A Renaissance for Oncolytic Adenoviruses?
Abstract
:1. Combining Oncolytic Adenovirus with Immune Checkpoint Inhibitors
2. Modifications in the E1A Gene
3. Modification of the E1B Gene
4. Modification of the Fibre Protein
5. Modifications of the E3 Region
6. VA-RNAs
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Martuza, R.L.; Malick, A.; Markert, J.M.; Ruffner, K.L.; Coen, D.M. Experimental therapy of human glioma by means of a genetically engineered virus mutant. Science 1991, 252, 854–856. [Google Scholar] [CrossRef]
- Twumasi-Boateng, K.; Pettigrew, J.L.; Kwok, Y.Y.E.; Bell, J.C.; Nelson, B.H. Oncolytic viruses as engineering platforms for combination immunotherapy. Nat. Rev. Cancer 2018, 18, 419–432. [Google Scholar] [CrossRef] [PubMed]
- Garber, K. China Approves World’s First Oncolytic Virus Therapy For Cancer Treatment. J. Natl. Cancer Inst. 2006, 98, 298–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bischoff, J.R.; Kirn, D.H.; Williams, A.; Heise, C.; Horn, S.; Muna, M.; Ng, L.; Nye, J.A.; Sampson-Johannes, A.; Fattaey, A.; et al. An Adenovirus Mutant That Replicates Selectively in p53- Deficient Human Tumor Cells. Science 1996, 274, 373–376. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, C.C.; Johnson, L.; Bagus, B.; Choi, S.; Nicholas, C.; Shen, A.; Boyle, L.; Pandey, K.; Soria, C.; Kunich, J.; et al. Late viral RNA export, rather than p53 inactivation, determines ONYX-015 tumor selectivity. Cancer Cell 2004, 6, 611–623. [Google Scholar] [CrossRef] [Green Version]
- Mast, T.C.; Kierstead, L.; Gupta, S.B.; Nikas, A.A.; Kallas, E.G.; Novitsky, V.; Mbewe, B.; Pitisuttithum, P.; Schechter, M.; Vardas, E.; et al. International epidemiology of human pre-existing adenovirus (Ad) type-5, type-6, type-26 and type-36 neutralizing antibodies: Correlates of high Ad5 titers and implications for potential HIV vaccine trials. Vaccine 2010, 28, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Steinberg, G.D.; Uchio, E.M.; Lamm, D.L.; Shah, P.; Kamat, A.M.; Bivalacqua, T.; Packiam, V.T.; Chisamore, M.J.; McAdory, J.; et al. CORE1: Phase 2, single-arm study of CG0070 combined with pembrolizumab in patients with nonmuscle-invasive bladder cancer (NMIBC) unresponsive to bacillus Calmette-Guerin (BCG). J. Clin. Oncol. 2022, 40, 4597. [Google Scholar] [CrossRef]
- Lei, J.; Li, Q.H.; Yang, J.L.; Liu, F.; Wang, L.; Xu, W.M.; Zhao, W.X. The antitumor effects of oncolytic adenovirus H101 against lung cancer. Int. J. Oncol. 2015, 47, 555–562. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.H.; Shine, H.D.; Goodman, J.C.; Grossman, R.G.; Woo, S.L. Gene therapy for brain tumors: Regression of experimental gliomas by adenovirus-mediated gene transfer in vivo. Proc. Natl. Acad. Sci. USA 1994, 91, 3054–3057. [Google Scholar] [CrossRef] [Green Version]
- Zheng, H.; Dai, W.; Antonia, S.; Cantwell, M.J.; Beg, A.A. Abstract 4578: Development of MEM-288, a Dual-Transgene Armed and Conditionally Replication-Enhanced Oncolytic Adenovirus with Potent Systemic Antitumor Immunity. 2020. Available online: https://aacrjournals.org/cancerres/article/80/16_Supplement/4578/643321/Abstract-4578-Development-of-MEM-288-a-dual (accessed on 20 November 2022).
- Eriksson, E.; Milenova, I.; Wenthe, J.; Stahle, M.; Leja-Jarblad, J.; Ullenhag, G.; Dimberg, A.; Moreno, R.; Alemany, R.; Loskog, A. Shaping the Tumor Stroma and Sparking Immune Activation by CD40 and 4-1BB Signaling Induced by an Armed Oncolytic Virus. Clin. Cancer Res. 2017, 23, 5846–5857. [Google Scholar] [CrossRef]
- Eriksson, E.; Moreno, R.; Milenova, I.; Liljenfeldt, L.; Dieterich, L.C.; Christiansson, L.; Karlsson, H.; Ullenhag, G.; Mangsbo, S.M.; Dimberg, A.; et al. Activation of myeloid and endothelial cells by CD40L gene therapy supports T-cell expansion and migration into the tumor microenvironment. Gene Ther 2017, 24, 92–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wenthe, J.; Eriksson, E.; Milenova, I.; Moreno, R.; Alemany, R.; Loskog, A. 516. A Novel Oncolytic Adenovirus Expressing Tumor Microenvironment Stimulators to Evoke and Facilitate Anti-Tumor Immune Responses. Cancer-Oncolytic DNA Viruses 2016, 24 (Suppl. 1), S206. [Google Scholar] [CrossRef]
- Burke, J.M.; Lamm, D.L.; Meng, M.V.; Nemunaitis, J.J.; Stephenson, J.J.; Arseneau, J.C.; Aimi, J.; Lerner, S.; Yeung, A.W.; Kazarian, T.; et al. A first in human phase 1 study of CG0070, a GM-CSF expressing oncolytic adenovirus, for the treatment of nonmuscle invasive bladder cancer. J. Urol. 2012, 188, 2391–2397. [Google Scholar] [CrossRef] [PubMed]
- Hedjran, F.; Shantanu, K.; Tony, R. Deletion analysis of Ad5 E1a transcriptional control region: Impact on tumor-selective expression of E1a and E1b. Cancer Gene Ther. 2011, 18, 717–723. [Google Scholar] [CrossRef] [Green Version]
- Larson, C.; Oronsky, B.; Abrouk, N.E.; Oronsky, A.; Reid, T.R. Toxicology and biodistribution of AdAPT-001, a replication-competent type 5 adenovirus with a trap for the immunosuppressive cytokine, TGF-beta. Am. J. Cancer Res. 2021, 11, 5184–5189. [Google Scholar]
