Development and Scalable Production of Newcastle Disease Virus-Vectored Vaccines for Human and Veterinary Use
Abstract
1. Introduction
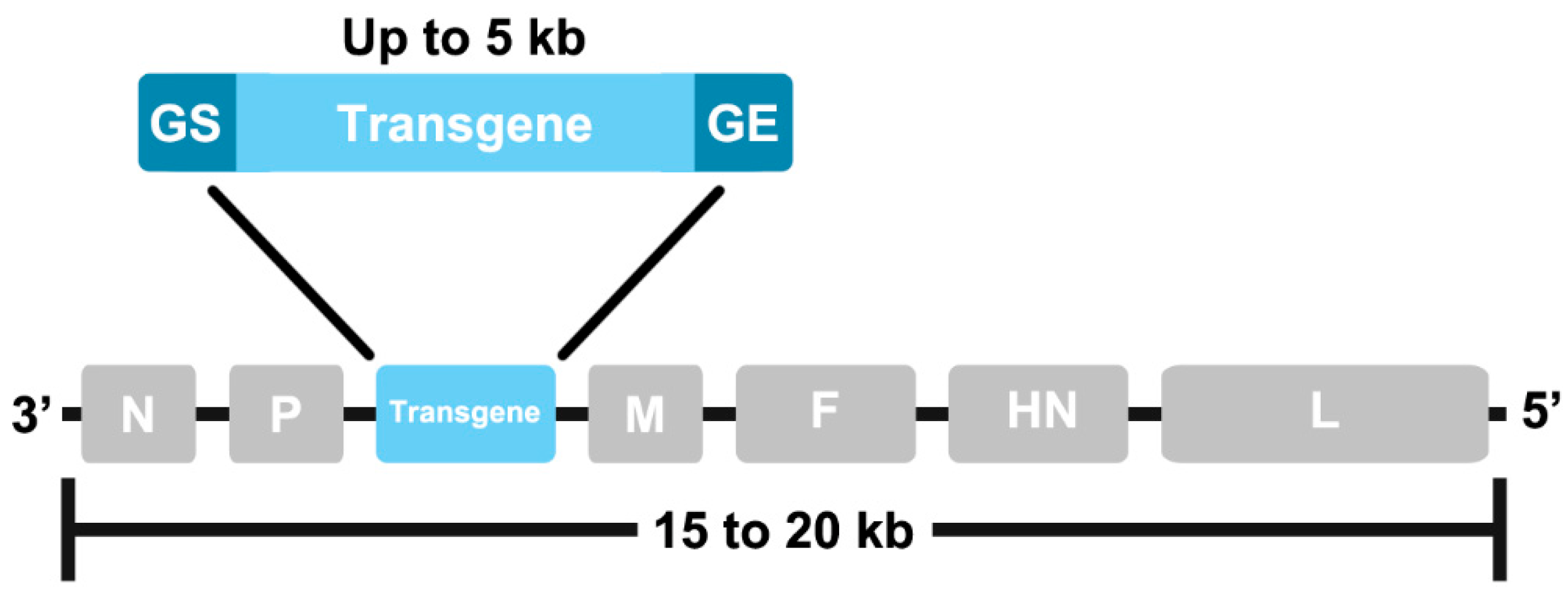
2. Characteristics of NDV as a Viral Vector
3. Designing and Generating Recombinant NDV
4. NDV-Vectored Vaccines
4.1. Vaccines for Human Use
4.2. Vaccines for Veterinary Use
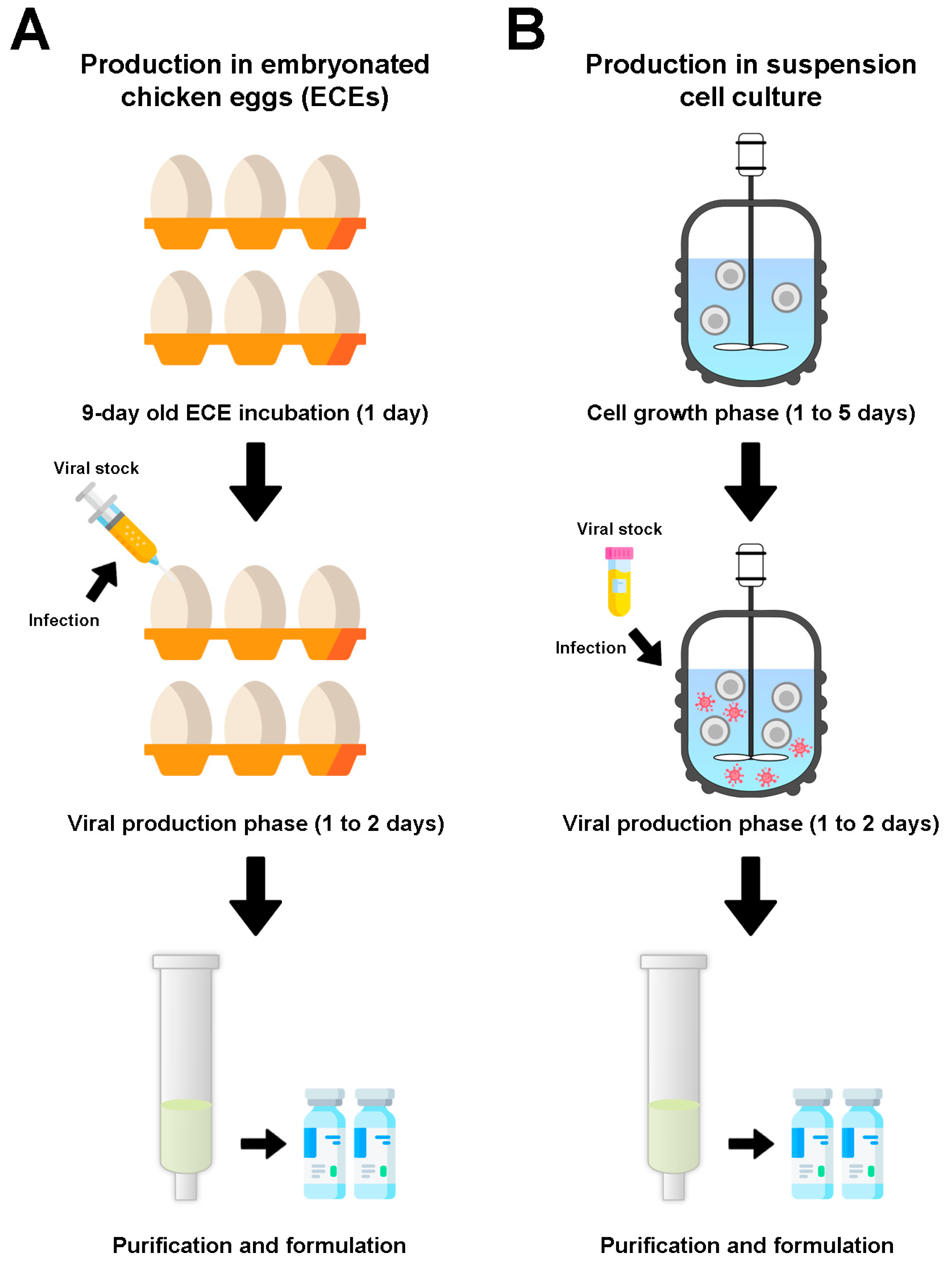
5. Manufacturing of NDV-Vectored Vaccines
5.1. Workflow for Viral Vector Production
5.2. Parameters for NDV Production in Cell Culture
5.3. NDV Production in Lab-Scale Bioreactors
5.4. Downstream Processing and Formulation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Vaccine Type | Pathogen | Disease | Antigen Expressed | Animal Model | Production Platform * | Route * | Dose * | Reference |
|---|---|---|---|---|---|---|---|---|
| Live B1 Strain | HPAIV H7N2 | Respiratory infection | HA | Chicken | ECEs | io | one dose of 1 × 106 EID50 | [116] |
| Live B1 strain | SIV | Simian AIDS | Gag | Mouse | ECEs | iv, ip, in | one or two doses of 5 × 107 PFU | [117] |
| Live LaSota strain | IBDV | Infectious bursal disease | VP2 | Chicken | ECEs | io | one or two doses of 1 × 104 EID50 | [118] |
| Live Clone 30 strain | HPAIV H5N1 | Respiratory infection | HA | Chicken | ECEs | on | one dose of 106 EID50 | [82] |
| Live B1 Strain | HPAIV H7N2 | Respiratory infection | HA | Chicken | ECEs, MDCK cell line | io | one or two doses of 5 × 105 to 1.25 × 106 mean EID50 | [41] |
| Live LaSota strain | HPAIV H5N1 | Flu (respiratory infection) | HA | Chicken, mouse | ECEs | on (chicken), ip (mice) | one dose of 106 EID50 (chicken), two doses of 108 EID50 (mice) | [83] |
| Live LaSota strain | HPAIV H7N1 | Respiratory infection | HA | Chicken | ECEs | in | one dose of 1 × 106 EID50 | [119] |
| Live LaSota strain | HPAIV H5N1 | Respiratory infection | HA | Chicken | ECEs | on | one dose of 1 × 106 EID50 | [84] |
| Live LaSota strain | HPAIV H5N2 | Respiratory infection | HA | Chicken | ECEs | io | one dose of 6 × 104, 6 × 105, 6 × 106 or 6 × 107 mean EID50 | [120] |
| Live LaSota strain | RVFV | Rift Valley fever | Gn | Calf | ECEs | in, im | one dose of 2 × 106 TCID50 (in), one dose of 3 × 107 TCID50 (im) | [121] |
| Live LaSota strain | BHV-1 | Respiratory infection | gD | Calf | ECEs | in + it | one dose of 1.5 × 107 PFU | [122] |
| Live LaSota strain | RVFV | Rift Valley fever | Gn/Gc | Mouse, lamb | ECEs | im | two doses of 2 × 105 TCID50 (mice), two doses of 2 × 107 TCID50 (lambs) | [51] |
| Live Clone 30 strain | HPAIV H6N2 | Respiratory infection | HA | Chicken, turkey | ECEs | on | one dose of 106 EID50 (chicken) or 107 EID50 (turkeys) | [123] |
| Live LaSota/VF strain | Borrelia burgdorferi | Lyme | BmpA, OspC | Hamster | ECEs | in, im, ip | one or two doses of 1 × 106 PFU | [69] |
| Live LaSota strain | RV | Rabies | G | Mouse, cat, dog | ECEs | im | one dose of 2 × 108 EID50, 2 × 107 EID50 or 2 × 106 EID50 (mice); three doses of 6 × 109 EID50 (cats); three doses of 6 × 109 EID50, 2 × 109 EID50 or 2 × 108 EID50 (dogs) | [109] |
| Live LaSota strain | AMPV | Respiratory infection | G | Turkey | ECEs | in, io | one or two doses of 106 TCID50 | [124] |
| Live LaSota strain | NiV | Encephalitis | F, G | Mouse, pig | ECEs | im | two doses of 1 × 108 EID50 (mice), two doses of 2 × 109 EID50 (pigs) | [71] |
| Live LaSota strain | HPAIV H7N9 | Respiratory infection | HA | Mouse | ECEs | in | two doses of 104 or 106 FFU | [125] |
| Live chimeric NDV | HPAIV H5N1 | Respiratory infection | HA | Chicken | ECEs | on | one dose of 106 TCID50 | [96] |
| Live LaSota strain | IBV | Respiratory infection | S2 | Chicken | ECEs | io | one dose of 106 EID50 followed by one dose of an attenuated IBV vaccine | [126] |
| Live LaSota strain | HPAIV H5N1 | Respiratory infection | HA | Duck | ECEs | io | two doses of 106 EID50 | [90] |
| Live LaC30L strain | IBDV | Infectious bursal disease | VP2 | Chicken embryo | ECEs | in ovo | one dose of 3 × 102, 3 × 103, 3 × 104 or 3 × 105 EID50 | [127] |
| Live LaSota strain | ILTV | Respiratory infection | gB, gC, gD | Chicken | ECEs | on | two doses of 2 × 105 TCID50 | [86] |
| Live LaSota strain | ILTV | Respiratory infection | gB, gD | Chicken | ECEs | in + io | one dose of 1 × 106 TCID50 | [87] |
| Live NA strain | GPV | Derzsy’s disease (goose hepatitis) | VP3 | Gosling | ECEs | sc | two doses of 106 EID50 | [91] |
| Live LaSota strain | CDV | Canine distemper | F, HN | Mink | ECEs | im | two doses of 109 EID50 | [93] |
| Live LaSota strain | H7N9, H5N1 | Respiratory infection | HA | Chicken | ECEs | im, on | two doses of 5 × 106 PFU | [128] |
| Live LaSota strain | VSV | Vesicular stomatitis | G | Mouse | ECEs | im | two doses of 1 × 107 TCID50 | [129] |
| Live LaSota strain | HPAIV H9N2 | Respiratory infection | HA | Chicken | ECEs | on, im | two doses of 107 FFU | [130] |
| Live LaSota strain | WNV | West Nile fever | PrM/E | Mouse, horse, chicken, duck, goose | ECEs | im, in, oral | two doses of 1 × 108 EID50 (im) (mice); two doses of 2 × 109 EID50 (im) (horses); two doses of 1 × 108 EID50 (im) or 1 × 1010 EID50 (oral) (chicken); two doses of 5 × 108 EID50 (im, in, or oral) (geese) | [131] |
| Live LaSota strain | BEFV | Bovine ephemeral fever | G | Mouse, calf | ECEs | im | one dose of 1 × 106 TCID50 (mice), two doses 8 × 107 TCID50 (calves) | [132] |
| Live Clone 30 strain | PaBV-4, CnBV-2 | Proventricular dilatation disease | N/P | Cockatiel, canary | ECEs | im | one dose of 8 × 105 FFU to 1 × 106 FFU (cockatiel) or 4 × 106 FFU (canary) | [94] |
| Live chimeric NDV | HPAIV H5N1 | Respiratory infection | HA | Chicken | ECEs | on | two doses of 106 PFU/mL | [97] |
| Live LaSota strain | IBV | Respiratory infection | S1 | Chicken | ECEs | on | one or two doses of 106 PFU | [133] |
