Vaccine Mismatches, Viral Circulation, and Clinical Severity Patterns of Influenza B Victoria and Yamagata Infections in Brazil over the Decade 2010–2020: A Statistical and Phylogeny–Trait Analyses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population
2.2. Influenza B Molecular Detection, Lineage Determination and Sequencing
2.3. Phylogenetic Analyses
2.4. Statistical Analyses
2.5. Ethical Statement
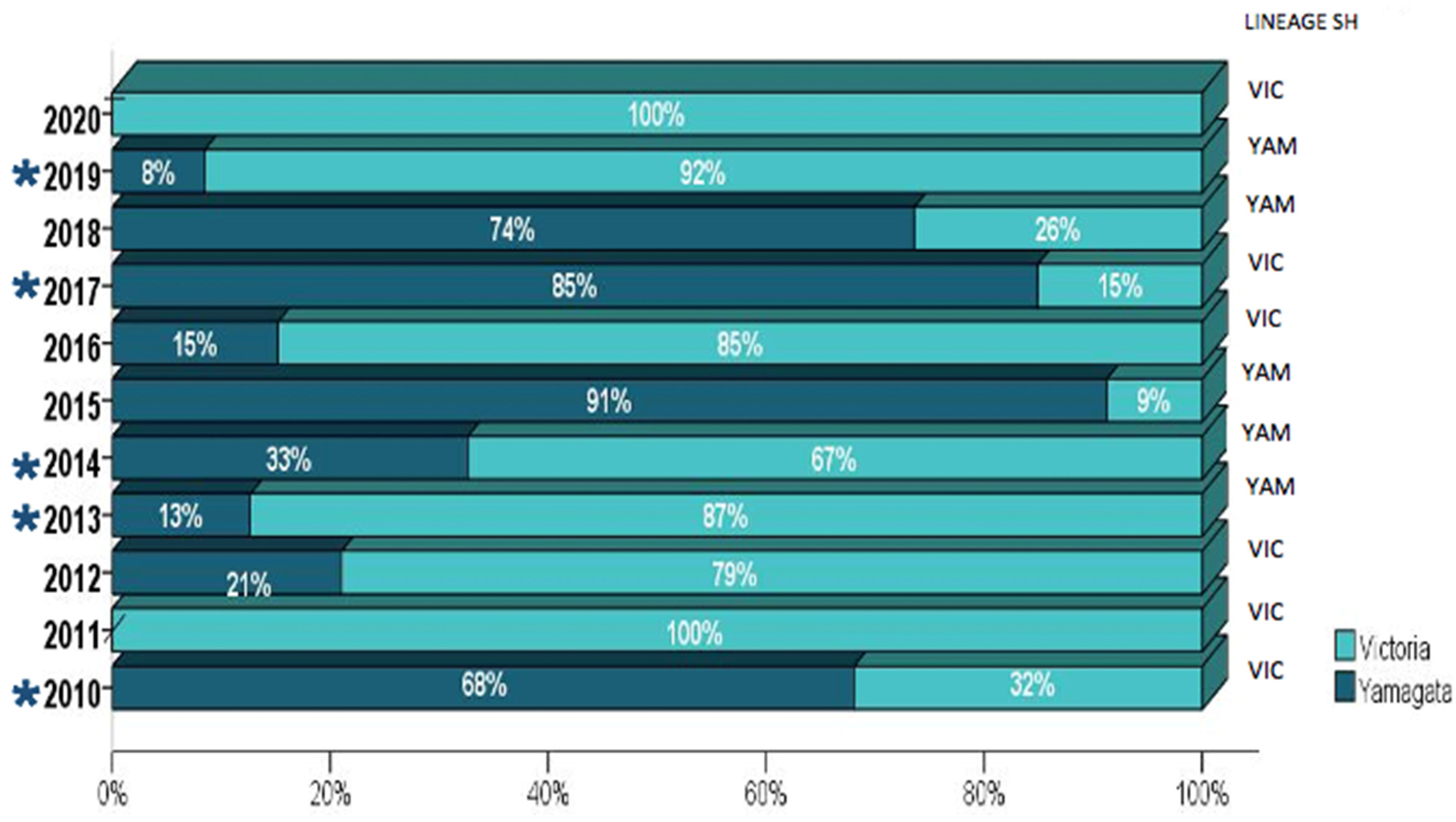
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Keech, M.; Beardsworth, P. The Impact of Influenza on Working Days Lost: A Review of the Literature. Pharmacoeconomics 2008, 26, 911–924. [Google Scholar] [CrossRef] [PubMed]
- Nair, H.; Brooks, W.A.; Katz, M.; Roca, A.; Berkley, J.A.; Madhi, S.A.; Simmerman, J.M.; Gordon, A.; Sato, M.; Howie, S.; et al. Global Burden of Respiratory Infections Due to Seasonal Influenza in Young Children: A Systematic Review and Meta-Analysis. Lancet 2011, 378, 1917–1930. [Google Scholar] [CrossRef] [Green Version]
- Irving, S.A.; Patel, D.C.; Kieke, B.A.; Donahue, J.G.; Vandermause, M.F.; Shay, D.K.; Belongia, E.A. Comparison of Clinical Features and Outcomes of Medically Attended Influenza A and Influenza B in a Defined Population over Four Seasons: 2004–2005 through 2007–2008. Influenza Other Respir Viruses 2012, 6, 37–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, K.-W.; Cheong, H.J.; Song, J.Y.; Noh, J.Y.; Yang, T.U.; Kim, W.J. Clinical Manifestations of Influenza A and B in Children and Adults at a Tertiary Hospital in Korea during the 2011–2012 Season. Jpn. J. Infect. Dis. 2015, 68, 20–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, D.R.; Heffernan, R.T.; Paladini, M.; Konty, K.; Weiss, D.; Mostashari, F. Monitoring the Impact of Influenza by Age: Emergency Department Fever and Respiratory Complaint Surveillance in New York City. PLoS Med. 2007, 4, e247. [Google Scholar] [CrossRef] [Green Version]
- McCullers, J.A.; Hayden, F.G. Fatal Influenza B Infections: Time to Reexamine Influenza Research Priorities. J. Infect. Dis. 2012, 205, 870–872. [Google Scholar] [CrossRef] [Green Version]