- Kawashima, T.; Kagawa, S.; Kobayashi, N.; Shirakiya, Y.; Umeoka, T.; Teraishi, F.; Taki, M.; Kyo, S.; Tanaka, N.; Fujiwara, T. Telomerase-specific replication-selective virotherapy for human cancer. Clin. Cancer Res. 2004, 10, 285–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamasaki, Y.; Tazawa, H.; Hashimoto, Y.; Kojima, T.; Kuroda, S.; Yano, S.; Yoshida, R.; Uno, F.; Mizuguchi, H.; Ohtsuru, A.; et al. A novel apoptotic mechanism of genetically engineered adenovirus-mediated tumour-specific p53 overexpression through E1A-dependent p21 and MDM2 suppression. Eur. J. Cancer 2012, 48, 2282–2291. [Google Scholar] [CrossRef] [Green Version]
- Kuhn, I.; Harden, P.; Bauzon, M.; Chartier, C.; Nye, J.; Thorne, S.; Reid, T.; Ni, S.; Lieber, A.; Fisher, K.; et al. Directed evolution generates a novel oncolytic virus for the treatment of colon cancer. PLoS ONE 2008, 3, e2409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
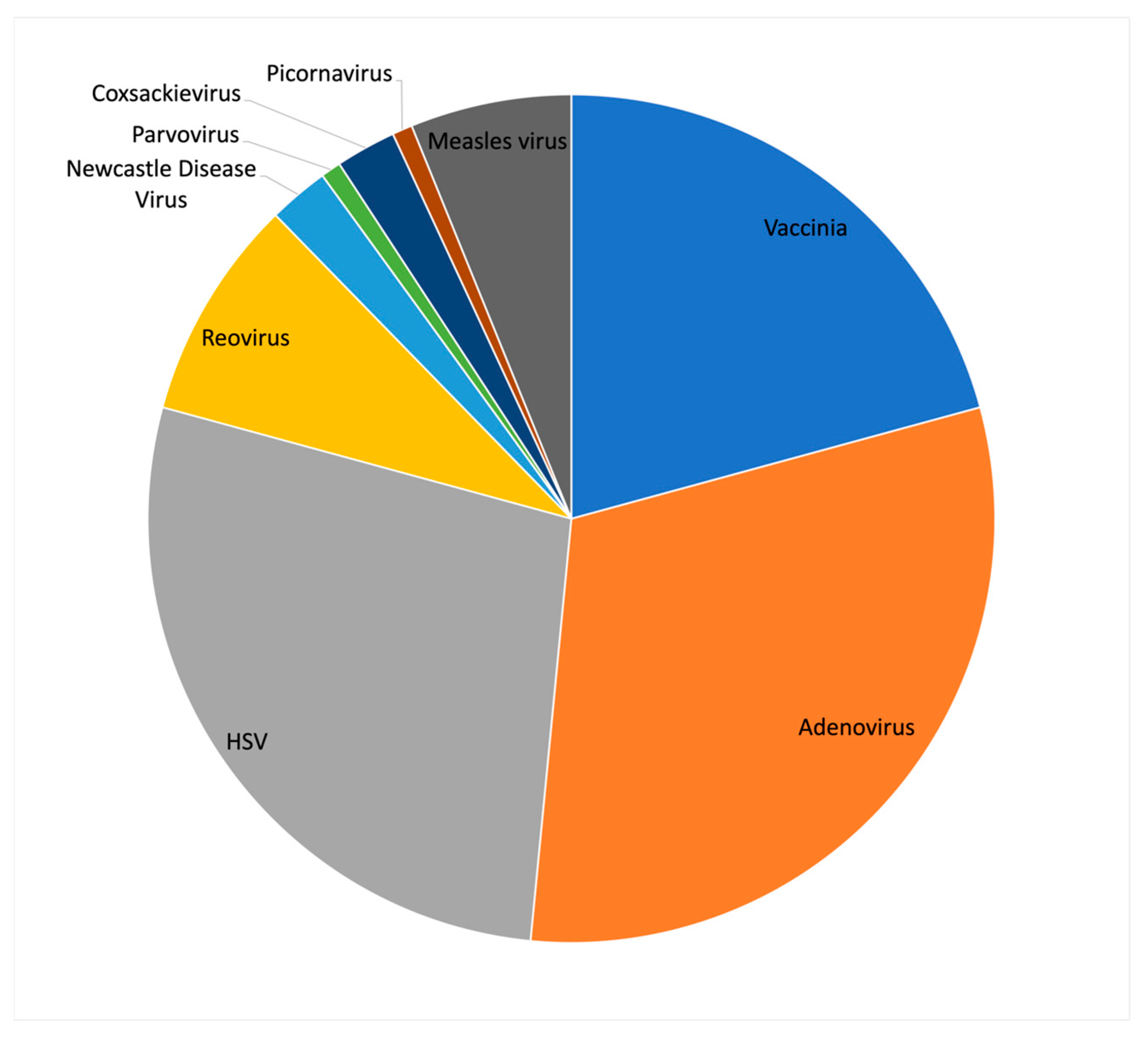
- Hernandez-Aiguirre, I.; Cassady, K.A. Chapter Twelve - Oncolytic viruses in immunotherapy. In Cancer Immunology and Immunotherapy; Amiji, M.M., Scheherazade Milane, L., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 375–437. [Google Scholar]
- Lang, F.F.; Conrad, C.; Gomez-Manzano, C.; Yung, W.K.A.; Sawaya, R.; Weinberg, J.S.; Prabhu, S.S.; Rao, G.; Fuller, G.N.; Aldape, K.D.; et al. Phase I Study of DNX-2401 (Delta-24-RGD) Oncolytic Adenovirus: Replication and Immunotherapeutic Effects in Recurrent Malignant Glioma. J. Clin. Oncol. 2018, 36, 1419–1427. [Google Scholar] [CrossRef]
- Kanerva, A.; Zinn, K.R.; Chaudhuri, T.R.; Lam, J.T.; Suzuki, K.; Uil, T.G.; Hakkarainen, T.; Bauerschmitz, G.J.; Wang, M.; Liu, B.; et al. Enhanced therapeutic efficacy for ovarian cancer with a serotype 3 receptor-targeted oncolytic adenovirus. Mol. Ther. 2003, 8, 449–458. [Google Scholar] [CrossRef]
- Koski, A.; Kangasniemi, L.; Escutenaire, S.; Pesonen, S.; Cerullo, V.; Diaconu, I.; Nokisalmi, P.; Raki, M.; Rajecki, M.; Guse, K.; et al. Treatment of cancer patients with a serotype 5/3 chimeric oncolytic adenovirus expressing GMCSF. Mol. Ther. 2010, 18, 1874–1884. [Google Scholar] [CrossRef] [PubMed]
- Siurala, M.; Bramante, S.; Vassilev, L.; Hirvinen, M.; Parviainen, S.; Tahtinen, S.; Guse, K.; Cerullo, V.; Kanerva, A.; Kipar, A.; et al. Oncolytic adenovirus and doxorubicin-based chemotherapy results in synergistic antitumor activity against soft-tissue sarcoma. Int. J. Cancer 2015, 136, 945–954. [Google Scholar] [CrossRef] [PubMed]
- Havunen, R.; Kalliokoski, R.; Siurala, M.; Sorsa, S.; Santos, J.M.; Cervera-Carrascon, V.; Anttila, M.; Hemminki, A. Cytokine-Coding Oncolytic Adenovirus TILT-123 Is Safe, Selective, and Effective as a Single Agent and in Combination with Immune Checkpoint Inhibitor Anti-PD-1. Cells 2021, 10. [Google Scholar] [CrossRef]
- Atherton, M.J.; Stephenson, K.B.; Nikota, J.K.; Hu, Q.N.; Nguyen, A.; Wan, Y.; Lichty, B.D. Preclinical development of peptide vaccination combined with oncolytic MG1-E6E7 for HPV-associated cancer. Vaccine 2018, 36, 2181–2192. [Google Scholar] [CrossRef]
- Jonker, D.J.; Hotte, S.J.; Razak, A.R.A.; Renouf, D.J.; Lichty, B.; Bell, J.C.; Powers, J.; Breitbach, C.J.; Stojdl, D.F.; Stephenson, K.B.; et al. Phase I study of oncolytic virus (OV) MG1 maraba/MAGE-A3 (MG1MA3), with and without transgenic MAGE-A3 adenovirus vaccine (AdMA3) in incurable advanced/metastatic MAGE-A3-expressing solid tumours: CCTG IND.214. J. Clin. Oncol. 2017, 35, e14637. [Google Scholar] [CrossRef]
- Farrera-Sal, M.; Moreno, R.; Mato-Berciano, A.; Maliandi, M.V.; Bazan-Peregrino, M.; Alemany, R. Hyaluronidase expression within tumors increases virotherapy efficacy and T cell accumulation. Mol. Ther. Oncolytics. 2021, 22, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Ulasov, I.V.; Zhu, Z.B.; Tyler, M.A.; Han, Y.; Rivera, A.A.; Khramtsov, A.; Curiel, D.T.; Lesniak, M.S. Survivin-driven and fiber-modified oncolytic adenovirus exhibits potent antitumor activity in established intracranial glioma. Hum. Gene Ther. 2007, 18, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; van Ginkel, J.W.; Au, K.Y.; Alemany, R.; Meulenberg, J.J.; van Beusechem, V.W. ORCA-010, a novel potency-enhanced oncolytic adenovirus, exerts strong antitumor activity in preclinical models. Hum. Gene Ther. 2014, 25, 897–904. [Google Scholar] [CrossRef] [Green Version]
- Klawitter, M.; El-Ayoubi, A.; Buch, J.; Rüttinger, J.; Ehrenfeld, M.; Lichtenegger, E.; Krüger, M.A.; Mantwill, K.; Koll, F.J.; Kowarik, M.C.; et al. The Oncolytic Adenovirus XVir-N-31, in Combination with the Blockade of the PD-1/PD-L1 Axis, Conveys Abscopal Effects in a Humanized Glioblastoma Mouse Model. Int. J. Mol. Sci. 2022, 23, 9965. [Google Scholar] [CrossRef]
- Zhao, Q.; Tong, J.; Liu, X.; Li, S.; Chen, D.; Miao, L. Reversing resistance to immune checkpoint inhibitor by adding recombinant human adenovirus type 5 in a patient with small cell lung cancer with promoted immune infiltration: A case report. J. Cancer Res. Clin. Oncol. 2022, 148, 1269–1273. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, H.; Shan, M.; Chen, H.; Xu, B.; He, Y.; Zhao, Y.; Liu, Z.; Chen, J.; Xu, Q. Oncolytic adenovirus H101 ameliorate the efficacy of anti-PD -1 monotherapy in colorectal cancer. Cancer Med. 2022, 11, 4575–4587. [Google Scholar] [CrossRef] [PubMed]
