Abstract
Hepatitis B virus (HBV) infection is the first cause of liver cirrhosis and cancer in West Africa. Although the exposure to additional environmental and infectious risk factors may lead to the faster progression of liver disease, few large-scale studies have evaluated the determinants of HBV-related liver fibrosis in the region. We used transient elastography to evaluate the prevalence of liver fibrosis and assessed the association between HBV markers and significant liver fibrosis in a cohort of people living with HBV in Dakar, Senegal. The prevalence of significant liver fibrosis was 12.5% (95% confidence interval [CI] 9.6%–15.9%) among 471 people with HBV mono-infection (pwHBV) and 6.4% (95% CI 2.6%–12.7%) in 110 people with HIV/HBV co-infection (pwHIV/HBV) on tenofovir-containing antiretroviral therapy (p = 0.07). An HBV viral load > 2000 IU/mL was found in 133 (28.3%) pwHBV and 5 (4.7%) pwHIV/HBV, and was associated with significant liver fibrosis (adjusted odds ratio (aOR) 1.95, 95% CI 1.04–3.66). Male participants (aOR 4.32, 95% CI 2.01–8.96) and those with elevated ALT (aOR 4.32, 95% CI 2.01–8.96) were especially at risk of having significant liver fibrosis. Our study shows that people with an HBV viral load above 2000 IU/mL have a two-fold increase in the risk of liver fibrosis and may have to be considered for antiviral therapy, independent of other disease parameters.
1. Introduction
Hepatitis B virus (HBV) infection affects >10% of the general population in West Africa, and is the first cause of liver cirrhosis and cancer [1,2]. According to a recent meta-analysis, between 4% and 13% of people living with HBV in Africa had signs of liver cirrhosis, an indication for the immediate initiation of antiviral therapy [3]. The risk of liver-related complications in the region is further exacerbated by co-existing environmental factors, such as the exposure to aflatoxin, and co-infections with HIV, hepatitis delta or Schistosoma mansoni [4,5,6]. Although antiviral therapy effectively suppresses the HBV viral load and reduces the risk of HBV-related complications, such as the progression to liver cirrhosis and hepatocellular carcinoma (HCC), the criteria for its initiation in Africa are still debated [7,8].
The World Health Organization recently called for the elimination of viral hepatitis as a public health problem by 2030, which includes the reduction of liver-related mortality by 65% [9]. Understanding the natural history of the infection and the key drivers of HBV-related liver fibrosis in highly-endemic regions is key to meeting this objective. The REVEAL study demonstrated the strong association between the level of HBV replication and the incidence of HCC in Asia [10]. Similarly, the risk of developing liver cirrhosis was linked to HBV viral load, even among the HBeAg-negative individuals without transaminase elevation [11]. On the African continent, most of the information available on HBV-related clinical outcomes comes from studies among people with HIV and HBV co-infection, who are generally receiving tenofovir-containing antiretroviral therapy. Thus, the link between the virological determinants of HBV infection and the manifestations of liver disease needs to be explored to guide recommendations on eligibility for antiviral therapy.
Taking advantage of the infrastructure of two large referral HIV clinics in Dakar, Senegal, we established a prospective cohort (SEN-B) of people living with HBV (pwHBV) and HIV/HBV (pwHIV/HBV), to study the determinants of HBV infection and functional cure. In this analysis, we aimed to evaluate the association between HBV replication and liver fibrosis in people living with HBV in Senegal.
2. Materials and Methods
We conducted a cross-sectional analysis within the Senegalese Hepatitis B Cohort study (SEN-B) in Dakar. Since October 2019, all of the individuals aged >16 years and presenting with a confirmed positive hepatitis B surface antigen (HBsAg) test result at the Infectious and Tropical Disease Service (SMIT) and the Ambulatory Treatment Centre (CTA) at Fann University Hospital, were invited to participate in SEN-B. SMIT and CTA are the largest referral centers for HIV care in Senegal, with >3000 people living with HIV (pwHIV) under regular follow-up. We also undertook the systematic HBsAg screening for all of the pwHIV in current follow-up at the SMIT/CTA clinics, and included individuals with HIV/HBV co-infection into SEN-B [12]. The SEN-B cohort was approved by the national Ethics Committee, and all of the patients signed an informed consent to participate in the study.