| Live LaSota strain | AMPV | Respiratory infection | F/G | Turkey | ECEs | in, io | one dose of 106 TCID50 | [52] |
| Live LaSota strain or chimeric NDV | HPAIV H5N1 | Respiratory infection | HA, HA/NA, HA/M1, HA/NS1 | Chicken | ECEs | on | one dose of 106 PFU/mL or two doses: prime with chimeric NDV construct, boost with LaSota construct (106 PFU/mL) | [55] |
| Live F strain | IBDV | Infectious bursal disease | VP2 | Chicken | ECEs, Vero cell line | in | two doses of 105, 106 or 107 EID50 | [106] |
| Live LaSota strain | MERS-CoV | Respiratory infection | S | Mouse, camel | ECEs | im | two doses of 108 EID50 (mouse) or 1 × 109 EID50 (camel) | [134] |
| Live or inactivated LaSota strain | HPAIV H5N2 | Respiratory infection | HA | Chicken | ECEs | im, spraying | two doses of 5 × 106 TCID50 (im live) or 107 TCID50 (im inactivated); around 106 TCID50 (spraying) | [135] |
| Live LX strain | HPAIV H7N9 | Respiratory infection | HA | Chicken | ECEs | in | two doses of 5 × 106 EID50 | [136] |
| Live attenuated GM strain | DTMUV | Duck Tembusu virus disease | PrM/E | Duck | ECEs | sc | two doses of 106 EID50 | [89] |
| Live LaSota strain or chimeric NDV | SIV | Simian AIDS | Env (gp160) | Guinea pig | ECEs | in | two doses of 105 TCID50 | [32] |
| Live chimeric NDV | HPAIV H9N2 | Respiratory infection | HA | Chicken | ECEs | on | one dose of 106 EID50 | [98] |
| Live LaSota strain or chimeric NDV | HPAIV H5N2 | Respiratory infection | HA/NA | Chicken | ECEs | in | two doses: prime with chimeric NDV construct (1 × 105 PFU), boost with LaSota construct (2 × 105 PFU) | [53] |
| Live rAI4 strain | HPAIV H7N9 | Respiratory infection | HA | Chicken | ECEs | in, io | one dose of 106 EID50 | [137] |
| Live NA Strain | HPAIV H9N2 | Respiratory infection | HA | Chicken | ECEs | on | one or two doses of 106 EID50 | [138] |
| Live LaSota strain | IBV | Respiratory infection | S | Chicken | ECEs | on | one or two doses of 1 × 106 PFU | [139] |
| Live LaSota strain or chimeric NDV | HPAIV H7N8 | Respiratory infection | HA, HA/NA | Chicken, turkey | ECEs | in | two doses: prime with chimeric NDV construct (1 × 105 PFU), boost with LaSota construct (2 × 105 PFU) | [56] |
| Live R2B strain | ARV | Viral arthritis/tenosynovitis | σC | Chicken | ECEs | oral + in, im | two doses of 1 × 105 EID50 | [85] |
| Live SH12 strain | GoAstV | Visceral gout | Cap | Gosling | ECEs | on | one dose of 1 × 107 TCID50 | [92] |
| Live LaSota strain | CSFV | Classical swine fever | E2, Erns | Pig | ECEs | in | two doses of 103 TCID50 | [140] |
| Live LaSota strain | IBV | Respiratory infection | S1 (multi-epitope) | Chicken | ECEs | on | one dose of 1 × 106 EID50 | [141] |
| Live LaSota strain | PRRSV | Porcine reproductive and respiratory syndrome | GP5, GP3/GP5 | Piglet | ECEs | im | two doses of 4 × 108 EID50 | [57] |
| Live TS09-C (thermostable) strain | HPAIV H5N1 | Respiratory infection | HA, HA1 | Chicken | ECEs | in, io | two doses of 106 TCID50 | [95] |
| Live LaSota strain | FAdV-4 | Hepatitis-hydropericardium syndrome | Fiber 2 | Chicken | ECEs | im | one dose of 107 EID50 | [88] |
| Live Clone 30 strain | PPRV | Peste des petits ruminants (PPR) | H | Goat | CEFs | sc | one or two doses of 6 × 106 TCID50/mL | [142] |
| Live R2B strain or chimeric NDV | RV | Rabies | G | Mouse | ECEs | im | two doses of 2 × 106 TCID50 | [110] |
| Live HR09 (thermostable) strain | HPAIV H9N2 | Respiratory infection | HA, chimeric HA | Chicken | ECEs | on | one dose of 106 EID50 | [14] |
| Live LaSota strain | IBV | Respiratory infection | N (multi-epitope) | Chicken | ECEs | on | one dose of 106 EID50 | [143] |
| Live LaSota strain | PPRV | Peste des petits ruminants (PPR) | H | Sheep, goat | ECEs | im | two doses of 1 × 108, 5 × 108 or 3 × 109 EID50 | [115] |
| Live R2B strain | CIAV | Chicken infectious anaemia | VP1/VP2 | Chicken | Vero cell line | on | three doses of 1 × 106 TCID50/mL | [58] |
| Live K148/08 strain | HPAIV H5N6 | Respiratory infection | HA | Chicken, duck | ECEs | on, spray | two doses of 107 EID50 | [144] |
References
- Kim, S.-H.; Samal, S.K. Newcastle Disease Virus as a Vaccine Vector for Development of Human and Veterinary Vaccines. Viruses 2016, 8, 183. [Google Scholar] [CrossRef] [PubMed]
- Annas, S.; Zamri-Saad, M. Intranasal Vaccination Strategy to Control the COVID-19 Pandemic from a Veterinary Medicine Perspective. Animals 2021, 11, 1876. [Google Scholar] [CrossRef] [PubMed]
- Fulber, J.P.C.; Farnós, O.; Kiesslich, S.; Yang, Z.; Dash, S.; Susta, L.; Wootton, S.K.; Kamen, A.A. Process Development for Newcastle Disease Virus-Vectored Vaccines in Serum-Free Vero Cell Suspension Cultures. Vaccines 2021, 9, 1335. [Google Scholar] [CrossRef] [PubMed]
- Kon, E.; Elia, U.; Peer, D. Principles for designing an optimal mRNA lipid nanoparticle vaccine. Curr. Opin. Biotechnol. 2022, 73, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Crommelin, D.J.A.; Anchordoquy, T.J.; Volkin, D.B.; Jiskoot, W.; Mastrobattista, E. Addressing the Cold Reality of mRNA Vaccine Stability. J. Pharm. Sci. 2021, 110, 997–1001. [Google Scholar] [CrossRef]
- Crommelin, D.J.A.; Volkin, D.B.; Hoogendoorn, K.H.; Lubiniecki, A.S.; Jiskoot, W. The Science is There: Key Considerations for Stabilizing Viral Vector-Based COVID-19 Vaccines. J. Pharm. Sci. 2021, 110, 627–634. [Google Scholar] [CrossRef]
- Samaranayake, L.P.; Seneviratne, C.J.; Fakhruddin, K.S. Coronavirus disease 2019 (COVID-19) vaccines: A concise review. Oral Dis. 2021, 1–11. [Google Scholar] [CrossRef]
- Tomori, O.; Kolawole, M.O. Ebola virus disease: Current vaccine solutions. Curr. Opin. Immunol. 2021, 71, 27–33. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA). Zabdeno Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/zabdeno-epar-product-information_en.pdf (accessed on 8 October 2021).
