Two Newly Isolated Enterobacter-Specific Bacteriophages: Biological Properties and Stability Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacterial Strains
2.2. Bacteriophage Isolation and Amplification
2.3. Assessment of the Lytic Spectrum of Phages
2.4. Assessment of Optimal Multiplicity of Infection (MOI) for Phages
2.5. Planktonic Bacterial Lysis Assay
2.6. Determination of the Phage Adsorption Time
2.7. Long-Term Study of Phage Stability under Various Temperature Conditions
2.8. Investigation of Phage Stability in Solutions of Different pH and Disinfectants
2.9. Stability of Phage Lysates in Urine Sample In Vitro
2.10. Transmission Electron Microscopy (TEM)
2.11. Phage DNA Isolation Procedure and DNA Sequencing
2.12. Statistical Analysis
3. Results
3.1. Characterization of the Bacterial Strains
3.2. Isolated Bacteriophages
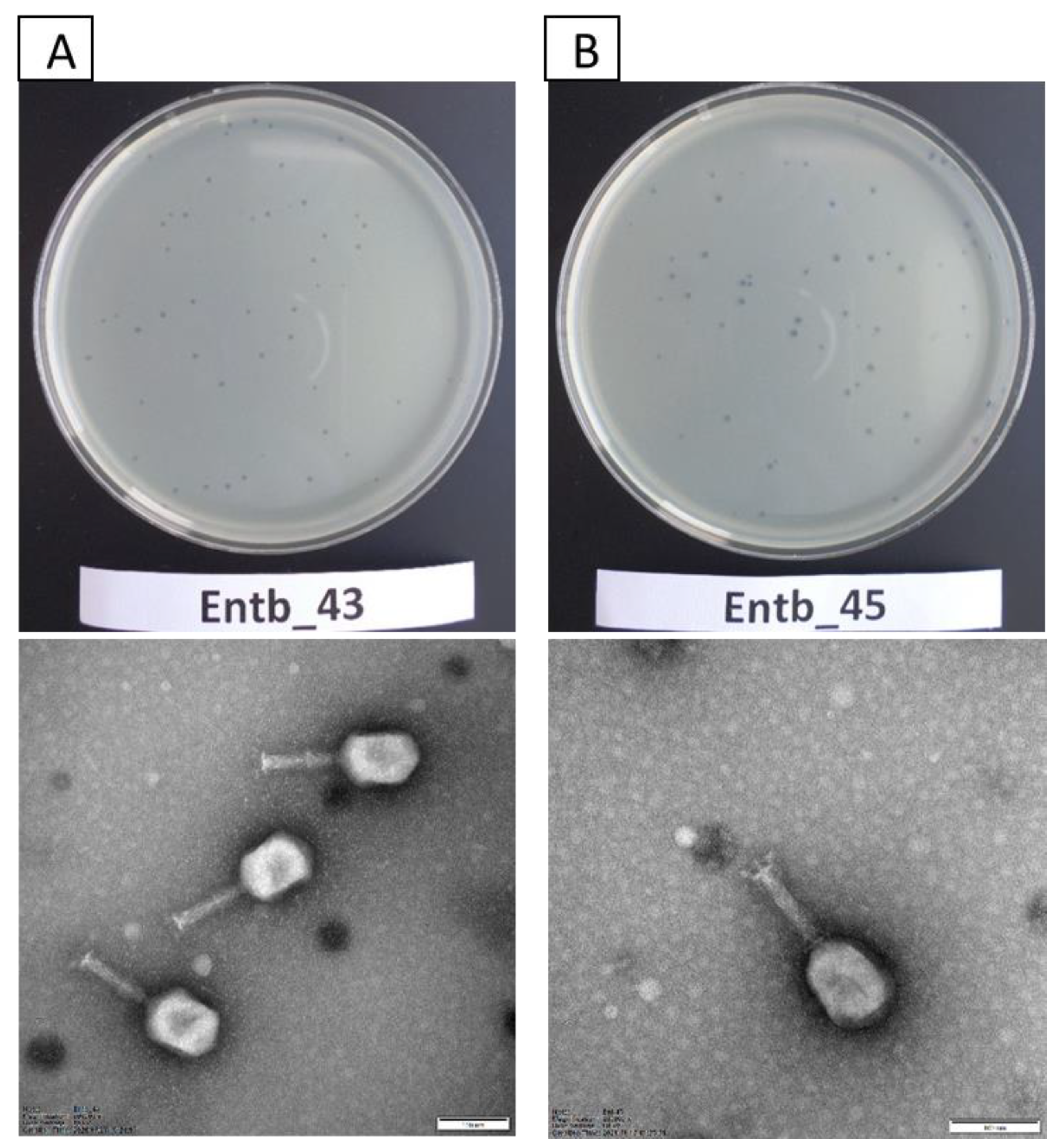
3.3. Morphology of Entb_43 and Entb_45 Phages and Their Plaques
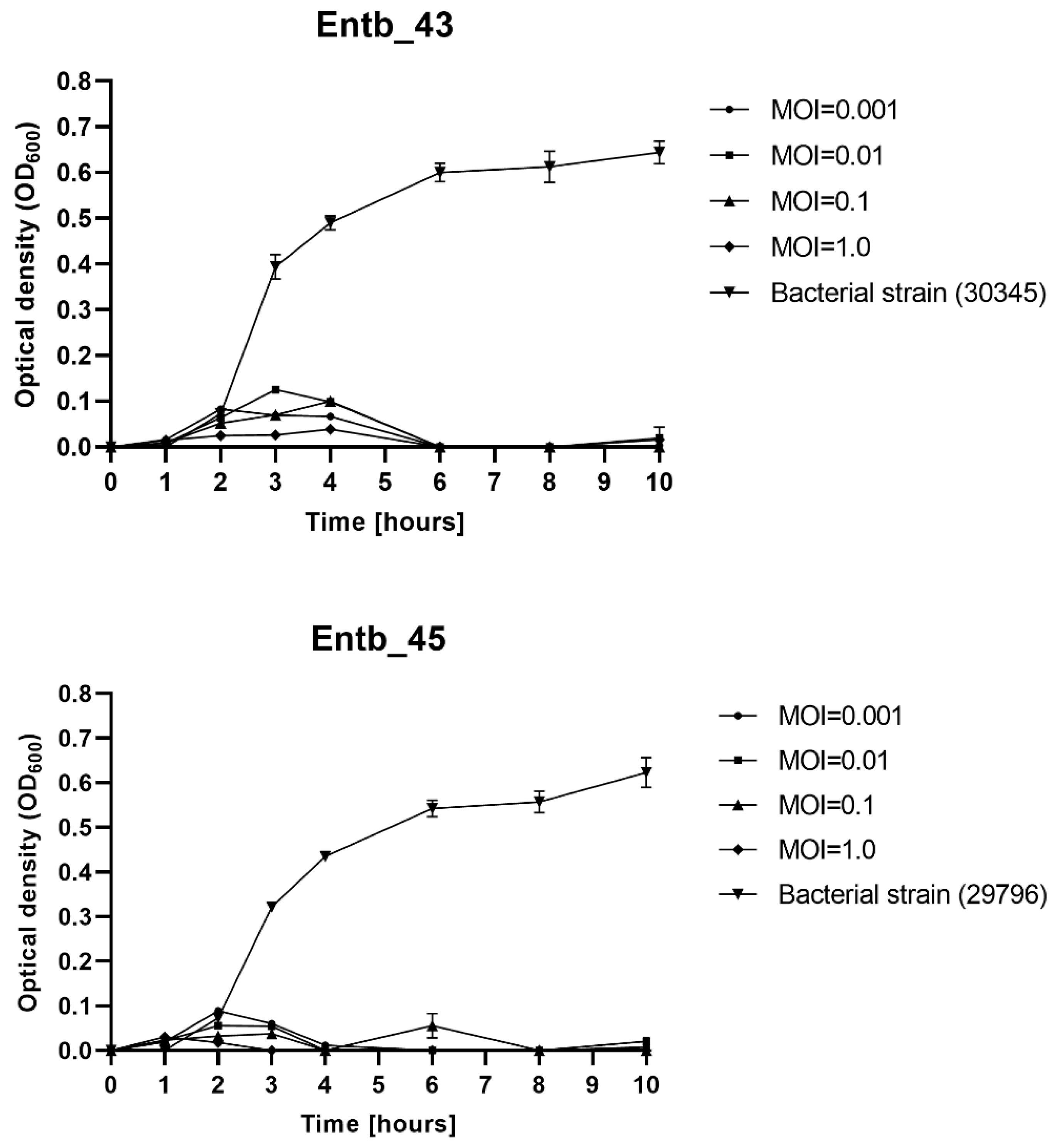
3.4. Influence of Different MOI on the Effectiveness of Phage Amplification and Antimicrobial Effect
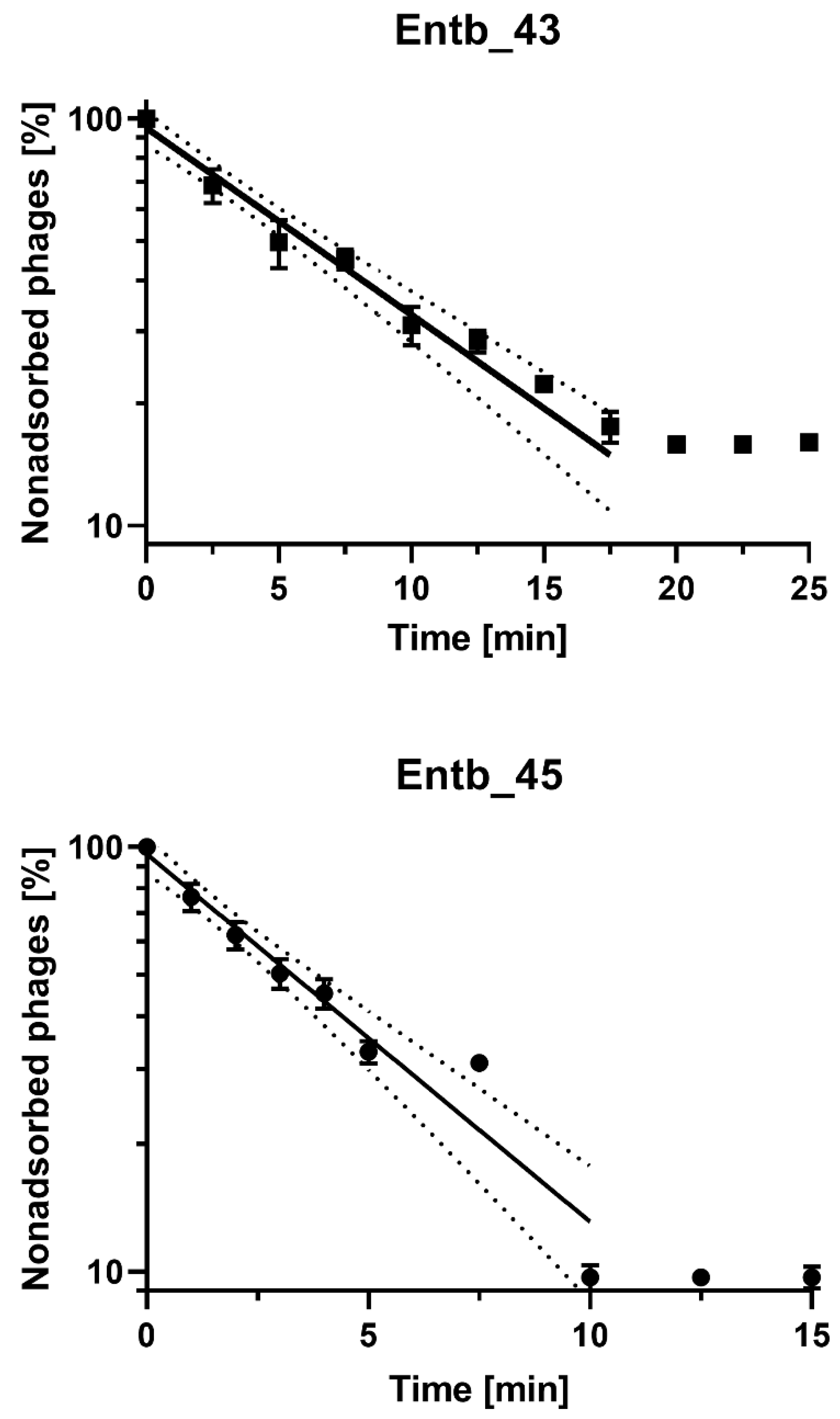
3.5. Phage Adsorption to Bacterial Cells
3.6. Genome Sequencing
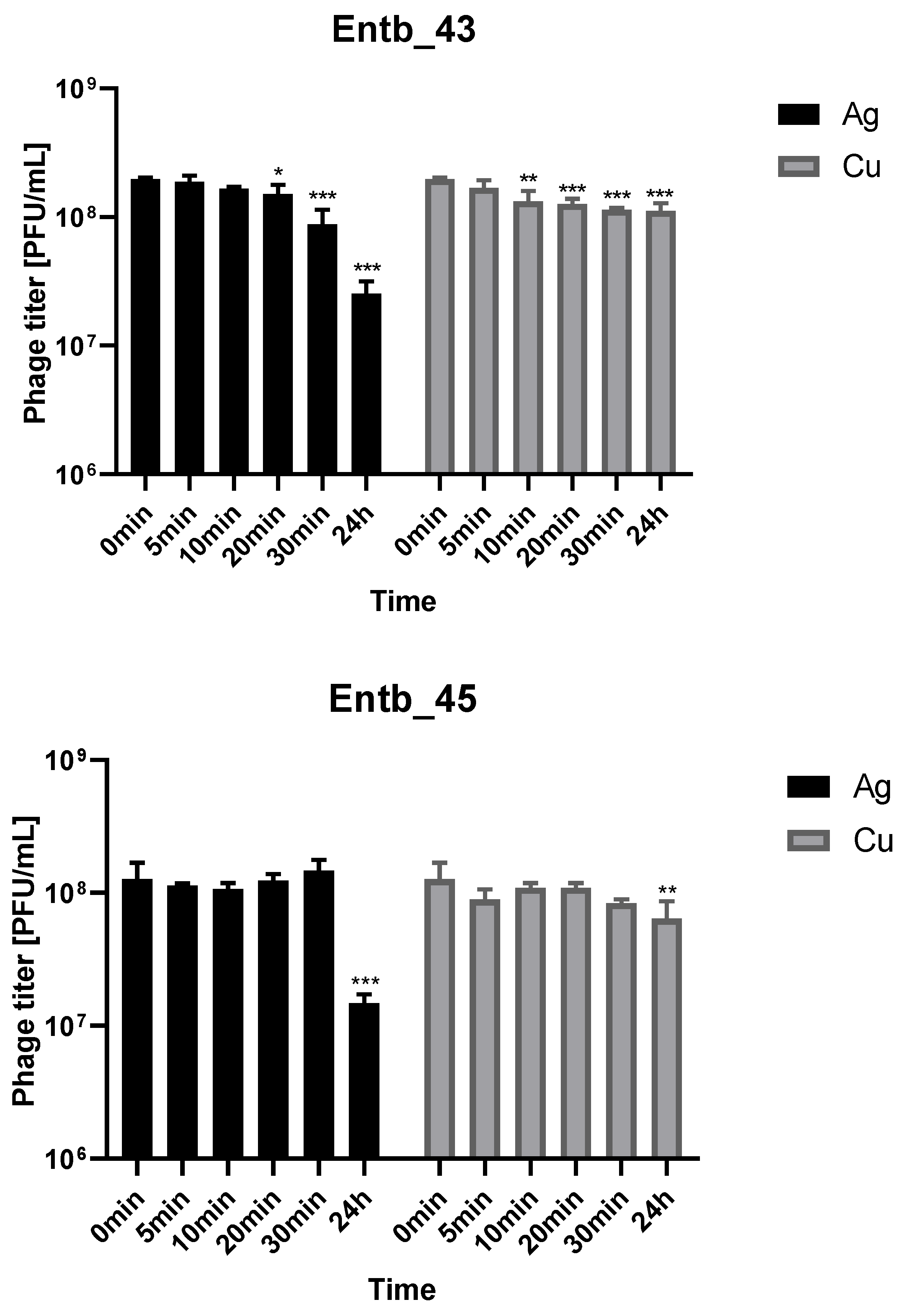
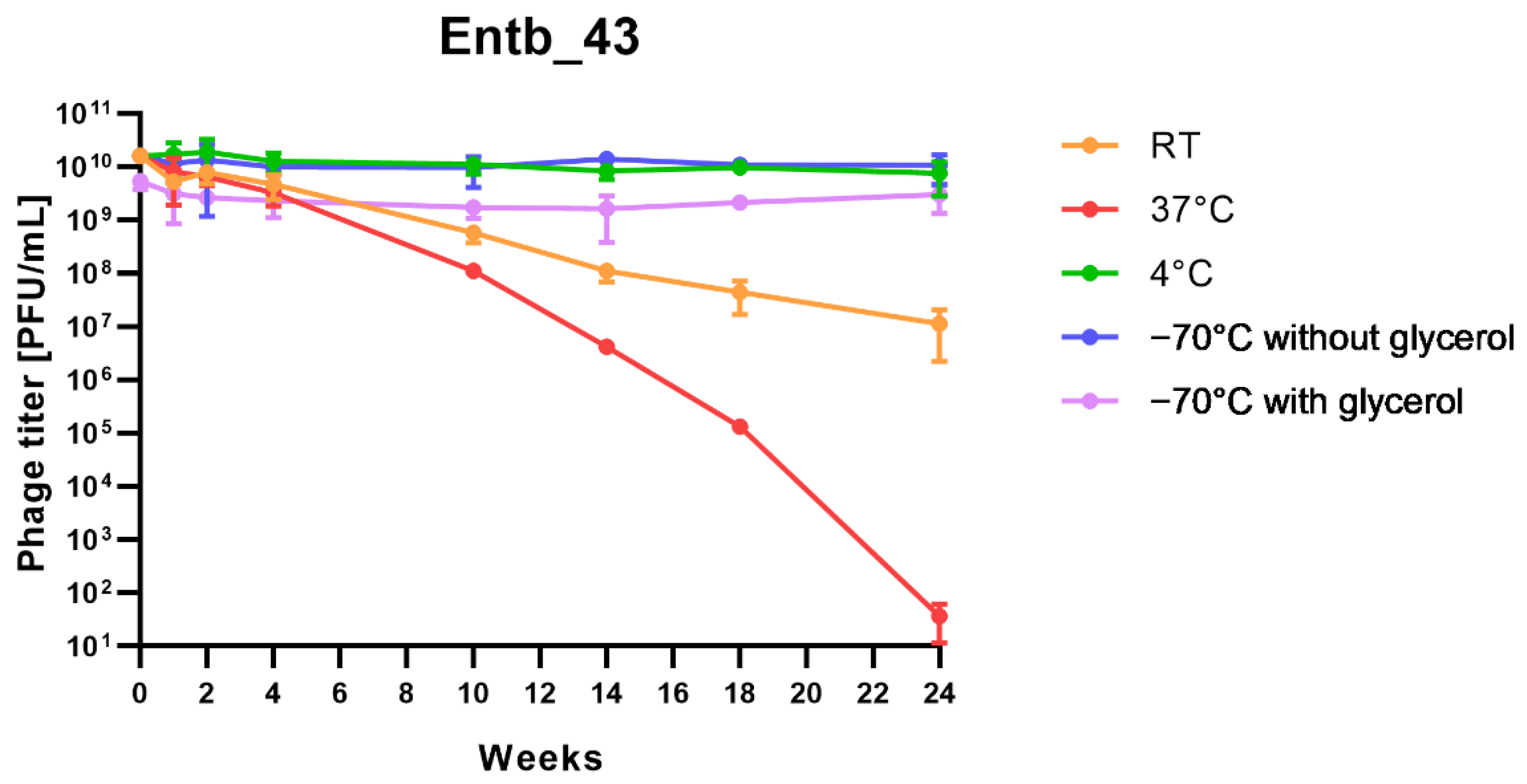
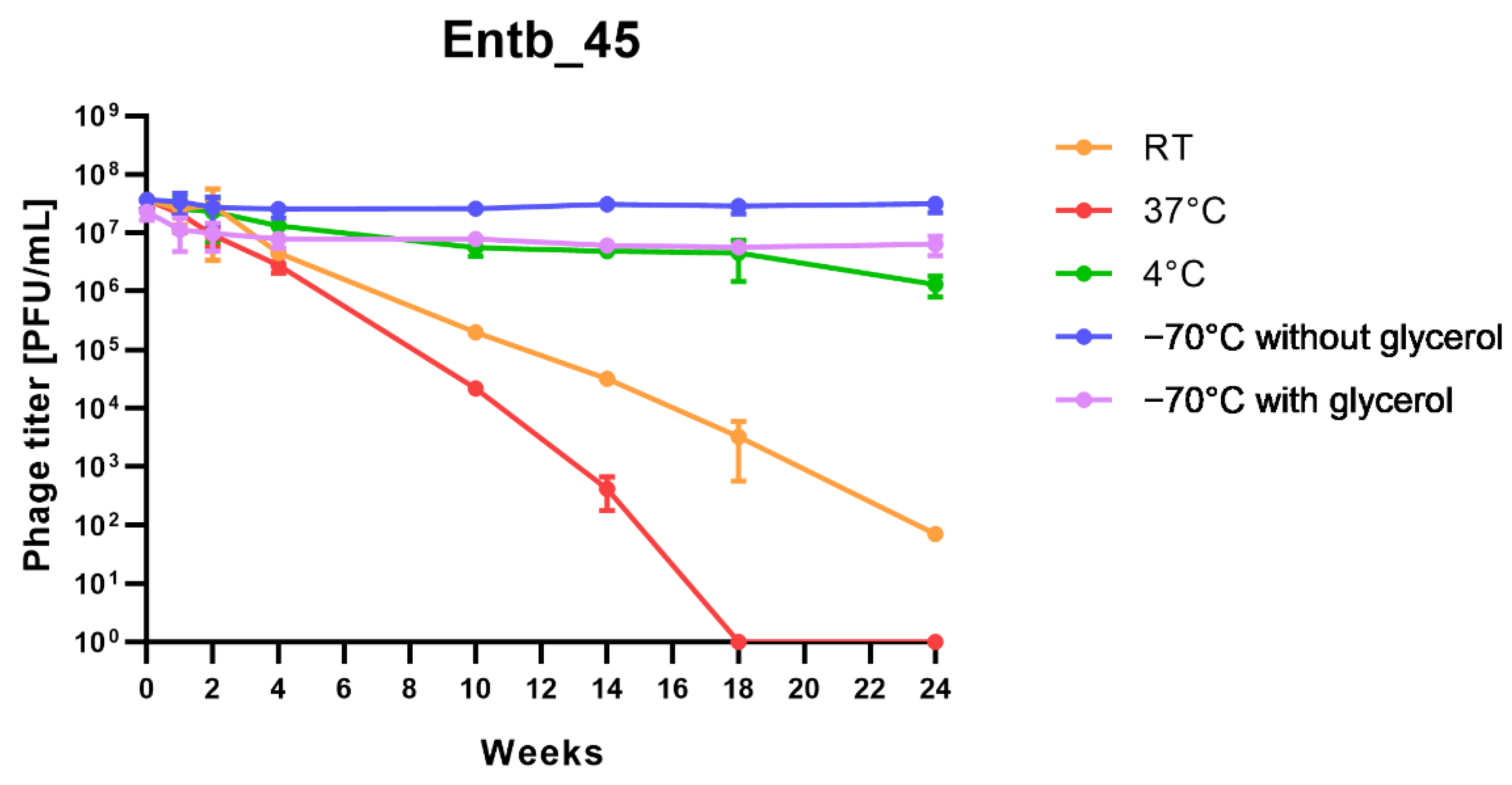
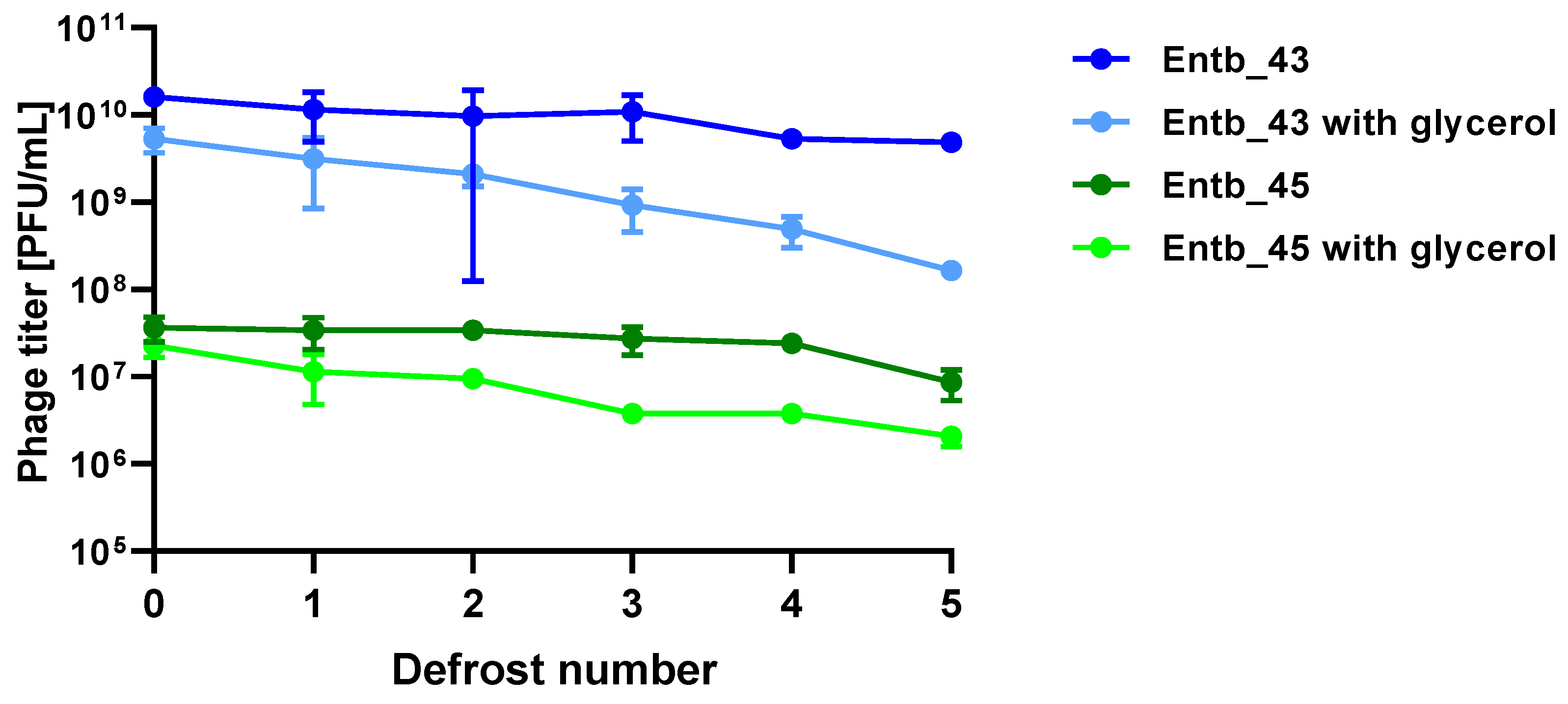
3.7. Stability Studies of New Enterobacter-Specific Phages
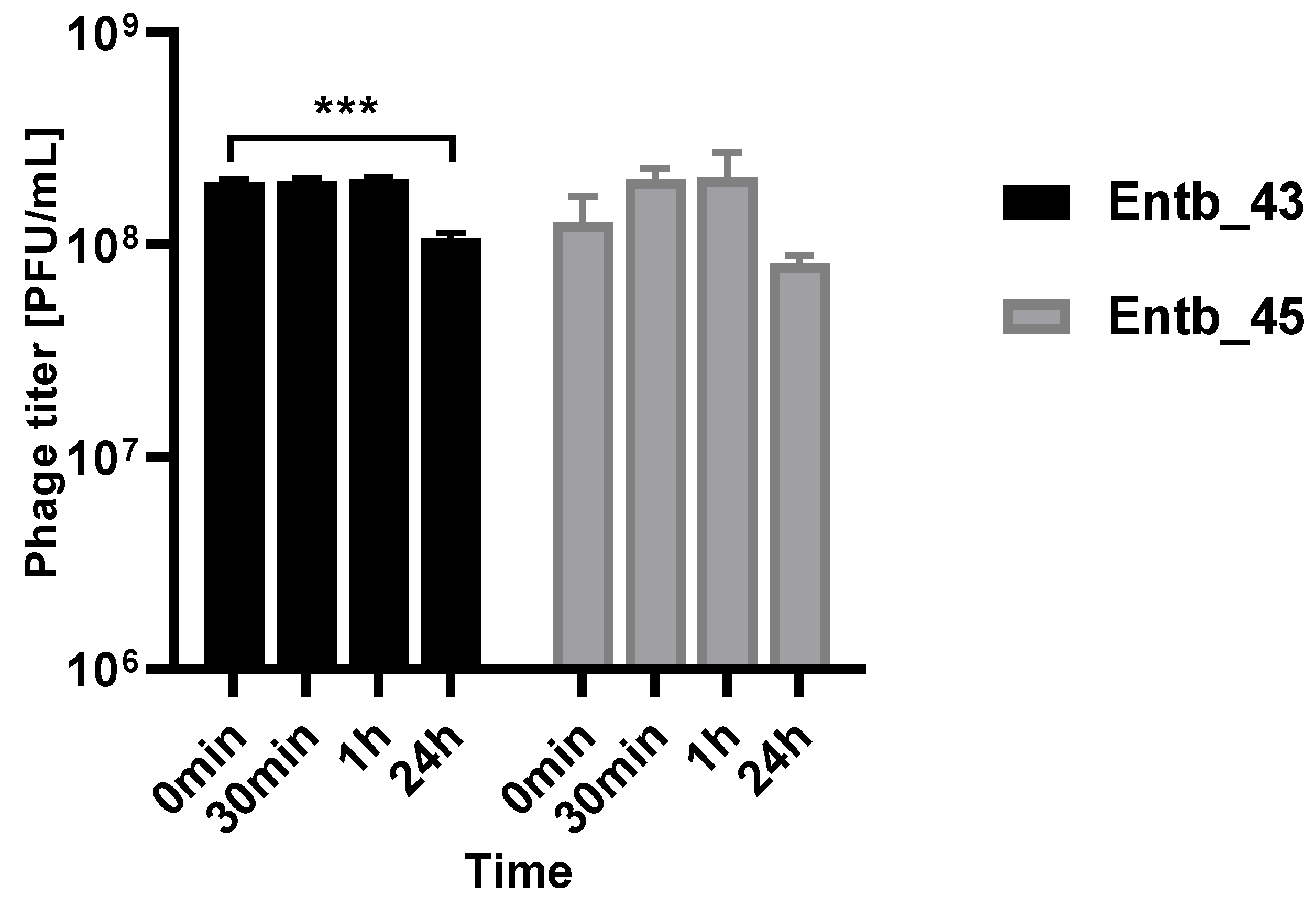
3.8. Phage Stability in a Urine Sample
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hormaeche, E.; Edwards, P.R. A proposed genus Enterobacter. Int. Bull. Bacteriol. Nomencl. Taxon. 1960, 10, 71–74. [Google Scholar] [CrossRef] [Green Version]
- Santajit, S.; Indrawattana, N. Mechanisms of Antimicrobial Resistance in ESKAPE Pathogens. Biomed Res. Int. 2016, 2016, 2475067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, Y.X.; Wang, C.Y.; Li, Y.Y.; Li, J.; Wan, Q.Q.; Chen, J.H.; Tay, F.R.; Niu, L.N. Considerations and Caveats in Combating ESKAPE Pathogens against Nosocomial Infections. Adv. Sci. 2019, 7, 1901872. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rice, L.B. Federal Funding for the Study of Antimicrobial Resistance in Nosocomial Pathogens: No ESKAPE. J. Infect. Dis. 2008, 197, 1079–1081. [Google Scholar] [CrossRef]
- Mulani, M.S.; Kamble, E.E.; Kumkar, S.N.; Tawre, M.S.; Pardesi, K.R. Emerging Strategies to Combat ESKAPE Pathogens in the Era of Antimicrobial Resistance: A Review. Front. Microbiol. 2019, 10, 539. [Google Scholar] [CrossRef]
- WHO Priority Pathogens List. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 12 August 2021).
- Ramos-Vivas, J.; Chapartegui-González, I.; Fernández-Martínez, M.; González-Rico, C.; Fortún, J.; Escudero, R.; Marco, F.; Linares, L.; Montejo, M.; Aranzamendi, M.; et al. Biofilm formation by multidrug resistant Enterobacteriaceae strains isolated from solid organ transplant recipients. Sci. Rep. 2019, 9, 8928. [Google Scholar] [CrossRef] [Green Version]
- Cunha, B.A.; Theodoris, A.C.; Yannelli, B. Enterobacter cloacae graft infection/bacteremia in a hemodialysis patient. Am. J. Infect. Control. 2000, 28, 181–183. [Google Scholar] [CrossRef]
