Comparison of Aerosol Stability of Different Variants of Ebola Virus and Marburg Virus and Virulence of Aerosolised Ebola Virus in an Immune-Deficient Mouse
Abstract
:1. Introduction
2. Materials and Methods
2.1. Viruses
2.2. Growth and Enumeration
2.3. Aerosol Decay Studies
2.4. Animal Studies
2.5. Statistical Analysis
3. Results
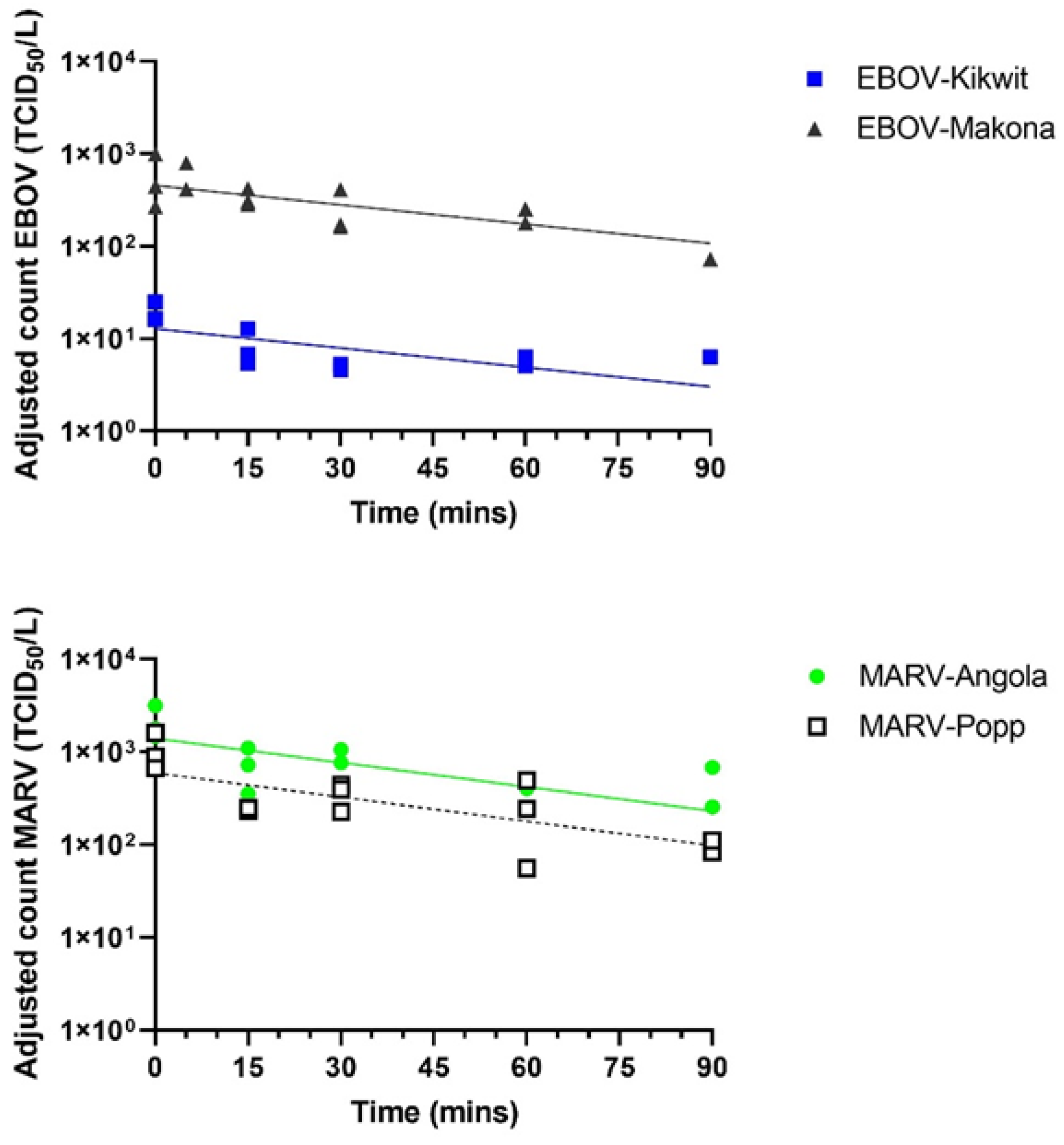
3.1. Different EBOV and MARV Variants Show Similar Biological Decay Rates in Aerosols
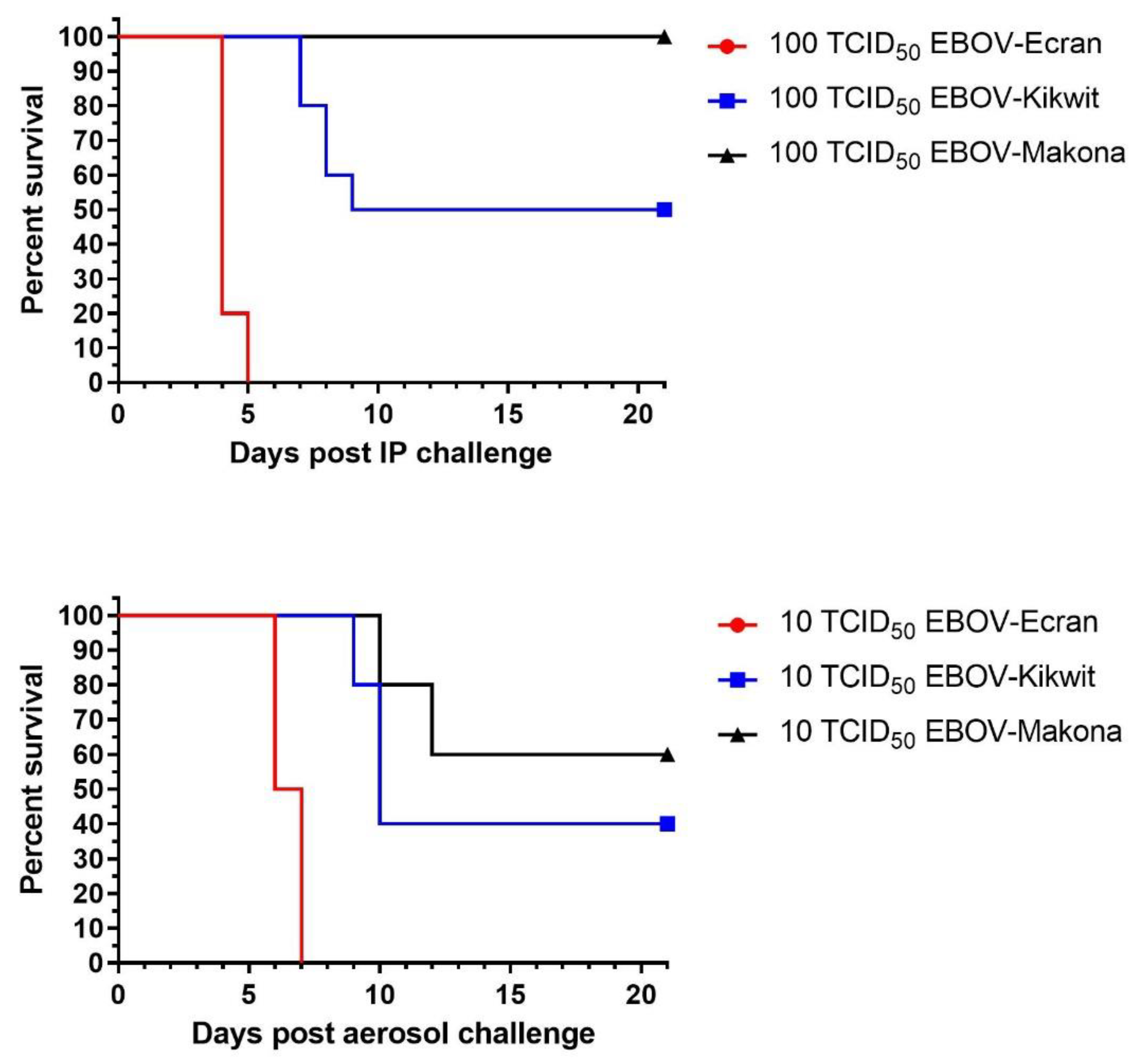
3.2. EBOV-Kikwit Shows Lethality in the Mouse Model at High Doses Only
3.3. Combined Historical Data Shows a Range of Lethality with Different EBOV Variants
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Funk, T.; Pharris, A.; Spiteri, G.; Bundle, N.; Melidou, A.; Carr, M.; Gonzalez, G.; Garcia-Leon, A.; Crispie, F.; O’Connor, L.; et al. Characteristics of SARS-CoV-2 variants of concern B.1.1.7, B.1.351 or P.1: Data from seven EU/EEA countries, weeks 38/2020 to 10/2021. Eurosurveillance 2021, 26, 2100348. [Google Scholar] [CrossRef] [PubMed]
- Plante, J.A.; Mitchell, B.M.; Plante, K.S.; Debbink, K.; Weaver, S.C.; Menachery, V.D. The variant gambit: COVID-19’s next move. Cell Host Microbe 2021, 29, 508–515. [Google Scholar] [CrossRef] [PubMed]
- CDC Website. History of Ebola Virus Disease (EVD) Outbreaks. Available online: https://www.cdc.gov/vhf/ebola/history/chronology.html (accessed on 20 July 2021).