- European Medicines Agency (EMA). Mvabea Summary of Product Characteristics. Available online: https://www.ema.europa.eu/en/documents/product-information/mvabea-epar-product-information_en.pdf (accessed on 8 October 2021).
- Henao-Restrepo, A.M.; Camacho, A.; Longini, I.M.; Watson, C.H.; Edmunds, W.J.; Egger, M.; Carroll, M.W.; Dean, N.E.; Diatta, I.; Doumbia, M.; et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: Final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 2017, 389, 505–518. [Google Scholar] [CrossRef]
- Pinschewer, D.D. Virally vectored vaccine delivery: Medical needs, mechanisms, advantages and challenges. Swiss Med. Wkly. 2017, 147, w14465. [Google Scholar] [CrossRef]
- Yoshida, A.; Kim, S.-H.; Manoharan, V.K.; Varghese, B.P.; Paldurai, A.; Samal, S.K. Novel avian paramyxovirus-based vaccine vectors expressing the Ebola virus glycoprotein elicit mucosal and humoral immune responses in guinea pigs. Sci. Rep. 2019, 9, 5520. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Bo, Z.; Meng, C.; Chen, Y.; Zhang, C.; Cao, Y.; Wu, Y. Generation and Evaluation of Recombinant Thermostable Newcastle Disease Virus Expressing the HA of H9N2 Avian Influenza Virus. Viruses 2021, 13, 1606. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.-S. Newcastle disease virus vectored vaccines as bivalent or antigen delivery vaccines. Clin. Exp. Vaccine Res. 2017, 6, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Bello, M.B.; Yusoff, K.; Ideris, A.; Hair-Bejo, M.; Jibril, A.H.; Peeters, B.P.H.; Omar, A.R. Exploring the Prospects of Engineered Newcastle Disease Virus in Modern Vaccinology. Viruses 2020, 12, 451. [Google Scholar] [CrossRef]
- Burman, B.; Pesci, G.; Zamarin, D. Newcastle Disease Virus at the Forefront of Cancer Immunotherapy. Cancers 2020, 12, 3552. [Google Scholar] [CrossRef]
- Sun, W.; Leist, S.R.; McCroskery, S.; Liu, Y.; Slamanig, S.; Oliva, J.; Amanat, F.; Schäfer, A.; Dinnon, K.H.; García-Sastre, A.; et al. Newcastle disease virus (NDV) expressing the spike protein of SARS-CoV-2 as a live virus vaccine candidate. EBioMedicine 2020, 62, 103132. [Google Scholar] [CrossRef]
- Silva, C.A.T.; Kamen, A.A.; Henry, O. Recent advances and current challenges in process intensification of cell culture-based influenza virus vaccine manufacturing. Can. J. Chem. Eng. 2021, 99, 2525–2535. [Google Scholar] [CrossRef]
- Bukreyev, A.; Huang, Z.; Yang, L.; Elankumaran, S.; Claire, M.S.; Murphy, B.R.; Samal, S.K.; Collins, P.L. Recombinant Newcastle Disease Virus Expressing a Foreign Viral Antigen Is Attenuated and Highly Immunogenic in Primates. J. Virol. 2005, 79, 13275–13284. [Google Scholar] [CrossRef]
- Shimkin, N. Conjunctival haemorrhage due to an infection of Newcastle virus of fowls in man (laboratory and contact infection). Br. J. Ophthalmol. 1946, 30, 260. [Google Scholar] [CrossRef]
- Nelson, C.; Pomeroy, B.; Schrall, K.; Park, W.; Lindeman, R. An outbreak of conjunctivitis due to Newcastle disease virus (NDV) occurring in poultry workers. Am. J. Public Health Nations Health 1952, 42, 672–678. [Google Scholar] [CrossRef]
- Mustaffa-Babjee, A.; Ibrahim, A.L.; Khim, T.S. A case of human infection with Newcastle disease virus. Southeast Asian J. Trop. Med. Public Health 1976, 7, 622–624. [Google Scholar] [PubMed]
- Prajna, N.V.; Lalitha, P.; Chen, C.; Zhong, L.; Lietman, T.M.; Doan, T.; Seitzman, G.D. Acute keratoconjunctivitis resulting from coinfection with avian Newcastle virus and human adenovirus. Cornea 2022, 41, 630–631. [Google Scholar] [CrossRef] [PubMed]
- Fausther-Bovendo, H.; Kobinger, G.P. Pre-existing immunity against Ad vectors. Hum. Vaccines Immunother. 2014, 10, 2875–2884. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-G.; Oladunni, F.S.; Rohaim, M.A.; Whittingham-Dowd, J.; Tollitt, J.; Hodges, M.D.J.; Fathallah, N.; Assas, M.B.; Alhazmi, W.; Almilaibary, A.; et al. Immunogenicity and protective efficacy of an intranasal live-attenuated vaccine against SARS-CoV-2. iScience 2021, 24, 102941. [Google Scholar] [CrossRef] [PubMed]
- Warner, B.M.; Santry, L.A.; Leacy, A.; Chan, M.; Pham, P.H.; Vendramelli, R.; Pei, Y.; Tailor, N.; Valcourt, E.; Leung, A.; et al. Intranasal vaccination with a Newcastle disease virus-vectored vaccine protects hamsters from SARS-CoV-2 infection and disease. iScience 2021, 24, 103219. [Google Scholar] [CrossRef] [PubMed]
- DiNapoli, J.M.; Kotelkin, A.; Yang, L.; Elankumaran, S.; Murphy, B.R.; Samal, S.K.; Collins, P.L.; Bukreyev, A. Newcastle disease virus, a host range-restricted virus, as a vaccine vector for intranasal immunization against emerging pathogens. Proc. Natl. Acad. Sci. USA 2007, 104, 9788. [Google Scholar] [CrossRef]
- DiNapoli, J.M.; Yang, L.; Samal, S.K.; Murphy, B.R.; Collins, P.L.; Bukreyev, A. Respiratory tract immunization of non-human primates with a Newcastle disease virus-vectored vaccine candidate against Ebola virus elicits a neutralizing antibody response. Vaccine 2010, 29, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Tcheou, J.; Raskin, A.; Singh, G.; Kawabata, H.; Bielak, D.; Sun, W.; González-Domínguez, I.; Sather, D.N.; García-Sastre, A.; Palese, P.; et al. Safety and Immunogenicity Analysis of a Newcastle Disease Virus (NDV-HXP-S) Expressing the Spike Protein of SARS-CoV-2 in Sprague Dawley Rats. Front. Immunol. 2021, 12, 791764. [Google Scholar] [CrossRef]
- Lara-Puente, J.H.; Carreño, J.M.; Sun, W.; Suárez-Martínez, A.; Ramírez-Martínez, L.; Quezada-Monroy, F.; de la Rosa, G.P.; Vigueras-Moreno, R.; Singh, G.; Rojas-Martínez, O.; et al. Safety and Immunogenicity of a Newcastle Disease Virus Vector-Based SARS-CoV-2 Vaccine Candidate, AVX/COVID-12-HEXAPRO (Patria), in Pigs. mBio 2021, 12, e01908-21. [Google Scholar] [CrossRef]
- Manoharan, V.K.; Khattar, S.K.; Labranche, C.C.; Montefiori, D.C.; Samal, S.K. Modified Newcastle Disease virus as an improved vaccine vector against Simian Immunodeficiency virus. Sci. Rep. 2018, 8, 8952. [Google Scholar] [CrossRef]
- Gallo, O.; Locatello, L.G.; Mazzoni, A.; Novelli, L.; Annunziato, F. The central role of the nasal microenvironment in the transmission, modulation, and clinical progression of SARS-CoV-2 infection. Mucosal. Immunol. 2021, 14, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Freeman, A.I.; Zakay-Rones, Z.; Gomori, J.M.; Linetsky, E.; Rasooly, L.; Greenbaum, E.; Rozenman-Yair, S.; Panet, A.; Libson, E.; Irving, C.S.; et al. Phase I/II Trial of Intravenous NDV-HUJ Oncolytic Virus in Recurrent Glioblastoma Multiforme. Mol. Ther. 2006, 13, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Schirrmacher, V. Fifty Years of Clinical Application of Newcastle Disease Virus: Time to Celebrate! Biomedicines 2016, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Schirrmacher, V.; van Gool, S.; Stuecker, W. Breaking Therapy Resistance: An Update on Oncolytic Newcastle Disease Virus for Improvements of Cancer Therapy. Biomedicines 2019, 7, 66. [Google Scholar] [CrossRef]
- Meng, Q.; He, J.; Zhong, L.; Zhao, Y. Advances in the Study of Antitumour Immunotherapy for Newcastle Disease Virus. Int. J. Med. Sci. 2021, 18, 2294–2302. [Google Scholar] [CrossRef] [PubMed]