The demographic, clinical and laboratory data, as well as transient elastography and abdominal ultrasound measurements, were collected at enrolment (baseline) and 6-monthly thereafter. The data were collected using standardized forms and were subsequently entered into an electronic database (ARPEGE®). The HBV surface antigens (HBsAg) were tested, using a lateral-flow assay test (NovaTest®|Atlaslink-inc ISO 13485) and confirmed with the e411 cobas® HBsAg II (2011–08 V.10) platform. The HBV DNA levels were measured using the cobas®/TaqMan® (Roche Diagnostic Systems, Meylan, France) with a threshold of detection of 20 IU/mL. HIV, hepatitis C virus (HCV) and hepatitis D were tested using commercial lateral-flow assays (Determine® HIV/HCV, Abbot, and Diasorin® for HDV). The alanine aminotransferase (ALT) elevation was defined as >40 IU.
Liver stiffness was measured by transient elastography (TE) during clinic visits by a single trained operator, according to the instructions provided by the manufacturer (Fibroscan®, Echosens, France). The liver stiffness measurements (LSM) were considered valid only if 10 successful acquisitions were obtained, and the interquartile range (IQR) to median ratio of the 10 acquisitions was <0.3 [13]. We used an M probe for standard assessment and a XL probe if BMI was >25 kg/m2. The cut-off value of 7.0 kPa was used to estimate the number of subjects with significant fibrosis, and 11.0 kPa for cirrhosis [14]. Alcohol consumption was assessed using the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C), modified to measure drinking in the prior 6 months [15,16]. Current abstinence was an AUDIT-C of 0 points, moderate drinking was one–two points for women and one–three for men, and unhealthy consumption was >two for women and >three for men.
Statistical Analysis
We compared the demographic and clinical characteristics between pwHBV and pwHIV/HBV at enrolment into the cohort using descriptive analyses. The χ2 test was used for the categorical variables and the Wilcoxon rank-sum test for the continuous ones. We evaluated the proportion of the participants in the different liver stiffness groups (no fibrosis, fibrosis, cirrhosis) by HIV status, sex, ALT and HBV DNA levels, and compared the estimates between pwHBV and pwHIV/HBV using Fisher’s exact test. We used multivariable logistic regression to evaluate the association between HBV viral load and significant fibrosis, after adjustment for the following baseline variables: age; sex; body mass index (BMI); use of traditional medicine; unhealthy alcohol consumption; HIV status and ALT values. The association was further explored by repeating the analyses after excluding (i) pwHIV/HBV and (ii) pwHBV who had received HBV antiviral treatment prior to the outcome measurement.
Since the individuals with elevated ALT levels tend to have higher LSM than those with normal ALT levels at the same stage of liver fibrosis, we performed a sensitivity analysis, adapting TE cut-offs based on levels of ALT [17]. For the individuals with elevated ALT (>40 IU) we used TE cut-off values >7.5 kPa for significant fibrosis and >12.0 kPa for cirrhosis. All of the statistical analysis were completed using Stata 16.1 (Stata corp.) and the regression plots were produced by user command “coefplot” and “grstyle” [18,19].
3. Results
3.1. Characteristics of Study Population
We included 581 individuals with a positive HBsAg test, of whom 110 (18.9%) were living with HIV. The median age at enrolment was 31 years (interquartile range (IQR) 25–39) among pwHBV and 46 years (IQR 38–54) in pwHIV/HBV (p < 0.001, Table 1). The median BMI as well as the proportion of women were similar in both of the groups. Unhealthy alcohol consumption was infrequent: 1.9% in pwHBV and 2.7% in pwHIV/HBV. Only two of the participants had antibodies against hepatitis C virus (HCV) infection, and three against hepatitis D virus (HDV) infection.

Table 1.
Characteristics of the study population at the time of liver fibrosis assessment, by HIV co-infection status.
