisom R, Achalapong J, Putiyanun C, Sabsanong P, Sangsawang S, Patamasingh Na Ayudhaya O, et al. Zika Virus Immunoglobulin G Seroprevalence among Young Adults Living with HIV or without HIV in Thailand from 1997 to 2017. Viruses. 2022; 14(2):368. https://doi.org/10.3390/v14020368
Chicago/Turabian StyleChoyrum, Sirinath, Nantawan Wangsaeng, Anouar Nechba, Nicolas Salvadori, Rumpaiphorn Saisom, Jullapong Achalapong, Chaiwat Putiyanun, Prapan Sabsanong, Suraphan Sangsawang, Orada Patamasingh Na Ayudhaya, and et al. 2022. "Zika Virus Immunoglobulin G Seroprevalence among Young Adults Living with HIV or without HIV in Thailand from 1997 to 2017" Viruses 14, no. 2: 368. https://doi.org/10.3390/v14020368
APA StyleChoyrum, S., Wangsaeng, N., Nechba, A., Salvadori, N., Saisom, R., Achalapong, J., Putiyanun, C., Sabsanong, P., Sangsawang, S., Patamasingh Na Ayudhaya, O., Jourdain, G., Ngo-Giang-Huong, N., & Khamduang, W. (2022). Zika Virus Immunoglobulin G Seroprevalence among Young Adults Living with HIV or without HIV in Thailand from 1997 to 2017. Viruses, 14(2), 368. https://doi.org/10.3390/v14020368