- Álvarez-Marín, R.; Lepe, J.A.; Gasch-Blasi, O.; Rodríguez-Martínez, J.M.; Calvo-Montes, J.; Lara-Contreras, R.; Martín-Gandul, C.; Tubau-Quintano, F.; Cano-García, M.E.; Rodríguez-López, F.; et al. Clinical characteristics and outcome of bacteraemia caused by Enterobacter cloacae and Klebsiella aerogenes: More similarities than differences. J. Glob. Antimicrob. Resist. 2021, 25, 351–358. [Google Scholar] [CrossRef]
- Boguniewicz, J.; Revell, P.A.; Scheurer, M.E.; Hulten, K.G.; Palazzi, D.L. Risk factors for microbiologic failure in children with Enterobacter species bacteremia. PLoS ONE 2021, 16, e0258114. [Google Scholar] [CrossRef]
- Khawcharoenporn, T.; Vasoo, S.; Singh, K. Urinary Tract Infections due to Multidrug-Resistant Enterobacteriaceae: Prevalence and Risk Factors in a Chicago Emergency Department. Emerg. Med. Int. 2013, 2013, 258517. [Google Scholar] [CrossRef] [Green Version]
- Akbari, M.; Bakhshi, B.; Najar Peerayeh, S. Particular Distribution of Enterobacter cloacae Strains Isolated from Urinary Tract Infection within Clonal Complexes. Iran. Biomed. J. 2016, 20, 49–55. [Google Scholar] [PubMed]
- Breathnach, A.S.; Riley, P.A.; Shad, S.; Jownally, S.M.; Law, R.; Chin, P.C.; Kaufmann, M.E.; Smith, E.J. An outbreak of wound infection in cardiac surgery patients caused by Enterobacter cloacae arising from cardioplegia ice. J. Hosp. Infect. 2006, 64, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, R.; Prudêncio, C. Post-surgical wound infections involving Enterobacteriaceae with reduced susceptibility to β-lactams in two Portuguese hospitals. Int. Wound J. 2010, 7, 508–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.; Wang, L.; Yang, Y.; Lu, F.; Ma, X.; Xia, X.; Jiang, J. Enterobacter cloacae infection after anterior cervical decompression and fusion: Case study and literature review. Int. J. Clin. Exp. Med. 2015, 8, 3438–3446. [Google Scholar]
- Al Yazidi, L.S.; Hameed, H.; Isaacs, D.; Axt, M.; Kesson, A. Enterobacter cloacae osteoarticular infection without risk factors: Case report and review of the literature. J. Paediatr. Child Health 2018, 54, 915–917. [Google Scholar] [CrossRef]
- Cisse, H.; Vernet-Garnier, V.; Hentzien, M.; Bajolet, O.; Lebrun, D.; Bonnet, M.; Ohl, X.; Diallo, S.; Bani-Sadr, F. Treatment of bone and joint infections caused by Enterobacter cloacae with a fluoroquinolone-cotrimoxazole combination. Int. J. Antimicrob. Agents 2019, 54, 245–248. [Google Scholar] [CrossRef]
- Huang, J.; Xu, Q.; Liu, F.; Xiong, H.; Yang, J. Enterobacter cloacae infection of the shoulder in a 52-year-old woman without apparent predisposing risk factor: A case report and literature review. BMC Infect. Dis. 2021, 21, 13. [Google Scholar] [CrossRef]
- Novak, A.; Goic-Barisic, I.; Andrasevic, A.T.; Butic, I.; Radic, M.; Jelic, M.; Rubic, Z.; Tonkic, M. Monoclonal outbreak of VIM-1-carbapenemase-producing Enterobacter cloacae in intensive care unit, University Hospital Centre Split, Croatia. Microb. Drug Resist. 2014, 20, 399–403. [Google Scholar] [CrossRef]
- Van Maerken, T.; de Brabandere, E.; Noël, A.; Coorevits, L.; de Waegemaeker, P.; Ablorh, R.; Bouchez, S.; Herck, I.; Peperstraete, H.; Bogaerts, P.; et al. A recurrent and transesophageal echocardiography-associated outbreak of extended-spectrum β-lactamase-producing Enterobacter cloacae complex in cardiac surgery patients. Antimicrob. Resist. Infect. Control. 2019, 8, 152. [Google Scholar] [CrossRef]