All of the pwHIV/HBV were receiving TDF as part of their ART regimen, for a median time of 5.3 years (IQR; 3.0–8.4), while only 4.7% of the pwHBV were on antiviral therapy at the time of inclusion, for a median time of 0.6 years (IQR 0–1.4). More of the pwHIV/HBV presented with elevated ALT measurements (>40 IU) compared to the pwHBV (17.3% vs. 7.8%; p = 0.01). HBV DNA was <20 IU in 76/471 (16.2%) of the pwHBV and in 89/110 (83.2%) of the pwHIV/HBV (p < 0.001). A higher proportion of the pwHBV presented with HBV DNA >2000 IU/mL compared to the pwHIV/HBV (28.3% vs. 4.7%; p < 0.001). A summary of the characteristics of the study population is presented in Table 1.
3.2. Prevalence of Significant Liver Fibrosis and Cirrhosis
The prevalence of significant liver fibrosis was 12.5% (95% CI 9.6–15.9) in the pwHBV and 6.4% (95% CI 2.6–12.7) in the pwHIV/HBV (p = 0.07), whereas the estimate for liver cirrhosis was similar in both of the groups (pwHBV: 4.0%, 95% CI 2.4–6.0; pwHIV/HBV: 3.6%, 95% CI 1.0–9.0, p = 1.00). Among the treatment-naïve pwHBV (n = 449), the prevalence of significant liver fibrosis was 12.2% (95% CI 9.3–15.6) and cirrhosis 3.6% (95% CI 2.1–5.8).
The distribution of LSM categories by HIV status, sex, ALT and HBV DNA values is presented in Figure 1. In the pwHBV, men were more likely to have significant fibrosis (19.9% vs. 3.7%, p < 0.001) and cirrhosis (7.4% vs. 0.0%, p < 0.001, Table S1, Supplementary Materials) compared to women. Furthermore, the pwHBV with HBV DNA >2000 IU/mL were more likely to have significant fibrosis compared to those with HBV DNA ≤ 2000 IU/mL (male: 29.5% vs. 15.8%, p = 0.01; female: 5.5% vs. 3.1%, p = 0.43). Likewise, male pwHBV with elevated ALT (> 40 IU) were more likely to present with significant fibrosis compared to those with normal ALT levels (45.4% vs. 16.6%, p = 0.001). Although the numbers were small, we found similar associations between HBV DNA or ALT and liver fibrosis among male pwHIV/HBV (Table S1, Supplementary Materials). In the secondary analyses, which focused on the treatment-naïve pwHBV, the differences in the proportions of participants with fibrosis and cirrhosis between HBV DNA and ALT groups were similar to those from the main analyses (Table S2, Supplementary Materials).
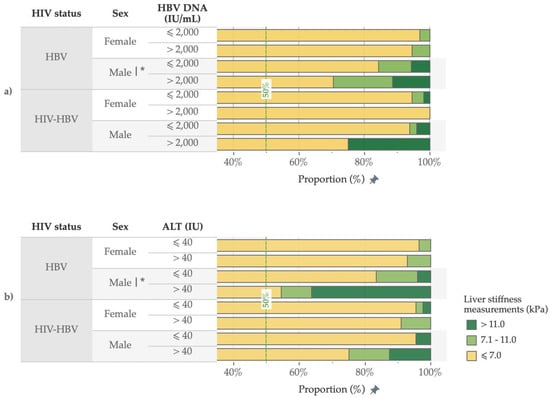
Figure 1.
Proportion of participants in the different liver stiffness measurement categories, by HIV status, sex, HBV DNA (a) and ALT (b) values. |* p < 0.05 in univariable analyses.
3.3. Risk Factors for Significant Fibrosis and Cirrhosis
In multivariable analyses including all of the participants, those with HBV DNA > 2000 IU/mL were more likely to have significant fibrosis than those with low levels of HBV DNA (adjusted odds ratio (aOR) 1.95, 95% CI 1.04–3.66, p = 0.04) (Figure 2).
