Inhibition of Venezuelan Equine Encephalitis Virus Using Small Interfering RNAs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture and Viruses
2.2. siRNA Design and Synthesis
2.3. Transfection
2.4. Infection
2.5. Cell Viability
2.6. Enzyme-Linked Immunosorbent Assay (ELISA)
2.7. Immunoprecipitation
2.8. Western Blot
2.9. Liquid Chromatography–Mass Spectrometry
2.10. Plaque Assay
2.11. Statistical Analysis
3. Results
3.1. Design of vsiRNAs That Target the VEEV Genome
3.2. Efficacy of Anti-VEEV siRNAs in Reducing TC-83 Replication In Vitro
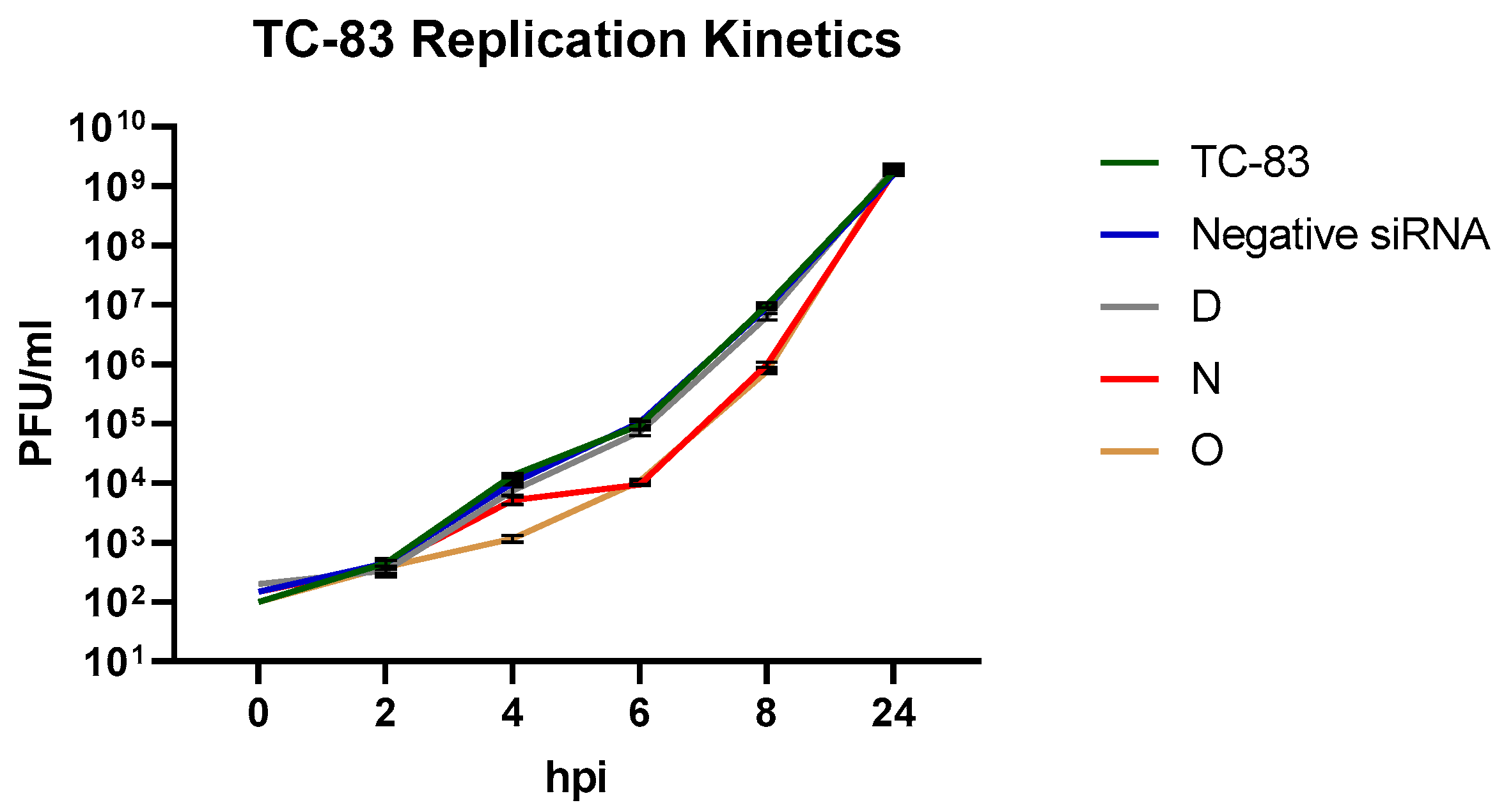
3.3. Impact of Efficient vsiRNAs on Viral Multiplication Kinetics
3.4. Efficacy of vsiRNAs in Reducing TrD Multiplication
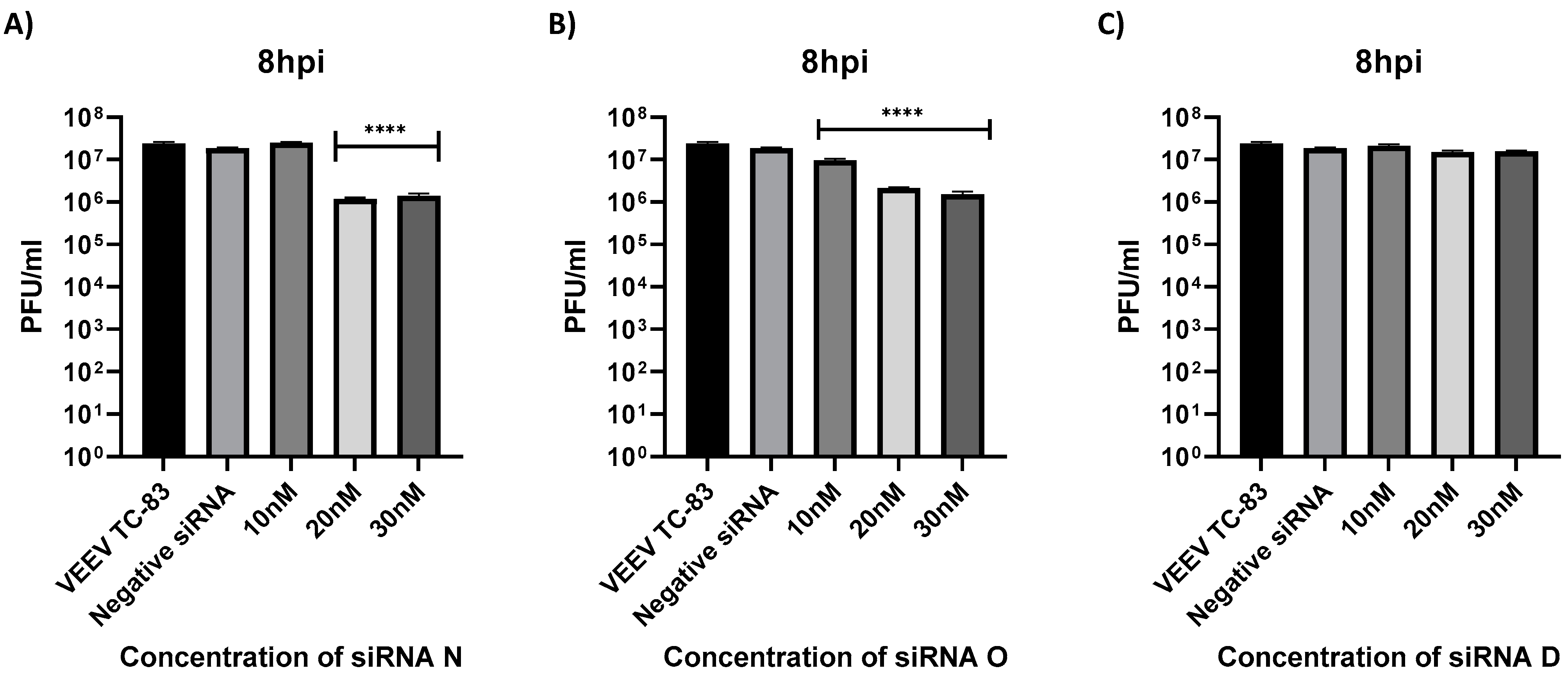
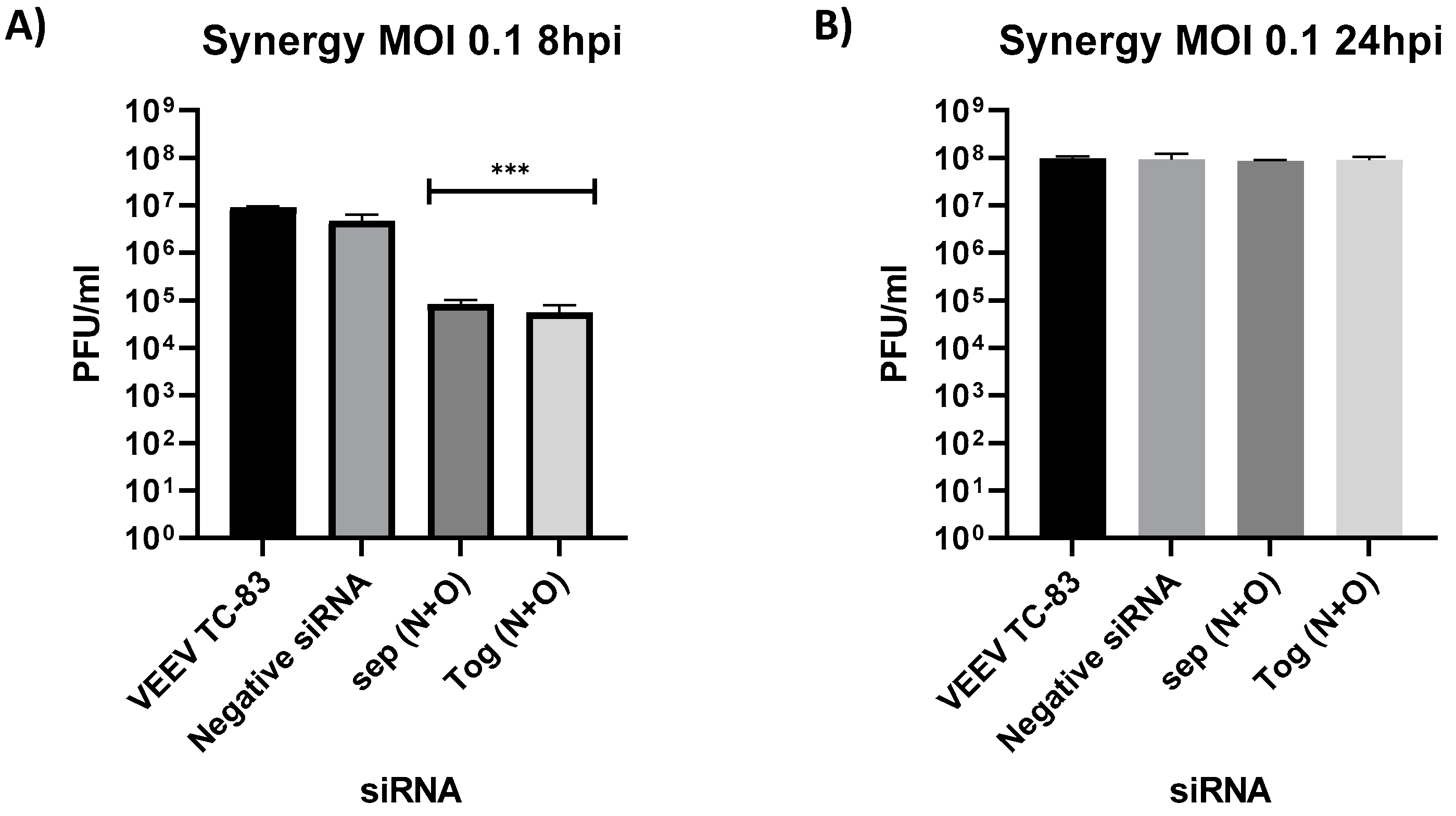
3.5. Dose Dependence and Impact of Combination of siRNA on Antiviral Efficacy
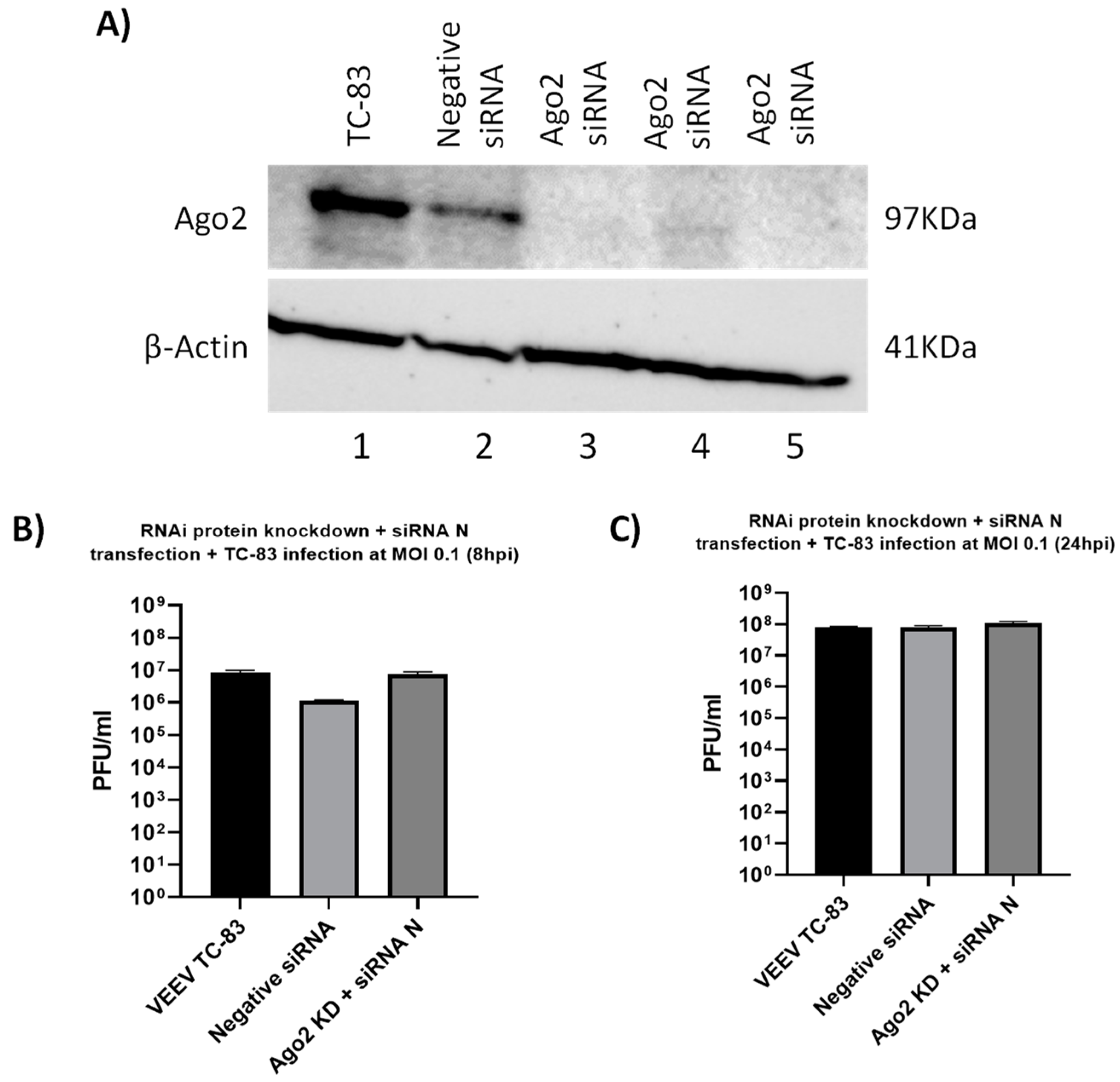
3.6. Mechanistic Assessment of Antiviral Activity of vsiRNAs
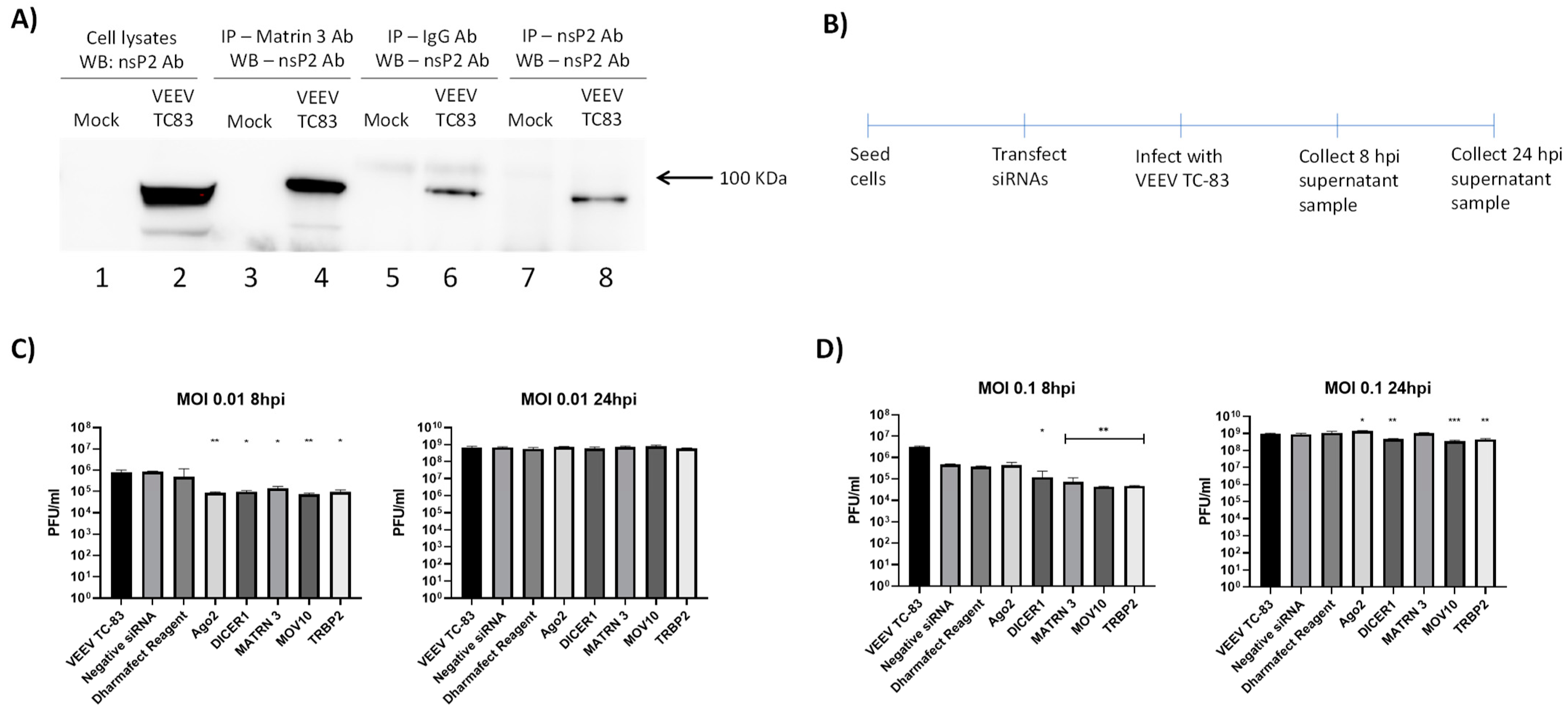
3.7. Interaction of VEEV nsP2 with the RNAi Pathway
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weaver, S.C.; Ferro, C.; Barrera, R.; Boshell, J.; Navarro, J.C. Venezuelan equine encephalitis. Annu Rev Entomol. 2004, 49, 141–174. [Google Scholar]
