Modeling Infectious Bursal Disease Virus (IBDV) Antigenic Drift In Vitro
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Lines, Viruses, and Antibodies
2.2. Titration of IBDV in DT40 Cells
2.3. Serial Dilution of Neutralizing Antibodies
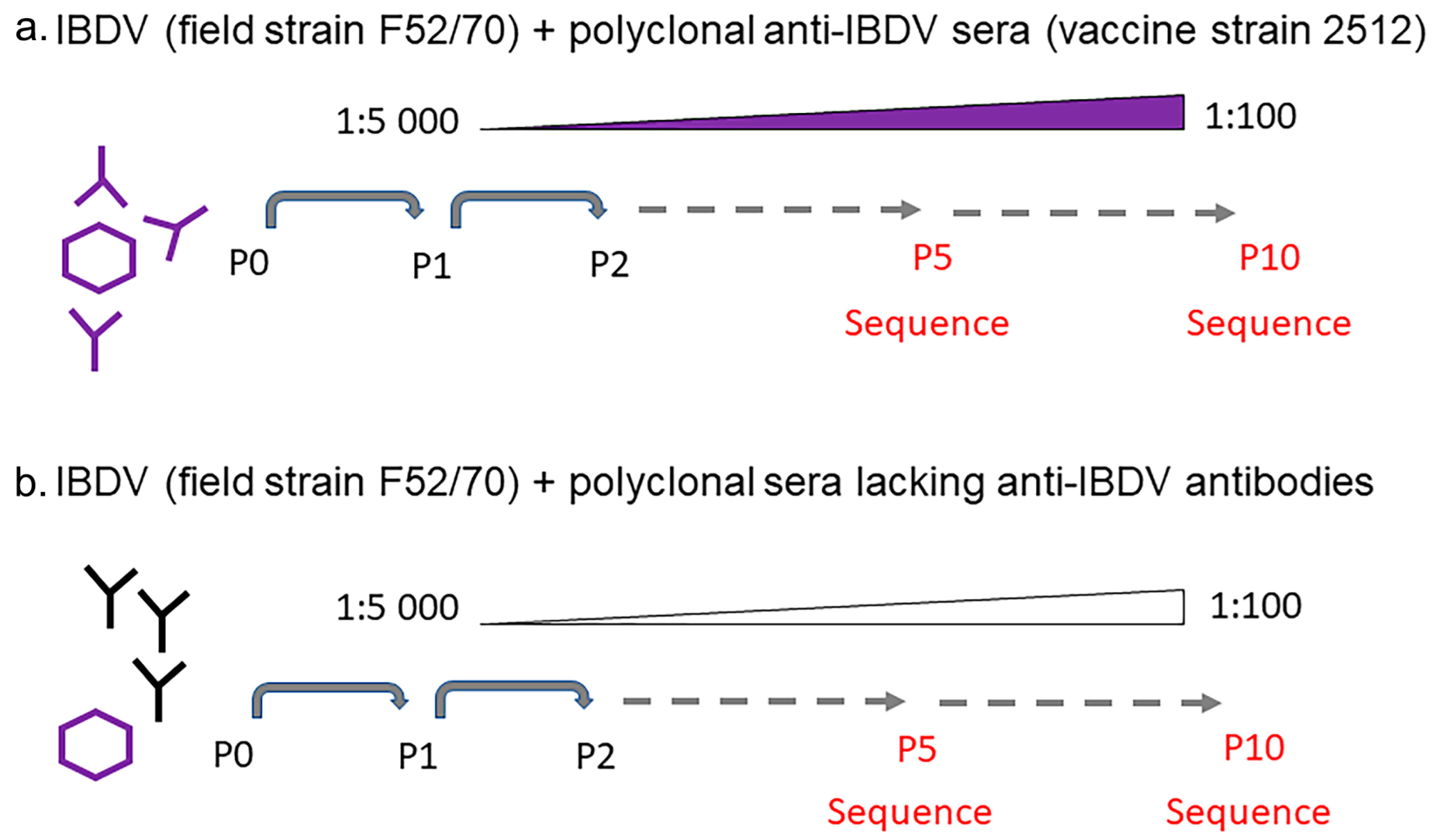
2.4. Generation of Escape Mutants
2.5. Sequencing
2.6. Bioinformatics Analysis of VP2 HVR
2.7. Structural Modelling of Chimeric VP2 Molecules
2.8. Statistical Analysis
2.9. Biosafety
3. Results
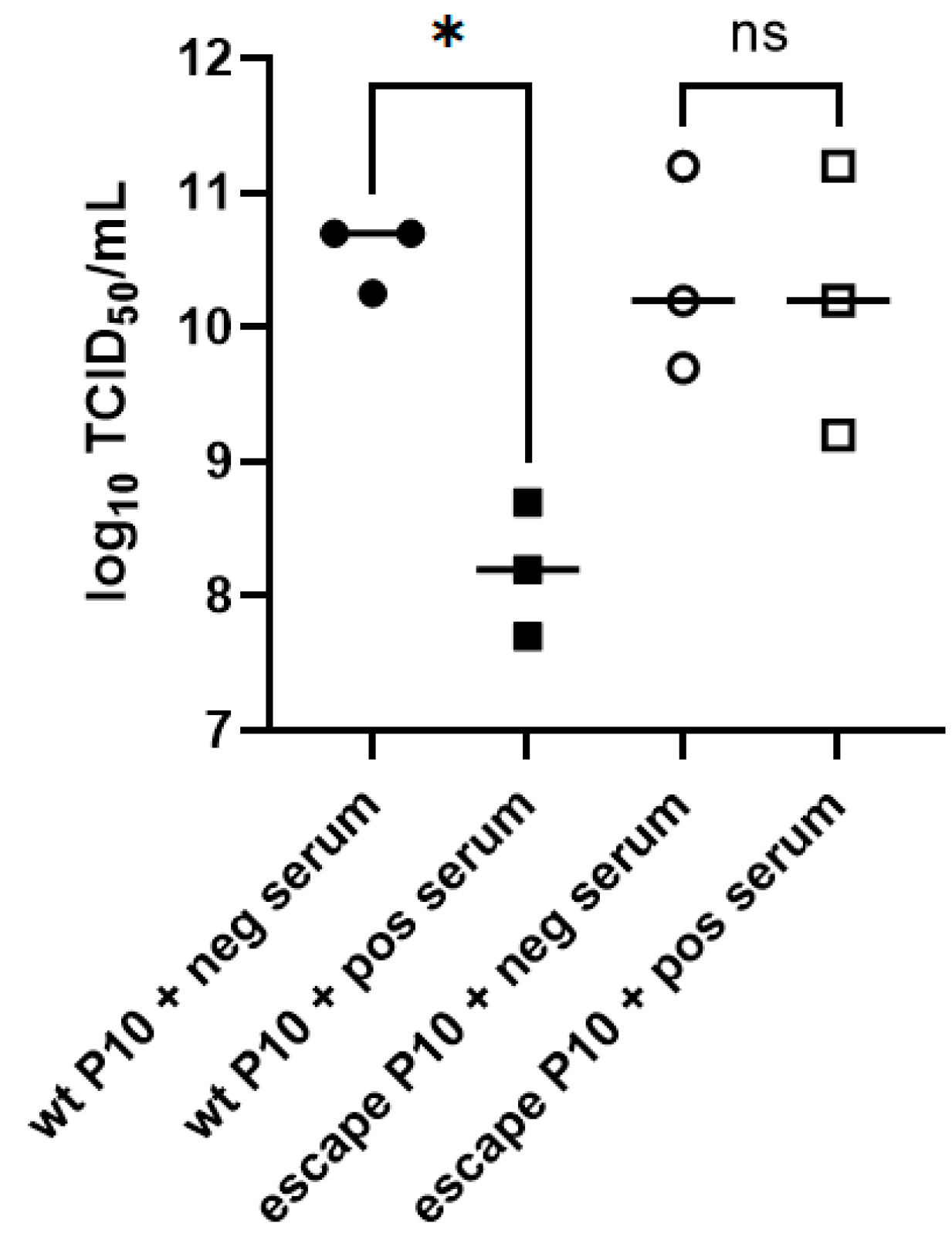
3.1. Serial Passage of F52/70 in Sub-Neutralizing Concentrations of Anti-2512 Serum Led to Immune Escape in DT40 Cells
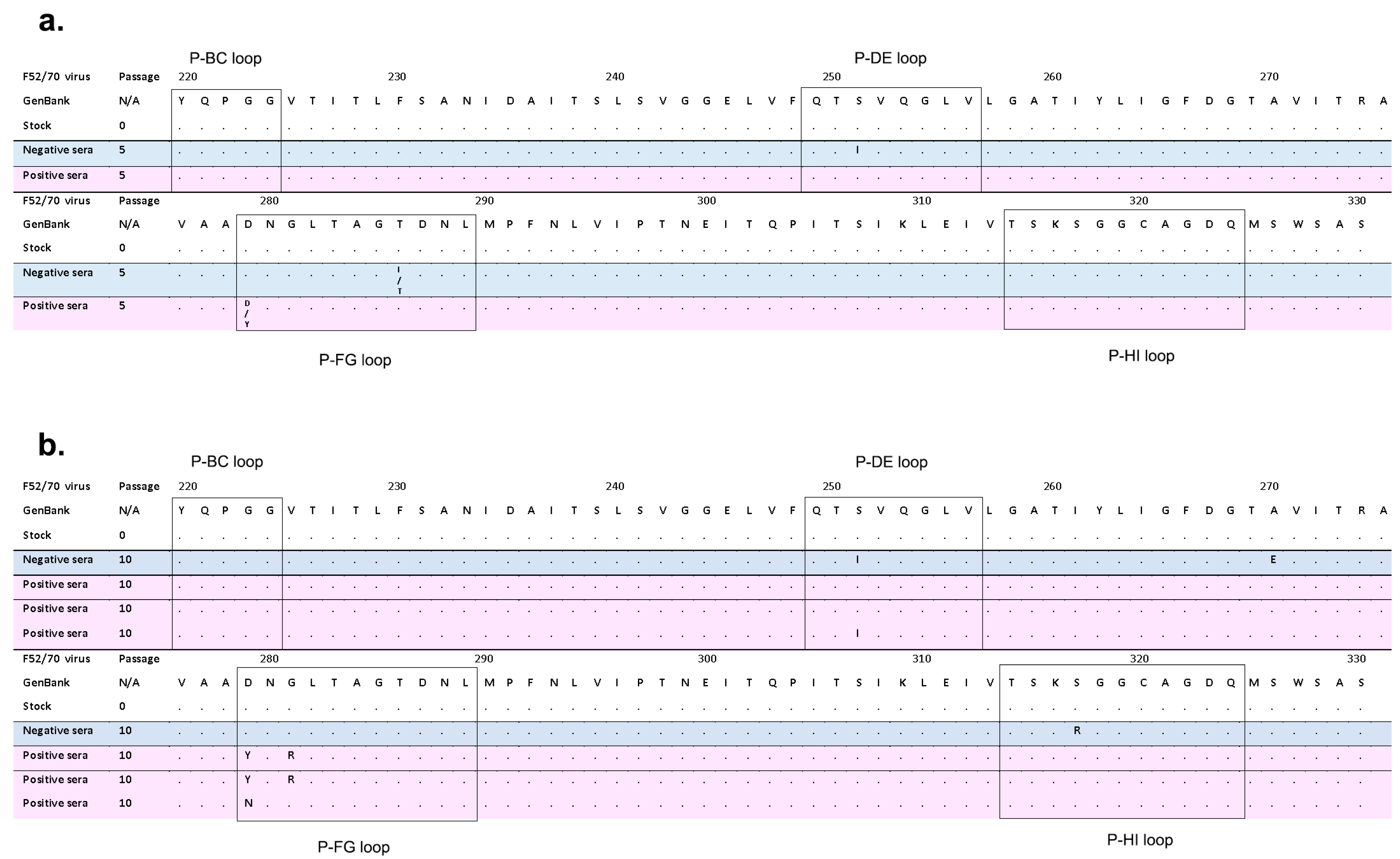
3.2. IBDV F52/70 Immune-Escape Mutants Had Mutations in the HVR