- Noël, A.; Vastrade, C.; Dupont, S.; de Barsy, M.; Huang, T.D.; van Maerken, T.; Leroux-Roels, I.; Delaere, B.; Melly, L.; Rondelet, B.; et al. Nosocomial outbreak of extended-spectrum β-lactamase-producing Enterobacter cloacae among cardiothoracic surgical patients: Causes and consequences. J. Hosp. Infect. 2019, 102, 54–60. [Google Scholar] [CrossRef]
- Ferry, A.; Plaisant, F.; Ginevra, C.; Dumont, Y.; Grando, J.; Claris, O.; Vandenesch, F.; Butin, M. Enterobacter cloacae colonisation and infection in a neonatal intensive care unit: Retrospective investigation of preventive measures implemented after a multiclonal outbreak. BMC Infect. Dis. 2020, 20, 682. [Google Scholar] [CrossRef] [PubMed]
- Yurdakul, D.; Yazgan-Karataş, A.; Şahin, F. Enterobacter Strains Might Promote Colon Cancer. Curr. Microbiol. 2015, 71, 403–411. [Google Scholar] [CrossRef] [PubMed]
- García-Fulgueiras, V.; Bado, I.; Mota, M.I.; Robino, L.; Cordeiro, N.F.; Varela, A.; Algorta, G.; Gutkind, G.; Ayala, J.A.; Vignoli, R. Extended-spectrum β-lactamases and plasmid-mediated quinolone resistance in enterobacterial clinical isolates in the paediatric hospital of Uruguay. J. Antimicrob. Chemother. 2011, 66, 1725–1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Huang, N.; Zhou, C.; Lin, Y.; Zhang, Y.; Wang, L.; Zheng, X.; Zhou, T.; Wang, Z. Molecular Mechanisms and Epidemiology of Carbapenem-Resistant Enterobacter cloacae Complex Isolated from Chinese Patients during 2004–2018. Infect. Drug Resist. 2021, 14, 3647–3658. [Google Scholar] [CrossRef] [PubMed]
- Annavajhala, M.K.; Gomez-Simmonds, A.; Uhlemann, A.C. Multidrug-Resistant Enterobacter cloacae Complex Emerging as a Global, Diversifying Threat. Front. Microbiol. 2019, 10, 44. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Fang, R.; Zhang, Y.; Chen, L.; Huang, N.; Yu, K.; Zhou, C.; Cao, J.; Zhou, T. Characterization of resistance mechanisms of Enterobacter cloacae Complex co-resistant to carbapenem and colistin. BMC Microbiol. 2021, 21, 208. [Google Scholar] [CrossRef]
- Ebomah, K.E.; Okoh, A.I. Enterobacter cloacae harbouring blaNDM-1, blaKPC, and blaOXA-48-like carbapenem-resistant genes isolated from different environmental sources in South Africa. Int. J. Environ. Sci. 2020, 78, 151–164. [Google Scholar] [CrossRef]
- Miftode, I.-L.; Pasare, M.-A.; Miftode, R.-S.; Nastase, E.; Plesca, C.E.; Lunca, C.; Miftode, E.-G.; Timpau, A.-S.; Iancu, L.S.; Dorneanu, O.S. What Doesn’t Kill Them Makes Them Stronger: The Impact of the Resistance Patterns of Urinary Enterobacterales Isolates in Patients from a Tertiary Hospital in Eastern Europe. Antibiotics 2022, 11, 548. [Google Scholar] [CrossRef]
- Brives, C.; Pourraz, J. Phage therapy as a potential solution in the fight against AMR: Obstacles and possible futures. Palgrave Commun. 2020, 6, 100. [Google Scholar] [CrossRef]
- Hyman, P. Phages for Phage Therapy: Isolation, Characterization, and Host Range Breadth. Pharmaceuticals 2019, 12, 35. [Google Scholar] [CrossRef] [Green Version]
