Comparative Analysis of Different Inbred Chicken Lines Highlights How a Hereditary Inflammatory State Affects Susceptibility to Avian Influenza Virus
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chicken Lines
2.2. Cell Preparation
2.3. Flow Cytometry
2.4. CD107a Degranulation Assay
2.5. Western Blot
2.6. Avian Influenza Virus
2.7. AIV Infection of Lung Macrophages
2.8. RNA Isolation
2.9. Pre-Amplification of cDNA
2.10. High-Throughput qPCR Using the 96.96 IFC Dynamic Array
| Antibody | Clone | Isotype | Product Info. | Dilution |
|---|---|---|---|---|
| Mouse anti-chicken CD45APC | LT40 | IgM | Southern Biotech | 1:100 [17,18] |
| Mouse anti-chicken γδ TCR-FITC | TCR1 | IgG1 | Southern Biotech | 1:500 |
| Mouse anti-chicken αβ (Vβ1) TCR FITC | TCR2 | IgG1 | Southern Biotech | 1:500 |
| Mouse anti-chicken CD8β and CD8β-PE | EP42 | IgG2a | Southern Biotech | 1:1000 [18,19] |
| Mouse anti-chicken CD8α pacific blue | CT-8 | IgG1 | Southern Biotech | 1:1000 [19,20] |
| Mouse anti-chicken CD4 | CT-4 | IgG1 | Southern Biotech | 1:750 [20,21] |
| Mouse anti-chicken CD107a * | 5G10 | IgG1 | DSHB | 1:1000 |
| Mouse anti-chicken CD3 AF647 | CT-3 | IgG1 | Southern Biotech | 1:100 |
| Mouse anti-chicken CD3 | AV36 | IgG1 | UK Immunological Toolbox | 1:100 |
| Rat anti-CD3 | CD3-12 | IgG1 | AbCam | 1:1000 |
| Rabbit anti-β actin | ab8227 | polyclonal | AbCam | 1:5000 |
2.11. Data Processing and Analysis
2.12. Statistical Analysis
3. Results
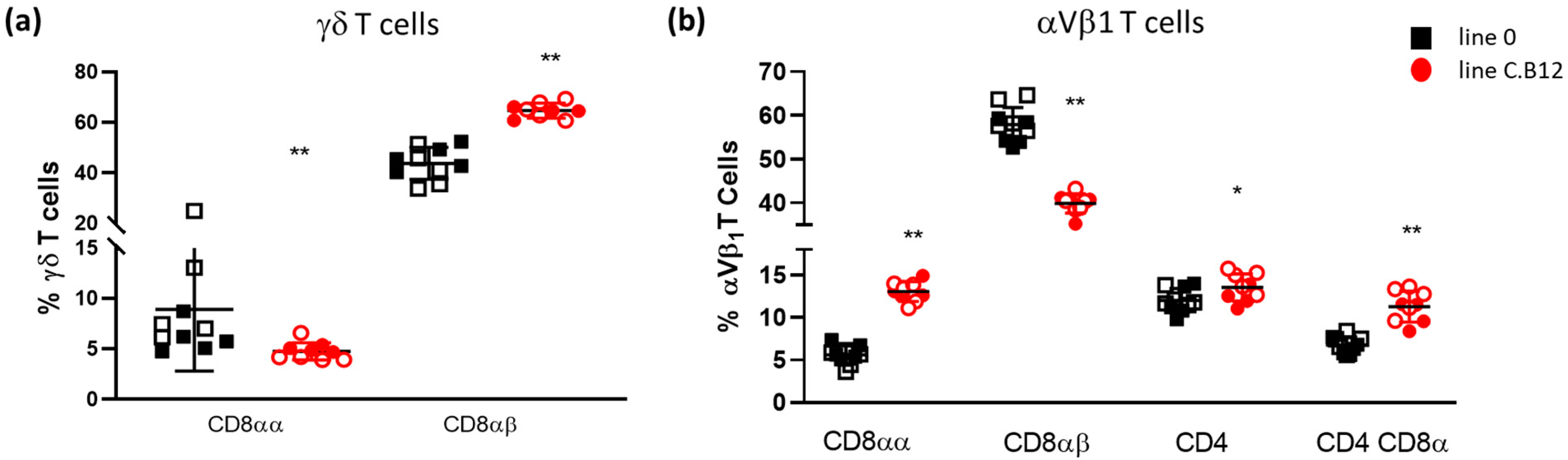
3.1. Line C.B12 and Line 0 Differ in γδ and αVβ1 T Cell Numbers
3.2. Phenotypic Analysis of Splenic Cytotoxic Cells
3.3. Differential Degranulation Potential of γδ and αVβ1 T Cells
3.4. Differential Innate Immune Responses in Lung Macrophages
Line-Specific Responses to H7N1 Infection
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lycett, S.J.; Duchatel, F.; Digard, P. A brief history of bird flu. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2019, 374, 20180257. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority; European Centre for Disease Prevention and Control; European Union Reference Laboratory for Avian Influenza; Adlhoch, C.; Fusaro, A.; Gonzales, J.L.; Kuiken, T.; Marangon, S.; Niqueux, E.; Staubach, C.; et al. Avian influenza overview February–May 2021. EFSA J. 2021, 19, e06951. [Google Scholar] [PubMed]
- Krauss, S.; Webster, R.G. Avian influenza virus surveillance and wild birds: Past and present. Avian. Dis. 2010, 54, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Peiris, J.S.; Cowling, B.J.; Wu, J.T.; Feng, L.; Guan, Y.; Yu, H.; Leung, G.M. Interventions to reduce zoonotic and pandemic risks from avian influenza in asia. Lancet Infect. Dis. 2016, 16, 252–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perdue, M.L.; Nguyen, T. The who research agenda for influenza: Two years later. Bull. World Health Organ. 2012, 90, 246. [Google Scholar] [CrossRef] [PubMed]