- Heiniö, C.; Clubb, J.; Kudling, T.; Quixabeira, D.; Cervera-Carrascon, V.; Havunen, R.; Grönberg-Vähä-Koskela, S.; Santos, J.M.; Tapper, J.; Kanerva, A.; et al. Effective Combination Immunotherapy with Oncolytic Adenovirus and Anti-PD-1 for Treatment of Human and Murine Ovarian Cancers. Diseases 2022, 10, 52. [Google Scholar] [CrossRef] [PubMed]
- Clubb, J.H.A.; Kudling, T.V.; Heiniö, C.; Basnet, S.; Pakola, S.; Cervera Carrascón, V.; Santos, J.M.; Quixabeira, D.C.A.; Havunen, R.; Sorsa, S.; et al. Adenovirus Encoding Tumor Necrosis Factor Alpha and Interleukin 2 Induces a Tertiary Lymphoid Structure Signature in Immune Checkpoint Inhibitor Refractory Head and Neck Cancer. Front. Immunol. 2022, 13, 794251. [Google Scholar] [CrossRef]
- Quixabeira, D.C.A.; Cervera-Carrascon, V.; Santos, J.M.; Clubb, J.H.; Kudling, T.V.; Basnet, S.; Heiniö, C.; Grönberg-Vähä-Koskela, S.; Anttila, M.; Havunen, R.; et al. Local therapy with an engineered oncolytic adenovirus enables antitumor response in non-injected melanoma tumors in mice treated with aPD-1. Oncoimmunology 2022, 11, 2028960. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Xie, W.; Zhang, Y.; Dong, X.; Liu, C.; Yi, J.; Zhang, S.; Wen, C.; Zheng, L.; Wang, H. Oncolytic adenoviruses synergistically enhance anti-PD-L1 and anti-CTLA-4 immunotherapy by modulating the tumour microenvironment in a 4T1 orthotopic mouse model. Cancer Gene Ther. 2022, 29, 456–465. [Google Scholar] [CrossRef]
- Jung, B.K.; Ko, H.Y.; Kang, H.; Hong, J.; Ahn, H.M.; Na, Y.; Kim, H.; Kim, J.S.; Yun, C.O. Relaxin-expressing oncolytic adenovirus induces remodeling of physical and immunological aspects of cold tumor to potentiate PD-1 blockade. J. Immunother. Cancer 2020, 8, e000763. [Google Scholar] [CrossRef]
- Ackrill, A.M.; Foster, G.R.; Laxton, C.D.; Flavell, D.M.; Stark, G.R.; Kerr, I.M. Inhibition of the cellular response to interferons by products of the adenovirus type 5 E1A oncogene. Nucleic Acids Res. 1991, 19, 4387–4393. [Google Scholar] [CrossRef] [Green Version]
- Gutch, M.J.; Reich, N.C. Repression of the interferon signal transduction pathway by the adenovirus E1A oncogene. Proc. Natl. Acad. Sci. USA 1991, 88, 7913–7917. [Google Scholar] [CrossRef] [Green Version]
- Kalvakolanu, D.V.; Bandyopadhyay, S.K.; Harter, M.L.; Sen, G.C. Inhibition of interferon-inducible gene expression by adenovirus E1A proteins: Block in transcriptional complex formation. Proc. Natl. Acad. Sci. USA 1991, 88, 7459–7463. [Google Scholar] [CrossRef] [Green Version]
- Aparicio, O.; Razquin, N.; Zaratiegui, M.; Narvaiza, I.; Fortes, P. Adenovirus Virus-Associated RNA Is Processed to Functional Interfering RNAs Involved in Virus Production. J. Virol. 2006, 80, 1376–1384. [Google Scholar] [CrossRef] [Green Version]
- Kitajewski, J.; Schneider, R.J.; Safer, B.; Munemitsu, S.M.; Samuel, C.E.; Thimmappaya, B.; Shenk, T. Adenovirus VAI RNA antagonizes the antiviral action of interferon by preventing activation of the interferon-induced eIF-2α kinase. Cell 1986, 45, 195–200. [Google Scholar] [CrossRef]
- O’Malley, R.P.; Mariano, T.M.; Siekierka, J.; Mathews, M.B. A mechanism for the control of protein synthesis by adenovirus VA RNAI. Cell 1986, 44, 391–400. [Google Scholar] [CrossRef]
- Fueyo, J.; Gomez-Manzano, C.; Alemany, R.; Lee, P.S.; McDonnell, T.J.; Mitlianga, P.; Shi, Y.-X.; A Levin, V.; Yung, W.K.A.; Kyritsis, A.P. A mutant oncolytic adenovirus targeting the Rb pathway produces anti-glioma effect in vivo. Oncogene 2000, 19, 2–12. [Google Scholar] [CrossRef] [Green Version]
- Yan, Y.; Xu, Y.; Zhao, Y.; Li, L.; Sun, P.; Liu, H.; Fan, Q.; Liang, K.; Liang, W.; Sun, H.; et al. Combination of E2F-1 promoter-regulated oncolytic adenovirus and cytokine-induced killer cells enhances the antitumor effects in an orthotopic rectal cancer model. Tumor Biol. 2014, 35, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, G.J.; Cohen, M.J.; Nichols, A.C.; Barrett, J.W.; Mymryk, J.S. Viral Retasking of hBre1/RNF20 to Recruit hPaf1 for Transcriptional Activation. PLoS Pathog. 2013, 9, e1003411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonseca, G.J.; Thillainadesan, G.; Yousef, A.F.; Ablack, J.N.; Mossman, K.L.; Torchia, J.; Mymryk, J.S. Adenovirus Evasion of Interferon-Mediated Innate Immunity by Direct Antagonism of a Cellular Histone Posttranslational Modification. Cell Host Microbe 2012, 11, 597–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berhane, S.; Aresté, C.; Ablack, J.N.; Ryan, G.B.; Blackbourn, D.J.; Mymryk, J.S.; Turnell, A.S.; Steele, J.C.; Grand, R.J. Adenovirus E1A interacts directly with, and regulates the level of expression of, the immunoproteasome component MECL1. Virology 2011, 421, 149–158. [Google Scholar] [CrossRef] [Green Version]
- Zemke, N.R.; Berk, A.J. The Adenovirus E1A C Terminus Suppresses a Delayed Antiviral Response and Modulates RAS Signaling. Cell Host Microbe 2017, 22, 789–800. [Google Scholar] [CrossRef] [Green Version]
- Hidalgo, P.; Ip, W.H.; Dobner, T.; Gonzalez, R.A. The biology of the adenovirus E1B 55K protein. FEBS Lett. 2019, 593, 3504–3517. [Google Scholar] [CrossRef]
- Dix, B.R.; Edwards, S.J.; Braithwaite, A.W. Does the Antitumor Adenovirus ONYX-015/dl1520 Selectively Target Cells Defective in the p53 Pathway? J. Virol. 2001, 75, 5443–5447. [Google Scholar] [CrossRef] [Green Version]