- Paul Glezen, W.; Schmier, J.K.; Kuehn, C.M.; Ryan, K.J.; Oxford, J. The Burden of Influenza B: A Structured Literature Review. Am. J. Public Health 2013, 103, e43–e51. [Google Scholar] [CrossRef]
- Savy, V.; Ciapponi, A.; Bardach, A.; Glujovsky, D.; Aruj, P.; Mazzoni, A.; Gibbons, L.; Ortega-Barría, E.; Colindres, R.E. Burden of Influenza in Latin America and the Caribbean: A Systematic Review and Meta-Analysis. Influenza Other Respir. Viruses 2013, 7, 1017–1032. [Google Scholar] [CrossRef]
- WHO. Vaccines against Influenza WHO Position Paper—November 2012 = Note de Synthèse de l’OMS Concernant Les Vaccins Antigrippaux—Novembre 2012. Wkly. Epidemiol. Rec. 2012, 87, 461–476. [Google Scholar]
- Brazil Informe Técnico 24a Campanha Nacional de Vacinação Contra a Influenza Brasília. Available online: https://www.gov.br/saude/pt-br/assuntos/saude-de-a-a-z/c/calendario-nacional-de-vacinacao/arquivos/informe-da-24a-campanha-nacional-de-vacinacao-contra-a-influenza.pdf (accessed on 7 May 2022).
- Cox, N.J.; Subbarao, K. Global Epidemiology of Influenza: Past and Present. Annu. Rev. Med. 2000, 51, 407–421. [Google Scholar] [CrossRef]
- Skowronski, D.M.; Masaro, C.; Kwindt, T.L.; Mak, A.; Petric, M.; Li, Y.; Sebastian, R.; Chong, M.; Tam, T.; De Serres, G. Estimating Vaccine Effectiveness against Laboratory-Confirmed Influenza Using a Sentinel Physician Network: Results from the 2005-2006 Season of Dual A and B Vaccine Mismatch in Canada. Vaccine 2007, 25, 2842–2851. [Google Scholar] [CrossRef] [PubMed]
- Skowronski, D.M.; De Serres, G.; Dickinson, J.; Petric, M.; Mak, A.; Fonseca, K.; Kwindt, T.L.; Chan, T.; Bastien, N.; Charest, H.; et al. Component-Specific Effectiveness of Trivalent Influenza Vaccine as Monitored through a Sentinel Surveillance Network in Canada, 2006–2007. J. Infect. Dis. 2009, 199, 168–179. [Google Scholar] [CrossRef]
- WHO. Global Influenza Surveillance and Response System (GISRS). Available online: https://www.who.int/initiatives/global-influenza-surveillance-and-response-system (accessed on 31 March 2022).
