Propagation of SARS-CoV-2 in a Closed Cell Culture Device: Potential GMP Compatible Production Platform for Live-Attenuated Vaccine Candidates under BSL-3 Conditions?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Propagation of Serum-Free Vero-E6 Cells
2.2. Generation of Serum-Free SARS-CoV-2 Virus Stocks
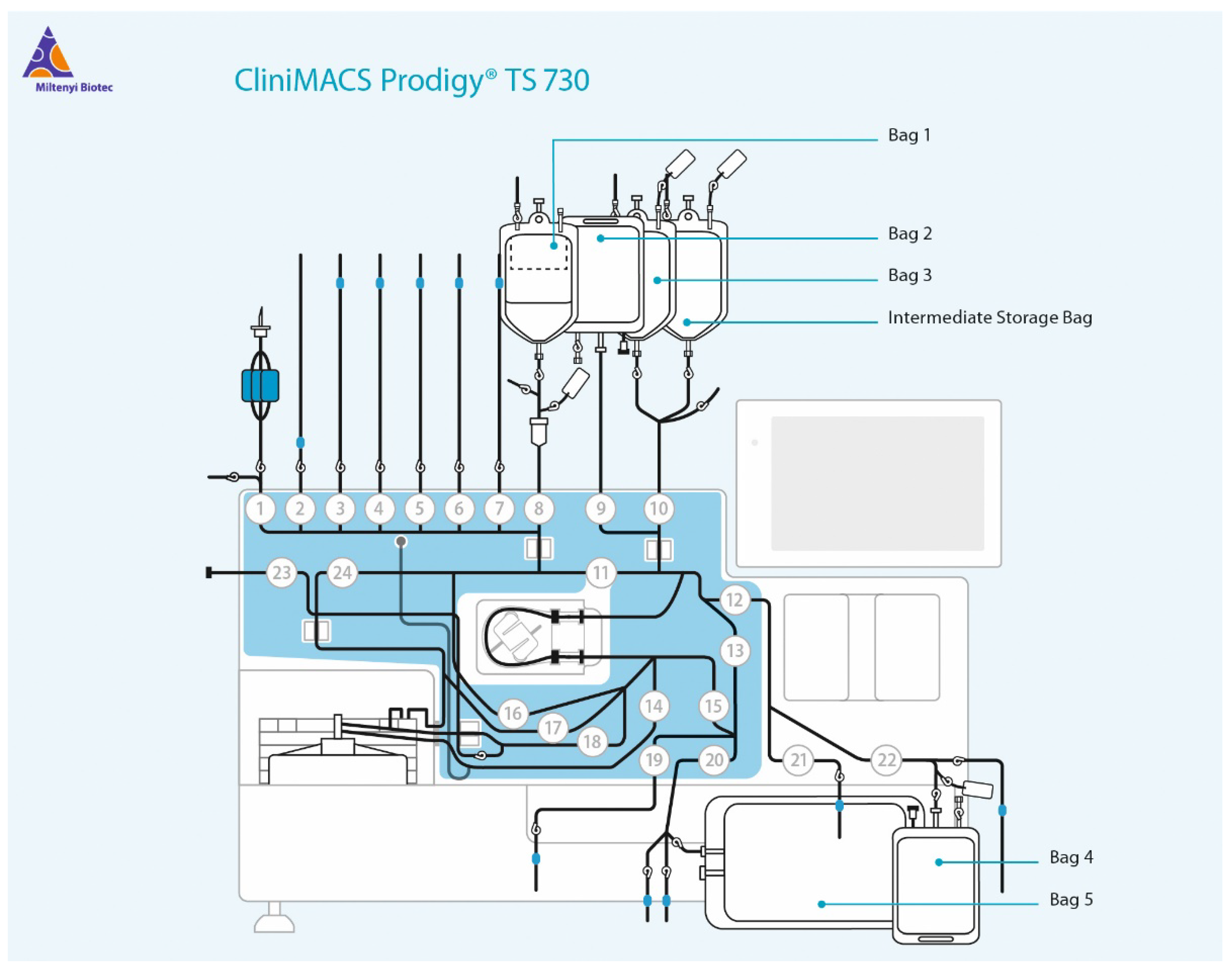
2.3. Propagation of Attenuated Influenza Virus and SARS-CoV-2 in a Closed Cell Culture Device
2.4. qPCR Analysis
2.5. TCID50 Determination
3. Results
3.1. Analysis of Vero E6 Closed Culture Conditions