- McCormick, F. Cancer-specific viruses and the development of ONYX-015. Cancer Biol. Ther. 2003, 2, S157–S160. [Google Scholar] [CrossRef] [PubMed]
- Degenhardt, K.; Perez, D.; White, E. Pathways used by adenovirus E1B 19K to inhibit apoptosis. Symp. Soc. Exp. Biol. 2000, 52, 241–251. [Google Scholar]
- White, E.; Grodzicker, T.; Stillman, B.W. Mutations in the gene encoding the adenovirus early region 1B 19,000-molecular-weight tumor antigen cause the degradation of chromosomal DNA. J. Virol. 1984, 52, 410–419. [Google Scholar] [CrossRef] [Green Version]
- Radke, J.R.; Grigera, F.; Ucker, D.S.; Cook, J.L. Adenovirus E1B 19-Kilodalton Protein Modulates Innate Immunity through Apoptotic Mimicry. J. Virol. 2014, 88, 2658–2669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergelson, J.M.; Cunningham, J.A.; Droguett, G.; Kurt-Jones, E.A.; Krithivas, A.; Hong, J.S.; Horwitz, M.S.; Crowell, R.L.; Finberg, R.W. Isolation of a Common Receptor for Coxsackie B Viruses and Adenoviruses 2 and 5. Science 1997, 275, 1320–1323. [Google Scholar] [CrossRef] [PubMed]
- Wickham, T.J.; Mathias, P.; Cheresh, D.A.; Nemerow, G.R. Integrins αvβ3 and αvβ5 promote adenovirus internalization but not virus attachment. Cell 1993, 73, 309–319. [Google Scholar] [CrossRef]
- Rebel, V.I.; Hartnett, S.; Denham, J.; Chan, M.; Finberg, R.; Sieff, C.A. Maturation and Lineage-Specific Expression of the Coxsackie and Adenovirus Receptor in Hematopoietic Cells. STEM CELLS 2000, 18, 176–182. [Google Scholar] [CrossRef]
- Korn, W.M.; Macal, M.; Christian, C.; Lacher, M.D.; McMillan, A.; Rauen, K.A.; Warren, R.S.; Ferrell, L. Expression of the coxsackievirus- and adenovirus receptor in gastrointestinal cancer correlates with tumor differentiation. Cancer Gene Ther. 2006, 13, 792–797. [Google Scholar] [CrossRef]
- Okegawa, T.; Pong, R.C.; Li, Y.; Bergelson, J.M.; Sagalowsky, A.I.; Hsieh, J.T. The mechanism of the growth-inhibitory effect of coxsackie and adenovirus receptor (CAR) on human bladder cancer: A functional analysis of car protein structure. Cancer Res. 2001, 61, 6592–6600. [Google Scholar]
- A Rauen, K.; Sudilovsky, D.; Le, J.L.; Chew, K.L.; Hann, B.; Weinberg, V.; Schmitt, L.D.; McCormick, F. Expression of the coxsackie adenovirus receptor in normal prostate and in primary and metastatic prostate carcinoma: Potential relevance to gene therapy. Cancer Res. 2002, 62, 3812–3818. [Google Scholar]
- Reeh, M.; Bockhorn, M.; Görgens, D.; Vieth, M.; Hoffmann, T.; Simon, R.; Izbicki, J.R.; Sauter, G.; Schumacher, U.; Anders, M. Presence of the Coxsackievirus and Adenovirus Receptor (CAR) in human neoplasms: A multitumour array analysis. Br. J. Cancer 2013, 109, 1848–1858. [Google Scholar] [CrossRef]
- Stecker, K.; Vieth, M.; Koschel, A.; Wiedenmann, B.; Röcken, C.; Anders, M. Impact of the coxsackievirus and adenovirus receptor on the adenoma–carcinoma sequence of colon cancer. Br. J. Cancer 2011, 104, 1426–1433. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.H.; Song, L.B.; Wu, X.J.; Li, R.P.; Zeng, M.S.; Zhu, X.F.; Wan, D.S.; Liu, Q.; Zeng, Y.X.; Zhang, X.S. Proteasome inhibitor MG-132 modifies coxsackie and adenovirus receptor expression in colon cancer cell line lovo. Cell Cycle 2008, 7, 925–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Persson, B.D.; Reiter, D.M.; Marttila, M.; Mei, Y.F.; Casasnovas, J.M.; Arnberg, N.; Stehle, T. Adenovirus type 11 binding alters the conformation of its receptor CD46. Nat. Struct. Mol. Biol. 2007, 14, 164–166. [Google Scholar] [CrossRef]
- Segerman, A.; Atkinson, J.P.; Marttila, M.; Dennerquist, V.; Wadell, G.; Arnberg, N. Adenovirus Type 11 Uses CD46 as a Cellular Receptor. J. Virol. 2003, 77, 9183–9191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trinh, H.V.; Lesage, G.; Chennamparampil, V.; Vollenweider, B.; Burckhardt, C.J.; Schauer, S.; Havenga, M.; Greber, U.F.; Hemmi, S. Avidity Binding of Human Adenovirus Serotypes 3 and 7 to the Membrane Cofactor CD46 Triggers Infection. J. Virol. 2012, 86, 1623–1637. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Li, Z.-Y.; Liu, Y.; Persson, J.; Beyer, I.; Möller, T.; Koyuncu, D.; Drescher, M.R.; Strauss, R.; Zhang, X.-B.; et al. Desmoglein 2 is a receptor for adenovirus serotypes 3, 7, 11 and 14. Nat. Med. 2010, 17, 96–104. [Google Scholar] [CrossRef]
- Elvington, M.; Liszewski, M.K.; Atkinson, J.P. CD46 and Oncologic Interactions: Friendly Fire against Cancer. Antibodies 2021, 9, 59. [Google Scholar] [CrossRef]
- Abbod, M.F.; Hamdy, F.C.; Linkens, D.A.; Catto, J.W. Predictive modeling in cancer: Where systems biology meets the stock market. Expert Rev. Anticancer. Ther. 2009, 9, 867–870. [Google Scholar] [CrossRef] [Green Version]
- Biedermann, K.; Vogelsang, H.; Becker, I.; Plaschke, S.; Siewert, J.R.; Höfler, H.; Keller, G. Desmoglein 2 is expressed abnormally rather than mutated in familial and sporadic gastric cancer. J. Pathol. 2005, 207, 199–206. [Google Scholar] [CrossRef]
