Transmission of Raccoon-Passaged Chronic Wasting Disease Agent to White-Tailed Deer
Abstract
:1. Introduction
2. Materials and Methods
Ethics Statement
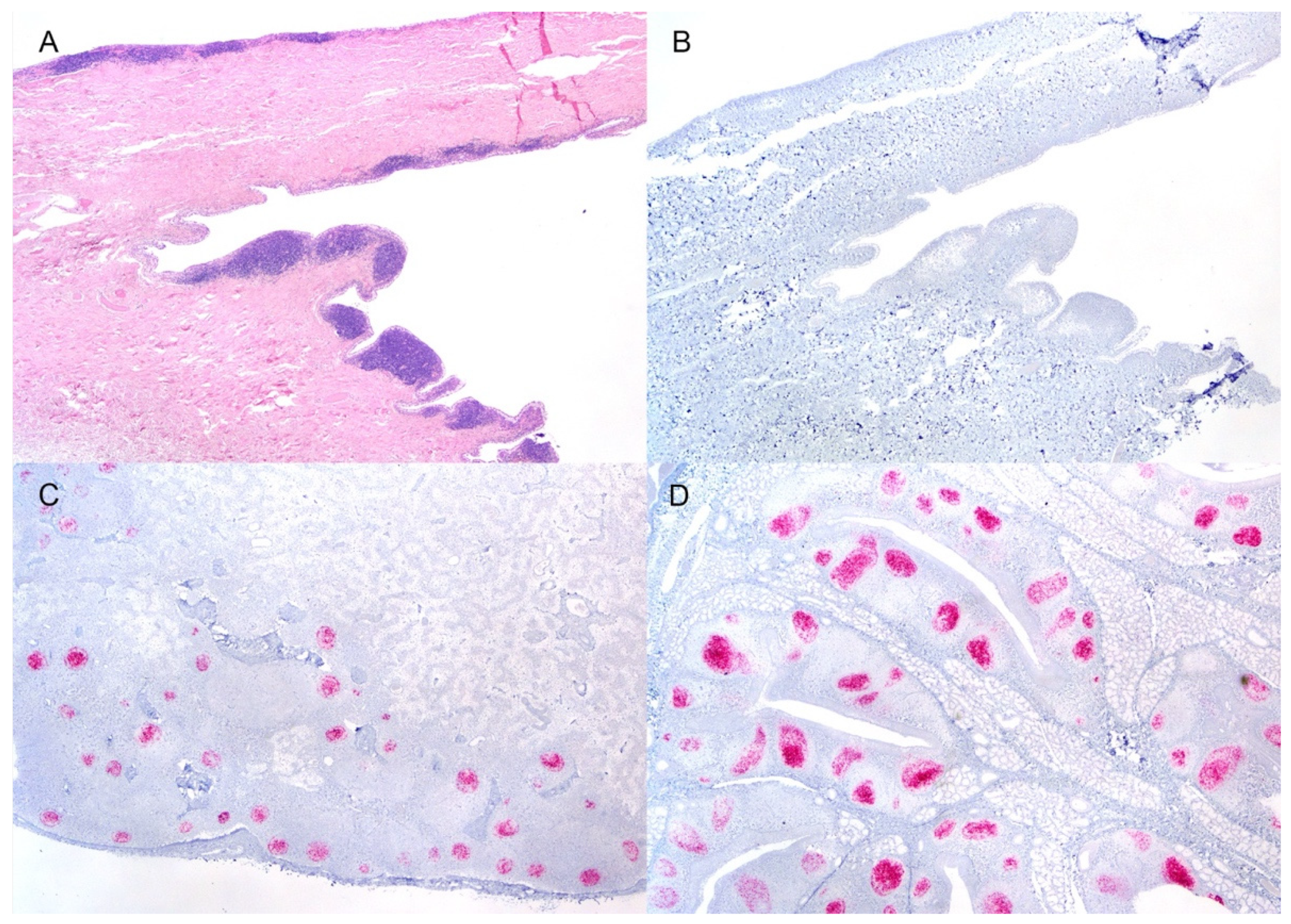
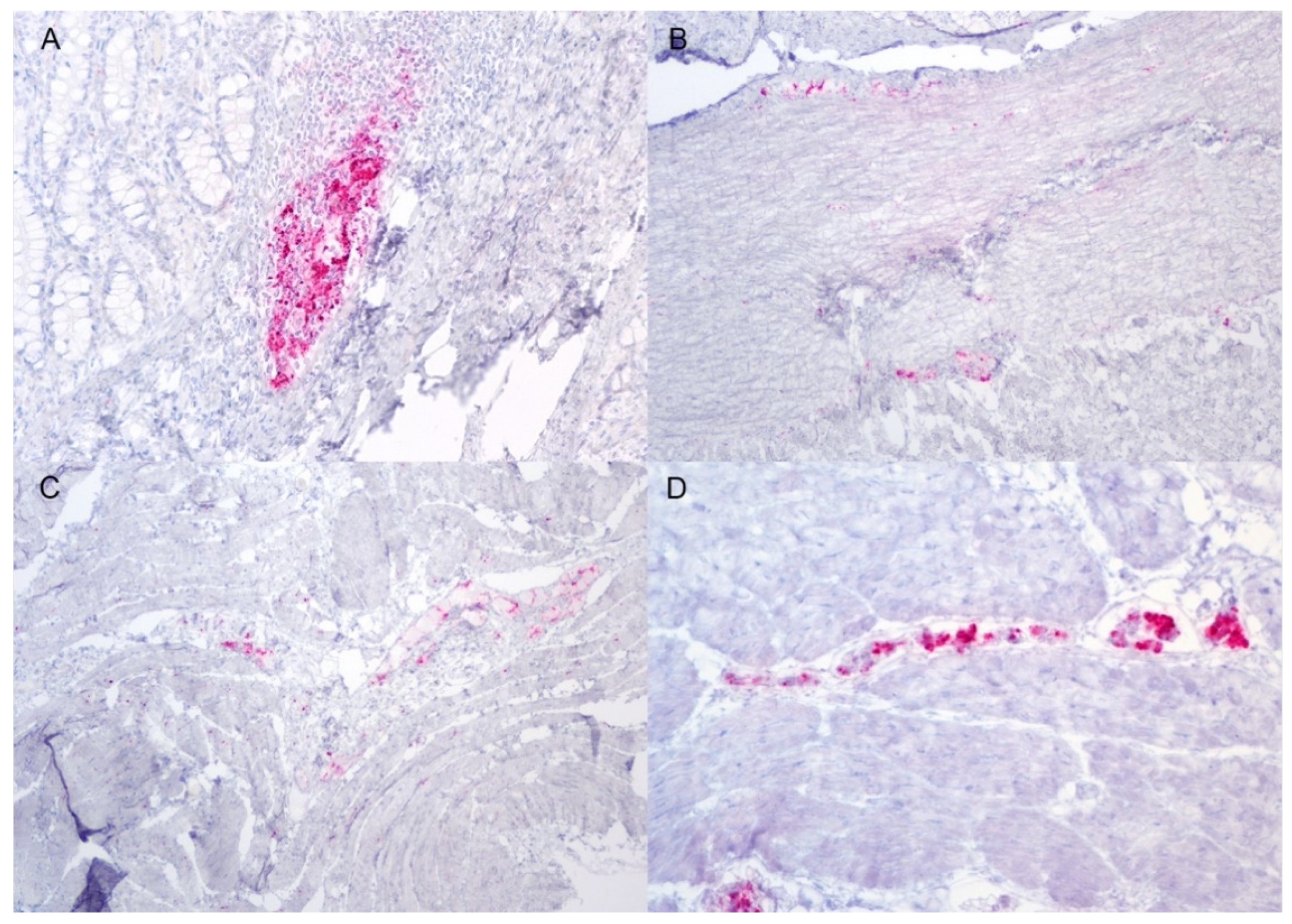
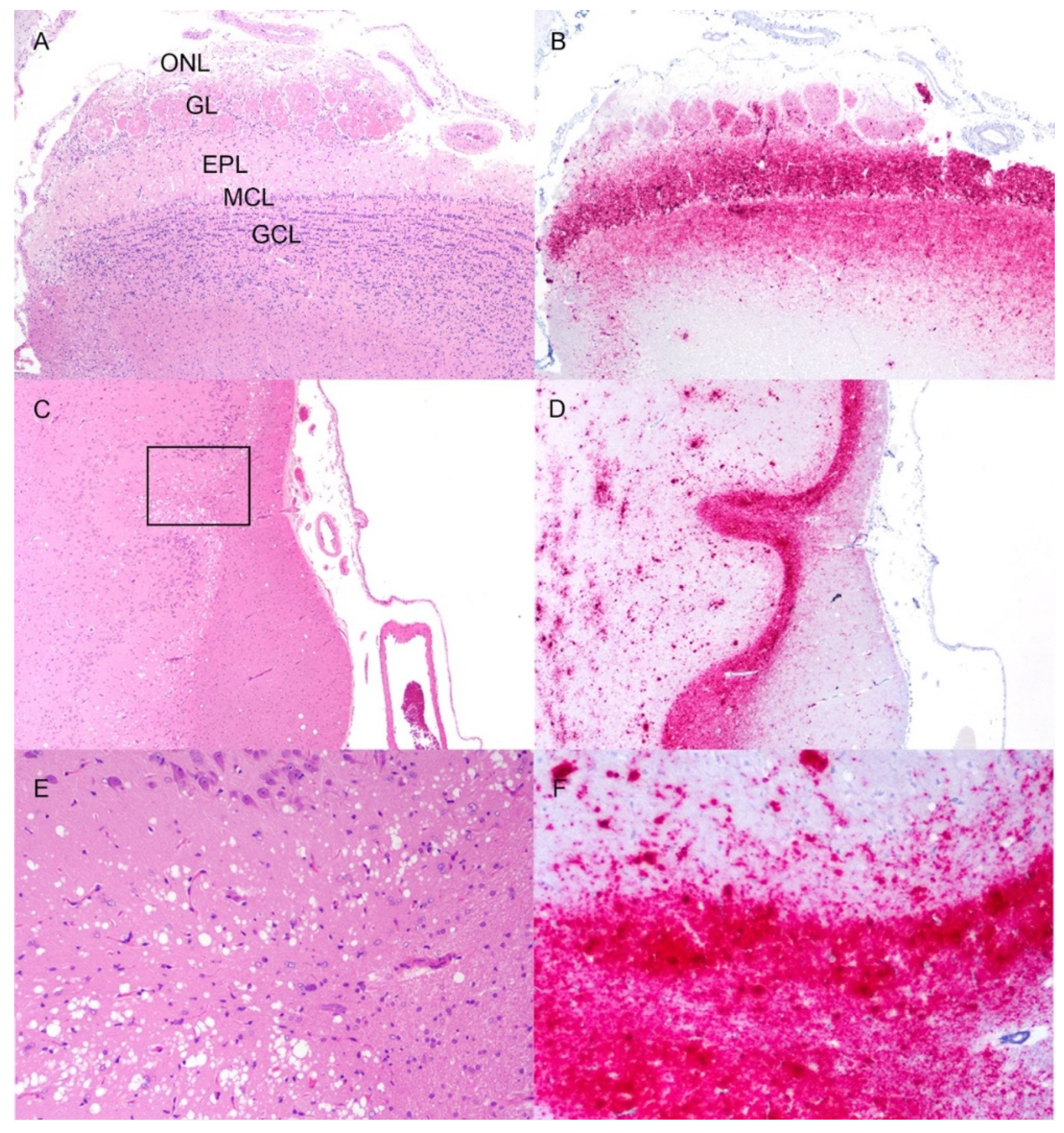
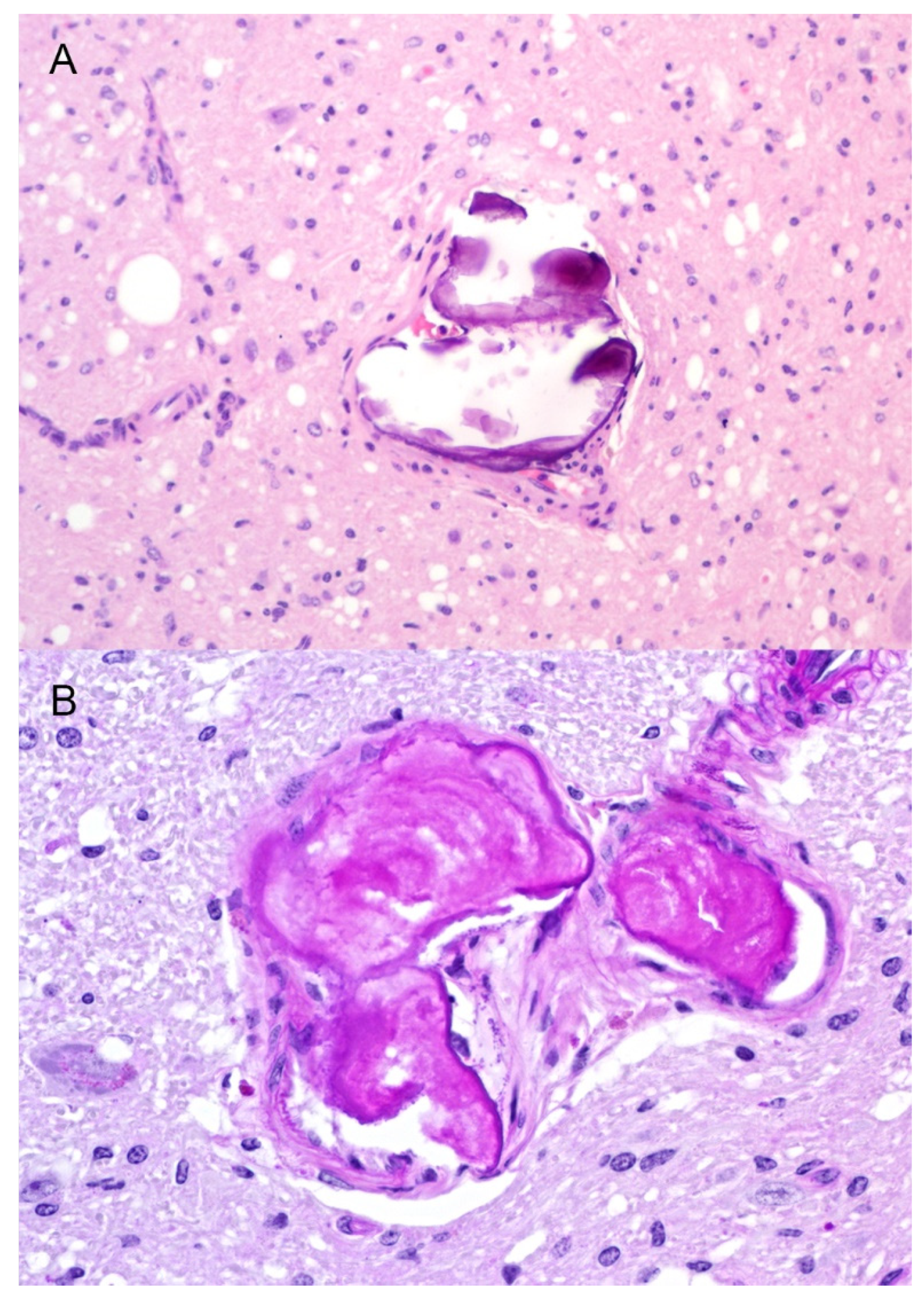
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prusiner, S.B. Novel proteinaceous infectious particles cause scrapie. Science 1982, 216, 136–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prusiner, S.B. Prions. Proc. Natl. Acad. Sci. USA 1998, 95, 13363–13383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, E.S.; Young, S. Spongiform encephalopathies in Cervidae. Rev. Sci. Tech. (Int. Off. Epizoot.) 1992, 11, 551–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richards, B. Expanding Distribution of Chronic Wasting Disease. Available online: https://www.usgs.gov/centers/nwhc/science/expanding-distribution-chronic-wasting-disease (accessed on 25 April 2022).
- Mathiason, C.K.; Powers, J.G.; Dahmes, S.J.; Osborn, D.A.; Miller, K.V.; Warren, R.J.; Mason, G.L.; Hays, S.A.; Hayes-Klug, J.; Seelig, D.M.; et al. Infectious prions in the saliva and blood of deer with chronic wasting disease. Science 2006, 314, 133–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathiason, C.K.; Hays, S.A.; Powers, J.; Hayes-Klug, J.; Langenberg, J.; Dahmes, S.J.; Osborn, D.A.; Miller, K.V.; Warren, R.J.; Mason, G.L.; et al. Infectious prions in pre-clinical deer and transmission of chronic wasting disease solely by environmental exposure. PLoS ONE 2009, 4, e5916. [Google Scholar] [CrossRef] [Green Version]