- Calisher, C.H. Medically important arboviruses of the United States and Canada. Clin. Microbiol. Rev. 1994, 7, 89–116. [Google Scholar]
- Guzmán-Terán, C.; Calderón-Rangel, A.; Rodriguez-Morales, A.; Mattar, S. Venezuelan equine encephalitis virus: The problem is not over for tropical America. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 19. [Google Scholar]
- Ferro, C.; Boshell, J.; Moncayo, A.C.; Gonzalez, M.; Ahumada, M.L.; Kang, W.; Weaver, S.C. Natural enzootic vectors of Venezuelan equine encephalitis virus, Magdalena Valley, Colombia. Emerg. Infect. Dis. 2003, 9, 49–54. [Google Scholar]
- Smith, D.R.; Aguilar, P.V.; Coffey, L.L.; Gromowski, G.D.; Wang, E.; Weaver, S.C. Venezuelan equine encephalitis virus transmission and effect on pathogenesis. Emerg. Infect. Dis. 2006, 12, 1190–1196. [Google Scholar]
- Taylor, K.G.; Paessler, S. Pathogenesis of Venezuelan equine encephalitis. Vet. Microbiol. 2013, 167, 145–150. [Google Scholar]
- Sharma, A.; Knollmann-Ritschel, B. Current Understanding of the Molecular Basis of Venezuelan Equine Encephalitis Virus Pathogenesis and Vaccine Development. Viruses 2019, 11, 164. [Google Scholar]
- Paessler, S.; Weaver, S.C. Vaccines for Venezuelan equine encephalitis. Vaccine 2009, 27 (Suppl. S4), D80–D85. [Google Scholar]