- Nale, J.Y.; Clokie, M.R. Preclinical data and safety assessment of phage therapy in humans. Curr. Opin. Biotechnol. 2021, 68, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Slopek, S.; Durlakowa, I.; Weber-Dabrowska, B.; Dabrowski, M.; Kucharewicz-Krukowska, A. Results of bacteriophage treatment of suppurative bacterial infections. III. Detailed evaluation of the results obtained in further 150 cases. Arch. Immunol. Ther. Exp. 1984, 32, 317–335. [Google Scholar]
- Gratia, A. Des relations numeriques entre bacteries lysogenes et particles de bacteriophage. Ann. Inst. Pasteur 1936, 57, 652–676. [Google Scholar]
- Adams, M.H. Enumeration of bacteriophage particles. In The Bacteriophages; Inter Science Publ.: New York, NY, USA, 1959. [Google Scholar]
- Kropinski, A.M.; Mazzocco, A.; Waddell, T.E.; Lingohr, E.; Johnson, R.P. Enumeration of bacteriophages by double agar overlay plaque assay. Methods Mol. Biol. 2009, 501, 69–76. [Google Scholar]
- Ács, N.; Gambino, M.; Brøndsted, L. Bacteriophage Enumeration and Detection Methods. Front. Microbiol. 2020, 11, 594868. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.; Kim, S.W.; Kim, S.G.; Kang, J.W.; Jung, W.J.; Lee, S.B.; Lee, Y.M.; Giri, S.S.; Chi, C.; Park, S.C. The Characterization of a Novel Phage, pPa_SNUABM_DT01, Infecting Pseudomonas aeruginosa. Microorganisms 2021, 9, 2040. [Google Scholar] [CrossRef]
- Laforêt, F.; Antoine, C.; Blasdel Reuter, B.; Detilleux, J.; Pirnay, J.-P.; Brisse, S.; Fall, A.; Duprez, J.-N.; Delcenserie, V.; Thiry, D. In Vitro and In Vivo Assessments of Two Newly Isolated Bacteriophages against an ST13 Urinary Tract Infection Klebsiella pneumoniae. Viruses 2022, 14, 1079. [Google Scholar] [CrossRef]
- Necel, A.; Bloch, S.; Nejman-Faleńczyk, B.; Grabski, M.; Topka, G.; Dydecka, A.; Kosznik-Kwaśnicka, K.; Grabowski, Ł.; Jurczak-Kurek, A.; Wołkowicz, T.; et al. Characterization of a bacteriophage, vB_Eco4M-7, that effectively infects many Escherichia coli O157 strains. Sci. Rep. 2020, 10, 3743. [Google Scholar] [CrossRef]
- Kropinski, A.M. Measurement of the rate of attachment of bacteriophage to cells. In Bacteriophages. Methods in Molecular Biology; Clokie, M.R., Kropinski, A.M., Eds.; Humana Press: Totowa, NJ, USA, 2009; Volume 501, pp. 151–155. [Google Scholar]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [Green Version]
- Antipov, D.; Korobeynikov, A.; McLean, J.S.; Pevzner, P.A. hybridSPAdes: An algorithm for hybrid assembly of short and long reads. Bioinformatics 2016, 32, 1009–1015. [Google Scholar] [CrossRef] [Green Version]
- Prjibelski, A.D.; Vasilinetc, I.; Bankevich, A.; Gurevich, A.; Krivosheeva, T.; Nurk, S.; Pham, S.; Korobeynikov, A.; Lapidus, A.; Pevzner, P.A. ExSPAnder: A universal repeat resolver for DNA fragment assembly. Bioinformatics 2014, 30, i293–i301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vasilinetc, I.; Prjibelski, A.D.; Gurevich, A.; Korobeynikov, A.; Pevzner, P.A. Assembling short reads from jumping libraries with large insert sizes. Bioinformatics 2015, 31, 3262–3268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef] [Green Version]
- Nurk, S.; Bankevich, A.; Antipov, D.; Gurevich, A.; Korobeynikov, A.; Lapidus, A.; Prjibelsky, A.; Pyshkin, A.; Sirotkin, A.; Sirotkin, Y.; et al. Assembling Genomes and Mini-metagenomes from Highly Chimeric Reads. In Research in Computational Molecular Biology; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2013; Volume 7821, pp. 158–170. [Google Scholar]