- Santry, L.A.; McAusland, T.M.; Susta, L.; Wood, G.A.; Major, P.P.; Petrik, J.J.; Bridle, B.W.; Wootton, S.K. Production and purification of high-titer Newcastle disease virus for use in preclinical mouse models of cancer. Mol. Ther.-Methods Clin. Dev. 2018, 9, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Yurchenko, K.; Yi, J.; Shestopalov, A. Adaptation of the Newcastle disease virus to cell cultures for enhancing its oncolytic properties. Acta Nat. 2019, 11, 66–73. [Google Scholar] [CrossRef]
- DiNapoli, J.M.; Yang, L.; Suguitan, A., Jr.; Elankumaran, S.; Dorward, D.W.; Murphy, B.R.; Samal, S.K.; Collins, P.L.; Bukreyev, A. Immunization of primates with a Newcastle disease virus-vectored vaccine via the respiratory tract induces a high titer of serum neutralizing antibodies against highly pathogenic avian influenza virus. J. Virol. 2007, 81, 11560–11568. [Google Scholar] [CrossRef]
- Park, M.-S.; Steel, J.; García-Sastre, A.; Swayne, D.; Palese, P. Engineered viral vaccine constructs with dual specificity: Avian influenza and Newcastle disease. Proc. Natl. Acad. Sci. USA 2006, 103, 8203–8208. [Google Scholar] [CrossRef]
- Zhan, Y.; Yu, S.; Yang, S.; Qiu, X.; Meng, C.; Tan, L.; Song, C.; Liao, Y.; Liu, W.; Sun, Y.; et al. Newcastle Disease virus infection activates PI3K/Akt/mTOR and p38 MAPK/Mnk1 pathways to benefit viral mRNA translation via interaction of the viral NP protein and host eIF4E. PLOS Pathog. 2020, 16, e1008610. [Google Scholar] [CrossRef]
- Schirrmacher, V. Immunobiology of Newcastle disease virus and its use for prophylactic vaccination in poultry and as adjuvant for therapeutic vaccination in cancer patients. Int. J. Mol. Sci. 2017, 18, 1103. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Xue, J.; Teng, Q.; Li, X.; Bu, Y.; Zhang, G. Mechanisms and consequences of Newcastle disease virus W protein subcellular localization in the nucleus or mitochondria. J. Virol. 2021, 95, e02087-20. [Google Scholar] [CrossRef] [PubMed]
- Vijayakumar, G.; Zamarin, D. Design and Production of Newcastle Disease Virus for Intratumoral Immunomodulation. In Oncolytic Viruses; Engeland, C.E., Ed.; Springer New York: New York, NY, USA, 2020; pp. 133–154. [Google Scholar]
- Gao, Q.; Park, M.-S.; Palese, P. Expression of Transgenes from Newcastle Disease Virus with a Segmented Genome. J. Virol. 2008, 82, 2692–2698. [Google Scholar] [CrossRef] [PubMed]
- Cardenas-Garcia, S.; Afonso, C.L. Reverse genetics of Newcastle disease virus. In Reverse Genetics of RNA Viruses; Springer: Berlin/Heidelberg, Germany, 2017; pp. 141–158. [Google Scholar]
- Pühler, F.; Willuda, J.; Puhlmann, J.; Mumberg, D.; Römer-Oberdörfer, A.; Beier, R. Generation of a recombinant oncolytic Newcastle disease virus and expression of a full IgG antibody from two transgenes. Gene Ther. 2008, 15, 371–383. [Google Scholar] [CrossRef]
- Viktorova, E.G.; Khattar, S.K.; Kouiavskaia, D.; Laassri, M.; Zagorodnyaya, T.; Dragunsky, E.; Samal, S.; Chumakov, K.; Belov, G.A.; Pfeiffer, J.K. Newcastle Disease Virus-Based Vectored Vaccine against Poliomyelitis. J. Virol. 2018, 92, e00976-18. [Google Scholar] [CrossRef]
- Khattar, S.K.; Manoharan, V.; Bhattarai, B.; LaBranche, C.C.; Montefiori, D.C.; Samal, S.K.; Meng, X.-J. Mucosal Immunization with Newcastle Disease Virus Vector Coexpressing HIV-1 Env and Gag Proteins Elicits Potent Serum, Mucosal, and Cellular Immune Responses That Protect against Vaccinia Virus Env and Gag Challenges. mBio 2015, 6, e01005. [Google Scholar] [CrossRef]
- Kortekaas, J.; de Boer, S.M.; Kant, J.; Vloet, R.P.M.; Antonis, A.F.G.; Moormann, R.J.M. Rift Valley fever virus immunity provided by a paramyxovirus vaccine vector. Vaccine 2010, 28, 4394–4401. [Google Scholar] [CrossRef]
- Hu, H.; Roth, J.P.; Zsak, L.; Yu, Q. Engineered Newcastle disease virus expressing the F and G proteins of AMPV-C confers protection against challenges in turkeys. Sci. Rep. 2017, 7, 4025. [Google Scholar] [CrossRef]
- Cho, Y.; Lamichhane, B.; Nagy, A.; Chowdhury, I.R.; Samal, S.K.; Kim, S.-H. Co-expression of the Hemagglutinin and Neuraminidase by Heterologous Newcastle Disease Virus Vectors Protected Chickens against H5 Clade 2.3.4.4 HPAI Viruses. Sci. Rep. 2018, 8, 16854. [Google Scholar] [CrossRef]
- Murr, M.; Karger, A.; Steglich, C.; Mettenleiter, T.C.; Römer-Oberdörfer, A. Coexpression of soluble and membrane-bound avian influenza virus H5 by recombinant Newcastle disease virus leads to an increase in antigen levels. J. Gen. Virol. 2020, 101, 473–483. [Google Scholar] [CrossRef]
- Kim, S.-H.; Samal, S.K. Heterologous prime-boost immunization of Newcastle disease virus vectored vaccines protected broiler chickens against highly pathogenic avian influenza and Newcastle disease viruses. Vaccine 2017, 35, 4133–4139. [Google Scholar] [CrossRef] [PubMed]
- Roy Chowdhury, I.; Yeddula, S.G.R.; Pierce, B.G.; Samal, S.K.; Kim, S.-H. Newcastle disease virus vectors expressing consensus sequence of the H7 HA protein protect broiler chickens and turkeys against highly pathogenic H7N8 virus. Vaccine 2019, 37, 4956–4962. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Nan, F.; Li, Z.; Zhao, G.; Xie, C.; Ha, Z.; Zhang, J.; Han, J.; Xiao, P.; Zhuang, X.; et al. Construction and immunological evaluation of recombinant Newcastle disease virus vaccines expressing highly pathogenic porcine reproductive and respiratory syndrome virus GP3/GP5 proteins in pigs. Vet. Microbiol. 2019, 239, 108490. [Google Scholar] [CrossRef] [PubMed]
- Chellappa, M.M.; Dey, S.; Pathak, D.C.; Singh, A.; Ramamurthy, N.; Ramakrishnan, S.; Mariappan, A.K.; Dhama, K.; Vakharia, V.N. Newcastle Disease Virus Vectored Chicken Infectious Anaemia Vaccine Induces Robust Immune Response in Chickens. Viruses 2021, 13, 1985. [Google Scholar] [CrossRef]
- He, L.; Zhang, Z.; Yu, Q. Expression of Two Foreign Genes by a Newcastle Disease Virus Vector From the Optimal Insertion Sites through a Combination of the ITU and IRES-Dependent Expression Approaches. Front. Microbiol. 2020, 11, 769. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Samal, S.K. Role of Untranslated Regions in Regulation of Gene Expression, Replication, and Pathogenicity of Newcastle Disease Virus Expressing Green Fluorescent Protein. J. Virol. 2010, 84, 2629–2634. [Google Scholar] [CrossRef] [PubMed]
- Ayllon, J.; García-Sastre, A.; Martínez-Sobrido, L. Rescue of recombinant Newcastle disease virus from cDNA. J. Vis. Exp. JoVE 2013, 80, 50830. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhang, Z.; Zsak, L.; Yu, Q. P and M gene junction is the optimal insertion site in Newcastle disease virus vaccine vector for foreign gene expression. J. Gen. Virol. 2015, 96, 40–45. [Google Scholar] [CrossRef]
- Molouki, A.; Peeters, B. Rescue of recombinant Newcastle disease virus: Current cloning strategies and RNA polymerase provision systems. Arch. Virol. 2017, 162, 1–12. [Google Scholar] [CrossRef]
- Hu, Z.; Ni, J.; Cao, Y.; Liu, X. Newcastle Disease Virus as a Vaccine Vector for 20 Years: A Focus on Maternally Derived Antibody Interference. Vaccines 2020, 8, 222. [Google Scholar] [CrossRef]