- García-Dorival, I.; Wu, W.; Dowall, S.; Armstrong, S.; Touzelet, O.; Wastling, J.; Barr, J.N.; Matthews, D.; Carroll, M.; Hewson, R.; et al. Elucidation of the Ebola virus VP24 cellular interactome and disruption of virus biology through targeted inhibition of host-cell protein function. J. Proteome Res. 2014, 13, 5120–5135. [Google Scholar]
- Hoenen, T.; Groseth, A.; Feldmann, H. Therapeutic strategies to target the Ebola virus life cycle. Nat. Rev. Microbiol. 2019, 17, 593–606. [Google Scholar]
- Li, J.; Guo, M.; Tian, X.; Wang, X.; Yang, X.; Wu, P.; Liu, C.; Xiao, Z.; Qu, Y.; Yin, Y.; et al. Virus-Host Interactome and Proteomic Survey Reveal Potential Virulence Factors Influencing SARS-CoV-2 Pathogenesis. Med 2021, 2, 99–112.e7. [Google Scholar]
- Messina, F.; Giombini, E.; Agrati, C.; Vairo, F.; Ascoli Bartoli, T.; Al Moghazi, S.; Piacentini, M.; Locatelli, F.; Kobinger, G.; Maeurer, M.; et al. COVID-19: Viral-host interactome analyzed by network based-approach model to study pathogenesis of SARS-CoV-2 infection. J. Transl. Med. 2020, 18, 233. [Google Scholar]
- Batra, J.; Hultquist, J.F.; Liu, D.; Shtanko, O.; Von Dollen, J.; Satkamp, L.; Jang, G.M.; Luthra, P.; Schwarz, T.M.; Small, G.I.; et al. Protein Interaction Mapping Identifies RBBP6 as a Negative Regulator of Ebola Virus Replication. Cell 2018, 175, 1917–1930.e13. [Google Scholar]