- Cuccuru, G.; Orsini, M.; Pinna, A.; Sbardellati, A.; Soranzo, N.; Travaglione, A.; Uva, P.; Zanetti, G.; Fotia, G. Orione, a web-based framework for NGS analysis in microbiology. Bioinformatics 2014, 30, 1928–1929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seemann, T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; O’Neill, K.R.; Haft, D.H.; DiCuccio, M.; Chetvernin, V.; Badretdin, A.; Coulouris, G.; Chitsaz, F.; Derbyshire, M.K.; Durkin, A.S.; et al. RefSeq: Expanding the Prokaryotic Genome Annotation Pipeline reach with protein family model curation. Nucleic Acids Res. 2021, 49, D1020–D1028. [Google Scholar] [CrossRef]
- Haft, D.H.; DiCuccio, M.; Badretdin, A.; Brover, V.; Chetvernin, V.; O’Neill, K.; Li, W.; Chitsaz, F.; Derbyshire, M.K.; Gonzales, N.R.; et al. RefSeq: An update on prokaryotic genome annotation and curation. Nucleic Acids Res. 2018, 46, D851–D860. [Google Scholar] [CrossRef]
- Tatusova, T.; DiCuccio, M.; Badretdin, A.; Chetvernin, V.; Nawrocki, E.P.; Zaslavsky, L.; Lomsadze, A.; Pruitt, K.D.; Borodovsky, M.; Ostell, J. NCBI prokaryotic genome annotation pipeline. Nucleic Acids Res. 2016, 44, 6614–6624. [Google Scholar] [CrossRef]
- Kearse, M.; Moir, R.; Wilson, A.; Stones-Havas, S.; Cheung, M.; Sturrock, S.; Buxton, S.; Cooper, A.; Markowitz, S.; Duran, C.; et al. Geneious Basic: An integrated and extendable desktop software platform for the organization and analysis of sequence data. Bioinformatics 2012, 28, 1647–1649. [Google Scholar] [CrossRef]
- Darling, A.E.; Mau, B.; Perna, N.T. progressiveMauve: Multiple genome alignment with gene gain, loss and rearrangement. PLoS ONE 2010, 5, e11147. [Google Scholar] [CrossRef] [Green Version]
- Grant, C.E.; Bailey, T.L. XSTREME: Comprehensive motif analysis of biological sequence datasets. bioRxiv 2021. [Google Scholar] [CrossRef]
- Turner, D.; Adriaenssens, E.M.; Tolstoy, I.; Kropinski, A.M. Phage Annotation Guide: Guidelines for Assembly and High-Quality Annotation. Phage 2021, 2, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, H.W. Bacteriophage classification. In Bacteriophages: Biology and Applications; Kutter, E., Sulakvelidze, A., Eds.; CRC Press: Boca Raton, FL, USA, 2005; pp. 67–89. [Google Scholar]
- Ackermann, H.W. Bacteriophage electron microscopy. Adv. Virus Res. 2012, 82, 1–32. [Google Scholar] [PubMed]
- Turner, D.; Kropinski, A.M.; Adriaenssens, E.M. A Roadmap for Genome-Based Phage Taxonomy. Viruses 2021, 13, 506. [Google Scholar] [CrossRef] [PubMed]
- Alcock, B.P.; Raphenya, A.R.; Lau, T.T.Y.; Tsang, K.K.; Bouchard, M.; Edalatmand, A.; Huynh, W.; Nguyen, A.V.; Cheng, A.A.; Liu, S.; et al. CARD 2020: Antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 2020, 48, D517–D525. [Google Scholar] [CrossRef]
- Schoch, C.L.; Ciufo, S.; Domrachev, M.; Hotton, C.L.; Kannan, S.; Khovanskaya, R.; Leipe, D.; Mcveigh, R.; O’Neill, K.; Robbertse, B.; et al. NCBI Taxonomy: A comprehensive update on curation, resources and tools. Database 2020, 2020, baaa062. [Google Scholar] [CrossRef]
- ICTV Taxonomy. Available online: https://ictv.global/taxonomy/ (accessed on 26 May 2022).