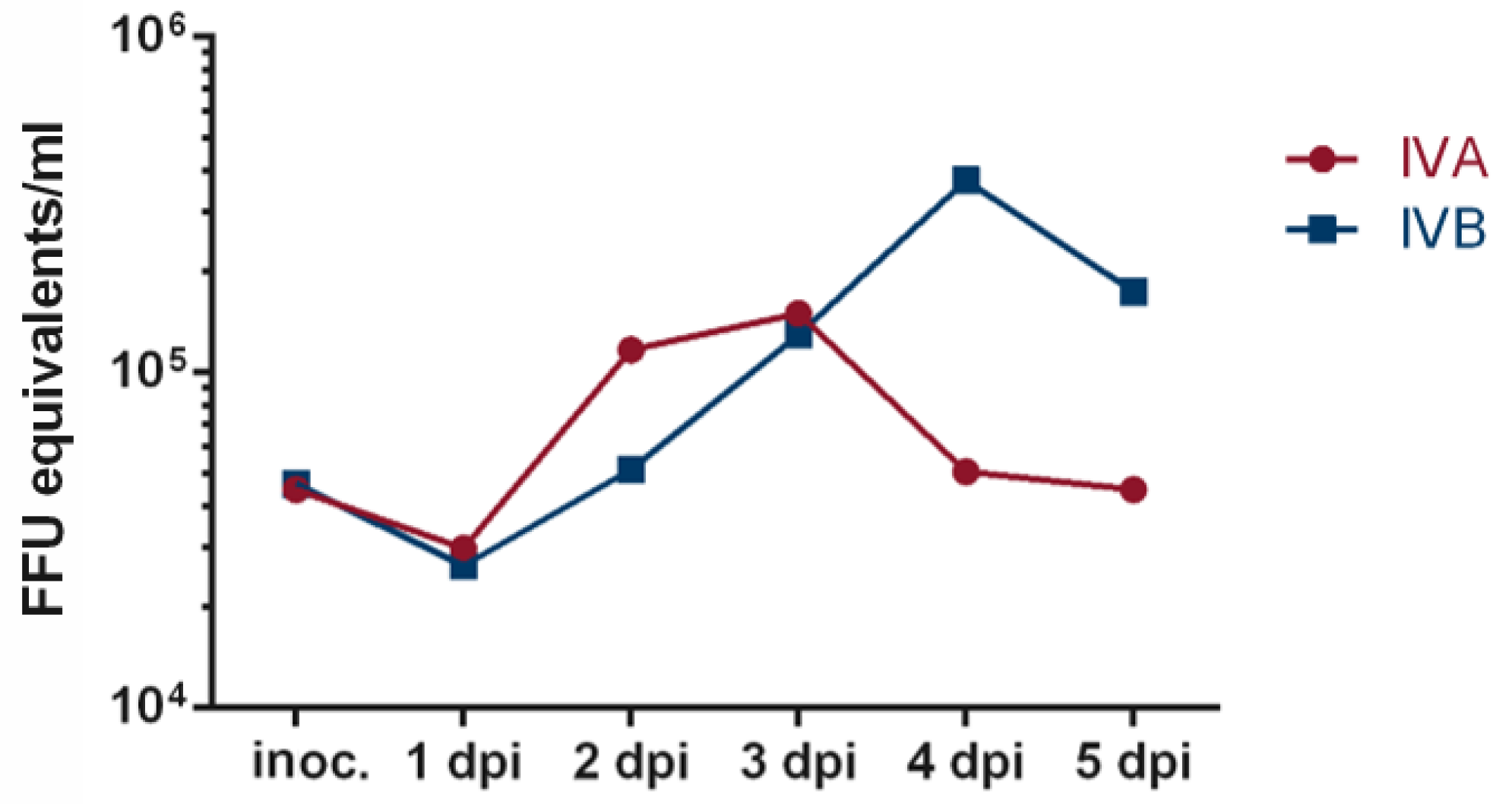
3.2. Establishing the Infection Protocol
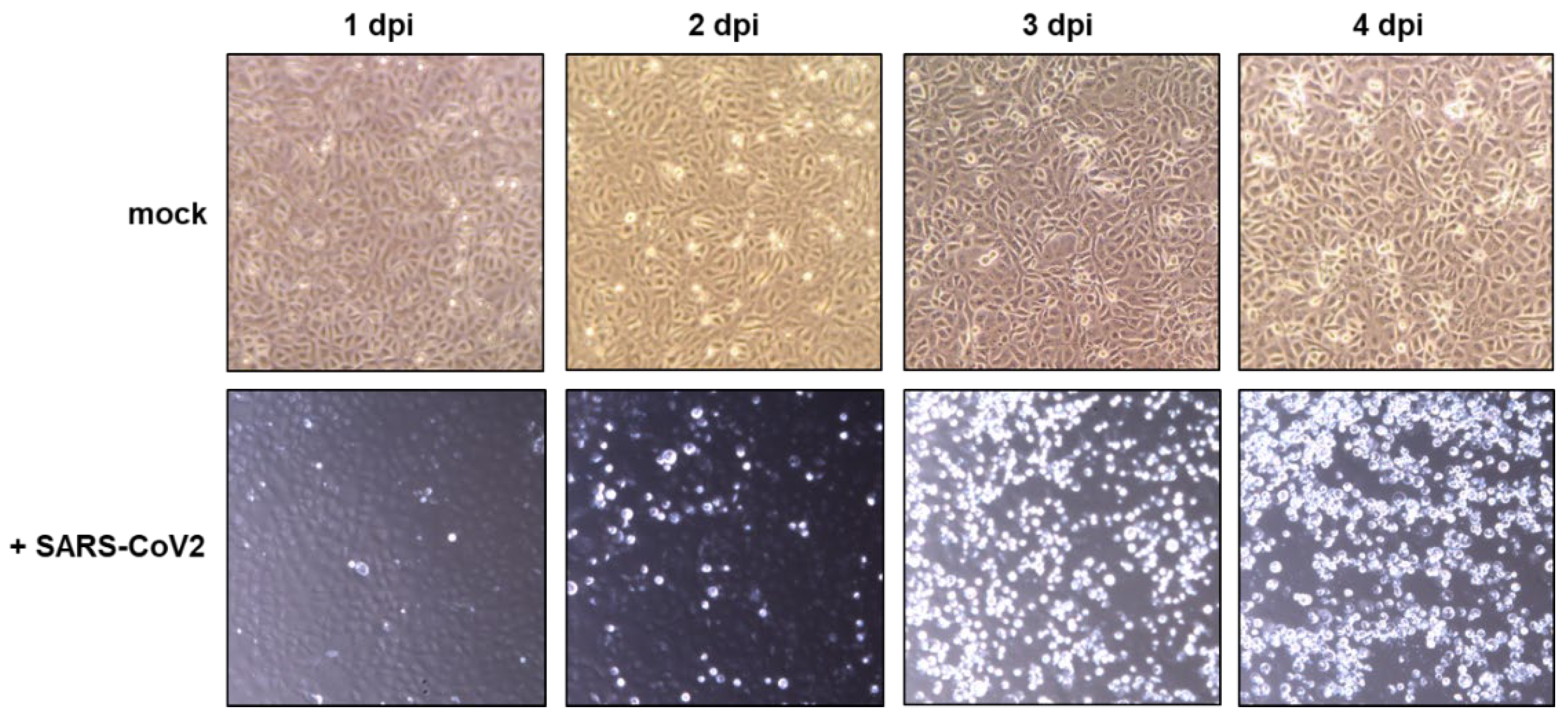
3.3. Propagation of SARS-CoV-2
4. Discussion
- A serum-free working cell bank of the producer cell and all reagents are prepared and stored in a conventional GMP laboratory.