- Nakaya, T.; Cros, J.; Park, M.-S.; Nakaya, Y.; Zheng, H.; Sagrera, A.; Villar, E.; García-Sastre, A.; Palese, P. Recombinant Newcastle disease virus as a vaccine vector. J. Virol. 2001, 75, 11868–11873. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Sobrido, L.; Gitiban, N.; Fernandez-Sesma, A.; Cros, J.; Mertz, S.E.; Jewell, N.A.; Hammond, S.; Flano, E.; Durbin, R.K.; García-Sastre, A.; et al. Protection against Respiratory Syncytial Virus by a Recombinant Newcastle Disease Virus Vector. J. Virol. 2006, 80, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Carnero, E.; Li, W.; Borderia, A.V.; Moltedo, B.; Moran, T.; García-Sastre, A. Optimization of Human Immunodeficiency Virus Gag Expression by Newcastle Disease Virus Vectors for the Induction of Potent Immune Responses. J. Virol. 2009, 83, 584–597. [Google Scholar] [CrossRef] [PubMed]
- Maamary, J.; Array, F.; Gao, Q.; García-Sastre, A.; Steinman, R.M.; Palese, P.; Nchinda, G. Newcastle Disease Virus Expressing a Dendritic Cell-Targeted HIV Gag Protein Induces a Potent Gag-Specific Immune Response in Mice. J. Virol. 2011, 85, 2235–2246. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xiao, S.; Kumar, M.; Yang, X.; Akkoyunlu, M.; Collins, P.L.; Samal, S.K.; Pal, U. A host-restricted viral vector for antigen-specific immunization against Lyme disease pathogen. Vaccine 2011, 29, 5294–5303. [Google Scholar] [CrossRef] [PubMed]
- Khattar, S.K.; Samal, S.; DeVico, A.L.; Collins, P.L.; Samal, S.K. Newcastle Disease Virus Expressing Human Immunodeficiency Virus Type 1 Envelope Glycoprotein Induces Strong Mucosal and Serum Antibody Responses in Guinea Pigs. J. Virol. 2011, 85, 10529–10541. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.; Wen, Z.; Su, H.; Ge, J.; Chen, W.; Wang, X.; Wu, C.; Yang, C.; Chen, H.; Bu, Z. Newcastle disease virus-vectored Nipah encephalitis vaccines induce B and T cell responses in mice and long-lasting neutralizing antibodies in pigs. Virology 2012, 432, 327–335. [Google Scholar] [CrossRef]
- Kim, S.-H.; Chen, S.; Jiang, X.; Green, K.Y.; Samal, S.K.; López, S. Newcastle Disease Virus Vector Producing Human Norovirus-Like Particles Induces Serum, Cellular, and Mucosal Immune Responses in Mice. J. Virol. 2014, 88, 9718–9727. [Google Scholar] [CrossRef]
- Khattar, S.K.; DeVico, A.L.; LaBranche, C.C.; Panda, A.; Montefiori, D.C.; Samal, S.K.; Silvestri, G. Enhanced Immune Responses to HIV-1 Envelope Elicited by a Vaccine Regimen Consisting of Priming with Newcastle Disease Virus Expressing HIV gp160 and Boosting with gp120 and SOSIP gp140 Proteins. J. Virol. 2016, 90, 1682–1686. [Google Scholar] [CrossRef]
- Nath, B.; Vandna; Saini, H.M.; Prasad, M.; Kumar, S. Evaluation of Japanese encephalitis virus E and NS1 proteins immunogenicity using a recombinant Newcastle disease virus in mice. Vaccine 2020, 38, 1860–1868. [Google Scholar] [CrossRef]
- Sun, W.; McCroskery, S.; Liu, W.-C.; Leist, S.R.; Liu, Y.; Albrecht, R.A.; Slamanig, S.; Oliva, J.; Amanat, F.; Schäfer, A.; et al. A Newcastle Disease Virus (NDV) Expressing a Membrane-Anchored Spike as a Cost-Effective Inactivated SARS-CoV-2 Vaccine. Vaccines 2020, 8, 771. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Liu, Y.; Amanat, F.; González-Domínguez, I.; McCroskery, S.; Slamanig, S.; Coughlan, L.; Rosado, V.; Lemus, N.; Jangra, S.; et al. A Newcastle disease virus expressing a stabilized spike protein of SARS-CoV-2 induces protective immune responses. Nat. Commun. 2021, 12, 6197. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhang, P.; Bai, S.; Lv, M.; Wang, J.; Chen, W.; Yu, Q.; Wu, J. Heterologous prime-boost regimens with HAdV-5 and NDV vectors elicit stronger immune responses to Ebola virus than homologous regimens in mice. Arch. Virol. 2021, 166, 3333–3341. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.-K.; An, Y.H.; Jang, J.-J.; Jeon, J.H.; Jang, S.H.; Jang, H. The human ACE-2 receptor binding domain of SARS-CoV-2 express on the viral surface of the Newcastle disease virus as a non-replicating viral vector vaccine candidate. PLoS ONE 2022, 17, e0263684. [Google Scholar] [CrossRef]
- Ponce-de-León, S.; Torres, M.; Soto-Ramírez, L.E.; José Calva, J.; Santillán-Doherty, P.; Carranza-Salazar, D.E.; Carreño, J.M.; Carranza, C.; Juárez, E.; Carreto-Binaghi, L.E.; et al. Safety and immunogenicity of a live recombinant Newcastle disease virus-based COVID-19 vaccine (Patria) administered via the intramuscular or intranasal route: Interim results of a non-randomized open label phase I trial in Mexico. medRxiv 2022, preprint. [Google Scholar] [CrossRef]
- Pitisuttithum, P.; Luvira, V.; Lawpoolsri, S.; Muangnoicharoen, S.; Kamolratanakul, S.; Sivakorn, C.; Narakorn, P.; Surichan, S.; Prangpratanporn, S.; Puksuriwong, S.; et al. Safety and immunogenicity of an inactivated recombinant Newcastle disease virus vaccine expressing SARS-CoV-2 spike: Interim results of a randomised, placebo-controlled, phase 1 trial. eClinicalMedicine 2022, 45, 101323. [Google Scholar] [CrossRef]
- Kim, S.-H.; Samal, S.K. Innovation in Newcastle Disease Virus Vectored Avian Influenza Vaccines. Viruses 2019, 11, 300. [Google Scholar] [CrossRef]
- Veits, J.; Wiesner, D.; Fuchs, W.; Hoffmann, B.; Granzow, H.; Starick, E.; Mundt, E.; Schirrmeier, H.; Mebatsion, T.; Mettenleiter, T.C.; et al. Newcastle disease virus expressing H5 hemagglutinin gene protects chickens against Newcastle disease and avian influenza. Proc. Natl. Acad. Sci. USA 2006, 103, 8197–8202. [Google Scholar] [CrossRef]
- Ge, J.; Deng, G.; Wen, Z.; Tian, G.; Wang, Y.; Shi, J.; Wang, X.; Li, Y.; Hu, S.; Jiang, Y.; et al. Newcastle Disease Virus-Based Live Attenuated Vaccine Completely Protects Chickens and Mice from Lethal Challenge of Homologous and Heterologous H5N1 Avian Influenza Viruses. J. Virol. 2007, 81, 150–158. [Google Scholar] [CrossRef]
- Nayak, B.; Rout, S.N.; Kumar, S.; Khalil, M.S.; Fouda, M.M.; Ahmed, L.E.; Earhart, K.C.; Perez, D.R.; Collins, P.L.; Samal, S.K. Immunization of chickens with Newcastle disease virus expressing H5 hemagglutinin protects against highly pathogenic H5N1 avian influenza viruses. PLoS ONE 2009, 4, e6509. [Google Scholar] [CrossRef]
- Saikia, D.P.; Yadav, K.; Pathak, D.C.; Ramamurthy, N.; D’Silva, A.L.; Marriappan, A.K.; Ramakrishnan, S.; Vakharia, V.N.; Chellappa, M.M.; Dey, S. Recombinant Newcastle Disease Virus (NDV) Expressing Sigma C Protein of Avian Reovirus (ARV) Protects against Both ARV and NDV in Chickens. Pathogens 2019, 8, 145. [Google Scholar] [CrossRef] [PubMed]
- Kanabagatte Basavarajappa, M.; Kumar, S.; Khattar, S.K.; Gebreluul, G.T.; Paldurai, A.; Samal, S.K. A recombinant Newcastle disease virus (NDV) expressing infectious laryngotracheitis virus (ILTV) surface glycoprotein D protects against highly virulent ILTV and NDV challenges in chickens. Vaccine 2014, 32, 3555–3563. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Spatz, S.; Zhang, Z.; Wen, G.; Garcia, M.; Zsak, L.; Yu, Q.; Sandri-Goldin, R.M. Newcastle Disease Virus (NDV) Recombinants Expressing Infectious Laryngotracheitis Virus (ILTV) Glycoproteins gB and gD Protect Chickens against ILTV and NDV Challenges. J. Virol. 2014, 88, 8397–8406. [Google Scholar] [CrossRef] [PubMed]
- Tian, K.-Y.; Guo, H.-F.; Li, N.; Zhang, Y.-H.; Wang, Z.; Wang, B.; Yang, X.; Li, Y.-T.; Zhao, J. Protection of chickens against hepatitis-hydropericardium syndrome and Newcastle disease with a recombinant Newcastle disease virus vaccine expressing the fowl adenovirus serotype 4 fiber-2 protein. Vaccine 2020, 38, 1989–1997. [Google Scholar] [CrossRef]