- Lefkowitz, E.J.; Dempsey, D.M.; Hendrickson, R.C.; Orton, R.J.; Siddell, S.G.; Smith, D.B. Virus taxonomy: The database of the International Committee on Taxonomy of Viruses (ICTV). Nucleic Acids Res. 2018, 46, D708–D717. [Google Scholar] [CrossRef] [Green Version]
- ICTV Proposal. Available online: https://talk.ictvonline.org/ictv/proposals/2021.082B.A.v1.Tevens_new_families.zip (accessed on 26 May 2022).
- Suh, G.A.; Lodise, T.P.; Tamma, P.D.; Knisely, J.M.; Alexander, J.; Aslam, S.; Barton, K.D.; Bizzell, E.; Totten, K.M.C.; Campbell, J.; et al. Antibacterial Resistance Leadership Group. Considerations for the Use of Phage Therapy in Clinical Practice. Antimicrob. Agents Chemother. 2022, 66, e02071-21. [Google Scholar] [CrossRef]
- Finney, A.G.; Perry, J.M.; Evans, D.R.; Westbrook, K.J.; McElheny, C.L.; Iovleva, A.; Doi, Y.; Shields, R.K.; van Tyne, D. Isolation and Characterization of Lytic Bacteriophages Targeting Diverse Enterobacter spp. Clinical Isolates. Ther. Appl. Res. 2022, 3, 50–58. [Google Scholar] [CrossRef]
- Wang, K.; Tamayo, M.G.; Penner, T.V.; Cook, B.W.M.; Court, D.A.; Theriault, S.S. Characterization of the Enterobacter Phage vB_EclM_CIP9. Microbiol. Resour. Announc. 2020, 9, e01600-19. [Google Scholar] [CrossRef] [Green Version]
- Asif, M.; Naseem, H.; Alvi, I.A.; Basit, A.; Rehman, S.U. Characterization of a lytic EBP bacteriophage with large size genome against Enterobacter cloacae. APMIS 2021, 129, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Ren, H.; Li, Z.; Li, X.; Wang, L.; Xu, Y. Genome sequence analysis of a novel Enterobacter cloacae phage, Ec_L1, belonging to the genus Eclunavirus. Arch. Virol. 2020, 165, 1929–1932. [Google Scholar] [CrossRef] [PubMed]
- Jeon, M.; Huh, K.; Ko, J.H.; Cho, S.Y.; Huh, H.J.; Lee, N.Y.; Kang, C.I.; Chung, D.R.; Peck, K.R. Difference in the Clinical Outcome of Bloodstream Infections Caused by Klebsiella aerogenes and Enterobacter cloacae Complex. Open Forum Infect. Dis. 2021, 8, ofab390. [Google Scholar] [CrossRef] [PubMed]
- Wesevich, A.; Sutton, G.; Ruffin, F.; Park, L.P.; Fouts, D.E.; Fowler, V.G., Jr.; Thaden, J.T. Newly Named Klebsiella aerogenes (formerly Enterobacter aerogenes) Is Associated with Poor Clinical Outcomes Relative to Other Enterobacter Species in Patients with Bloodstream Infection. J. Clin. Microbiol. 2020, 58, e00582-20. [Google Scholar] [CrossRef] [PubMed]
- Manohar, P.; Tamhankar, A.J.; Lundborg, C.S.; Nachimuthu, R. Therapeutic Characterization and Efficacy of Bacteriophage Cocktails Infecting Escherichia coli, Klebsiella pneumoniae, and Enterobacter Species. Front. Microbiol. 2019, 10, 574. [Google Scholar] [CrossRef] [Green Version]
- Morozova, V.; Jdeed, G.; Kozlova, Y.; Babkin, I.; Tikunov, A.; Tikunova, N. A New Enterobacter cloacae Bacteriophage EC151 Encodes the Deazaguanine DNA Modification Pathway and Represents a New Genus within the Siphoviridae Family. Viruses 2021, 13, 1372. [Google Scholar] [CrossRef]
- Addablah, A.Y.A.; Kakou-Ngazoa, S.; Akpa, E.E.; M’Bourou Ndombi, F.; Adioumani, E.; Koudou, A.; N’Golo, D.C.; Sina, M.K.; Kouassi, S.K.; Aoussi, S.; et al. Investigation of Phages Infecting Escherichia coli Strains B and C, and Enterobacter cloacae in Sewage and Ebrié Lagoon, Côte d’Ivoire. PHAGE 2021, 2, 104–111. [Google Scholar]
- Jamal, M.; Andleeb, S.; Jalil, F.; Imran, M.; Nawaz, M.A.; Hussain, T.; Ali, M.; Ur Rahman, S.; Das, C.R. Isolation, characterization and efficacy of phage MJ2 against biofilm forming multi-drug resistant Enterobacter cloacae. Folia Microbiol. 2019, 64, 101–111. [Google Scholar] [CrossRef]
- Ross, A.; Ward, S.; Hyman, P. More Is Better: Selecting for Broad Host Range Bacteriophages. Front. Microbiol. 2016, 7, 1352. [Google Scholar] [CrossRef] [Green Version]
- Gibson, S.B.; Green, S.I.; Liu, C.G.; Salazar, K.C.; Clark, J.R.; Terwilliger, A.L.; Kaplan, H.B.; Maresso, A.W.; Trautner, B.W.; Ramig, R.F. Constructing and Characterizing Bacteriophage Libraries for Phage Therapy of Human Infections. Front. Microbiol. 2019, 10, 2537. [Google Scholar] [CrossRef] [Green Version]
- Nair, A.; Vyawahare, R.; Khairnar, K. Characterization of a novel, biofilm dispersing, lytic bacteriophage against drug-resistant Enterobacter cloacae. J. Appl. Microbiol. 2021, 132, 2721–2732. [Google Scholar] [CrossRef] [PubMed]
- Topka, G.; Bloch, S.; Nejman-Faleńczyk, B.; Gąsior, T.; Jurczak-Kurek, A.; Necel, A.; Dydecka, A.; Richert, M.; Węgrzyn, G.; Węgrzyn, A. Characterization of Bacteriophage vB-EcoS-95, Isolated From Urban Sewage and Revealing Extremely Rapid Lytic Development. Front. Microbiol. 2019, 9, 3326. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.W.; Yuan, L.; Zhou, W.Y.; Mgomi, F.C.; Zhang, Y.S.; Wang, Y.; Zheng, X.F.; Hu, Q.; Gao, L.; Rao, S.Q.; et al. Isolation and genomic characterization of P.A-5, a novel virulent bacteriophage against Enterobacter hormaechei. Microb. Pathog. 2021, 152, 104767. [Google Scholar] [CrossRef] [PubMed]
- Topka-Bielecka, G.; Nejman-Faleńczyk, B.; Bloch, S.; Dydecka, A.; Necel, A.; Węgrzyn, A.; Węgrzyn, G. Phage-Bacteria Interactions in Potential Applications of Bacteriophage vB_EfaS-271 against Enterococcus faecalis. Viruses 2021, 13, 318. [Google Scholar] [CrossRef]
- Abedon, S.T. Phage therapy dosing: The problem(s) with multiplicity of infection (MOI). Bacteriophage 2016, 6, e1220348. [Google Scholar] [CrossRef] [Green Version]
- Duyvejonck, H.; Merabishvili, M.; Vaneechoutte, M.; de Soir, S.; Wright, R.; Friman, V.P.; Verbeken, G.; de Vos, D.; Pirnay, J.P.; van Mechelen, E.; et al. Evaluation of the Stability of Bacteriophages in Different Solutions Suitable for the Production of Magistral Preparations in Belgium. Viruses 2021, 13, 865. [Google Scholar] [CrossRef]
- Kering, K.K.; Zhang, X.; Nyaruaba, R.; Yu, J.; Wei, H. Application of Adaptive Evolution to Improve the Stability of Bacteriophages during Storage. Viruses 2020, 12, 423. [Google Scholar] [CrossRef] [Green Version]
- Jończyk, E.; Kłak, M.; Międzybrodzki, R.; Górski, A. The influence of external factors on bacteriophages. Folia Microbiol. 2011, 56, 191–200. [Google Scholar] [CrossRef] [Green Version]
- Thompson, S. Isolation and Characterization of Bacteriophages Infecting Enterobacter cloacae to Reduce Bloater Defect in Cucumber Fermentations. Master’s Thesis, Kennesaw State University, Kennesaw, GA, USA, 2020. [Google Scholar]
- Kuo, S.H.; Shen, C.J.; Shen, C.F.; Cheng, C.M. Role of pH Value in Clinically Relevant Diagnosis. Diagnostics 2020, 10, 107. [Google Scholar] [CrossRef] [Green Version]
- Beasley, D.E.; Koltz, A.M.; Lambert, J.E.; Fierer, N.; Dunn, R.R. The Evolution of Stomach Acidity and Its Relevance to the Human Microbiome. PLoS ONE 2015, 10, e0134116. [Google Scholar]
- Sánchez-Clemente, R.; Igeño, M.I.; Población, A.G.; Guijo, M.I.; Merchán, F.; Blasco, R. Study of pH Changes in Media during Bacterial Growth of Several Environmental Strains. Proceedings 2018, 2, 1297. [Google Scholar]