- Haley, N.J.; Mathiason, C.K.; Carver, S.; Zabel, M.; Telling, G.C.; Hoover, E.A. Detection of chronic wasting disease prions in salivary, urinary, and intestinal tissues of deer: Potential mechanisms of prion shedding and transmission. J. Virol. 2011, 85, 6309–6318. [Google Scholar] [CrossRef] [Green Version]
- Miller, M.W.; Williams, E.S.; Hobbs, N.T.; Wolfe, L.L. Environmental sources of prion transmission in mule deer. Emerg. Infect. Dis. 2004, 10, 1003–1006. [Google Scholar] [CrossRef]
- Osterholm, M.T.; Anderson, C.J.; Zabel, M.D.; Scheftel, J.M.; Moore, K.A.; Appleby, B.S. Chronic Wasting Disease in Cervids: Implications for Prion Transmission to Humans and Other Animal Species. mBio 2019, 10, e01091-19. [Google Scholar] [CrossRef] [Green Version]
- Otero, A.; Velasquez, C.D.; Aiken, J.; McKenzie, D. Chronic wasting disease: A cervid prion infection looming to spillover. Vet. Res. 2021, 52, 115. [Google Scholar] [CrossRef]
- Wang, Z.; Qin, K.; Camacho, M.V.; Cali, I.; Yuan, J.; Shen, P.; Greenlee, J.; Kong, Q.; Mastrianni, J.A.; Zou, W.Q. Generation of human chronic wasting disease in transgenic mice. Acta. Neuropathol. Commun. 2021, 9, 158. [Google Scholar] [CrossRef]