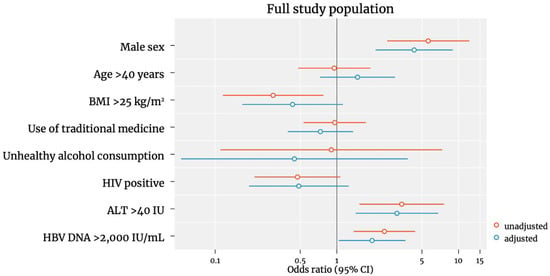
Figure 2.
Predictors of significant liver fibrosis in the full study population. Odds ratios were plotted on a logscale.
Male sex (aOR 4.32, 2.01–8.96, p < 0.001) and elevated ALT (aOR 4.32, 2.01–8.96, p < 0.001) were also independent risk factors of significant fibrosis. However, HIV/HBV co-infection, age > 40 years, use of traditional medicine and hazardous alcohol consumption were not associated with liver fibrosis. Being overweight (BMI > 25) was associated with a reduced risk of significant fibrosis in the unadjusted analysis, however this association did not remain significant in the adjusted analysis (aOR 0.43, 95% CI 0.16–1.12; p = 0.09). We additionally performed an analysis including only the untreated pwHBV and the same factors remained associated with liver fibrosis (Figure 3). Due to the low number of cirrhosis cases (22 in male and 1 in female|19 in pwHBV and 4 in pwHIV/HBV), our analysis was underpowered to estimate the associations with cirrhosis.
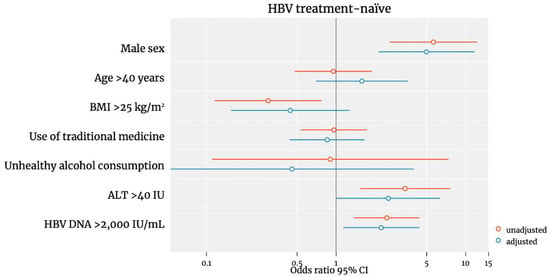
Figure 3.
Predictors of significant liver fibrosis among treatment-naïve pwHBV. Odds ratios were plotted on a logscale.
Our results were similar in the sensitivity analysis using the definitions of significant fibrosis and cirrhosis adapted to ALT measurements (Figure S1, Supplementary Materials). Male sex (aOR 4.80, 95% CI 2.24–10.31; p < 0.001), elevated HBV DNA > 2000 IU/mL (aOR 3.22, 95% CI 1.46–7.09; p = 0.004) and elevated ALT (aOR 3.22, 95% CI 1.46–7.09; p = 0.004) remained associated with higher odds of significant fibrosis.
4. Discussion
In our cross-sectional assessment of the people living with HBV in urban Senegal, 12% of the treatment-naïve people living with HBV and 6% of those living with HIV and HBV on ART had significant liver fibrosis. The participants with an HBV viral load >2000 IU/mL were twice as likely to present with significant fibrosis as those with lower HBV DNA levels. Male sex and elevated ALT were additional independent risk factors for liver fibrosis. Our findings suggest a strong association between HBV replication and liver fibrosis in Senegal, and, if confirmed in prospective cohort studies in the region, they may argue for the early initiation of antiviral therapy in the context of HBV replication, to reduce the risk of development of liver disease.
Although transient elastography is considered the best method for the non-invasive measurement of liver fibrosis in individuals with HBV infection, it is rarely available in African healthcare-settings. A recent meta-analysis, including both pwHBV and pwHIV/HBV, found only seven studies across Africa reporting fibrosis using TE [3]. The pooled prevalence of significant fibrosis was 11.6%, and the estimate for cirrhosis was 6.1%, both very similar to our results. In contrast, Aberra et al. found a prevalence of fibrosis reaching 26% in a large tertiary care referral center in Ethiopia, highlighting the importance of considering the type of healthcare setting in the interpretation of the HBV-related liver complications in sub-Saharan Africa [20]. Although our participants were enrolled into the SEN-B cohort in a tertiary care center, our study population can be considered to represent the general population, as >80% were referred from community/primary care structures after routine testing at a transfusion center, patients’ association or general practitioner’s office in the absence of signs of liver disease.