- Kuhn, J.H.; Amarasinghe, G.K.; Perry, D.L. Filoviridae. Fields VIROLOGY, 7th ed.; Emerging Viruses; Wolters Kluwer: Alphen aan den Rijn, The Netherlands, 2000; Volume 1. [Google Scholar]
- Languon, S.; Quaye, O. Filovirus Disease Outbreaks: A Chronological Overview. Virology 2019, 10, 1178122X19849927. [Google Scholar] [CrossRef] [PubMed]
- Adepoju, P. Ebola and COVID-19 in DR Congo and Guinea. Lancet Infect. Dis. 2021, 21, 461. [Google Scholar] [CrossRef]
- Mahase, E. Guinea reports west Africa’s first ever case of Marburg virus disease. BMJ 2021, 374, n1988. [Google Scholar] [CrossRef]
- WHO. Prioritizing Diseases for Research and Development in Emergency Contexts. Available online: https://www.who.int/activities/prioritizing-diseases-for-research-and-development-in-emergency-contexts (accessed on 22 September 2021).
- Kuhn, J.H.; Dodd, L.E.; Wahl-Jensen, V.; Radoshitzky, S.R.; Bavari, S.; Jahrling, P.B. Evaluation of perceived threat differences posed by filovirus variants. Biosecur. Bioterror. 2011, 9, 361–371. [Google Scholar] [CrossRef] [Green Version]
- Kuhn, J.H.; Bao, Y.; Bavari, S.; Becker, S.; Bradfute, S.; Brister, J.R.; Bukreyev, A.A.; Chandran, K.; Davey, R.A.; Dolnik, O.; et al. Virus nomenclature below the species level: A standardized nomenclature for natural variants of viruses assigned to the family Filoviridae. Arch. Virol. 2013, 158, 301–311. [Google Scholar] [CrossRef]
- Hirschberg, R.; Ward, L.A.; Kilgore, N.; Kurnat, R.; Schiltz, H.; Albrecht, M.T.; Christopher, G.W.; Nuzum, E. Challenges, progress, and opportunities: Proceedings of the filovirus medical countermeasures workshop. Viruses 2014, 6, 2673–2697. [Google Scholar] [CrossRef] [Green Version]
- Lever, M.S.; Piercy, T.J.; Steward, J.A.; Eastaugh, L.; Smither, S.J.; Taylor, C.; Salguero, F.J.; Phillpotts, R.J. Lethality and pathogenesis of airborne infection with filoviruses in A129 α/β -/- interferon receptor-deficient mice. J. Med. Microbiol. 2012, 61, 8–15. [Google Scholar] [CrossRef] [Green Version]
- Smither, S.J.; Eastaugh, L.; Ngugi, S.; O’Brien, L.; Phelps, A.; Steward, J.; Lever, M.S. Ebola Virus Makona Shows Reduced Lethality in an Immune-deficient Mouse Model. J. Infect. Dis. 2016, 214, S268–S274. [Google Scholar] [CrossRef] [Green Version]
- Kuhn, J.H.; Lofts, L.L.; Kugelman, J.R.; Smither, S.J.; Lever, M.S.; van der Groen, G.; Johnson, K.M.; Radoshitzky, S.R.; Bavari, S.; Jahrling, P.B.; et al. Reidentification of Ebola Virus E718 and ME as Ebola Virus/H.sapiens-tc/COD/1976/Yambuku-Ecran. Genome Announc. 2014, 2, e01178-14. [Google Scholar] [CrossRef] [PubMed]
- Smither, S.J.; Lear-Rooney, C.; Biggins, J.; Pettitt, J.; Lever, M.S.; Olinger, G.G. Comparison of the plaque assay and 50% tissue culture infectious dose assay as methods for measuring filovirus infectivity. J. Virol. Methods 2013, 193, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; Lever, M.S. Experimental aerosol survival of SARS-CoV-2 in artificial saliva and tissue culture media at medium and high humidity. Emerg. Microbes Infect. 2020, 9, 1415–1417. [Google Scholar] [CrossRef]
- Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; O’Brien, L.M.; Lever, M.S. Survival of Lassa Virus in Blood and Tissue Culture Media and in a Small Particle Aerosol. Pathogens 2020, 9, 680. [Google Scholar] [CrossRef]