- Moore, S.J.; Smith, J.D.; Richt, J.A.; Greenlee, J.J. Raccoons accumulate PrPSc after intracranial inoculation of the agents of chronic wasting disease or transmissible mink encephalopathy but not atypical scrapie. J. Vet. Diagn. Investig. 2019, 31, 1040638718825290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, S.J.; Carlson, C.M.; Schneider, J.R.; Johnson, C.J.; Greenlee, J.J. Increased Attack Rates and Decreased Incubation Periods in Raccoons with Chronic Wasting Disease Passaged through Meadow Voles. Emerg. Infect. Dis. 2022, 28, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Hamir, A.N.; Kunkle, R.A.; Richt, J.A.; Miller, J.M.; Greenlee, J.J. Experimental transmission of US scrapie agent by nasal, peritoneal, and conjunctival routes to genetically susceptible sheep. Vet. Pathol. 2008, 45, 7–11. [Google Scholar] [CrossRef]
- Cassmann, E.D.; Frese, R.D.; Greenlee, J.J. Second passage of chronic wasting disease of mule deer to sheep by intracranial inoculation compared to classical scrapie. J. Vet. Diagn. Investig. 2021, 33, 10406387211017615. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.J.; Herbst, A.; Duque-Velasquez, C.; Vanderloo, J.P.; Bochsler, P.; Chappell, R.; McKenzie, D. Prion protein polymorphisms affect chronic wasting disease progression. PLoS ONE 2011, 6, e17450. [Google Scholar] [CrossRef] [PubMed]
- Seabury, C.M.; Oldeschulte, D.L.; Bhattarai, E.K.; Legare, D.; Ferro, P.J.; Metz, R.P.; Johnson, C.D.; Lockwood, M.A.; Nichols, T.A. Accurate Genomic Predictions for Chronic Wasting Disease in U.S. White-Tailed Deer. G3 2020, 10, 1433–1441. [Google Scholar] [CrossRef] [Green Version]