Our findings highlight the strong association between HBV viral replication and significant liver fibrosis in pwHBV from sub-Saharan Africa. Two landmark studies from the REVEAL-HBV cohort identified HBV DNA levels as the most important predictor for the progression to end-stage liver disease [10,11]. These two analyses of the pwHBV in Taiwan showed that HBV DNA levels at enrolment was an independent predictor of cirrhosis, HCC and all-cause mortality. Importantly, the same observation was made when considering only the HBeAg-negative individuals with normal ALT values [11]. In one of the few studies from Africa, HBV viremia was also found to be linked with an increased risk of cirrhosis and HCC [21]. In our study, elevated HBV DNA was independently associated with liver fibrosis, including in the subset of treatment-naive pwHBV and after adjustment for ALT values. If the prospective studies show a similar link between elevated DNA levels and the development of liver fibrosis, the presence of HBV replication could become a strong argument for the early initiation of antiviral therapy, independent of other markers of activity. In a recently published study of >80,000 individuals with chronic HBV infection in the USA, Wong et al. suggested a simplified stepwise strategy to increase eligibility for antiviral therapy and estimated that treating individuals with a viral load >2000 IU/mL, regardless of ALT values, would increase the proportion of treatment eligible individuals by 34% [22]. To progress towards hepatitis B elimination in Africa, simplified treatment criteria, using HBV replication as the central criterion, may be crucial to overcome the barriers to treatment and reduce the burden of liver disease in pwHBV [7,22].
Male sex was associated with a five-fold increased risk of significant fibrosis, and this association remained similar when considering only untreated pwHBV. Similar results were observed in other studies, using TE to measure liver fibrosis among Asian populations with HBV [23,24]. It has been suggested that female sex hormones could play a protective role for liver fibrosis, but this hypothesis has yet to be evaluated in African populations [25]. In contrast to the existing literature, we did not find an association between HIV status and an increased risk of liver fibrosis. However, most of the previous studies showed HIV co-infection to be linked to elevated LSM before ART was initiated, and limited data exist on the treatment-experienced populations [26,27,28,29]. In prospective studies from Tanzania and Zambia, liver fibrosis regression occurred during ART, irrespective of HBV infection [27,30]. The long-term follow-up of cohorts, including pwHBV with and without HIV-coinfection, will be crucial to understand the impact of HIV infection on liver disease progression.
Our study is among the first in sub-Saharan Africa to assess the determinants of liver fibrosis using TE in people with different degrees of HBV replication. However, despite the high diagnostic accuracy of TE for the detection of liver fibrosis in pwHBV [31], optimal thresholds are yet to be determined for HIV/HBV co-infection and in the presence of liver inflammation. Nevertheless, our results remained similar across sensitivity analyses, including after adjustment of the TE thresholds according to the ALT levels. We had incomplete data on HDV co-infection for half of the study participants, which may have under/over-estimated the prevalence. Furthermore, we could not account for other liver fibrosis risk factors, such as Schistosomiasis sp. infection, which is highly endemic in Senegal. However, its association with liver fibrosis is still a matter of debate in individuals with HBV infection [32].
5. Conclusions
Our findings from a large cohort of people living with HBV in Senegal suggest a strong association between HBV replication and liver fibrosis. Considering antiviral therapy eligibility based on HBV DNA levels independently of other factors may help reduce the burden of liver fibrosis among people with HBV infection in sub-Saharan Africa, should our results be confirmed in prospective studies.
Supplementary Materials
Table S1. Proportions of participants with significant fibrosis and cirrhosis among pwHIV/HBV by sex, ALT and HBV DNA values. Table S2. Proportions of participants with significant fibrosis and cirrhosis among untreated pwHBV by sex, ALT and HBV DNA values. Figure S1. Predictors of significant liver fibrosis using adapted liver stiffness measurments thresholds to ALT levels in the full study population. Odds ratios were plotted on a logscale. The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v14081614/s1.