- Bakovic, A.; Bhalla, N.; Alem, F.; Campbell, C.; Zhou, W.; Narayanan, A. Inhibitors of Venezuelan Equine Encephalitis Virus Identified Based on Host Interaction Partners of Viral Non-Structural Protein 3. Viruses 2021, 13, 1533. [Google Scholar]
- Barrera, M.D.; Callahan, V.; Akhrymuk, I.; Bhalla, N.; Zhou, W.; Campbell, C.; Narayanan, A.; Kehn-Hall, K. Proteomic Discovery of VEEV E2-Host Partner Interactions Identifies GRP78 Inhibitor HA15 as a Potential Therapeutic for Alphavirus Infections. Pathogens 2021, 10, 283. [Google Scholar]
- Sioud, M. RNA interference and innate immunity. Adv. Drug Deliv. Rev. 2007, 59, 153–163. [Google Scholar]
- Berkhout, B. RNAi-mediated antiviral immunity in mammals. Curr. Opin. Virol. 2018, 32, 9–14. [Google Scholar]
- Alkhalil, A.; Strand, S.; Mucker, E.; Huggins, J.W.; Jahrling, P.B.; Ibrahim, S.M. Inhibition of monkeypox virus replication by RNA interference. Virol. J. 2009, 6, 188. [Google Scholar]
- Backes, S.; Shapiro, J.S.; Sabin, L.R.; Pham, A.M.; Reyes, I.; Moss, B.; Cherry, S.; tenOever, B.R. Degradation of host microRNAs by poxvirus poly(A) polymerase reveals terminal RNA methylation as a protective antiviral mechanism. Cell Host Microbe 2012, 12, 200–210. [Google Scholar]