- Sun, M.; Dong, J.; Li, L.; Lin, Q.; Sun, J.; Liu, Z.; Shen, H.; Zhang, J.; Ren, T.; Zhang, C. Recombinant Newcastle disease virus (NDV) expressing Duck Tembusu virus (DTMUV) pre-membrane and envelope proteins protects ducks against DTMUV and NDV challenge. Vet. Microbiol. 2018, 218, 60–69. [Google Scholar] [CrossRef]
- Ferreira, H.L.; Pirlot, J.F.; Reynard, F.; van den Berg, T.; Bublot, M.; Lambrecht, B. Immune Responses and Protection Against H5N1 Highly Pathogenic Avian Influenza Virus Induced by the Newcastle Disease Virus H5 Vaccine in Ducks. Avian Dis. 2012, 56, 940–948. [Google Scholar] [CrossRef]
- Wang, J.; Cong, Y.; Yin, R.; Feng, N.; Yang, S.; Xia, X.; Xiao, Y.; Wang, W.; Liu, X.; Hu, S.; et al. Generation and evaluation of a recombinant genotype VII Newcastle disease virus expressing VP3 protein of Goose parvovirus as a bivalent vaccine in goslings. Virus Res. 2015, 203, 77–83. [Google Scholar] [CrossRef]
- Xu, D.; Li, C.; Liu, G.; Chen, Z.; Jia, R. Generation and evaluation of a recombinant goose origin Newcastle disease virus expressing Cap protein of goose origin avastrovirus as a bivalent vaccine in goslings. Poult. Sci. 2019, 98, 4426–4432. [Google Scholar] [CrossRef]
- Ge, J.; Wang, X.; Tian, M.; Gao, Y.; Wen, Z.; Yu, G.; Zhou, W.; Zu, S.; Bu, Z. Recombinant Newcastle disease viral vector expressing hemagglutinin or fusion of canine distemper virus is safe and immunogenic in minks. Vaccine 2015, 33, 2457–2462. [Google Scholar] [CrossRef]
- Olbert, M.; Römer-Oberdörfer, A.; Herden, C.; Malberg, S.; Runge, S.; Staeheli, P.; Rubbenstroth, D. Viral vector vaccines expressing nucleoprotein and phosphoprotein genes of avian bornaviruses ameliorate homologous challenge infections in cockatiels and common canaries. Sci. Rep. 2016, 6, 36840. [Google Scholar] [CrossRef]
- Xu, L.; Qin, Z.; Qiao, L.; Wen, J.; Shao, H.; Wen, G.; Pan, Z. Characterization of thermostable Newcastle disease virus recombinants expressing the hemagglutinin of H5N1 avian influenza virus as bivalent vaccine candidates. Vaccine 2020, 38, 1690–1699. [Google Scholar] [CrossRef] [PubMed]
- Steglich, C.; Grund, C.; Ramp, K.; Breithaupt, A.; Höper, D.; Keil, G.; Veits, J.; Ziller, M.; Granzow, H.; Mettenleiter, T.C. Chimeric newcastle disease virus protects chickens against avian influenza in the presence of maternally derived NDV immunity. PLoS ONE 2013, 8, e72530. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Paldurai, A.; Samal, S.K. A novel chimeric Newcastle disease virus vectored vaccine against highly pathogenic avian influenza virus. Virology 2017, 503, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xue, L.; Hu, S.; Cheng, H.; Deng, Y.; Hu, Z.; Wang, X.; Liu, X. Chimeric Newcastle disease virus-vectored vaccine protects chickens against H9N2 avian influenza virus in the presence of pre-existing NDV immunity. Arch. Virol. 2018, 163, 3365–3371. [Google Scholar] [CrossRef] [PubMed]
- Yadav, K.; Pathak, D.C.; Saikia, D.P.; Debnath, A.; Ramakrishnan, S.; Dey, S.; Chellappa, M.M. Generation and evaluation of a recombinant Newcastle disease virus strain R2B with an altered fusion protein cleavage site as a vaccine candidate. Microb. Pathog. 2018, 118, 230–237. [Google Scholar] [CrossRef]
- Arifin, M.A.; Mel, M.; Abdul Karim, M.I.; Ideris, A. Production of Newcastle Disease Virus by Vero Cells Grown on Cytodex 1 Microcarriers in a 2-Litre Stirred Tank Bioreactor. J. Biomed. Biotechnol. 2010, 2010, 586363. [Google Scholar] [CrossRef]
- Jaafar, J.N. Investigation of the Effectiveness of Newcastle Disease Virus Production in Different Bioreactors; International Islamic University Malaysia: Gombak, Malaysia, 2009. [Google Scholar]
- Arifin, M.A. Optimization of Cell Culture Conditions for the Production of Newcastle Disease Virus; International Islamic University Malaysia: Kuala Lumpur, Malaysia, 2011. [Google Scholar]
- Al-Ziaydi, A.G.; Al-Shammari, A.M.; Hamzah, M.I. Propagation of oncolytic Newcastle Disease Virus in Embryonated Chicken Eggs and its Research Applications in Cell lines. In Proceedings of the 1st International Virtual Conference on Pure Science, Qadisiyah, Iraq, 10–11 June 2020; College of Science, University of Al-Qadisiyah: Al-Qadisiyah, Iraq, 2020; Volume 1664, p. 012129. [Google Scholar]
- Chen, L.-M.; Donis, R.O.; Suarez, D.L.; Wentworth, D.E.; Webby, R.; Engelhardt, O.G.; Swayne, D.E. Biosafety risk assessment for production of candidate vaccine viruses to protect humans from zoonotic highly pathogenic avian influenza viruses. Influenza Other Respir. Viruses 2020, 14, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Harrison, S.T.L.; Tai, S.L. Advances in Bioreactor Systems for the Production of Biologicals in Mammalian Cells. ChemBioEng Rev. 2022, 9, 42–62. [Google Scholar] [CrossRef]
- Dey, S.; Chellappa, M.M.; Pathak, D.C.; Gaikwad, S.; Yadav, K.; Ramakrishnan, S.; Vakharia, V.N. Newcastle Disease Virus Vectored Bivalent Vaccine against Virulent Infectious Bursal Disease and Newcastle Disease of Chickens. Vaccines 2017, 5, 31. [Google Scholar] [CrossRef]
- Le Ru, A.; Jacob, D.; Transfiguracion, J.; Ansorge, S.; Henry, O.; Kamen, A.A. Scalable production of influenza virus in HEK-293 cells for efficient vaccine manufacturing. Vaccine 2010, 28, 3661–3671. [Google Scholar] [CrossRef]
- Kiesslich, S.; Kamen, A.A. Vero cell upstream bioprocess development for the production of viral vectors and vaccines. Biotechnol. Adv. 2020, 44, 107608. [Google Scholar] [CrossRef] [PubMed]
- Ge, J.; Wang, X.; Tao, L.; Wen, Z.; Feng, N.; Yang, S.; Xia, X.; Yang, C.; Chen, H.; Bu, Z. Newcastle Disease Virus-Vectored Rabies Vaccine Is Safe, Highly Immunogenic, and Provides Long-Lasting Protection in Dogs and Cats. J. Virol. 2011, 85, 8241–8252. [Google Scholar] [CrossRef] [PubMed]
- Debnath, A.; Pathak, D.C.; D’silva, A.L.; Batheja, R.; Ramamurthy, N.; Vakharia, V.N.; Chellappa, M.M.; Dey, S. Newcastle disease virus vectored rabies vaccine induces strong humoral and cell mediated immune responses in mice. Vet. Microbiol. 2020, 251, 108890. [Google Scholar] [CrossRef] [PubMed]
- Kiesslich, S.; Vila-Chã Losa, J.P.; Gélinas, J.-F.; Kamen, A.A. Serum-free production of rVSV-ZEBOV in Vero cells: Microcarrier bioreactor versus scale-X™ hydro fixed-bed. J. Biotechnol. 2020, 310, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.F.; Guilbault, C.; Li, X.; Elahi, S.M.; Ansorge, S.; Kamen, A.; Gilbert, R. Development of suspension adapted Vero cell culture process technology for production of viral vaccines. Vaccine 2019, 37, 6996–7002. [Google Scholar] [CrossRef]
- Segura, M.M.; Kamen, A.A.; Garnier, A. Overview of current scalable methods for purification of viral vectors. Viral Vectors Gene Ther. 2011, 737, 89–116. [Google Scholar]
- Moreira, A.S.; Cavaco, D.G.; Faria, T.Q.; Alves, P.M.; Carrondo, M.J.T.; Peixoto, C. Advances in Lentivirus Purification. Biotechnol. J. 2021, 16, 2000019. [Google Scholar] [CrossRef]
- Fakri, F.Z.; Bamouh, Z.; Elmejdoub, S.; Elkarhat, Z.; Tadlaoui, K.; Chen, W.; Bu, Z.; Elharrak, M. Long term immunity against Peste Des Petits Ruminants mediated by a recombinant Newcastle disease virus vaccine. Vet. Microbiol. 2021, 261, 109201. [Google Scholar] [CrossRef]
- Swayne, D.E.; Suarez, D.L.; Schultz-Cherry, S.; Tumpey, T.M.; King, D.J.; Nakaya, T.; Palese, P.; Garcia-Sastre, A. Recombinant Paramyxovirus Type 1-Avian Influenza-H7 Virus as a Vaccine for Protection of Chickens Against Influenza and Newcastle Disease. Avian Dis. 2003, 47, 1047–1050. [Google Scholar] [CrossRef]