- Harada, H.; Iwatsuki, K.; Ohtsuka, M.; Han, G.W.; Kaneko, F. Abnormal desmoglein expression by squamous cell carcinoma cells. Acta Derm. Venereol. 1996, 76, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Kemper, C.; Leung, M.; Stephensen, C.B.; Pinkert, C.A.; Liszewski, M.K.; Cattaneo, R.; Atkinson, J.P. Membrane cofactor protein (MCP; CD46) expression in transgenic mice. Clin. Exp. Immunol. 2001, 124, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, C.J.; Franke, W.W.; Goerdt, S.; Falkowska-Hansen, B.; Rickelt, S.; Peitsch, W.K. Homo- and Heterotypic Cell Contacts in Malignant Melanoma Cells and Desmoglein 2 as a Novel Solitary Surface Glycoprotein. J. Investig. Dermatol. 2007, 127, 2191–2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shang, Y.; Chai, N.; Gu, Y.; Ding, L.; Yang, Y.; Zhou, J.; Ren, G.; Hao, X.; Fan, D.; Wu, K.; et al. Systematic Immunohistochemical Analysis of the Expression of CD46, CD55, and CD59 in Colon Cancer. Arch. Pathol. Lab. Med. 2014, 138, 910–919. [Google Scholar] [CrossRef] [PubMed]
- Surowiak, P.; Materna, V.; Maciejczyk, A.; Kaplenko, I.; Spaczynski, M.; Dietel, M.; Lage, H.; Zabel, M. CD46 expression is indicative of shorter revival-free survival for ovarian cancer patients. Anticancer. Res. 2007, 26, 4943–4948. [Google Scholar]
- Thorsteinsson, L.; O’Dowd, G.M.; Harrington, P.M.; Johnson, P.M. The complement regulatory proteins CD46 and CD59, but not CD55, are highly expressed by glandular epithelium of human breast and colorectal tumour tissues. Apmis 1998, 106, 869–878. [Google Scholar] [CrossRef]
- Trojan, L.; Schaaf, A.; Steidler, A.; Haak, M.; Thalmann, G.; Knoll, T.; Gretz, N.; Alken, P.; Michel, M.S. Identification of metastasis-associated genes in prostate cancer by genetic profiling of human prostate cancer cell lines. Anticancer. Res. 2005, 25, 183–191. [Google Scholar] [CrossRef]
- Nilsson, M.; Ljungberg, J.; Richter, J.; Kiefer, T.; Magnusson, M.; Lieber, A.; Widegren, B.; Karlsson, S.; Fan, X. Development of an adenoviral vector system with adenovirus serotype 35 tropism; efficient transient gene transfer into primary malignant hematopoietic cells. J. Gene Med. 2004, 6, 631–641. [Google Scholar] [CrossRef]
- Campbell, M.; Qu, S.; Wells, S.; Sugandha, H.; Jensen, R.A. An adenoviral vector containing an arg–gly–asp (RGD) motif in the fiber knob enhances protein product levels from transgenes refractory to expression. Cancer Gene Ther. 2003, 10, 559–570. [Google Scholar] [CrossRef] [Green Version]
- Dmitriev, I.; Krasnykh, V.; Miller, C.R.; Wang, M.; Kashentseva, E.; Mikheeva, G.; Belousova, N.; Curiel, D.T. An Adenovirus Vector with Genetically Modified Fibers Demonstrates Expanded Tropism via Utilization of a Coxsackievirus and Adenovirus Receptor-Independent Cell Entry Mechanism. J. Virol. 1998, 72, 9706–9713. [Google Scholar] [CrossRef] [Green Version]
- Wu, H.; Seki, T.; Dmitriev, I.; Uil, T.; Kashentseva, E.; Han, T.; Curiel, D.T. Double Modification of Adenovirus Fiber with RGD and Polylysine Motifs Improves Coxsackievirus–Adenovirus Receptor-Independent Gene Transfer Efficiency. Hum. Gene Ther. 2002, 13, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.J., Jr.; Lewis, A.M., Jr. Use of Nondefective Adenovirus-Simian Virus 40 Hybrids for Mapping the Simian Virus 40 Genome. J. Virol. 1973, 12, 643–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, N.; Shenk, T. Isolation of deletion and substitution mutants of adenovirus type 5. Cell 1978, 13, 181–188. [Google Scholar] [CrossRef]
- Lichtenstein, D.L.; Toth, K.; Doronin, K.; Tollefson, A.E.; Wold, W.S. Functions and Mechanisms of Action of the Adenovirus E3 Proteins. Int. Rev. Immunol. 2004, 23, 75–111. [Google Scholar] [CrossRef] [PubMed]
- Benedict, C.A.; Norris, P.S.; Prigozy, T.I.; Bodmer, J.L.; Mahr, J.A.; Garnett, C.T.; Martinon, F.; Tschopp, J.; Gooding, L.R.; Ware, C.F. Three Adenovirus E3 Proteins Cooperate to Evade Apoptosis by Tumor Necrosis Factor-related Apoptosis-inducing Ligand Receptor-1 and -2. J. Biol. Chem. 2001, 276, 3270–3278. [Google Scholar] [CrossRef] [PubMed]
- Elsing, A.; Burgert, H.-G. The adenovirus E3/10.4K–14.5K proteins down-modulate the apoptosis receptor Fas/Apo-1 by inducing its internalization. Proc. Natl. Acad. Sci. USA 1998, 95, 10072–10077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNees, A.L.; Garnett, C.T.; Gooding, L.R. The Adenovirus E3 RID Complex Protects Some Cultured Human T and B Lymphocytes from Fas-Induced Apoptosis. J. Virol. 2002, 76, 9716–9723. [Google Scholar] [CrossRef] [Green Version]
- Shisler, J.; Yang, C.; Walter, B.; Ware, C.F.; Gooding, L.R. The adenovirus E3-10.4K/14.5K complex mediates loss of cell surface Fas (CD95) and resistance to Fas-induced apoptosis. J. Virol. 1997, 71, 8299–8306. [Google Scholar] [CrossRef] [Green Version]
- Tollefson, A.E.; Hermiston, T.W.; Lichtenstein, D.L.; Colle, C.F.; Tripp, R.A.; Dimitrov, T.; Toth, K.; Wells, C.E.; Doherty, P.C.; Wold, W.S. Forced degradation of Fas inhibits apoptosis in adenovirus-infected cells. Nature 1998, 392, 726–730. [Google Scholar] [CrossRef]
- Tollefson, A.E.; Toth, K.; Doronin, K.; Kuppuswamy, M.; Doronina, O.A.; Lichtenstein, D.L.; Hermiston, T.W.; Smith, C.A.; Wold, W.S. Inhibition of TRAIL-Induced Apoptosis and Forced Internalization of TRAIL Receptor 1 by Adenovirus Proteins. J. Virol. 2001, 75, 8875–8887. [Google Scholar] [CrossRef] [Green Version]