- Afanasieva, E.G.; Kushnirov, V.V.; Ter-Avanesyan, M.D. Interspecies transmission of prions. Biochemistry 2011, 76, 1375–1384. [Google Scholar] [CrossRef]
- Davenport, K.A.; Henderson, D.M.; Bian, J.; Telling, G.C.; Mathiason, C.K.; Hoover, E.A. Insights into Chronic Wasting Disease and Bovine Spongiform Encephalopathy Species Barriers by Use of Real-Time Conversion. J. Virol. 2015, 89, 9524–9531. [Google Scholar] [CrossRef] [Green Version]
- Williams, E.S. Chronic wasting disease. Vet. Pathol. 2005, 42, 530–549. [Google Scholar] [CrossRef]
- Rohn, T.T. Corpora Amylacea in Neurodegenerative Diseases: Cause or Effect? Int. J. Neurol. Neurother. 2015, 2, 31. [Google Scholar] [CrossRef]
- Howerth, E.W.; Nemeth, N.M.; Ryser-Degiorgis, M.-P. Chapter 6—Cervidae. In Pathology of Wildlife and Zoo Animals; Terio, K.A., McAloose, D., Leger, J.S., Eds.; Academic Press: Cambridge, MA, USA, 2018; pp. 149–183. [Google Scholar]
- Ferrer, I.; Vidal, N. Chapter 7—Neuropathology of cerebrovascular diseases. In Handbook of Clinical Neurology; Kovacs, G.G., Alafuzoff, I., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; Volume 145, pp. 79–114. [Google Scholar]
- Vandevelde, M.; Higgins, R.J.; Oevermann, A. Veterinary Neuropathology: Essentials of Theory and Practice; Wiley-Blackwell: Oxford, UK, 2012. [Google Scholar]