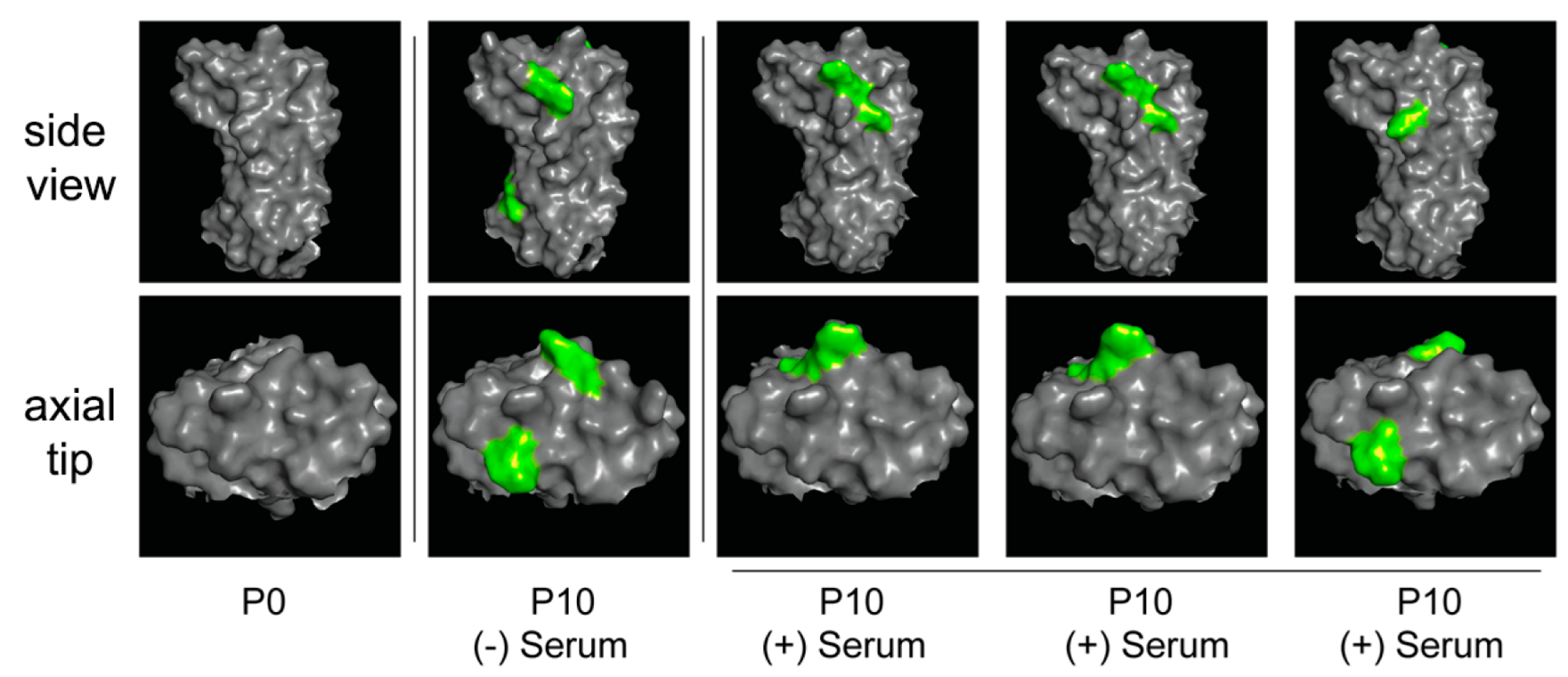
3.3. IBDV F52/70 Immune-Escape Mutants Had Mutations on Both the Side and Axial Tip of the VP2 Molecule
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eterradossi, N.; Saif, Y. Infectious Bursal Disease Virus. In Diseases of Poultry, 14th ed.; Swayne, D., Ed.; John Wiley & Sons, Inc: Hoboken, NJ, USA, 2020. [Google Scholar]
- Letzel, T.; Coulibaly, F.; Rey, F.A.; Delmas, B.; Jagt, E.; van Loon, A.A.; Mundt, E. Molecular and structural bases for the antigenicity of VP2 of infectious bursal disease virus. J. Virol. 2007, 81, 12827–12835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, B.L.; Cao, Y.; Yu, T.; Mo, C.W. Adaptation of very virulent infectious bursal disease virus to chicken embryonic fibroblasts by site-directed mutagenesis of residues 279 and 284 of viral coat protein VP2. J. Virol. 