- Fabozzi, G.; Nabel, C.S.; Dolan, M.A.; Sullivan, N.J. Ebolavirus proteins suppress the effects of small interfering RNA by direct interaction with the mammalian RNA interference pathway. J. Virol. 2011, 85, 2512–2523. [Google Scholar]
- Garcia, S.; Billecocq, A.; Crance, J.M.; Prins, M.; Garin, D.; Bouloy, M. Viral suppressors of RNA interference impair RNA silencing induced by a Semliki Forest virus replicon in tick cells. J. Gen. Virol. 2006, 87 Pt 7, 1985–1989. [Google Scholar]
- Qian, Q.; Zhou, H.; Shu, T.; Mu, J.; Fang, Y.; Xu, J.; Li, T.; Kong, J.; Qiu, Y.; Zhou, X. The Capsid Protein of Semliki Forest Virus Antagonizes RNA Interference in Mammalian Cells. J. Virol. 2020, 94, e01233-19. [Google Scholar]
- O’Brien, L. Inhibition of multiple strains of Venezuelan equine encephalitis virus by a pool of four short interfering RNAs. Antivir. Res. 2007, 75, 20–29. [Google Scholar]
- Cross, R.W.; Mire, C.E.; Feldmann, H.; Geisbert, T.W. Post-exposure treatments for Ebola and Marburg virus infections. Nat. Rev. Drug. Discov. 2018, 17, 413–434. [Google Scholar]