- Belshe, R.B.; Coelingh, K.; Ambrose, C.S.; Woo, J.C.; Wu, X. Efficacy of Live Attenuated Influenza Vaccine in Children against Influenza B Viruses by Lineage and Antigenic Similarity. Vaccine 2010, 28, 2149–2156. [Google Scholar] [CrossRef] [PubMed]
- Ambrose, C.S.; Levin, M.J. The Rationale for Quadrivalent Influenza Vaccines. Hum. Vaccin Immunother. 2012, 8, 81–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tricco, A.C.; Chit, A.; Soobiah, C.; Hallett, D.; Meier, G.; Chen, M.H.; Tashkandi, M.; Bauch, C.T.; Loeb, M. Comparing Influenza Vaccine Efficacy against Mismatched and Matched Strains: A Systematic Review and Meta-Analysis. BMC Med. 2013, 11, 153. [Google Scholar] [CrossRef] [Green Version]
- Heikkinen, T.; Ikonen, N.; Ziegler, T. Impact of Influenza B Lineage-Level Mismatch between Trivalent Seasonal Influenza Vaccines and Circulating Viruses, 1999–2012. Clin. Infect. Dis. 2014, 59, 1519–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caini, S.; Kusznierz, G.; Garate, V.V.; Wangchuk, S.; Thapa, B.; de Paula Júnior, F.J.; Ferreira de Almeida, W.A.; Njouom, R.; Fasce, R.A.; Bustos, P.; et al. The Epidemiological Signature of Influenza B Virus and Its B/Victoria and B/Yamagata Lineages in the 21st Century. PLoS ONE 2019, 14, e0222381. [Google Scholar] [CrossRef] [Green Version]
- WHO. Surveillance Case Definitions for ILI and SARI. Available online: https://www.who.int/teams/control-of-neglected-tropical-diseases/lymphatic-filariasis/morbidity-management-and-disability-prevention/global-influenza-programme (accessed on 31 March 2022).
- Brazil. Ministry of Health. Guia de Vigilância em Saúde; 2019; p. 741. Brasília. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_saude_3ed.pdf (accessed on 7 May 2022).
- World Health Organization. WHO Information for Molecular Diagnosis of Influenza Virus—Update. Available online: http://www.who.int/influenza/gisrs_laboratory/molecular_diagnosis/en/ (accessed on 31 July 2020).
- Edgar, R.C. MUSCLE: Multiple Sequence Alignment with High Accuracy and High Throughput. Nucleic Acids Res. 2004, 32, 1792–1797. [Google Scholar] [CrossRef] [Green Version]
- Guindon, S.; Dufayard, J.-F.; Lefort, V.; Anisimova, M.; Hordijk, W.; Gascuel, O. New Algorithms and Methods to Estimate Maximum-Likelihood Phylogenies: Assessing the Performance of PhyML 3.0. Syst. Biol. 2010, 59, 307–321. [Google Scholar] [CrossRef] [Green Version]
- Darriba, D.; Taboada, G.L.; Doallo, R.; Posada, D. JModelTest 2: More Models, New Heuristics and Parallel Computing. Nat. Methods 2012, 9, 772. [Google Scholar] [CrossRef] [Green Version]
- Rambaut, A.; Lam, T.T.; Max Carvalho, L.; Pybus, O.G. Exploring the Temporal Structure of Heterochronous Sequences Using TempEst (Formerly Path-O-Gen). Virus Evol. 2016, 2, vew007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drummond, A.J.; Rambaut, A. BEAST: Bayesian Evolutionary Analysis by Sampling Trees. BMC Evol. Biol. 2007, 7, 214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suchard, M.A.; Rambaut, A. Many-Core Algorithms for Statistical Phylogenetics. Bioinformatics 2009, 25, 1370–1376. [Google Scholar] [CrossRef] [Green Version]