1999, 73, 2854–2862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mundt, E. Tissue culture infectivity of different strains of infectious bursal disease virus is determined by distinct amino acids in VP2. J. Gen. Virol. 1999, 80 Pt 8, 2067–2076. [Google Scholar] [CrossRef] [PubMed]
- van Loon, A.; de Haas, N.; Zeyda, I.; Mundt, E. Alteration of amino acids in VP2 of very virulent infectious bursal disease virus results in tissue culture adaptation and attenuation in chickens. J. Gen. Virol. 2002, 83, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Muller, H.; Mundt, E.; Eterradossi, N.; Islam, M.R. Current status of vaccines against infectious bursal disease. Avian Pathol. 2012, 41, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Birhane, N.; Fesseha, H. Vaccine Failure in Poultry Production and its Control Methods: A Review. Biomed. J. Sci. Tech. Res. 2020, 29, 22588–22596. [Google Scholar] [CrossRef]
- Campbell, E.A.; Reddy, V.; Gray, A.G.; Wells, J.; Simpson, J.; Skinner, M.A.; Hawes, P.C.; Broadbent, A.J. Discrete Virus Factories Form in the Cytoplasm of Cells Coinfected with Two Replication-Competent Tagged Reporter Birnaviruses That Subsequently Coalesce over Time. J. Virol. 2020, 94, e02107-19. [Google Scholar] [CrossRef] [PubMed]
- Pirbright. The UK Immunological Toolbox. Available online: https://www.immunologicaltoolbox.co.uk/search?query=ibdv (accessed on 12 August 2022).