- Gooding, L.R.; Aquino, L.; Duerksen-Hughes, P.J.; Day, D.; Horton, T.M.; Yei, S.P.; Wold, W.S. The E1B 19,000-molecular-weight protein of group C adenoviruses prevents tumor necrosis factor cytolysis of human cells but not of mouse cells. J. Virol. 1991, 65, 3083–3094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krajcsi, P.; Dimitrov, T.; Hermiston, T.W.; E Tollefson, A.; Ranheim, T.S.; Vande Pol, S.B.; Stephenson, A.H.; Wold, W.S. The adenovirus E3-14.7K protein and the E3-10.4K/14.5K complex of proteins, which independently inhibit tumor necrosis factor (TNF)-induced apoptosis, also independently inhibit TNF-induced release of arachidonic acid. J. Virol. 1996, 70, 4904–4913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wold, W.S.; Doronin, K.; Toth, K.; Kuppuswamy, M.; Lichtenstein, D.L.; Tollefson, A.E. Immune responses to adenoviruses: Viral evasion mechanisms and their implications for the clinic. Curr. Opin. Immunol. 1999, 11, 380–386. [Google Scholar] [CrossRef]
- Moise, A.R.; Grant, J.R.; Vitalis, T.Z.; Jefferies, W.A. Adenovirus E3-6.7K Maintains Calcium Homeostasis and Prevents Apoptosis and Arachidonic Acid Release. J. Virol. 2002, 76, 1578–1587. [Google Scholar] [CrossRef] [Green Version]
- Gooding, L.R.; Ranheim, T.S.; Tollefson, A.E.; Aquino, L.; Duerksen-Hughes, P.; Horton, T.M.; Wold, W.S. The 10,400- and 14,500-dalton proteins encoded by region E3 of adenovirus function together to protect many but not all mouse cell lines against lysis by tumor necrosis factor. J. Virol. 1991, 65, 4114–4123. [Google Scholar] [CrossRef]
- Gooding, L.R.; Sofola, I.O.; Tollefson, A.E.; Duerksen-Hughes, P.; Wold, W.S. The adenovirus E3-14.7K protein is a general inhibitor of tumor necrosis factor-mediated cytolysis. J. Immunol. 1990, 145, 3080–3086. [Google Scholar] [CrossRef]
- Thorne, T.E.; Voelkel-Johnson, C.; Casey, W.M.; Parks, L.W.; Laster, S.M. The activity of cytosolic phospholipase A2 is required for the lysis of adenovirus-infected cells by tumor necrosis factor. J. Virol. 1996, 70, 8502–8507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, M.; McMichael, A.; Peterson, P.A. Reduced allorecognition of adenovirus-2 infected cells. J. Immunol. 1987, 138, 3960–3966. [Google Scholar] [CrossRef]
- Andersson, M.; Paabo, S.; Nilsson, T.; Peterson, P.A. Impaired intracellular transport of class I MHC antigens as a possible means for adenoviruses to evade immune surveillance. Cell 1985, 43, 215–222. [Google Scholar] [CrossRef]
- Burgert, H.G.; Kvist, S. An adenovirus type 2 glycoprotein blocks cell surface expression of human histocompatibility class I antigens. Cell 1985, 41, 987–997. [Google Scholar] [CrossRef]
- Burgert, H.G.; Maryanski, J.L.; Kvist, S. “E3/19K” protein of adenovirus type 2 inhibits lysis of cytolytic T lymphocytes by blocking cell-surface expression of histocompatibility class I antigens. Proc. Natl. Acad. Sci. USA 1987, 84, 1356–1360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, J.H.; Bennink, J.R.; Yewdell, J.W. Retention of adenovirus E19 glycoprotein in the endoplasmic reticulum is essential to its ability to block antigen presentation. J. Exp. Med. 1991, 174, 1629–1637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rawle, F.C.; Tollefson, A.E.; Wold, W.S.; Gooding, L.R. Mouse anti-adenovirus cytotoxic T lymphocytes. Inhibition of lysis by E3 gp19K but not E3 14.7K. J. Immunol. 1989, 143, 2031–2037. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.R.; Nilsson, T.; Peterson, P.A. Identification of a consensus motif for retention of transmembrane proteins in the endoplasmic reticulum. EMBO J. 1990, 9, 3153–3162. [Google Scholar] [CrossRef]
- Tollefson, A.E.; Scaria, A.; Hermiston, T.W.; Ryerse, J.S.; Wold, L.J.; Wold, W.S. The adenovirus death protein (E3-11.6K) is required at very late stages of infection for efficient cell lysis and release of adenovirus from infected cells. J. Virol. 1996, 70, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.G.; Eidenschink, B.B.; Iguchi, E.; Zakharkin, S.O.; LaRocca, C.J.; Tolosa, E.J.; Truty, M.J.; Jacobsen, K.; Fernandez-Zapico, M.E.; Davydova, J. Cancer imaging and therapy utilizing a novel NIS-expressing adenovirus: The role of adenovirus death protein deletion. Mol. Ther. Oncolytics 2021, 20, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Davydova, J.; Gavrikova, T.; Brown, E.J.; Luo, X.; Curiel, D.T.; Vickers, S.M.; Yamamoto, M. In Vivo bioimaging tracks conditionally replicative adenoviral replication and provides an early indication of viral antitumor efficacy. Cancer Sci. 2010, 101, 474–481. [Google Scholar] [CrossRef] [Green Version]
- Mathews, M.B.; Shenk, T. Adenovirus virus-associated RNA and translation control. J. Virol. 1991, 65, 5657–5662. [Google Scholar] [CrossRef] [Green Version]
- Akusjärvi, G.; Mathews, M.B.; Andersson, P.; Vennström, B.; Pettersson, U. Structure of genes for virus-associated RNAI and RNAII of adenovirus type 2. Proc. Natl. Acad. Sci. USA 1980, 77, 2424–2428. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Mathews, M.B. Structure, function, and evolution of adenovirus-associated RNA: A phylogenetic approach. J. Virol. 1996, 70, 5083–5099. [Google Scholar] [CrossRef] [Green Version]