- Zhao, J.; Zhang, Z.; Tian, C.; Chen, X.; Hu, L.; Wei, X.; Li, H.; Lin, W.; Jiang, A.; Feng, R.; et al. Characterizing the Biology of Lytic Bacteriophage vB_EaeM_φEap-3 Infecting Multidrug-Resistant Enterobacter aerogenes. Front. Microbiol. 2019, 10, 420. [Google Scholar] [CrossRef] [PubMed]
- Li, E.; Wei, X.; Ma, Y.; Yin, Z.; Li, H.; Lin, W.; Wang, X.; Li, C.; Shen, Z.; Zhao, R.; et al. Isolation and characterization of a bacteriophage phiEap-2 infecting multidrug resistant Enterobacter aerogenes. Sci. Rep. 2016, 6, 28338. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, K.A.; Abbas, Z.; ur Rehman, S. Isolation and characterization of lytic phages TSE1-3 against Enterobacter cloacae. Open Life Sci. 2016, 11, 287–292. [Google Scholar] [CrossRef] [Green Version]
- Montso, P.K.; Mlambo, V.; Ateba, C.N. Characterization of Lytic Bacteriophages Infecting Multidrug-Resistant Shiga Toxigenic Atypical Escherichia coli O177 Strains Isolated from Cattle Feces. Front. Public Health 2019, 7, 355. [Google Scholar] [CrossRef] [PubMed]
- Wójcicki, M.; Średnicka, P.; Błażejak, S.; Gientka, I.; Kowalczyk, M.; Emanowicz, P.; Świder, O.; Sokołowska, B.; Juszczuk-Kubiak, E. Characterization and Genome Study of Novel Lytic Bacteriophages against Prevailing Saprophytic Bacterial Microflora of Minimally Processed Plant-Based Food Products. Int. J. Mol. Sci. 2021, 22, 12460. [Google Scholar] [CrossRef]
- Chen, C.W.; Yuan, L.; Zhang, Y.S.; Mgomi, F.C.; Wang, Y.; Yang, Z.Q.; Jiao, X.A. Comparison of biological and genomic characteristics of five virulent bacteriophages against Enterobacter hormaechei. Microb. Pathog. 2022, 162, 105375. [Google Scholar] [CrossRef]
- Tobin, E.; Brenner, S. Nanotechnology Fundamentals Applied to Clinical Infectious Diseases and Public Health. Open Forum Infect. Dis. 2021, 8, ofab583. [Google Scholar] [CrossRef]
- Durán, N.; Durán, M.; de Jesus, M.B.; Seabra, A.B.; Fávaro, W.J.; Nakazato, G. Silver nanoparticles: A new view on mechanistic aspects on antimicrobial activity. Nanomedicine 2016, 12, 789–799. [Google Scholar] [CrossRef]
- Roe, D.; Karandikar, B.; Bonn-Savage, N.; Gibbins, B.; Roullet, J.B. Antimicrobial surface functionalization of plastic catheters by silver nanoparticles. J. Antimicrob. Chemother. 2008, 61, 869–876. [Google Scholar] [CrossRef]
- Thomas, R.; Soumya, K.R.; Mathew, J.; Radhakrishnan, E.K. Inhibitory effect of silver nanoparticle fabricated urinary catheter on colonization efficiency of Coagulase Negative Staphylococci. J. Photochem. Photobiol. B 2015, 149, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Prateeksha, P.; Bajpai, R.; Rao, C.V.; Upreti, D.K.; Barik, S.K.; Singh, B.N. Chrysophanol-Functionalized Silver Nanoparticles for Anti-Adhesive and Anti-Biofouling Coatings to Prevent Urinary Catheter-Associated Infections. ACS Appl. Nano Mater. 2021, 4, 1512–1528. [Google Scholar] [CrossRef]
- Ermini, M.L.; Voliani, V. Antimicrobial Nano-Agents: The Copper Age. ACS Nano 2021, 15, 6008–6029. [Google Scholar] [CrossRef] [PubMed]
- Crisan, M.C.; Teodora, M.; Lucian, M. Copper Nanoparticles: Synthesis and Characterization, Physiology, Toxicity and Antimicrobial Applications. Appl. Sci. 2021, 12, 141. [Google Scholar] [CrossRef]
- Richter, Ł.; Paszkowska, K.; Cendrowska, U.; Olgiati, F.; Silva, P.J.; Gasbarri, M.; Guven, Z.P.; Paczesny, J.; Stellacci, F. Broad-spectrum nanoparticles against bacteriophage infections. Nanoscale 2021, 13, 18684–18694. [Google Scholar] [CrossRef]
- Sinclair, T.R.; van den Hengel, S.K.; Raza, B.G.; Rutjes, S.A.; de Roda Husman, A.M.; Peijnenburg, W.J.G.M.; Roesink, H.E.D.W.; de Vos, W.M. Surface chemistry-dependent antiviral activity of silver nanoparticles. Nanotechnology 2021, 32, 365101. [Google Scholar] [CrossRef]
- Abdelsattar, A.S.; Nofal, R.; Makky, S.; Safwat, A.; Taha, A.; El-Shibiny, A. The Synergistic Effect of Biosynthesized Silver Nanoparticles and Phage ZCSE2 as a Novel Approach to Combat Multidrug-Resistant Salmonella enterica. Antibiotics 2021, 10, 678. [Google Scholar] [CrossRef]
- Tomat, D.; Balagué, C.; Aquili, V.; Verdini, R.; Quiberoni, A. Resistance of phages lytic to pathogenic Escherichia coli to sanitisers used by the food industry and in home settings. Int. J. Food Sci. Technol. 2018, 53, 533–540. [Google Scholar] [CrossRef]
- Sommer, J.; Trautner, C.; Witte, A.K.; Fister, S.; Schoder, D.; Rossmanith, P.; Mester, P.J. Don’t Shut the Stable Door after the Phage Has Bolted-The Importance of Bacteriophage Inactivation in Food Environments. Viruses 2019, 11, 468. [Google Scholar] [CrossRef] [Green Version]
- Teklu, D.S.; Negeri, A.A.; Legese, M.H.; Bedada, T.L.; Woldemariam, H.K.; Tullu, K.D. Extended-spectrum beta-lactamase production and multi-drug resistance among Enterobacteriaceae isolated in Addis Ababa, Ethiopia. Antimicrob. Resist. Infect. Control. 2019, 8, 39. [Google Scholar] [CrossRef]
- Osthoff, M.; Mcguinness, S.L.; Wagen, A.Z.; Eisen, D.P. Urinary tract infections due to extended-spectrum beta-lactamase-producing Gram-negative bacteria: Identification of risk factors and outcome predictors in an Australian tertiary referral hospital. Int. J. Infect. Dis. 2015, 34, 79–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alevizakos, M.; Nasioudis, D.; Mylonakis, E. Urinary tract infections caused by ESBL-producing Enterobacteriaceae in renal transplant recipients: A systematic review and meta-analysis. Transpl. Infect. Dis. 2017, 19, e12759. [Google Scholar] [CrossRef] [PubMed]
- Castanheira, M.; Simner, P.J.; Bradford, P.A. Extended-spectrum β-lactamases: An update on their characteristics, epidemiology and detection. JAC Antimicrob. Resist. 2021, 3, dlab092. [Google Scholar] [CrossRef]
- Sybesma, W.; Zbinden, R.; Chanishvili, N.; Kutateladze, M.; Chkhotua, A.; Ujmajuridze, A.; Mehnert, U.; Kessler, T.M. Bacteriophages as Potential Treatment for Urinary Tract Infections. Front. Microbiol. 2016, 7, 465. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.; Pereira, C.; Santos, L.; Klumpp, J.; Almeida, A. Potential of phage cocktails in the inactivation of Enterobacter cloacae--An in vitro study in a buffer solution and in urine samples. Virus Res. 2016, 211, 199–208. [Google Scholar] [CrossRef]
- Chegini, Z.; Khoshbayan, A.; Vesal, S.; Moradabadi, A.; Hashemi, A.; Shariati, A. Bacteriophage therapy for inhibition of multi drug-resistant uropathogenic bacteria: A narrative review. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 30. [Google Scholar] [CrossRef]
- Malik, S.; Sidhu, P.K.; Rana, J.S.; Nehra, K. Managing urinary tract infections through phage therapy: A novel approach. Folia Microbiol. 2020, 65, 217–231. [Google Scholar] [CrossRef]
- De Miguel, T.; Rama, J.L.R.; Sieiro, C.; Sánchez, S.; Villa, T.G. Bacteriophages and Lysins as Possible Alternatives to Treat Antibiotic-Resistant Urinary Tract Infections. Antibiotics 2020, 9, 466. [Google Scholar] [CrossRef]