- A clone of a virus isolate is passaged under serum-free conditions in the producer cell from the GMP laboratory using conventional cell culture flasks and the reagents from the GMP laboratory in the biosafety level 3 laboratory to generate a seed virus stock. The seed virus stock is aliquoted in the BSL-3 laboratory in a compounding aseptic containment isolator and stored under controlled freezing conditions.
- To generate a virus working stock, an aliquot of the seed virus stock is expanded using the automated closed cell culture system and the producer cell and reagents from the GMP laboratory. The virus working stocks are aliquoted and stored as described for the seed virus stocks.
- The virus working stocks are used in the closed cell culture system to generate different lots of the investigational live-attenuated vaccine or the challenge virus stock.
- The filling of the investigational products could be performed in a compounding aseptic containment isolator also located in the BSL-3 laboratory. Since live-attenuated vaccines or challenge viruses will most likely be administered by a mucosal rather than a parenteral route, purification by filtration seems sufficient, although additional purification steps could be implemented within the compounding aseptic containment isolator. The aliquoted samples are stored under controlled freezing conditions in the BSL-3 laboratory until use in the clinical study.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- WHO. COVID-19 Weekly Epidemiological Update. 19 October 2022. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20221019_weekly_epi_update_114 (accessed on 31 October 2022).
- Saborni, C.; Vamsee, M.; Cristina, M.T.; Gene, S.T.; Taia, T.W. SARS-CoV-2 vaccines in advanced clinical trials: Where do we stand? Adv. Drug Deliv. Rev. 2021, 172, 314–338. [Google Scholar]
- Florian, K. SARS-CoV-2 vaccines in development. Nature 2020, 586, 516–527. [Google Scholar]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Logunov, D.Y.; Dolzhikova, I.V.; Shcheblyakov, D.V.; Tukhvatulin, A.I.; Zubkova, O.V.; Dzharullaeva, A.S.; Kovyrshina, A.V.; Lubenets, N.L.; Grousova, D.M.; Erokhova, A.S.; et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: An interim analysis of a randomised controlled phase 3 trial in Russia. Lancet 2021, 397, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2020, 384, 403–416. [Google Scholar] [CrossRef]
- Madhi, S.A.; Baillie, V.; Cutland, C.L.; Voysey, M.; Koen, A.L.; Fairlie, L.; Padayachee, S.D.; Dheda, K.; Barnabas, S.L.; Bhorat, Q.E.; et al. Efficacy of the ChAdOx1 nCoV-19 Covid-19 Vaccine against the B.1.351 Variant. N. Engl. J. Med. 2021, 384, 1885–1898. [Google Scholar] [CrossRef]
- Kustin, T.; Harel, N.; Finkel, U.; Perchik, S.; Harari, S.; Tahor, M.; Caspi, I.; Levy, R.; Leshchinsky, M.; Ken Dror, S.; et al. Evidence for increased breakthrough rates of SARS-CoV-2 variants of concern in BNT162b2-mRNA-vaccinated individuals. Nat. Med. 2021, 27, 1379–1384. [Google Scholar] [CrossRef]
- Abu-Raddad, L.J.; Chemaitelly, H.; Butt, A.A. Effectiveness of the BNT162b2 Covid-19 Vaccine against the B.1.1.7 and B.1.351 Variants. N. Engl. J. Med. 2021, 385, 187–189. [Google Scholar] [CrossRef]
- Emary, K.R.W.; Golubchik, T.; Aley, P.K.; Ariani, C.V.; Angus, B.; Bibi, S.; Blane, B.; Bonsall, D.; Cicconi, P.; Charlton, S.; et al. Efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 variant of concern 202012/01 (B.1.1.7): An exploratory analysis of a randomised controlled trial. Lancet 2021, 397, 1351–1362. [Google Scholar] [CrossRef]