- Wark, K.L. Expression and Processing of Infectious Bursal Disease Virus Proteins; University of Hertfordshire, EThOS: Hertfordshire, UK, 2000. [Google Scholar]
- Reed, R.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 494–497. [Google Scholar]
- Michel, L.O.; Jackwood, D.J. Classification of infectious bursal disease virus into genogroups. Arch. Virol. 2017, 162, 3661–3670. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jumper, J.; Evans, R.; Pritzel, A.; Green, T.; Figurnov, M.; Ronneberger, O.; Tunyasuvunakool, K.; Bates, R.; Zidek, A.; Potapenko, A.; et al. Highly accurate protein structure prediction with AlphaFold. Nature 2021, 596, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Delgui, L.; Gonzalez, D.; Rodriguez, J.F. Infectious bursal disease virus persistently infects bursal B-lymphoid DT40 cells. J. Gen. Virol. 2009, 90, 1148–1152. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.; Nazki, S.; Brodrick, A.J.; Asfor, A.; Urbaniec, J.; Morris, Y.; Broadbent, A.J. Evaluating the Breadth of Neutralizing Antibody Responses Elicited by Infectious Bursal Disease Virus Genogroup A1 Strains Using a Novel Chicken B-Cell Rescue System and Neutralization Assay. J. Virol. 2022, 96, e0125522. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, K.; Hirayama, H.; Kasanga, C.J.; Maw, M.T.; Ohya, K.; Yamaguchi, T.; Fukushi, H. Chicken B lymphoma DT40 cells as a useful tool for in vitro analysis of pathogenic infectious bursal disease virus. J. Vet. Med. Sci. 2008, 70, 407–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azad, A.A.; Jagadish, M.N.; Brown, M.A.; Hudson, P.J. Deletion mapping and expression in Escherichia coli of the large genomic segment of a birnavirus. Virology 1987, 161, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Ali Khan, R.S.; Habib, M.; Ali, W.; Salah Ud Din Shah, M.; Ashraf, A.; Ali Tahir, Z.; Helal, Z.H.; Khan, M.I.; Mahboob, S.; A-Al-Ghanim, K.; et al. Phylogenetic analysis of Infectious Bursal Disease viruses according to newly proposed model of classification into geno-groups. J. Infect. Public Health 2019, 12, 410–418. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asfor, A.S.; Reddy, V.R.A.P.; Nazki, S.; Urbaniec, J.; Brodrick, A.J.; Broadbent, A.J. Modeling Infectious Bursal Disease Virus (IBDV) Antigenic Drift In Vitro. Viruses 2023, 15, 130. https://doi.org/10.3390/v15010130
Asfor AS, Reddy VRAP, Nazki S, Urbaniec J, Brodrick AJ, Broadbent AJ. Modeling Infectious Bursal Disease Virus (IBDV) Antigenic Drift In Vitro. Viruses. 2023; 15(1):130. https://doi.org/10.3390/v15010130
Chicago/Turabian StyleAsfor, Amin S., Vishwanatha R. A. P. Reddy, Salik Nazki, Joanna Urbaniec, Andrew J. Brodrick, and Andrew J. Broadbent. 2023. "Modeling Infectious Bursal Disease Virus (IBDV) Antigenic Drift In Vitro" Viruses 15, no. 1: 130. https://doi.org/10.3390/v15010130
APA StyleAsfor, A. S., Reddy, V. R. A. P., Nazki, S., Urbaniec, J., Brodrick, A. J., & Broadbent, A. J. (2023). Modeling Infectious Bursal Disease Virus (IBDV) Antigenic Drift In Vitro. Viruses, 15(1), 130. https://doi.org/10.3390/v15010130