- Thi, E.P.; Lee, A.C.; Geisbert, J.B.; Ursic-Bedoya, R.; Agans, K.N.; Robbins, M.; Deer, D.J.; Fenton, K.A.; Kondratowicz, A.S.; MacLachlan, I.; et al. Rescue of non-human primates from advanced Sudan ebolavirus infection with lipid encapsulated siRNA. Nat. Microbiol. 2016, 1, 16142. [Google Scholar]
- Thi, E.P.; Mire, C.E.; Lee, A.C.; Geisbert, J.B.; Zhou, J.Z.; Agans, K.N.; Snead, N.M.; Deer, D.J.; Barnard, T.R.; Fenton, K.A.; et al. Lipid nanoparticle siRNA treatment of Ebola-virus-Makona-infected nonhuman primates. Nature 2015, 521, 362–365. [Google Scholar]
- Mu, J.; Xu, J.; Zhang, L.; Shu, T.; Wu, D.; Huang, M.; Ren, Y.; Li, X.; Geng, Q.; Xu, Y.; et al. SARS-CoV-2-encoded nucleocapsid protein acts as a viral suppressor of RNA interference in cells. Sci. China Life Sci. 2020, 63, 1413–1416. [Google Scholar]
- Samuel, G.H.; Wiley, M.R.; Badawi, A.; Adelman, Z.N.; Myles, K.M. Yellow fever virus capsid protein is a potent suppressor of RNA silencing that binds double-stranded RNA. Proc Natl Acad. Sci USA 2016, 113, 13863–13868. [Google Scholar]
- Zeng, J.; Dong, S.; Luo, Z.; Xie, X.; Fu, B.; Li, P.; Liu, C.; Yang, X.; Chen, Y.; Wang, X.; et al. The Zika Virus Capsid Disrupts Corticogenesis by Suppressing Dicer Activity and miRNA Biogenesis. Cell Stem Cell 2020, 27, 618–632.e9. [Google Scholar]