- Bhat, R.A.; Thimmappaya, B. Adenovirus mutants with DNA sequence perturbations in the intragenic promoter of VAI RNA gene allow the enhanced transcription of VAII RNA gene in HeLa cells. Nucleic Acids Res. 1984, 12, 7377–7388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subramanian, S.; Bhat, R.A.; Rundell, M.K.; Thimmappaya, B. Suppression of the translation defect phenotype specific for a virus-associated RNA-deficient adenovirus mutant in monkey cells by simian virus 40. J. Virol. 1986, 60, 363–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thimmappaya, B.; Weinberger, C.; Schneider, R.J.; Shenk, T. Adenovirus VAI RNA is required for efficient translation of viral mRNAs at late times after infection. Cell 1982, 31, 543–551. [Google Scholar] [CrossRef]
- Machitani, M.; Yamaguchi, T.; Shimizu, K.; Sakurai, F.; Katayama, K.; Kawabata, K.; Mizuguchi, H. Adenovirus Vector-Derived VA-RNA-Mediated Innate Immune Responses. Pharmaceutics 2011, 3, 338–353. [Google Scholar] [CrossRef] [Green Version]
- Weber, F.; Wagner, V.; Kessler, N.; Haller, O. Induction of Interferon Synthesis by the PKR-Inhibitory VA RNAs of Adenoviruses. J. Interf. Cytokine Res. 2006, 26, 1–7. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Kawabata, K.; Kouyama, E.; Ishii, K.J.; Katayama, K.; Suzuki, T.; Kurachi, S.; Sakurai, F.; Akira, S.; Mizuguchi, H. Induction of type I interferon by adenovirus-encoded small RNAs. Proc. Natl. Acad. Sci. USA 2010, 107, 17286–17291. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Ortega, M.B.; Lopez, G.J.; Jimenez, G.; Garcia-Garcia, J.A.; Conde, V.; Boulaiz, H.; Carrillo, E.; Perán, M.; Marchal, J.A.; Garcia, M.A. Clinical and therapeutic potential of protein kinase PKR in cancer and metabolism. Expert Rev. Mol. Med. 2017, 19, e9. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Bennett, R.L.; Liu, X.; Byrne, M.; Stratford May, W. PKR negatively regulates leukemia progression in association with PP2A activation, Bcl-2 inhibition and increased apoptosis. Blood Cancer J. 2013, 3, e144. [Google Scholar] [CrossRef] [Green Version]
- Marchal, J.A.; Lopez, G.J.; Peran, M.; Comino, A.; Delgado, J.R.; García-García, J.A.; Conde, V.; Aranda, F.M.; Rivas, C.; Esteban, M.; et al. The impact of PKR activation: From neurodegeneration to cancer. FASEB J. 2014, 28, 1965–1974. [Google Scholar] [CrossRef]
- Roh, M.S.; Kwak, J.Y.; Kim, S.J.; Lee, H.W.; Kwon, H.C.; Hwang, T.H.; Choi, P.J.; Hong, Y.S. Expression of double-stranded RNA-activated protein kinase in small-size peripheral adenocarcinoma of the lung. Pathol. Int. 2005, 55, 688–693. [Google Scholar] [CrossRef]
- Terada, T.; Ueyama, J.; Ukita, Y.; Ohta, T. Protein expression of double-stranded RNA-activated protein kinase (PKR) in intrahepatic bile ducts in normal adult livers, fetal livers, primary biliary cirrhosis, hepatolithiasis and intrahepatic cholangiocarcinoma. Liver 2000, 20, 450–457. [Google Scholar] [CrossRef] [PubMed]
| Name | Serotype Based on | E1A | Fiber | Transgene | E3 Status | Other Modification | References |
|---|---|---|---|---|---|---|---|
| H101 (oncorin) | Ad5 | untouched | Ad5 | none | del of 78.3-85.8 m.u. Probably only E3-12.5K left | deletion of E1B55K | [8] |
| ADV/HSV-tk | Ad5 viral vector | transgene in deleted E1 | Ad5 | HSV tk gene with the RSV LTR promoter | Deletion of RIDα, RIDβ and E3-14.7K | [9] | |
| MEM-288 | Ad5 | delta 24 | Ad5 | chimeric CD40 ligand and IFNb | deleted | deletion of E1B55K | [10] |
| LOAd703 | Ad5 | E2F promoter, delta 24 | chimeric Ad5/Ad35 | TMZ-CD40L + 4-1BBL | deleted E3-6.7K and gp19K | [11,12,13] | |
| CG0070 | Ad5 | E2F promoter | Ad5 | GM-CSF under control of E3 promoter | gp19K deleted | [14] | |
| AdAPT-001 | Ad5 | 50bp del in E1A promoter (tumor specific) | Ad5 | mTGFbR-IgG (TGFb trap) | Deletion of RIDα, RIDβ and E3-14.7K | deletion E1B19K | [15,16] |
| OBP-301 (Telomelysin) | Ad5 | human TERT promoter E1A-IRES-E1B in E1 deleted backbone | Ad5 | none | deleted | [17,18] | |
| Colo-Ad1 (Enadenotucirev) | Ad11/Ad3 chimera | untouched (Ad11) | Ad11 | none | near complete deletion | deletion in E4orf4 gene | [19] |
| DNX-2440 | Ad5 | delta 24 | Ad5 with RGD-motif into the H-loop | OX40 ligand | deleted | [20,21] | |
| CAdVEC | Ad5 + Ad5 gutted vector | delta24 | Ad5 | undisclosed immunomodulatory molecules in vector | deleted | ||
| CGTG-102(ONCOS-102) | Ad5 | delta 24 | Ad5 with fiber knob of Ad3 | GM-CSF under control of E3 promoter | E3-6.7K and gp19K deleted | [22,23,24] | |
| DNX-2401 | Ad5 | delta 24 | Ad5 with RGD-motif into the H-loop | none | deleted | [21] | |
| TILT-123 | Ad5 | E2F promoter, delta 24 | Ad5 with fiber knob of Ad3 | TNFa and IL-2 | transgenes in E3 unclear what is deleted | [25] | |
| Ad-E6E7 | Ad5 viral vector (vaccine) | E1 deleted | Ad5 | attenuated fusion E6E7 transgene | deleted | + Maraba virus | [26] |
| Ad-MAGEA3 | Ad5 viral vector (vaccine) | E1 deleted | Ad5 | MAGE-A3 | deleted | + Maraba virus | [27] |
| VCN-01 | Ad5 | E2F promoter, delta 24 | Ad5 with RGDK motif in shaft | soluble version of human PH20 under late promoter | WT | [28] | |
| NG-350A | Ad11/Ad3 chimera | untouched (Ad11) | Ad11 | heavy and light chains for a secreted CD40 agonist monoclonal antibody | near complete deletion | PsiOxus Therapeutics | |