- Drummond, A.J.; Nicholls, G.K.; Rodrigo, A.G.; Solomon, W. Estimating Mutation Parameters, Population History and Genealogy Simultaneously from Temporally Spaced Sequence Data. Genetics 2002, 161, 1307–1320. [Google Scholar] [CrossRef] [PubMed]
- Minin, V.N.; Bloomquist, E.W.; Suchard, M.A. Smooth Skyride through a Rough Skyline: Bayesian Coalescent-Based Inference of Population Dynamics. Mol. Biol. Evol. 2008, 25, 1459–1471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rambaut, A.; Drummond, A.J.; Xie, D.; Baele, G.; Suchard, M.A. Posterior Summarization in Bayesian Phylogenetics Using Tracer 1.7. Syst. Biol. 2018, 67, 901–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parker, J.; Rambaut, A.; Pybus, O.G. Correlating Viral Phenotypes with Phylogeny: Accounting for Phylogenetic Uncertainty. Infect. Genet. Evol. 2008, 8, 239–246. [Google Scholar] [CrossRef]
- Yap, J.; Tan, C.H.; Cook, A.R.; Loh, J.P.; Tambyah, P.A.; Tan, B.H.; Lee, V.J. Differing Clinical Characteristics between Influenza Strains among Young Healthy Adults in the Tropics. BMC Infect. Dis. 2012, 12, 12. [Google Scholar] [CrossRef] [Green Version]
- Sočan, M.; Prosenc, K.; Učakar, V.; Berginc, N. A Comparison of the Demographic and Clinical Characteristics of Laboratory-Confirmed Influenza B Yamagata and Victoria Lineage Infection. J. Clin. Virol. 2014, 61, 156–160. [Google Scholar] [CrossRef]
- Orsi, A.; Colomba, G.M.E.; Pojero, F.; Calamusa, G.; Alicino, C.; Trucchi, C.; Canepa, P.; Ansaldi, F.; Vitale, F.; Tramuto, F. Trends of Influenza B during the 2010-2016 Seasons in 2 Regions of North and South Italy: The Impact of the Vaccine Mismatch on Influenza Immunisation Strategy. Hum. Vaccine Immunother. 2018, 14, 523–531. [Google Scholar] [CrossRef]
- Hönemann, M.; Martin, D.; Pietsch, C.; Maier, M.; Bergs, S.; Bieck, E.; Liebert, U.G. Influenza B Virus Infections in Western Saxony, Germany in Three Consecutive Seasons between 2015 and 2018: Analysis of Molecular and Clinical Features. Vaccine 2019, 37, 6550–6557. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Guan, W.; Lam, T.T.-Y.; Pan, S.; Wu, S.; Zhan, Y.; Viboud, C.; Holmes, E.C.; Yang, Z. Differing Epidemiological Dynamics of Influenza B Virus Lineages in Guangzhou, Southern China, 2009–2010. J. Virol. 2013, 87, 12447–12456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perosa, A.H.; Granato, C.; Bellei, N. Detection of Influenza B Lineages from 2001 to 2013 in a Tertiary Hospital in the City of São Paulo, Brazil. Mem. Inst. Oswaldo Cruz. 2015, 110, 606–610. [Google Scholar] [CrossRef] [Green Version]
- Vijaykrishna, D.; Holmes, E.C.; Joseph, U.; Fourment, M.; Su, Y.C.F.; Halpin, R.; Lee, R.T.C.; Deng, Y.-M.; Gunalan, V.; Lin, X.; et al. The Contrasting Phylodynamics of Human Influenza B Viruses. Elife 2015, 4, e05055. [Google Scholar] [CrossRef] [PubMed]
- Barr, I.G.; Vijaykrishna, D.; Sullivan, S.G. Differential Age Susceptibility to Influenza B/Victoria Lineage Viruses in the 2015 Australian Influenza Season. Euro Surveill 2016, 21, 30118. [Google Scholar] [CrossRef]