Author Contributions
Conceptualization, A.R.M. and G.W.; methodology, A.R.M. and G.W.; software, A.R.M.; statistical analyses, A.R.M. and G.W.; writing of first draft of the manuscript, A.R.M. and G.W.; data collection, A.R.M., N.F.N., J.T., K.N., L.F., O.N., M.F., A.G., D.K., M.S. and on behalf of the SEN-B Study Group. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a Swiss National Science Foundation Professorship Grant to Gilles Wandeler (PP00P3_176944), and an investigator-initiated study from Roche Diagnostics.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Senegalese National Health Research Ethics Committee (CNERS) at the Health and Social Action Ministry of Senegal (0061/MSAS/DPRS/CNERS). All participants signed an informed consent.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We warmly thank all patients for their acceptance on study participation. A special acknowledgment for Ibrahima Gueye and Ndeye Fatou Guirane from SAAFARA hepatitis patient’s association in Senegal. We thank all the SEN-B team, in particular Amady Ndiaye, Oumy Camara, Ahmadou Mboup, Aminata Diallo, Khady Ndaw, Khady Ghassama, Sadio Alassane Ndiaye, Abibatou Diaw, Aminata Ndoye Badji, Melissa Sandrine Penda, Hubert Akotia, Bineta Seck Fall, Mariama Diedhiou, Albert Gautier Ndione, Ibrahima Niang, Mbaye Thiam, Cheik Tidiane et Aissatou Niang.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- GBD 2017 Cirrhosis Collaborators. The Global, Regional, and National Burden of Cirrhosis by Cause in 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 245–266. [Google Scholar] [CrossRef]
- Mc Naughton, A.L.; Lourenço, J.; Bester, P.A.; Mokaya, J.; Lumley, S.F.; Obolski, U.; Forde, D.; Maponga, T.G.; Katumba, K.R.; Goedhals, D.; et al. Hepatitis B Virus Seroepidemiology Data for Africa: Modelling Intervention Strategies Based on a Systematic Review and Meta-Analysis. PLoS Med. 2020, 17, e1003068. [Google Scholar] [CrossRef]
- Surial, B.; Wyser, D.; Béguelin, C.; Ramírez-Mena, A.; Rauch, A.; Wandeler, G. Prevalence of Liver Cirrhosis in Individuals with Hepatitis B Virus Infection in Sub-Saharan Africa: Systematic Review and Meta-Analysis. Liver Int. 2021, 41, 710–719. [Google Scholar] [CrossRef] [PubMed]
- Kamal, H.; Fornes, R.; Simin, J.; Stål, P.; Duberg, A.-S.; Brusselaers, N.; Aleman, S. Risk of Hepatocellular Carcinoma in Hepatitis B and D Virus Co-Infected Patients: A Systematic Review and Meta-Analysis of Longitudinal Studies. J. Viral Hepat. 2021, 28, 1431–1442. [Google Scholar] [CrossRef]
- Kew, M.C. Aflatoxins as a Cause of Hepatocellular Carcinoma. J. Gastrointestin. Liver Dis. 2013, 22, 305–310. [Google Scholar] [PubMed]
- Khatami, A.; Bahadory, S.; Ghorbani, S.; Saadati, H.; Zarei, M.; Soleimani, A.; Zibaei, M. Two Rivals or Colleagues in the Liver? Hepatit B Virus and Schistosoma Mansoni Co-Infections: A Systematic Review and Meta-Analysis. Microb. Pathog. 2021, 154, 104828. [Google Scholar] [CrossRef]
- McNaughton, A.L.; Lemoine, M.; van Rensburg, C.; Matthews, P.C. Extending Treatment Eligibility for Chronic Hepatitis B Virus Infection. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 146–147. [Google Scholar] [CrossRef]
- Jeng, W.-J.; Lok, A.S. Should Treatment Indications for Chronic Hepatitis B Be Expanded? Clin. Gastroenterol. Hepatol. 2021, 19, 2006–2014. [Google Scholar] [CrossRef]
- Global Hepatitis Report. 2017. Available online: https://www.who.int/publications-detail-redirect/9789241565455 (accessed on 30 May 2022).