- Nakaya, Y.; Nakaya, T.; Park, M.-S.; Cros, J.; Imanishi, J.; Palese, P.; García-Sastre, A. Induction of Cellular Immune Responses to Simian Immunodeficiency Virus Gag by Two Recombinant Negative-Strand RNA Virus Vectors. J. Virol. 2004, 78, 9366–9375. [Google Scholar] [CrossRef]
- Huang, Z.; Elankumaran, S.; Yunus, A.S.; Samal, S.K. A Recombinant Newcastle Disease Virus (NDV) Expressing VP2 Protein of Infectious Bursal Disease Virus (IBDV) Protects against NDV and IBDV. J. Virol. 2004, 78, 10054–10063. [Google Scholar] [CrossRef] [PubMed]
- Schröer, D.; Veits, J.; Grund, C.; Dauber, M.; Keil, G.; Granzow, H.; Mettenleiter, T.C.; Römer-Oberdörfer, A. Vaccination with Newcastle Disease Virus Vectored Vaccine Protects Chickens Against Highly Pathogenic H7 Avian Influenza Virus. Avian Dis. 2009, 53, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Sarfati-Mizrahi, D.; Lozano-Dubernard, B.; Soto-Priante, E.; Castro-Peralta, F.; Flores-Castro, R.; Loza-Rubio, E.; Gay-Gutiérrez, M. Protective Dose of a Recombinant Newcastle Disease LaSota–Avian Influenza Virus H5 Vaccine Against H5N2 Highly Pathogenic Avian Influenza Virus and Velogenic Viscerotropic Newcastle Disease Virus in Broilers with High Maternal Antibody Levels. Avian Dis. 2010, 54, 239–241. [Google Scholar] [CrossRef] [PubMed]
- Kortekaas, J.; Dekker, A.; de Boer, S.M.; Weerdmeester, K.; Vloet, R.P.M.; Wit, A.A.C.d.; Peeters, B.P.H.; Moormann, R.J.M. Intramuscular inoculation of calves with an experimental Newcastle disease virus-based vector vaccine elicits neutralizing antibodies against Rift Valley fever virus. Vaccine 2010, 28, 2271–2276. [Google Scholar] [CrossRef] [PubMed]
- Khattar, S.K.; Collins, P.L.; Samal, S.K. Immunization of cattle with recombinant Newcastle disease virus expressing bovine herpesvirus-1 (BHV-1) glycoprotein D induces mucosal and serum antibody responses and provides partial protection against BHV-1. Vaccine 2010, 28, 3159–3170. [Google Scholar] [CrossRef] [PubMed]
- Schröer, D.; Veits, J.; Keil, G.; Römer-Oberdörfer, A.; Weber, S.; Mettenleiter, T.C. Efficacy of Newcastle Disease Virus Recombinant Expressing Avian Influenza Virus H6 Hemagglutinin Against Newcastle Disease and Low Pathogenic Avian Influenza in Chickens and Turkeys. Avian Dis. 2011, 55, 201–211. [Google Scholar] [CrossRef]
- Hu, H.; Roth, J.P.; Estevez, C.N.; Zsak, L.; Liu, B.; Yu, Q. Generation and evaluation of a recombinant Newcastle disease virus expressing the glycoprotein (G) of avian metapneumovirus subgroup C as a bivalent vaccine in turkeys. Vaccine 2011, 29, 8624–8633. [Google Scholar] [CrossRef]
- Goff, P.H.; Krammer, F.; Hai, R.; Seibert, C.W.; Margine, I.; García-Sastre, A.; Palese, P. Induction of Cross-Reactive Antibodies to Novel H7N9 Influenza Virus by Recombinant Newcastle Disease Virus Expressing a North American Lineage H7 Subtype Hemagglutinin. J. Virol. 2013, 87, 8235–8240. [Google Scholar] [CrossRef]
- Toro, H.; Zhao, W.; Breedlove, C.; Zhang, Z.; van Santen, V.; Yu, Q. Infectious Bronchitis Virus S2 Expressed from Recombinant Virus Confers Broad Protection Against Challenge. Avian Dis. 2013, 58, 83–89. [Google Scholar] [CrossRef]
- Ge, J.; Wang, X.; Tian, M.; Wen, Z.; Feng, Q.; Qi, X.; Gao, H.; Wang, X.; Bu, Z. Novel in-ovo chimeric recombinant Newcastle disease vaccine protects against both Newcastle disease and infectious bursal disease. Vaccine 2014, 32, 1514–1521. [Google Scholar] [CrossRef]
- Liu, Q.; Mena, I.; Ma, J.; Bawa, B.; Krammer, F.; Lyoo, Y.S.; Lang, Y.; Morozov, I.; Mahardika, G.N.; Ma, W.; et al. Newcastle Disease Virus-Vectored H7 and H5 Live Vaccines Protect Chickens from Challenge with H7N9 or H5N1 Avian Influenza Viruses. J. Virol. 2015, 89, 7401–7408. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Ge, J.; Li, X.; Chen, W.; Wang, X.; Wen, Z.; Bu, Z. Protective efficacy of a recombinant Newcastle disease virus expressing glycoprotein of vesicular stomatitis virus in mice. Virol. J. 2016, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Nagy, A.; Lee, J.; Mena, I.; Henningson, J.; Li, Y.; Ma, J.; Duff, M.; Li, Y.; Lang, Y.; Yang, J.; et al. Recombinant Newcastle disease virus expressing H9 HA protects chickens against heterologous avian influenza H9N2 virus challenge. Vaccine 2016, 34, 2537–2545. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yang, J.; Ge, J.; Hua, R.; Liu, R.; Li, X.; Wang, X.; Shao, Y.; Sun, E.; Wu, D.; et al. Newcastle disease virus-vectored West Nile fever vaccine is immunogenic in mammals and poultry. Virol. J. 2016, 13, 109. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Ge, J.; Wen, Z.; Chen, W.; Wang, X.; Liu, R.; Bu, Z. Characterization of a recombinant Newcastle disease virus expressing the glycoprotein of bovine ephemeral fever virus. Arch. Virol. 2017, 162, 359–367. [Google Scholar] [CrossRef]
- Zhao, R.; Sun, J.; Qi, T.; Zhao, W.; Han, Z.; Yang, X.; Liu, S. Recombinant Newcastle disease virus expressing the infectious bronchitis virus S1 gene protects chickens against Newcastle disease virus and infectious bronchitis virus challenge. Vaccine 2017, 35, 2435–2442. [Google Scholar] [CrossRef]
- Liu, R.-q.; Ge, J.-y.; Wang, J.-l.; Shao, Y.; Zhang, H.-l.; Wang, J.-l.; Wen, Z.-y.; Bu, Z.-g. Newcastle disease virus-based MERS-CoV candidate vaccine elicits high-level and lasting neutralizing antibodies in Bactrian camels. J. Integr. Agric. 2017, 16, 2264–2273. [Google Scholar] [CrossRef]
- Ma, J.; Lee, J.; Liu, H.; Mena, I.; Davis, A.S.; Sunwoo, S.Y.; Lang, Y.; Duff, M.; Morozov, I.; Li, Y.; et al. Newcastle disease virus-based H5 influenza vaccine protects chickens from lethal challenge with a highly pathogenic H5N2 avian influenza virus. npj Vaccines 2017, 2, 33. [Google Scholar] [CrossRef]
- Hu, Z.; Liu, X.; Jiao, X.; Liu, X. Newcastle disease virus (NDV) recombinant expressing the hemagglutinin of H7N9 avian influenza virus protects chickens against NDV and highly pathogenic avian influenza A (H7N9) virus challenges. Vaccine 2017, 35, 6585–6590. [Google Scholar] [CrossRef]
- Shi, L.; Hu, Z.; Hu, J.; Liu, D.; He, L.; Liu, J.; Gu, H.; Gan, J.; Wang, X.; Liu, X. Single Immunization with Newcastle Disease Virus-Vectored H7N9 Vaccine Confers a Complete Protection against Challenge with Highly Pathogenic Avian Influenza H7N9 Virus. Avian Dis. 2018, 63, 61–67. [Google Scholar] [CrossRef]
- Xu, X.; Xue, C.; Liu, X.; Li, J.; Fei, Y.; Liu, Z.; Mu, J.; Bi, Y.; Qian, J.; Yin, R.; et al. A novel recombinant attenuated Newcastle disease virus expressing H9 subtype hemagglutinin protected chickens from challenge by genotype VII virulent Newcastle disease virus and H9N2 avian influenza virus. Vet. Microbiol. 2019, 228, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Abozeid, H.H.; Paldurai, A.; Varghese, B.P.; Khattar, S.K.; Afifi, M.A.; Zouelfakkar, S.; El-Deeb, A.H.; El-Kady, M.F.; Samal, S.K. Development of a recombinant Newcastle disease virus-vectored vaccine for infectious bronchitis virus variant strains circulating in Egypt. Vet. Res. 2019, 50, 12. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Kumar, V.; Kekungu, P.; Barman, N.N.; Kumar, S. Evaluation of surface glycoproteins of classical swine fever virus as immunogens and reagents for serological diagnosis of infections in pigs: A recombinant Newcastle disease virus approach. Arch. Virol. 2019, 164, 3007–3017. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.; Wen, G.; Qiu, X.; Yuan, Y.; Meng, C.; Sun, Y.; Liao, Y.; Song, C.; Liu, W.; Shi, Y.; et al. A Recombinant La Sota Vaccine Strain Expressing Multiple Epitopes of Infectious Bronchitis Virus (IBV) Protects Specific Pathogen-Free (SPF) Chickens against IBV and NDV Challenges. Vaccines 2019, 7, 170. [Google Scholar] [CrossRef] [PubMed]