- Marin, B.; Otero, A.; Lugan, S.; Espinosa, J.C.; Marin-Moreno, A.; Vidal, E.; Hedman, C.; Romero, A.; Pumarola, M.; Badiola, J.J.; et al. Classical BSE prions emerge from asymptomatic pigs challenged with atypical/Nor98 scrapie. Sci. Rep. 2021, 11, 17428. [Google Scholar] [CrossRef] [PubMed]
- Huor, A.; Espinosa, J.C.; Vidal, E.; Cassard, H.; Douet, J.Y.; Lugan, S.; Aron, N.; Marin-Moreno, A.; Lorenzo, P.; Aguilar-Calvo, P.; et al. The emergence of classical BSE from atypical/Nor98 scrapie. Proc. Natl. Acad. Sci. USA 2019, 116, 26853–26862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marin-Moreno, A.; Huor, A.; Espinosa, J.C.; Douet, J.Y.; Aguilar-Calvo, P.; Aron, N.; Piquer, J.; Lugan, S.; Lorenzo, P.; Tillier, C.; et al. Radical Change in Zoonotic Abilities of Atypical BSE Prion Strains as Evidenced by Crossing of Sheep Species Barrier in Transgenic Mice. Emerg. Infect. Dis. 2020, 26, 1130–1139. [Google Scholar] [CrossRef] [PubMed]



| RPLN | Palatine Tonsil | Spleen | Mesenteric Lymph Node | RAMALT | ||||
|---|---|---|---|---|---|---|---|---|
| ID # | IP | EIA | IHC | EIA | IHC | IHC | IHC | IHC |
| 1542 | 34 | + | + | + | + | + | + | + |
| 1546 | 30 | + | + | + | + | + | + | + |
| 1555 | 62 | + | + | + | + | nd | + | + |
| 1558 | 19 | + | + | + | + | + | + | + |
| 1561 | 38 | + | + | + | + | + | + | + |
| 1564 | 57 | + | + | nd | + | nd | + | + |
| Neuroanatomic Location | 1542 | 1546 | 1555 | 1558 | 1561 | 1564 |
|---|---|---|---|---|---|---|