- Chen, C.-J.; Yang, H.-I.; Su, J.; Jen, C.-L.; You, S.-L.; Lu, S.-N.; Huang, G.-T.; Iloeje, U.H.; REVEAL-HBV Study Group. Risk of Hepatocellular Carcinoma across a Biological Gradient of Serum Hepatitis B Virus DNA Level. JAMA 2006, 295, 65–73. [Google Scholar] [CrossRef]
- Iloeje, U.H.; Yang, H.-I.; Su, J.; Jen, C.-L.; You, S.-L.; Chen, C.-J.; Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer-In HBV (the REVEAL-HBV) Study Group. Predicting Cirrhosis Risk Based on the Level of Circulating Hepatitis B Viral Load. Gastroenterology 2006, 130, 678–686. [Google Scholar] [CrossRef]
- Ramírez Mena, A.; Tine, J.M.; Fortes, L.; Ndiaye, O.; Ka, D.; Ngom, N.F.; Ramette, A.; Bittel, P.; Seydi, M.; Wandeler, G. Hepatitis B Screening Practices and Viral Control among Persons Living with HIV in Urban Senegal. J. Viral Hepat. 2021, 29, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Boursier, J.; Zarski, J.-P.; de Ledinghen, V.; Rousselet, M.-C.; Sturm, N.; Lebail, B.; Fouchard-Hubert, I.; Gallois, Y.; Oberti, F.; Bertrais, S.; et al. Determination of Reliability Criteria for Liver Stiffness Evaluation by Transient Elastography. Hepatology 2013, 57, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. Available online: http://www.who.int/hepatitis/publications/hepatitis-b-guidelines/en/ (accessed on 24 August 2020).
- Bradley, K.A.; DeBenedetti, A.F.; Volk, R.J.; Williams, E.C.; Frank, D.; Kivlahan, D.R. AUDIT-C as a Brief Screen for Alcohol Misuse in Primary Care. Alcohol. Clin. Exp. Res. 2007, 31, 1208–1217. [Google Scholar] [CrossRef] [PubMed]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT Alcohol Consumption Questions (AUDIT-C): An Effective Brief Screening Test for Problem Drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- Chan, H.L.-Y.; Wong, G.L.-H.; Choi, P.C.-L.; Chan, A.W.-H.; Chim, A.M.-L.; Yiu, K.K.-L.; Chan, F.K.-L.; Sung, J.J.-Y.; Wong, V.W.-S. Alanine Aminotransferase-Based Algorithms of Liver Stiffness Measurement by Transient Elastography (Fibroscan) for Liver Fibrosis in Chronic Hepatitis B. J. Viral Hepat. 2009, 16, 36–44. [Google Scholar] [CrossRef]
- Jann, B. Plotting Regression Coefficients and Other Estimates. Stata J. 2014, 14, 708–737. [Google Scholar] [CrossRef]
- Jann, B. Customizing Stata Graphs Made Easy (Part 2). Stata J. 2018, 18, 786–802. [Google Scholar] [CrossRef]
- Aberra, H.; Desalegn, H.; Berhe, N.; Mekasha, B.; Medhin, G.; Gundersen, S.G.; Johannessen, A. The WHO Guidelines for Chronic Hepatitis B Fail to Detect Half of the Patients in Need of Treatment in Ethiopia. J. Hepatol. 2019, 70, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Mendy, M.E.; Welzel, T.; Lesi, O.A.; Hainaut, P.; Hall, A.J.; Kuniholm, M.H.; McConkey, S.; Goedert, J.J.; Kaye, S.; Rowland-Jones, S.; et al. Hepatitis B Viral Load and Risk for Liver Cirrhosis and Hepatocellular Carcinoma in The Gambia, West Africa. J. Viral Hepat 2010, 17, 115–122. [Google Scholar] [CrossRef]