- Boonyanuwat, K.; Thummabutra, S.; Sookmanee, N.; Vatchavalkhu, V.; Siripholvat, V.; Mitsuhashi, T. Influences of mhc class ii haplotypes on avian influenza traits in thai indigenous chicken. J. Poult. Sci. 2006, 43, 120–125. [Google Scholar] [CrossRef] [Green Version]
- Sartika, T.; Sulandari, S.; Zein, M.S.A. Selection of mx gene genotype as genetic marker for avian influenza resistance in indonesian native chicken. BMC Proc. 2011, 5 (Suppl. 4), S37. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.; Smith, N.; Yu, L.; Paton, I.R.; Gutowska, M.W.; Forrest, H.L.; Danner, A.F.; Seiler, J.P.; Digard, P.; Webster, R.G.; et al. A comparative analysis of host responses to avian influenza infection in ducks and chickens highlights a role for the interferon-induced transmembrane proteins in viral resistance. BMC Genom. 2015, 16, 574. [Google Scholar] [CrossRef] [Green Version]
- Hunt, H.D.; Jadhao, S.; Swayne, D.E. Major histocompatibility complex and background genes in chickens influence susceptibility to high pathogenicity avian influenza virus. Avian. Dis. 2010, 54, 572–575. [Google Scholar] [CrossRef]
- Wang, Y.; Lupiani, B.; Reddy, S.M.; Lamont, S.J.; Zhou, H. Rna-seq analysis revealed novel genes and signaling pathway associated with disease resistance to avian influenza virus infection in chickens. Poult. Sci. 2014, 93, 485–493. [Google Scholar] [CrossRef]
- Drobik-Czwarno, W.; Wolc, A.; Fulton, J.E.; Jankowski, T.; Arango, J.; O’Sullivan, N.P.; Dekkers, J.C.M. Genetic basis of resistance to avian influenza in different commercial varieties of layer chickens. Poult. Sci. 2018, 97, 3421–3428. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Hernandez, R.; Mwangi, W.; Peroval, M.; Sadeyen, J.R.; Ascough, S.; Balkissoon, D.; Staines, K.; Boyd, A.; McCauley, J.; Smith, A.; et al. Host genetics determine susceptibility to avian influenza infection and transmission dynamics. Sci. Rep. 2016, 6, 26787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alber, A.; Morris, K.M.; Bryson, K.J.; Sutton, K.M.; Monson, M.S.; Chintoan-Uta, C.; Borowska, D.; Lamont, S.J.; Schouler, C.; Kaiser, P.; et al. Avian pathogenic Escherichia coli (apec) strain-dependent immunomodulation of respiratory granulocytes and mononuclear phagocytes in csf1r-reporter transgenic chickens. Front. Immunol. 2019, 10, 3055. [Google Scholar] [CrossRef] [PubMed]
- Garrido, D.; Alber, A.; Kut, E.; Chanteloup, N.K.; Lion, A.; Trotereau, A.; Dupont, J.; Tedin, K.; Kaspers, B.; Vervelde, L.; et al. The role of type i interferons (ifns) in the regulation of chicken macrophage inflammatory response to bacterial challenge. Dev. Comp. Immunol. 2018, 86, 156–170. [Google Scholar] [CrossRef] [Green Version]