- Hacisuleyman, E.; Hale, C.; Saito, Y.; Blachere, N.E.; Bergh, M.; Conlon, E.G.; Schaefer-Babajew, D.J.; DaSilva, J.; Muecksch, F.; Gaebler, C.; et al. Vaccine Breakthrough Infections with SARS-CoV-2 Variants. N. Engl. J. Med. 2021, 384, 2212–2218. [Google Scholar] [CrossRef] [PubMed]
- Farinholt, T.; Doddapaneni, H.; Qin, X.; Menon, V.; Meng, Q.; Metcalf, G.; Chao, H.; Gingras, M.-C.; Avadhanula, V.; Farinholt, P.; et al. Transmission event of SARS-CoV-2 delta variant reveals multiple vaccine breakthrough infections. BMC Med. 2021, 19, 255. [Google Scholar] [CrossRef] [PubMed]
- Brosh-Nissimov, T.; Orenbuch-Harroch, E.; Chowers, M.; Elbaz, M.; Nesher, L.; Stein, M.; Maor, Y.; Cohen, R.; Hussein, K.; Weinberger, M.; et al. BNT162b2 vaccine breakthrough: Clinical characteristics of 152 fully vaccinated hospitalized COVID-19 patients in Israel. Clin. Microbiol. Infect. 2021, 27, 1652–1657. [Google Scholar] [CrossRef] [PubMed]
- Buchan, S.A.; Chung, H.; Brown, K.A.; Austin, P.C.; Fell, D.B.; Gubbay, J.B.; Nasreen, S.; Schwartz, K.L.; Sundaram, M.E.; Tadrous, M.; et al. Estimated Effectiveness of COVID-19 Vaccines Against Omicron or Delta Symptomatic Infection and Severe Outcomes. JAMA Netw. Open 2022, 5, e2232760. [Google Scholar] [CrossRef] [PubMed]
- Collie, S.; Champion, J.; Moultrie, H.; Bekker, L.-G.; Gray, G. Effectiveness of BNT162b2 Vaccine against Omicron Variant in South Africa. N. Engl. J. Med. 2021, 386, 494–496. [Google Scholar] [CrossRef]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. Covid-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef]
- Higdon, M.M.; Baidya, A.; Walter, K.K.; Patel, M.K.; Issa, H.; Espié, E.; Feikin, D.R.; Knoll, M.D. Duration of effectiveness of vaccination against COVID-19 caused by the omicron variant. Lancet Infect. Dis. 2022, 22, 1114–1116. [Google Scholar] [CrossRef]
- Alu, A.; Chen, L.; Lei, H.; Wei, Y.; Tian, X.; Wei, X. Intranasal COVID-19 vaccines: From bench to bed. Ebiomedicine 2022, 76, 103841. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, C.; Song, Y.; Coleman, J.R.; Stawowczyk, M.; Tafrova, J.; Tasker, S.; Boltz, D.; Baker, R.; Garcia, L.; et al. Scalable live-attenuated SARS-CoV-2 vaccine candidate demonstrates preclinical safety and efficacy. Proc. Natl. Acad. Sci. USA 2021, 118, e2102775118. [Google Scholar] [CrossRef]
- Sanchez-Felipe, L.; Vercruysse, T.; Sharma, S.; Ma, J.; Lemmens, V.; Van Looveren, D.; Arkalagud Javarappa, M.P.; Boudewijns, R.; Malengier-Devlies, B.; Liesenborghs, L.; et al. A single-dose live-attenuated YF17D-vectored SARS-CoV-2 vaccine candidate. Nature 2021, 590, 320–325. [Google Scholar] [CrossRef]
- Russ, A.; Wittmann, S.; Tsukamoto, Y.; Herrmann, A.; Deutschmann, J.; Lagisquet, J.; Ensser, A.; Kato, H.; Gramberg, T. Nsp16 shields SARS–CoV-2 from efficient MDA5 sensing and IFIT1-mediated restriction. EMBO Rep. 2022, 23, e55648. [Google Scholar] [CrossRef] [PubMed]
- Lapuente, D.; Fuchs, J.; Willar, J.; Antão, A.V.; Eberlein, V.; Uhlig, N.; Issmail, L.; Schmidt, A.; Oltmanns, F.; Peter, A.S.; et al. Protective mucosal immunity against SARS-CoV-2 after heterologous systemic RNA-mucosal adenoviral vector immunization. Biorxiv 2021, 2021, 454858. [Google Scholar]
- Halkjær-Knudsen, V. Designing a Facility with Both Good Manufacturing Practice (GMP) and Biosafety in Mind: Synergies and Conflicts. Appl. Biosaf. 2007, 12, 7–16. [Google Scholar] [CrossRef]
- WHO. Expert Committee on Biological Standardization, Geneva, 17 to 21 October 2016. 2016. Available online: http://apps.who.int/iris/bitstream/handle/10665/253055/WHO-BS-2016.2294-eng.pdf?sequence=1 (accessed on 31 October 2022).