| Olfactory bulb | +++ | +++ | +++ | n/a | +++ | ++ |
| Olfactory tract | +++ | +++ | +++ | +++ | +++ | ++ |
| Basal nuclei | ++ | ++ | ++ | + | ++ | + |
| Thalamus | +++ | +++ | ++ | ++ | ++ | ++ |
| Hypothalamus | ++ | ++ | +++ | + | ++ | ++ |
| Colliculi | +++ | ++ | +++ | ++ | +++ | + |
| Pons | +++ | ++ | +++ | ++ | +++ | + |
| Cerebellum | ++ | + | + | + | ++ | + |
| Brainstem, obex | +++ | +++ | +++ | +++ | +++ | +++ |
| Neocortex, caudate nucleus | ++ | + | + | + | ++ | + |
| Neocortex, thalamus | + | + | + | + | + | + |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cassmann, E.D.; Frese, A.J.; Moore, S.J.; Greenlee, J.J. Transmission of Raccoon-Passaged Chronic Wasting Disease Agent to White-Tailed Deer. Viruses 2022, 14, 1578. https://doi.org/10.3390/v14071578
Cassmann ED, Frese AJ, Moore SJ, Greenlee JJ. Transmission of Raccoon-Passaged Chronic Wasting Disease Agent to White-Tailed Deer. Viruses. 2022; 14(7):1578. https://doi.org/10.3390/v14071578
Chicago/Turabian StyleCassmann, Eric D., Alexis J. Frese, S. Jo Moore, and Justin J. Greenlee. 2022. "Transmission of Raccoon-Passaged Chronic Wasting Disease Agent to White-Tailed Deer" Viruses 14, no. 7: 1578. https://doi.org/10.3390/v14071578
APA StyleCassmann, E. D., Frese, A. J., Moore, S. J., & Greenlee, J. J. (2022). Transmission of Raccoon-Passaged Chronic Wasting Disease Agent to White-Tailed Deer. Viruses, 14(7), 1578. https://doi.org/10.3390/v14071578