- Thomas, R.J.; Webber, D.; Sellors, W.; Collinge, A.; Frost, A.; Stagg, A.J.; Bailey, S.C.; Jayasekera, P.N.; Taylor, R.R.; Eley, S.; et al. Characterization and deposition of respirable large- and small-particle bioaerosols. Appl. Environ. Microbiol. 2008, 74, 6437–6443. [Google Scholar] [CrossRef] [Green Version]
- Guyton, A.C. Measurement of the respiratory volumes of laboratory animals. Am. J. Physiol. 1947, 150, 70–77. [Google Scholar] [CrossRef] [Green Version]
- Harper, G.J.; Morton, J.D. The respiratory retention of bacterial aerosols: Experiments with radioactive spores. Epidemiol. Infect. 1953, 51, 372–385. [Google Scholar] [CrossRef] [Green Version]
- Mekibib, B.; Ariën, K.K. Aerosol Transmission of Filoviruses. Viruses 2016, 8, 148. [Google Scholar] [CrossRef] [Green Version]
- Leffel, E.K.; Reed, D.S. Marburg and Ebola viruses as aerosol threats. Biosecur. Bioterror. 2004, 2, 186–191. [Google Scholar] [CrossRef]
- Judson, S.D.; Munster, V.J. Nosocomial Transmission of Emerging Viruses via Aerosol-Generating Medical Procedures. Viruses 2019, 11, 940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fischer, R.J.; Bushmaker, T.; Judson, S.; Munster, V.J. Comparison of the Aerosol Stability of 2 Strains of Zaire ebolavirus from the 1976 and 2013 Outbreaks. J. Infect. Dis. 2016, 214, S290–S293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, N.H.L. Transmissibility and transmission of respiratory viruses. Nat. Rev. Microbiol. 2021, 19, 528–545. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W. The effect of environmental parameters on the survival of airborne infectious agents. J. R. Soc. Interface 2009, 6, S737–S746. [Google Scholar] [CrossRef] [Green Version]
- Benbough, J.E. Some factors affecting the survival of airborne viruses. J. Gen. Virol. 1971, 10, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Schaffer, F.L.; Soergel, M.E.; Straube, D.C. Survival of airborne influenza virus: Effects of propagating host, relative humidity, and composition of spray fluids. Arch. Virol. 1976, 51, 263–273. [Google Scholar] [CrossRef]
- Harper, G.J. Airborne micro-organisms: Survival tests with four viruses. J. Hyg. 1961, 59, 479–486. [Google Scholar] [CrossRef] [Green Version]
- Schuit, M.; Gardner, S.; Wood, S.; Bower, K.; Williams, G.; Freeburger, D.; Dabisch, P. The Influence of Simulated Sunlight on the Inactivation of Influenza Virus in Aerosols. J. Infect. Dis. 2020, 221, 372–378. [Google Scholar] [CrossRef]
- Schuit, M.; Biryukov, J.; Beck, K.; Yolitz, J.; Bohannon, J.; Weaver, W.; Miller, D.; Holland, B.; Krause, M.; Freeburger, D.; et al. The stability of an isolate of the SARS-CoV-2 B.1.1.7 lineage in aerosols is similar to three earlier isolates. J. Infect. Dis. 2021, 224, 1641–1648. [Google Scholar] [CrossRef]
- Bray, M. The role of the Type I interferon response in the resistance of mice to filovirus infection. J. Gen. Virol. 2001, 82, 1365–1373. [Google Scholar] [CrossRef]
- Yamaoka, S.; Ebihara, H. Pathogenicity and Virulence of Ebolaviruses with Species- and Variant-specificity. Virulence 2021, 12, 885–901. [Google Scholar] [CrossRef] [PubMed]
- Brannan, J.M.; Froude, J.W.; Prugar, L.I.; Bakken, R.R.; Zak, S.E.; Daye, S.P.; Wilhelmsen, C.E.; Dye, J.M. Interferon α/β Receptor-Deficient Mice as a Model for Ebola Virus Disease. J. Infect. Dis. 2015, 212, S282–S294. [Google Scholar] [CrossRef] [PubMed]