| NG-641 | Ad11/Ad3 chimera | untouched (Ad11) | Ad11 | secreted Interferon alpha, the chemokines CXCL9, CXCL10 and an anti-FAP/anti-CD3 bispecific T-cell activator | near complete deletion | PsiOxus Therapeutics | |
| cells with CRAd-survivin-pk7 virus | Ad5 | human survivin promoter | Ad5 modified with polylysine | none | WT | [29] | |
| ORCA-010 | Ad5 | delta 24 | Ad5 with RGD-motif into the H-loop | none | mutated GP19K | T1 mutation in E3-19K | [30] |
| Trial Identifier | Phase | Conditions | Virus Name | E3 Status | Additional Treatment |
|---|---|---|---|---|---|
| NCT05051696 | N/A | Genital Neoplasms, Female | Oncorine (H101) | only 12.5K present | +/- radiotherapy |
| NCT04771676 | 2 | Refractory Malignant Ascites | Oncorine (H101) | only 12.5K present | none |
| NCT03004183 | 2 | Metastatic Non-small Cell Lung Cancer, Metastatic Triple-negative Breast Cancer | ADV/HSV-tk | deletion of RIDα/β and 14.7K | Valacyclovir, SBRT, Pembrolizumab |
| NCT05076760 | 1 | Advanced Solid Tumors | MEM-288 | deleted | MEM-288 Intratumoral Injection |
| NCT02705196 | 1/2 | Pancreatic Cancer | LOAd703 | deletion of 6.7K and gp19K | gemcitabine, nab-paclitaxel, atezolizumab |
| NCT02143804 | 2 | High Grade, Bladder Cancer, Non Muscle Invasive | CG0070 | gp19K deletion | none |
| NCT02365818 | 2 | Bladder Cancer | CG0070 | gp19K deletion | CG0070 |
| NCT05234905 | 2 | Uterine Cervical Neoplasms | Oncorine (H101) | only 12.5K present | Camrelizumab |
| NCT05113290 | 4 | Hepatocellular Carcinoma | Oncorine (H101) | only 12.5K present | Sorafenib |
| NCT05124002 | 4 | Cholangiocarcinoma, Intrahepatic | Oncorine (H101) | only 12.5K present | HAIC or FOLFOX |
| NCT04673942 | 1 | Refractory Solid Tumor, Adult | AdAPT-001 | deletion of RIDα/β and 14.7K | none |
| NCT03190824 | 2 | Melanoma Stage III and iv | OBP-301 (Telomelysin) | deleted | none |
| NCT01438112 | 2 | Non Muscle Invasive Bladder Cancer | CG0070 | gp19K deletion | none |
| NCT03916510 | 1 | Locally Advanced Rectal Cancer | Enadenotucirev (previously ColoAd-1) | near complete deletion | Capecitabine, Radiotherapy |
| NCT03714334 | 1 | Glioblastoma | DNX-2440 | deleted | none |
| NCT03740256 | 1 | Various solid tumors | CAdVEC | deleted | none |
| NCT01437280 | 1 | Solid Tumors | CGTG-102 | 6.7K and gp19K deleted | none |
| NCT05180851 | 1 | Various solid tumors | Recombinant L-IFN adenovirus | unknown | none |
| NCT02197169 | 1 | Glioblastoma or Gliosarcoma | DNX-2401 | deleted | Interferon-gamma |
| NCT02053220 | 1 | Solid Cancers | Colo-Ad1 | near complete deletion | none |
| NCT02028442 | 1/2 | Solid Tumors of Epithelial Origin | Enadenotucirev (previously ColoAd-1) | near complete deletion | none |
| NCT02028117 | 1 | Recurrent Platinum Resistant Ovarian Cancer | Enadenotucirev (previously ColoAd-1) | near complete deletion | none |
| NCT05222932 | 1 | Melanoma, Head and Neck Squamous Cell Carcinoma | TILT-123 | unknown deletion | Avelumab |
| NCT01598129 | 1 | Malignant Solid Tumor | CGTG-102 | 6.7K and gp19K deleted | low-dose metronomic cyclophosphamide. |
| NCT02798406 | 2 | Brain Cancers | DNX-2401 | deleted | pembrolizumab |
| NCT04217473 | 1 | Metastatic Melanoma | TILT-123 | unknown deletion | TILT-123 |
| NCT03618953 | 1 | HPV-Associated Cancers | Ad-E6E7, MG1-E6E7 | deleted | Atezolizumab |
| NCT04695327 | 1 | Solid Tumor | TILT-123 | unknown deletion | TILT-123 |
| NCT03773744 | 1 | Metastatic Melanoma, Squamous Cell Skin Carcinoma | Ad-MAGEA3, MG1-MAGEA3 | deleted | Pembrolizumab, Cyclophosphamide |
| NCT02045602 | 1 | Locally Advanced Solid Tumors | VCN-01 | WT | Gemcitabine, Abraxane® |
| NCT02045589 | 1 | Pancreatic Adenocarcinoma | VCN-01 | WT | Gemcitabine, Abraxane® |
| NCT02879760 | 1/2 | Non-Small Cell Lung Cancer | Ad-MAGEA3, MG1-MAGEA3 | deleted | Pembrolizumab |
| NCT04685499 | 2 | Head and Neck Squamous Cell Carcinoma With Inoperable Recurrent or Progressive Disease | OBP-301 | deleted | Pembrolizumab |
| NCT03225989 | 1/2 | Solid Cancers | LOAd703 | deletion of 6.7K and gp19K | none |
| NCT03896568 | 1 | High Grade Glioma | DNX-2401 | deleted | none |
| NCT01956734 | 1 | Glioblastoma Multiforme | DNX-2401 | deleted | Temozolomide |
| NCT03178032 | 1 | Brainstem Glioma | DNX-2401 | deleted | none |
| NCT03852511 | 1 | Metastatic Cancer | NG-350A | near complete deletion | none |
| NCT04053283 | 1 | Metastatic Cancer | NG-641 | near complete deletion | none |
| NCT03072134 | 1 | Malignant Glioma | Neural stem cells loaded with NSC-CRAd-Survivin-pk7 | WT | none |
| NCT04097002 | 1/2 | Adenocarcinoma of the Prostate | ORCA-010 | mutated gp19K | none |
| NCT05561491 | 2 | Melanoma | ONCOS-102 (Previously known as CGTG-102) | 6.7K and gp19K deleted | Balstilimab |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blanchette, P.; Teodoro, J.G. A Renaissance for Oncolytic Adenoviruses? Viruses 2023, 15, 358. https://doi.org/10.3390/v15020358
Blanchette P, Teodoro JG. A Renaissance for Oncolytic Adenoviruses? Viruses. 2023; 15(2):358. https://doi.org/10.3390/v15020358
Chicago/Turabian StyleBlanchette, Paola, and Jose G. Teodoro. 2023. "A Renaissance for Oncolytic Adenoviruses?" Viruses 15, no. 2: 358. https://doi.org/10.3390/v15020358