- Wong, R.J.; Kaufman, H.W.; Niles, J.K.; Kapoor, H.; Gish, R.G. Simplifying Treatment Criteria in Chronic Hepatitis B: Reducing Barriers to Elimination. Clin. Infect. Dis. 2022, ciac385. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, P.; Zhang, M. Predictors for Advanced Liver Fibrosis in Chronic Hepatitis B Virus Infection with Persistently Normal or Mildly Elevated Alanine Aminotransferase. Exp. Med. 2017, 14, 5363–5370. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, J.-F.; Song, S.-H.; Lee, C.-S.; Chen, H.-L.; Ni, Y.-H.; Hsu, H.-Y.; Wu, T.-C.; Chang, M.-H. Clinical Predictors of Liver Fibrosis in Patients With Chronic Hepatitis B Virus Infection From Children to Adults. J. Infect. Dis. 2018, 217, 1408–1416. [Google Scholar] [CrossRef] [PubMed]
- Xiong, M.; Li, J.; Yang, S.; Zeng, F.; Ji, Y.; Liu, J.; Wu, Q.; He, Q.; Jiang, R.; Zhou, F.; et al. Influence of Gender and Reproductive Factors on Liver Fibrosis in Patients With Chronic Hepatitis B Infection. Clin. Transl. Gastroenterol. 2019, 10, e00085. [Google Scholar] [CrossRef]
- Hawkins, C.; Agbaji, O.; Ugoagwu, P.; Thio, C.L.; Auwal, M.M.; Ani, C.; Okafo, C.; Wallender, E.; Murphy, R.L. Assessment of Liver Fibrosis by Transient Elastography in Patients with HIV and Hepatitis B Virus Coinfection in Nigeria. Clin. Infect. Dis. 2013, 57, e189–e192. [Google Scholar] [CrossRef] [PubMed]
- Vinikoor, M.J.; Sinkala, E.; Chilengi, R.; Mulenga, L.B.; Chi, B.H.; Zyambo, Z.; Hoffmann, C.J.; Saag, M.S.; Davies, M.-A.; Egger, M.; et al. Impact of Antiretroviral Therapy on Liver Fibrosis Among Human Immunodeficiency Virus-Infected Adults With and Without HBV Coinfection in Zambia. Clin. Infect. Dis. 2017, 64, 1343–1349. [Google Scholar] [CrossRef]
- Jaquet, A.; Wandeler, G.; Nouaman, M.; Ekouevi, D.K.; Tine, J.; Patassi, A.; Coffie, P.A.; Tanon, A.; Seydi, M.; Attia, A.; et al. Alcohol Use, Viral Hepatitis and Liver Fibrosis among HIV-Positive Persons in West Africa: A Cross-Sectional Study. J. Int. AIDS Soc. 2017, 19, 21424. [Google Scholar] [CrossRef]
- Stockdale, A.J.; Phillips, R.O.; Beloukas, A.; Appiah, L.T.; Chadwick, D.; Bhagani, S.; Bonnett, L.; Sarfo, F.S.; Dusheiko, G.; Geretti, A.M. Liver Fibrosis by Transient Elastography and Virologic Outcomes After Introduction of Tenofovir in Lamivudine-Experienced Adults With HIV and Hepatitis B Virus Coinfection in Ghana. Clin. Infect. Dis. 2015, 61, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.L.; Agaba, P.; Ugoagwu, P.; Muazu, A.; Okpokwu, J.; Akpa, S.; Machenry, S.; Imade, G.; Agbaji, O.; Thio, C.L.; et al. Changes in Liver Stiffness after ART Initiation in HIV-Infected Nigerian Adults with and without Chronic HBV. J. Antimicrob. Chemother. 2019, 74, 2003–2008. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Huang, Y.-S.; Wang, Z.-Z.; Yang, Z.-R.; Sun, F.; Zhan, S.-Y.; Liu, X.-E.; Zhuang, H. Systematic Review with Meta-Analysis: The Diagnostic Accuracy of Transient Elastography for the Staging of Liver Fibrosis in Patients with Chronic Hepatitis B. Aliment. Pharm. 2016, 43, 458–469. [Google Scholar] [CrossRef]
- Abruzzi, A.; Fried, B.; Alikhan, S.B. Coinfection of Schistosoma Species with Hepatitis B or Hepatitis C Viruses. Adv. Parasitol. 2016, 91, 111–231. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).