- Murr, M.; Hoffmann, B.; Grund, C.; Römer-Oberdörfer, A.; Mettenleiter, T.C. A Novel Recombinant Newcastle Disease Virus Vectored DIVA Vaccine against Peste des Petits Ruminants in Goats. Vaccines 2020, 8, 205. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Tu, K.; Teng, Q.; Feng, D.; Zhao, Y.; Zhang, G.; Gallagher, T. Identification of Novel T-Cell Epitopes on Infectious Bronchitis Virus N Protein and Development of a Multi-epitope Vaccine. J. Virol. 2021, 95, e00667-21. [Google Scholar] [CrossRef]
- Lee, J.; Kim, D.-H.; Noh, J.; Youk, S.; Jeong, J.-H.; Lee, J.-B.; Park, S.-Y.; Choi, I.-S.; Lee, S.-W.; Song, C.-S. Live Recombinant NDV-Vectored H5 Vaccine Protects Chickens and Domestic Ducks from Lethal Infection of the Highly Pathogenic H5N6 Avian Influenza Virus. Front. Vet. Sci. 2022, 8, 773715. [Google Scholar] [CrossRef]
| Vaccine Type | Pathogen | Disease | Antigen | Animal Model | Production Platform * | Route * | Dose * | Reference |
|---|---|---|---|---|---|---|---|---|
| Live B1 strain | Influenza A H1N1 | Respiratory infection | HA | Mouse | ECEs | iv, ip | two doses; 3 × 107 PFU | [65] |
| Live LaSota or BC strain | HPIV3 | Respiratory infection | HN | African green monkey; rhesus monkey | ECEs, DF-1 cell line | in + it | two doses; 3 × 106 PFU | [20] |
| Live B1 strain | HRSV | Respiratory infection | F | Mouse | ECEs | in | one dose; 5 × 105 PFU | [66] |
| Live BC or LaSota/VF strain | SARS-CoV | Respiratory infection | S, S1 | African green monkey | ECEs, DF-1 cell line | in + it | one or two doses; 2 × 107 PFU | [28] |
| Live LaSota strain | HPAIV H5N1 | Respiratory infection | HA | African green monkey | DF-1 cell line | in | two doses; 2 × 107 PFU | [40] |
| Live B1 strain | HIV | AIDS | Gag | Mouse | ECEs, Vero cell line | in | two doses; 5 × 105 PFU prime and 106 PFU boost | [67] |
| Live LaSota or BC strain | EBOV | Ebola virus disease (hemorrhagic fever) | GP | Rhesus monkey | DF-1 cell line | in + it | two doses; 107 PFU | [29] |
| Live LaSota strain | HIV | AIDS | Gag | Mouse | ECEs | in | two doses; 5 × 105 PFU prime and 106 PFU boost | [68] |
| Live LaSota/VF strain | Borrelia burgdorferi | Lyme | BmpA, OspC | Hamster | ECEs | in, im, ip | one or two doses; 106 PFU | [69] |
| Live LaSota strain | HIV | AIDS | Env (gp160) | Guinea pig | ECEs | in, im, in + im | two or three doses; 3 × 105 PFU (in) or 5 × 105 PFU (im) | [70] |
| Live LaSota strain | NiV | Encephalitis | F, G | Mouse, pig | ECEs | im | two doses; 108 EID50 (mice) or 2 × 109 EID50 (pigs) | [71] |
| Live LaSota or Lasota/BC strain | NoV | Gastroenteritis | VP1 | Mouse | ECEs | in | one dose; 106 EID50 | [72] |
| Live LaSota strain | HIV | AIDS | Env (gp160)/Gag (p55) | Guinea pig, mouse | ECEs | in | two doses; 2 × 105 PFU (guinea pigs) or 4 × 104 PFU (mice) | [50] |
| Live LaSota strain | HIV | AIDS | Env (gp160) | Guinea pig | ECEs | in | four doses of 2 × 105 PFU or two doses of 2 × 105 PFU followed by two doses of recombinant protein (gp120 or gp140) | [73] |
| Live LaSota strain | Poliovirus | Poliomyelitis | P1/3CD | Guinea pig | ECEs | in | two doses; 105 PFU | [49] |
| Live chimeric NDV strain | EBOV | Ebola virus disease (hemorrhagic fever) | GP | Guinea pig | ECEs | in | two doses; 2 × 106 TCID50 | [13] |
| Live LaSota strain | JEV | Encephalitis | E, NS1 | Mouse | ECEs | in | one dose; 106 EID50 | [74] |
| Live LaSota strain | SARS-CoV-2 | COVID-19 | S, S-F chimera | Mouse | ECEs | in | two doses; 10 or 50 μg | [18] |
| Inactivated LaSota strain | SARS-CoV-2 | COVID-19 | S, S-F chimera | Mouse, hamster | ECEs | im | two doses; 5 or 10 μg | [75] |
| Live B1 strain | SARS-CoV-2 | COVID-19 | S | Mouse, hamster | ECEs | in | one or two doses; 104 PFU (mice) or 106 PFU (hamster) | [26] |
| Live or inactivated LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | Pig | ECEs | in, im, in + im | two doses of 107, 3 × 107, 108 or 3 × 108 EID50 (live); two doses of 108 EID50 (inactivated) | [31] |
| Live or inactivated LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | Hamster, mouse | ECEs | in, im, in + im | two doses of 1.0, 0.3, 0.1, 0.03 or 0.03 μg (im, inactivated, hamsters); two doses of 106 EID50 (in, live, hamsters); two doses of 104, 105 or 106 EID50 (in prime and im boost, live, mice); two doses of 1 μg (im, inactivated, mice) | [76] |
| Live LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | Rat | ECEs | in, im, in + im | two doses; 7.4 × 108 EID50 | [30] |
| Live LaSota strain | SARS-CoV-2 | COVID-19 | S, truncated S | Hamster | ECEs | in | one or two doses; 107 PFU | [27] |
| Live LaSota strain | EBOV | Ebola virus disease (hemorrhagic fever) | GP | Mouse | ECEs | in | two doses of 106 PFU; one dose of 106 PFU and one dose of adenovirus-vectored vaccine | [77] |
| Inactivated VG/GA strain | SARS-CoV-2 | COVID-19 | RBD | Mouse | ECEs | im | two doses of 1, 5 or 10 μg | [78] |
| Responsible Group | Vaccine Type | Pathogen | Disease | Antigen | Phase | Route * | Dose * | Reference |
|---|---|---|---|---|---|---|---|---|
| Icahn School of Medicine at Mount Sinai, USA | Live LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | I | in, im, in + im | 3.3 × 108 EID50 1 × 109 EID50 | NCT05181709 |
| Laboratorio Avi-Mex, Mexico | Live LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | I/II | im, in + im | 108 EID50 | NCT04871737 [79] NCT05205746 |
| Institute of Vaccines and Medical Biologicals, Vietnam | Inactivated LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | I/II | im | 1, 3 or 10 μg | NCT04830800 |
| Butantan Institute, Brazil | Inactivated LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | I/II | im | 1, 3 or 10 μg | NCT04993209 |
| Mahidol University, Thailand | Inactivated LaSota strain | SARS-CoV-2 | COVID-19 | HXP-S | I/II | im | 1, 3 or 10 μg | NCT04764422 [80] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fulber, J.P.C.; Kamen, A.A. Development and Scalable Production of Newcastle Disease Virus-Vectored Vaccines for Human and Veterinary Use. Viruses 2022, 14, 975. https://doi.org/10.3390/v14050975
Fulber JPC, Kamen AA. Development and Scalable Production of Newcastle Disease Virus-Vectored Vaccines for Human and Veterinary Use. Viruses. 2022; 14(5):975. https://doi.org/10.3390/v14050975
Chicago/Turabian StyleFulber, Julia P. C., and Amine A. Kamen. 2022. "Development and Scalable Production of Newcastle Disease Virus-Vectored Vaccines for Human and Veterinary Use" Viruses 14, no. 5: 975. https://doi.org/10.3390/v14050975
APA StyleFulber, J. P. C., & Kamen, A. A. (2022). Development and Scalable Production of Newcastle Disease Virus-Vectored Vaccines for Human and Veterinary Use. Viruses, 14(5), 975. https://doi.org/10.3390/v14050975