- Morazzani, E.M.; Compton, J.R.; Leary, D.H.; Berry, A.V.; Hu, X.; Marugan, J.J.; Glass, P.J.; Legler, P.M. Proteolytic cleavage of host proteins by the Group IV viral proteases of Venezuelan equine encephalitis virus and Zika virus. Antivir. Res. 2019, 164, 106–122. [Google Scholar]
- Dash, P.K.; Tiwari, M.; Santhosh, S.R.; Parida, M.; Lakshmana Rao, P.V. RNA interference mediated inhibition of Chikungunya virus replication in mammalian cells. Biochem. Biophys. Res. Commun. 2008, 376, 718–722. [Google Scholar]
- Parashar, D.; Paingankar, M.S.; Kumar, S.; Gokhale, M.D.; Sudeep, A.B.; Shinde, S.B.; Arankalle, V.A. Administration of E2 and NS1 siRNAs inhibit chikungunya virus replication in vitro and protects mice infected with the virus. PLoS Negl. Trop. Dis. 2013, 7, e2405. [Google Scholar]


| siRNA | vsiRNA Sequence (Sense Strand) | Genomic Location | Gene Target |
|---|---|---|---|
| A | GGUCAAAGGUGCAGCUAAA | 4202–4220 | nsP3 |
| B | GGAAAUAACUGAUAAGGAA | 359–377 | nsP1 |
| C | GAGCAAUGGAAGAAAGAUA | 10721–10739 | E1 |
| D | AGGAAUAAUCACUGGGAUA | 3276–3294 | nsP2 |
| F | UGGGAAACGUUUAAAGAAA | 6411–6429 | nsP4 |
| G | UGGAAUGCUUCAAGAAAUA | 6373–6391 | nsP4 |
| H | GGAAAUGACUCUCAAGGAA | 4475–4493 | nsP3 |
| I | UCGCCGUUGCACUAAAUCU | 2576–2594 | nsP2 |
| J | CCAGGAAGGUGGAGAACAU | 5899–5917 | nsP4 |
| K | GAACUUGGCUGGAGCAUAU | 602–620 | nsP1 |
| L | UGAACAAGUCAUAGUGAUA | 1784–1802 | nsP2 |