- Marzi, A.; Chadinah, S.; Haddock, E.; Feldmann, F.; Arndt, N.; Martellaro, C.; Scott, D.P.; Hanley, P.W.; Nyenswah, T.G.; Sow, S.; et al. Recently Identified Mutations in the Ebola Virus-Makona Genome Do Not Alter Pathogenicity in Animal Models. Cell Rep. 2018, 23, 1806–1816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, G.; Leung, A.; He, S.; Cao, W.; De La Vega, M.A.; Griffin, B.D.; Soule, G.; Kobinger, G.P.; Kobasa, D.; Qiu, X. The Makona Variant of Ebola Virus Is Highly Lethal to Immunocompromised Mice and Immunocompetent Ferrets. J. Infect. Dis. 2018, 218, S466–S470. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.; Leung, A.; Griffin, B.D.; Vendramelli, R.; Tailor, N.; Tierney, K.; Audet, J.; Kobasa, D. Generation and Characterization of a Mouse-Adapted Makona Variant of Ebola Virus. Viruses 2019, 11, 987. [Google Scholar] [CrossRef] [Green Version]
- Arcos González, P.; Fernández Camporro, Á.; Eriksson, A.; Alonso Llada, C. The Epidemiological Presentation Pattern of Ebola Virus Disease Outbreaks: Changes from 1976 to 2019. Prehosp. Disaster Med. 2020, 35, 247–253. [Google Scholar] [CrossRef]

| Virus | Ebola Virus | Marburg Virus | |||
|---|---|---|---|---|---|
| Variant-Isolate used in this work | Yambuku-Ecran | 13625-Kikwit | Makona-C07 | Hesse-Poppinga | Angola-200501379 |
| Name in this paper | EBOV-Ecran | EBOV-Kikwit | EBOV-Makona | MARV-Popp | MARV-Angola |
| Country of origin | Zaire | Zaire | Guinea 1 | Uganda 2 | Angola |
| Year of outbreak | 1976 | 1995 | 2013–2016 | 1967 | 2004–2005 |
| No. fatalities/Total No. cases | 280/318 | 245/317 | 11,325/28,652 | 7/31 | 227/252 |
| Case fatality rate | 88% | 77% | 40% | 23% | 90% |
| Passage used | 4 | 3 | 6 | 8 | 4 |
| Stock titre (TCID50/mL) | 1 × 107 | 1 × 107 | 8 × 106 | 2 × 107 | 1 × 107 |
| Illumina MiSeq sequencing top hit (NCBI Reference No.) | Ebola virus/H.sapiens-tc/COD/1976/Yambuku-Mayinga (NC_002549) | Ebola virus/H.sapiens-tc/COD/1995/Kikwit-807223 (KR063672) | Ebola virus/H.sapiens-wt/GIN/2014/Makona-C05 (KT013255) | n/d, partial sequencing and PCR confirmation only | Marburg virus/H.sapiens-tc/AGO/2005/Angola-200501379 (KR867677) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smither, S.J.; Eastaugh, L.S.; Lever, M.S. Comparison of Aerosol Stability of Different Variants of Ebola Virus and Marburg Virus and Virulence of Aerosolised Ebola Virus in an Immune-Deficient Mouse. Viruses 2022, 14, 780. https://doi.org/10.3390/v14040780
Smither SJ, Eastaugh LS, Lever MS. Comparison of Aerosol Stability of Different Variants of Ebola Virus and Marburg Virus and Virulence of Aerosolised Ebola Virus in an Immune-Deficient Mouse. Viruses. 2022; 14(4):780. https://doi.org/10.3390/v14040780
Chicago/Turabian StyleSmither, Sophie J., Lin S. Eastaugh, and Mark S. Lever. 2022. "Comparison of Aerosol Stability of Different Variants of Ebola Virus and Marburg Virus and Virulence of Aerosolised Ebola Virus in an Immune-Deficient Mouse" Viruses 14, no. 4: 780. https://doi.org/10.3390/v14040780
APA StyleSmither, S. J., Eastaugh, L. S., & Lever, M. S. (2022). Comparison of Aerosol Stability of Different Variants of Ebola Virus and Marburg Virus and Virulence of Aerosolised Ebola Virus in an Immune-Deficient Mouse. Viruses, 14(4), 780. https://doi.org/10.3390/v14040780