- Seleka, M.; Treurnicht, F.K.; Tempia, S.; Hellferscee, O.; Mtshali, S.; Cohen, A.L.; Buys, A.; McAnerney, J.M.; Besselaar, T.G.; Pretorius, M.; et al. Epidemiology of Influenza B/Yamagata and B/Victoria Lineages in South Africa, 2005–2014. PLoS ONE 2017, 12, e0177655. [Google Scholar] [CrossRef] [PubMed]
- Skowronski, D.M.; Chambers, C.; De Serres, G.; Sabaiduc, S.; Winter, A.-L.; Dickinson, J.A.; Gubbay, J.B.; Fonseca, K.; Drews, S.J.; Charest, H.; et al. Age-Related Differences in Influenza B Infection by Lineage in a Community-Based Sentinel System, 2010–2011 to 2015–2016, Canada. J. Infect. Dis. 2017, 216, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Virk, R.K.; Jayakumar, J.; Mendenhall, I.H.; Moorthy, M.; Lam, P.; Linster, M.; Lim, J.; Lin, C.; Oon, L.L.E.; Lee, H.K.; et al. Divergent Evolutionary Trajectories of Influenza B Viruses Underlie Their Contemporaneous Epidemic Activity. Proc. Natl. Acad. Sci. USA 2020, 117, 619–628. [Google Scholar] [CrossRef] [Green Version]
- Skowronski, D.M.; Hottes, T.S.; De Serres, G.; Ward, B.J.; Janjua, N.Z.; Sabaiduc, S.; Chan, T.; Petric, M. Influenza B/Victoria Antigen Induces Strong Recall of B/Yamagata But Lower B/Victoria Response in Children Primed With Two Doses of B/Yamagata. Pediatric Infect. Dis. J. 2011, 30, 833–839. [Google Scholar] [CrossRef]
- Vieira, M.C.; Donato, C.M.; Arevalo, P.; Rimmelzwaan, G.F.; Wood, T.; Lopez, L.; Huang, Q.S.; Dhanasekaran, V.; Koelle, K.; Cobey, S. Lineage-Specific Protection and Immune Imprinting Shape the Age Distributions of Influenza B Cases. Nat. Commun. 2021, 12, 4313. [Google Scholar] [CrossRef]
- Gostic, K.M.; Bridge, R.; Brady, S.; Viboud, C.; Worobey, M.; Lloyd-Smith, J.O. Childhood Immune Imprinting to Influenza A Shapes Birth Year-Specific Risk during Seasonal H1N1 and H3N2 Epidemics. PLoS Pathog. 2019, 15, e1008109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedford, T.; Suchard, M.A.; Lemey, P.; Dudas, G.; Gregory, V.; Hay, A.J.; McCauley, J.W.; Russell, C.A.; Smith, D.J.; Rambaut, A. Integrating Influenza Antigenic Dynamics with Molecular Evolution. eLife 2014, 3, e01914. [Google Scholar] [CrossRef] [PubMed]
- Brazil. IBGE The Brazilian Institute of Geography and Statistics. IBGE. Available online: https://www.ibge.gov.br/apps/populacao/projecao/index.html (accessed on 30 March 2022).
- McCullers, J.A.; Saito, T.; Iverson, A.R. Multiple Genotypes of Influenza B Virus Circulated between 1979 and 2003. J. Virol. 2004, 78, 12817–12828. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, R.; Holmes, E.C. The Evolutionary Dynamics of Human Influenza B Virus. J. Mol. Evol. 2008, 66, 655–663. [Google Scholar] [CrossRef] [Green Version]
- Langat, P.; Raghwani, J.; Dudas, G.; Bowden, T.A.; Edwards, S.; Gall, A.; Bedford, T.; Rambaut, A.; Daniels, R.S.; Russell, C.A.; et al. Genome-Wide Evolutionary Dynamics of Influenza B Viruses on a Global Scale. PLoS Pathog. 2017, 13, e1006749. [Google Scholar] [CrossRef] [Green Version]
- Motta, F.C.; Siqueira, M.M.; Lugon, A.K.; Straliotto, S.M.; Fernandes, S.B.; Krawczuk, M.M. The Reappearance of Victoria Lineage Influenza B Virus in Brazil, Antigenic and Molecular Analysis. J. Clin. Virol. 2006, 36, 208–214. [Google Scholar] [CrossRef]