- Peter, A.S.; Roth, E.; Schulz, S.R.; Fraedrich, K.; Steinmetz, T.; Damm, D.; Hauke, M.; Richel, E.; Mueller-Schmucker, S.; Habenicht, K.; et al. A pair of noncompeting neutralizing human monoclonal antibodies protecting from disease in a SARS-CoV-2 infection model. Eur. J. Immunol. 2021, 52, 770–783. [Google Scholar] [CrossRef] [PubMed]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.; Bleicker, T.; Brünink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020, 25, 2000045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peter, A.S.; Grüner, E.; Socher, E.; Fraedrich, K.; Richel, E.; Mueller-Schmucker, S.; Cordsmeier, A.; Ensser, A.; Sticht, H.; Überla, K. Characterization of SARS-CoV-2 Escape Mutants to a Pair of Neutralizing Antibodies Targeting the RBD and the NTD. Int. J. Mol. Sci. 2022, 23, 8177. [Google Scholar] [CrossRef]
- Johnson, V.A.; Byington, R.E.; Nara, P.L. Quantitative Assays for Virus Infectivity. In Techniques in HIV Research; Aldovini, A., Walker, B.D., Eds.; Palgrave Macmillan: London, UK, 1990. [Google Scholar]
- Lock, D.; Mockel-Tenbrinck, N.; Drechsel, K.; Barth, C.; Mauer, D.; Schaser, T.; Kolbe, C.; Al Rawashdeh, W.; Brauner, J.; Hardt, O.; et al. Automated Manufacturing of Potent CD20-Directed Chimeric Antigen Receptor T Cells for Clinical Use. Hum. Gene Ther. 2017, 28, 914–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mock, U.; Nickolay, L.; Philip, B.; Cheung, G.W.-K.; Zhan, H.; Johnston, I.C.D.; Kaiser, A.D.; Peggs, K.; Pule, M.; Thrasher, A.J.; et al. Automated manufacturing of chimeric antigen receptor T cells for adoptive immunotherapy using CliniMACS Prodigy. Cytotherapy 2016, 18, 1002–1011. [Google Scholar] [CrossRef]
- Levine, B.L.; Miskin, J.; Wonnacott, K.; Keir, C. Global Manufacturing of CAR T Cell Therapy. Mol. Ther. Methods Clin. Dev. 2017, 4, 92–101. [Google Scholar] [CrossRef] [Green Version]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klessing, S.; Peter, A.S.; Fraedrich, K.; Wagner, J.T.; Kummer, M.; Deutschmann, J.; Steininger, P.; Steibl, H.-D.; Überla, K. Propagation of SARS-CoV-2 in a Closed Cell Culture Device: Potential GMP Compatible Production Platform for Live-Attenuated Vaccine Candidates under BSL-3 Conditions? Viruses 2023, 15, 397. https://doi.org/10.3390/v15020397
Klessing S, Peter AS, Fraedrich K, Wagner JT, Kummer M, Deutschmann J, Steininger P, Steibl H-D, Überla K. Propagation of SARS-CoV-2 in a Closed Cell Culture Device: Potential GMP Compatible Production Platform for Live-Attenuated Vaccine Candidates under BSL-3 Conditions? Viruses. 2023; 15(2):397. https://doi.org/10.3390/v15020397
Chicago/Turabian StyleKlessing, Stephan, Antonia Sophia Peter, Kirsten Fraedrich, Jannik T. Wagner, Mirko Kummer, Janina Deutschmann, Philipp Steininger, Hans-Dieter Steibl, and Klaus Überla. 2023. "Propagation of SARS-CoV-2 in a Closed Cell Culture Device: Potential GMP Compatible Production Platform for Live-Attenuated Vaccine Candidates under BSL-3 Conditions?" Viruses 15, no. 2: 397. https://doi.org/10.3390/v15020397