| M | GAAGAAGAGGAUAGCAUAA | 5160–5178 | nsP3 |
| N | GCGAAUACCUGUACGACAU | 2038–2056 | nsP2 |
| O | AGACUAAGAUUGUGAUUGA | 2656–2674 | nsP2 |
| P | GGUACAAGGUGAAUGAAAA | 2827–2845 | nsP2 |
| Q | GAAAGUGACUCCAGGAACA | 6581–6599 | nsP4 |
| R | CGUUAAUGAUUCUGGAAGA | 6859–6877 | nsP4 |
| S | CGGCGAAAUUUCAUCAAUA | 6923–6941 | nsP4 |
| T | CGAAGAAAGCAUCCAAAUA | 8061–8079 | Capsid |
| U | GGAGAAAGCAUGAGCAGUA | 4752–4770 | nsP3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haikerwal, A.; Barrera, M.D.; Bhalla, N.; Zhou, W.; Boghdeh, N.; Anderson, C.; Alem, F.; Narayanan, A. Inhibition of Venezuelan Equine Encephalitis Virus Using Small Interfering RNAs. Viruses 2022, 14, 1628. https://doi.org/10.3390/v14081628
Haikerwal A, Barrera MD, Bhalla N, Zhou W, Boghdeh N, Anderson C, Alem F, Narayanan A. Inhibition of Venezuelan Equine Encephalitis Virus Using Small Interfering RNAs. Viruses. 2022; 14(8):1628. https://doi.org/10.3390/v14081628
Chicago/Turabian StyleHaikerwal, Amrita, Michael D. Barrera, Nishank Bhalla, Weidong Zhou, Niloufar Boghdeh, Carol Anderson, Farhang Alem, and Aarthi Narayanan. 2022. "Inhibition of Venezuelan Equine Encephalitis Virus Using Small Interfering RNAs" Viruses 14, no. 8: 1628. https://doi.org/10.3390/v14081628