- Paiva, T.M.; Benega, M.A.; Silva, D.B.B.; Santos, K.C.O.; Cruz, A.S.; Hortenci, M.F.; Barbieri, M.T.; Monteiro, M.M.; Barbosa, H.A.; Carvalhanas, T.R.M.P. Evolutionary Pattern of Reemerging Influenza B/Victoria Lineage Viruses in São Paulo, Brazil, 1996–2012: Implications for Vaccine Composition Strategy. J. Med. Virol. 2013, 85, 1983–1989. [Google Scholar] [CrossRef]
- de Barros, E.N.C.; Cintra, O.; Rossetto, E.; Freitas, L.; Colindres, R. Patterns of Influenza B Circulation in Brazil and Its Relevance to Seasonal Vaccine Composition. Braz. J. Infect. Dis. 2016, 20, 81–90. [Google Scholar] [CrossRef] [Green Version]
- Lapinscki, B.; Pereira, L.A.; Nogueira, M.B.; Vidal, L.R.; Riediger, I.; Debur, M.C.; Presibella, M.; Raboni, S.M. Molecular Epidemiology of Influenza B Virus and Implications in Immunization Strategy, Southern Brazil. Vaccine 2018, 36, 107–113. [Google Scholar] [CrossRef]
- Ray, R.; Dos Santos, G.; Buck, P.O.; Claeys, C.; Matias, G.; Innis, B.L.; Bekkat-Berkani, R. A Review of the Value of Quadrivalent Influenza Vaccines and Their Potential Contribution to Influenza Control. Hum. Vaccine Immunother. 2017, 13, 1640–1652. [Google Scholar] [CrossRef] [Green Version]
- WHO. Recommended Composition of Influenza Virus Vaccines for Use in the 2013 Influenza Season. Available online: https://www.who.int/influenza/vaccines/virus/recommendations/201209_recommendation.pdf?ua=1 (accessed on 31 March 2022).
- Crépey, P.; Boiron, L.; Araujo, R.R.; Lopez, J.G.; Petitjean, A.; de Albuquerque Luna, E.J. Impact of Quadrivalent Influenza Vaccines in Brazil: A Cost-Effectiveness Analysis Using an Influenza Transmission Model. BMC Public Health 2020, 20, 1374. [Google Scholar] [CrossRef] [PubMed]
- Tisa, V.; Barberis, I.; Faccio, V.; Paganino, C.; Trucchi, C.; Martini, M.; Ansaldi, F. Quadrivalent Influenza Vaccine: A New Opportunity to Reduce the Influenza Burden. J. Prev. Med. Hyg. 2016, 57, E28–E33. [Google Scholar] [PubMed]
- Jamotte, A.; Chong, C.F.; Manton, A.; Macabeo, B.; Toumi, M. Impact of Quadrivalent Influenza Vaccine on Public Health and Influenza-Related Costs in Australia. BMC Public Health 2016, 16, 630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Boer, P.T.; van Maanen, B.M.; Damm, O.; Ultsch, B.; Dolk, F.C.K.; Crépey, P.; Pitman, R.; Wilschut, J.C.; Postma, M.J. A Systematic Review of the Health Economic Consequences of Quadrivalent Influenza Vaccination. Expert Rev. Pharm. Outcomes Res. 2017, 17, 249–265. [Google Scholar] [CrossRef] [PubMed]

| Influenza B Lineages | ||||
|---|---|---|---|---|
| Variables | All (n = 514) | Victoria (n = 265) | Yamagata (n = 249) | p-Value |
| Brazilian geographical region (%) | 51.6 (265) | 48.4 (249) | 0.157 | |
| Northeast | 6.2 (32/514) | 7.9 (21) | 4.4 (11) | |
| Southeast | 23.5 (121/514) | 24.9 (66) | 22.1 (55) | |
| South | 67.2 (178/514) | 73.5 (178) | 73.5 (183) | |
| Gender (masc %) | 54.2 (278/514) | 57.4 (152) | 50.8 (126) | 0.081 |
| Comorbidities (%) | 28.5 (103/361) | 29.9(49) | 27.4 (54) | 0.344 |
| Hospitalization | 90.4 (255/282) | 92.6 (138) | 88.0 (117) | 0.131 |
| Fatal outcome (%) | 3.4 (14/409) | 3.4 (6) | 3.4 (8) | 0.599 |