- Leitner, L.; Sybesma, W.; Chanishvili, N.; Goderdzishvili, M.; Chkhotua, A.; Ujmajuridze, A.; Schneider, M.P.; Sartori, A.; Mehnert, U.; Bachmann, L.M.; et al. Bacteriophages for treating urinary tract infections in patients undergoing transurethral resection of the prostate: A randomized, placebo-controlled, double-blind clinical trial. BMC Urol. 2017, 17, 90. [Google Scholar] [CrossRef] [Green Version]
- Leitner, L.; Ujmajuridze, A.; Chanishvili, N.; Goderdzishvili, M.; Chkonia, I.; Rigvava, S.; Chkhotua, A.; Changashvili, G.; McCallin, S.; Schneider, M.P.; et al. Intravesical bacteriophages for treating urinary tract infections in patients undergoing transurethral resection of the prostate: A randomised, placebo-controlled, double-blind clinical trial. Lancet Infect. Dis. 2021, 21, 427–436. [Google Scholar] [CrossRef]
- Górski, A.; Borysowski, J.; Międzybrodzki, R. Phage Therapy: Towards a Successful Clinical Trial. Antibiotics 2020, 9, 827. [Google Scholar] [CrossRef] [PubMed]
- Terwilliger, A.; Clark, J.; Karris, M.; Hernandez-Santos, H.; Green, S.; Aslam, S.; Maresso, A. Phage Therapy Related Microbial Succession Associated with Successful Clinical Outcome for a Recurrent Urinary Tract Infection. Viruses 2021, 13, 2049. [Google Scholar] [CrossRef] [PubMed]





| Strain Number | Name of Bacterial Strain | Source of Isolation |
|---|---|---|
| 1. | Enterobacter cloacae 30345 | fistula |
| 2. | Enterobacter cloacae (ESBL+) 29796 | urine |
| 3. | Enterobacter cloacae 3344 | urethra |
| 4. | Enterobacter cloacae 3345 | foreskin |
| 5. | Enterobacter cloacae 30697 | semen |
| 6. | Enterobacter cloacae 30528 | pus |
| 7. | Enterobacter cloacae 30103 | pus |
| 8. | Enterobacter cloacae 29916 | pus |
| 9. | Enterobacter cloacae (ESBL+) 29779 | pus |
| 10. | Enterobacter cloacae (ESBL+) 29731 | sore |
| 11. | Enterobacter cloacae 30642 | foot ulcer |
| 12. | Enterobacter cloacae (ESBL+) 30256 | amputation wound swab |
| 13. | Enterobacter cloacae 3354 | ear |
| 14. | Enterobacter cloacae 30612 | ear |
| 15. | Enterobacter cloacae (ESBL+) 30300 | fistula |
| 16. | Enterobacter hormaechei 30165 | discharge from the prostate gland |
| 17. | Enterobacter hormaechei 30426 | urine |
| 18. | Enterobacter hormaechei 30550 | urine |
| 19. | Enterobacter hormaechei (ESBL+) 29753 | pus |
| 20. | Enterobacter kobei 30367 | sore |
| Bacterial Strain | Entb_43 | Entb_45 |
|---|---|---|
| E. cloacae 30345 | CL | SCL |
| E. cloacae 29796 | CL | CL |
| E. cloacae 3344 | - | - |
| E. cloacae 3345 | - | - |
| E. cloacae 30697 | - | SCL |
| E. cloacae 30528 | - | ++ |
| E. cloacae 30103 | - | - |
| E. cloacae 29916 | CL | SCL |
| E. cloacae 29779 | SCL | SCL |
| E. cloacae 29731 | OL | ++ |
| E. cloacae 30642 | - | - |
| E. cloacae 30256 | - | - |
| E. cloacae 3354 | - | SCL |
| E. cloacae 30612 | - | - |
| E. cloacae 30300 | CL | SCL |
| E. hormaechei 30165 | - | +++ |
| E. hormaechei 30426 | CL | SCL |
| E. hormaechei 30550 | - | - |
| E. hormaechei 29753 | OL | - |
| E. kobei 30367 | - | ++ |
| E. faecalis 3 | - | - |
| E. faecalis 4 | - | - |
| S. aureus 1 | - | - |
| S. aureus 2 | - | - |
| K. pneumoniae 7 | - | - |
| A. baumannii 703 | - | - |
| A. baumannii 3940 | - | - |
| A. baumannii 1326 | - | - |
| P. aeruginosa 5 | - | - |
| P. aeruginosa PS735 | - | - |
| E. coli 8 | - | - |
| E. coli 9 | - | - |
| Phage Symbol | Phage ICTV Name | Host Strain | Species Specificity | Source of Isolation | Lytic Spectrum |
|---|---|---|---|---|---|
| Entb_43 | Enterobacter phage vB_EclM-43 | E. cloacae 30345 | E. cloacae, E. hormaechei | water sample from river (Thames, London, UK)—raw sample | 8 of 20 strains (40%) |
| Entb_45 | Enterobacter phage vB_EclM-45 | E. cloacae 29796 | E. cloacae, E. hormaechei, E. kobei | water sample from river (Fatima, Portugal)—raw sample | 12 of 20 strains (60%) |
| Phage Symbol | Family | Morphotype | Total Dimension [nm] | Capsid Length [nm] | Capsid Width [nm] | Capsid Diagonal [nm] | Tail Length [nm] | Tail Width [nm] | Base Plate Width [nm] |
|---|---|---|---|---|---|---|---|---|---|
| Entb_43 | Myoviridae | A2 | 223.4 | 116.7 | 82.1 | 103.9 | 106.7 | 21.2 | 33 |
| Entb_45 | Myoviridae | A2 | 220.9 | 113.6 | 89.8 | 107.3 | 107.3 | 20.3 | 33.7 |
| Phage Name | MOI | Host Bacteria [CFU/mL] | Phage Titer [PFU/mL] | Phage Titer after Overnight Incubation [PFU/mL] |
|---|---|---|---|---|
| Entb_43 | 0.001 | 106 | 103 | 6.33 × 109 |
| 0.01 | 106 | 104 | 6.93 × 109 | |
| 0.1 | 106 | 105 | 3.20 × 109 | |
| 1 | 106 | 106 | 2.87 × 109 | |
| 10 | 106 | 107 | 1.19 × 108 | |
| 100 | 106 | 108 | 7.13 × 108 | |
| 1000 | 106 | 109 | 8.80 × 108 | |
| Entb_45 | 0.001 | 106 | 103 | 4.93 × 109 |
| 0.01 | 106 | 104 | 2.67 × 109 | |
| 0.1 | 106 | 105 | 1.49 × 109 | |
| 1 | 106 | 106 | 5.73 × 108 | |
| 10 | 106 | 107 | 7.73 × 107 | |
| 100 | 106 | 108 | 3.38 × 107 | |
| 1000 | 106 | 109 | 5.53 × 107 |
| Adsorption Rate Constant [mL/min] | |
|---|---|
| Entb_43 | 4.92 × 10−10 |
| Entb_45 | 9.29 × 10−10 |
| Phage Name | Genome Size [bp] | Start Codons [%] | Coverage | Genes | GC Content [%] |
|---|---|---|---|---|---|
| Enterobacter phage Entb_43 | 174 681 | ATG: 95.3 GTG: 2.90 TTG: 1.81 | 902 | positive strand: 240 negative strand: 41 | 39.7 |
| Enterobacter phage Entb_45 | 172 771 | ATG: 97.8 GTG: 1.48 TTG: 0.74 | 661 | positive strand: 230 negative strand: 43 | 40 |
| Phage Entb_43 | Phage Entb_45 | |||||||
|---|---|---|---|---|---|---|---|---|
| 5 min | 10 min | 20 min | 30 min | 5 min | 10 min | 20 min | 30 min | |
| 10% dish soap | 77.8 % | 78.3 % | 83.9 % | 77.8 % | 74.3 % | 75.7 % | 93.3 % | 74.3 % |
| 10% liquid soap | 83.3 % | 79.4 % | 97.2 % | 77.8 % | 80.6 % | 86.2 % | 82.9 % | 80 % |
| disinfectant (1) (diluted 2×) | 65.3 % | 41.4 % | 17 % | 7.8 % | 15.6 % | 2.1 % | 0.1 % | 0.01 % |
| 10% hand wash gel | 138.9 % | 107 % | 126.4 % | 87.8 % | 129.5 % | 112 % | 81.7 % | 85.4 % |
| skin disinfectant (2) (diluted 2×) | 120.6 % | 130.6 % | 87.5 % | 67.1 % | 61 % | 80 % | 68.6 % | 80 % |
| 70% ethanol | 57.5 % | 56.7 % | 35.8 % | 27 % | 21 % | 7.7 % | 8.4 % | 3 % |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cieślik, M.; Harhala, M.; Orwat, F.; Dąbrowska, K.; Górski, A.; Jończyk-Matysiak, E. Two Newly Isolated Enterobacter-Specific Bacteriophages: Biological Properties and Stability Studies. Viruses 2022, 14, 1518. https://doi.org/10.3390/v14071518
Cieślik M, Harhala M, Orwat F, Dąbrowska K, Górski A, Jończyk-Matysiak E. Two Newly Isolated Enterobacter-Specific Bacteriophages: Biological Properties and Stability Studies. Viruses. 2022; 14(7):1518. https://doi.org/10.3390/v14071518
Chicago/Turabian StyleCieślik, Martyna, Marek Harhala, Filip Orwat, Krystyna Dąbrowska, Andrzej Górski, and Ewa Jończyk-Matysiak. 2022. "Two Newly Isolated Enterobacter-Specific Bacteriophages: Biological Properties and Stability Studies" Viruses 14, no. 7: 1518. https://doi.org/10.3390/v14071518
APA StyleCieślik, M., Harhala, M., Orwat, F., Dąbrowska, K., Górski, A., & Jończyk-Matysiak, E. (2022). Two Newly Isolated Enterobacter-Specific Bacteriophages: Biological Properties and Stability Studies. Viruses, 14(7), 1518. https://doi.org/10.3390/v14071518