| Reported clinical symptoms (%) | ||||
| Dyspnea | 39.7 (204/514) | 39.6 (105) | 39.8 (99) | 0.523 |
| Fever | 93.6 (480/513) | 94.3 (249) | 92.8 (231) | 0.297 |
| Cough | 93.8 (480/512) | 93.6 (247) | 94.0 (233) | 0.501 |
| Sore throat | 48.0 (243/506) | 45.4 (118) | 50.8 (125) | 0.129 |
| Myalgia | 26.6 (136/511) | 24.7 (65) | 28.6 (71) | 0.184 |
| Coryza | 21.4 (109/510) | 24.1 (63) | 18.5 (46) | 0.073 |
| Arthralgia | 4.3 (22/512) | 3.8 (10) | 4.8 (12) | 0.363 |
| Age (median, range in years) | 20.5 (0–99) | 16.7 (0–99) | 31.4 (0–88) | <0.001 |
| Statistic | Observed Mean (95%CI) | Null Mean (95%CI) | Significance (p-Value) |
|---|---|---|---|
| AI | 6.4 (5.5–7.2) | 6.3 (5.1–7.4) | 0.550 |
| PS | 37.8 (36.0–40.0) | 38.9 (34.9–43.1) | 0.370 |
| MC SARI | 2.9 (2.0–5.0) | 3.4 (2.6–4.5) | 0.810 |
| MC ILI | 3.7 (3.0–5.0) | 4.4(3.1–6.2) | 0.569 |
| Influenza Season | Northern Hemisphere (NH) | Influenza Season | Southern Hemisphere (SH) | ||
|---|---|---|---|---|---|
| Lineage | Strain | Lineage | Strain | ||
| 2019/20 | Yamagata | B/Phuket/3072/2013 | 2020 | Victoria | B/Washington/02/2019 |
| 2018/19 | Yamagata | B/Phuket/3072/20131 | 2019 | Yamagata | B/Phuket/3072/20132 |
| 2017/18 | Victoria | B/Brisbane/60/2008 | 2018 | Yamagata | B/Phuket/3072/2013 |
| 2016/17 | Victoria | B/Brisbane/60/2008 | 2017 | Victoria | B/Brisbane/60/2008 |
| 2015/16 | Yamagata | B/Phuket/3072/2013 | 2016 | Victoria | B/Brisbane/60/2008 |
| 2014/15 | Yamagata | B/Massachusetts/2/2012 | 2015 | Yamagata | B/Phuket/3072/2013 |
| 2013/14 | Yamagata | B/Massachusetts/2/2012 | 2014 | Yamagata | B/Massachusetts/2/2012 |
| 2012/13 | Yamagata | B/Wisconsin/1/2010 | 2013 | Yamagata | B/Wisconsin/1/2010 |
| 2011/12 | Victoria | B/Brisbane/60/2008 | 2012 | Victoria | B/Brisbane/60/2008 |
| 2010/11 | Victoria | B/Brisbane/60/2008 | 2011 | Victoria | B/Brisbane/60/2008 |
| 2009/10 | Victoria | B/Brisbane/60/2008 | 2010 | Victoria | B/Brisbane/60/2008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, J.C.d.; Siqueira, M.M.; Brown, D.; Lopes, J.O.; Costa, B.C.d.; Gama, E.L.; Aguiar-Oliveira, M.d.L. Vaccine Mismatches, Viral Circulation, and Clinical Severity Patterns of Influenza B Victoria and Yamagata Infections in Brazil over the Decade 2010–2020: A Statistical and Phylogeny–Trait Analyses. Viruses 2022, 14, 1477. https://doi.org/10.3390/v14071477
Costa JCd, Siqueira MM, Brown D, Lopes JO, Costa BCd, Gama EL, Aguiar-Oliveira MdL. Vaccine Mismatches, Viral Circulation, and Clinical Severity Patterns of Influenza B Victoria and Yamagata Infections in Brazil over the Decade 2010–2020: A Statistical and Phylogeny–Trait Analyses. Viruses. 2022; 14(7):1477. https://doi.org/10.3390/v14071477
Chicago/Turabian StyleCosta, Jaline Cabral da, Marilda Mendonça Siqueira, David Brown, Jonathan Oliveira Lopes, Braulia Caetano da Costa, Eric Lopes Gama, and Maria de Lourdes Aguiar-Oliveira. 2022. "Vaccine Mismatches, Viral Circulation, and Clinical Severity Patterns of Influenza B Victoria and Yamagata Infections in Brazil over the Decade 2010–2020: A Statistical and Phylogeny–Trait Analyses" Viruses 14, no. 7: 1477. https://doi.org/10.3390/v14071477