- Bryson, K.J.; Garrido, D.; Esposito, M.; McLachlan, G.; Digard, P.; Schouler, C.; Guabiraba, R.; Trapp, S.; Vervelde, L. Precision cut lung slices: A novel versatile tool to examine host-pathogen interaction in the chicken lung. Vet. Res. 2020, 51, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borowska, D.; Kuo, R.; Bailey, R.A.; Watson, K.A.; Kaiser, P.; Vervelde, L.; Stevens, M.P. Highly multiplexed quantitative pcr-based platform for evaluation of chicken immune responses. PLoS ONE 2019, 14, e0225658. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative pcr and the 2(-delta delta c(t)) method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Kaufman, J.; Skjoedt, K.; Salomonsen, J.; Simonsen, M.; Du Pasquier, L.; Parisot, R.; Riegert, P. Mhc-like molecules in some nonmammalian vertebrates can be detected by some cross-reactive xenoantisera. J. Immunol. (Baltim. Md. 1950) 1990, 144, 2258–2272. [Google Scholar] [CrossRef]
- Wu, Z.; Rothwell, L.; Young, J.R.; Kaufman, J.; Butter, C.; Kaiser, P. Generation and characterization of chicken bone marrow-derived dendritic cells. Immunology 2010, 129, 133–145. [Google Scholar] [CrossRef]
- Jeurissen, S.H.; Janse, E.M.; Kok, G.L.; De Boer, G.F. Distribution and function of non-lymphoid cells positive for monoclonal antibody cvi-chnl-68.2 in healthy chickens and those infected with marek’s disease virus. Vet. Immunol. Immunopathol. 1989, 22, 123–133. [Google Scholar] [CrossRef]
- Jeurissen, S.H.; Claassen, E.; Janse, E.M. Histological and functional differentiation of non-lymphoid cells in the chicken spleen. Immunology 1992, 77, 75–80. [Google Scholar] [PubMed]
- Gobel, T.W.; Kaspers, B.; Stangassinger, M. Nk and t cells constitute two major, functionally distinct intestinal epithelial lymphocyte subsets in the chicken. Int. Immunol. 2001, 13, 757–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Lin, L.; Tong, Y.; Liu, Y.; Mou, J.; Wang, X.; Wang, X.; Gong, Y.; Zhao, Y.; Liu, Y.; et al. Erratum: Author correction to: Trim29 negatively controls antiviral immune response through targeting sting for degradation. Cell Discov. 2018, 4, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, B.; Jin, M.; Zhang, Y.; Wei, T.; Bai, Z. Evolution of the il17 receptor family in chordates: A new subfamily il17rel. Immunogenetics 2011, 63, 835–845. [Google Scholar] [CrossRef]
- Nehyba, J.; Hrdlickova, R.; Burnside, J.; Bose, H.R., Jr. A novel interferon regulatory factor (irf), irf-10, has a unique role in immune defense and is induced by the v-rel oncoprotein. Mol. Cell Biol. 2002, 22, 3942–3957. [Google Scholar] [CrossRef] [Green Version]
- Tallam, A.; Perumal, T.M.; Antony, P.M.; Jager, C.; Fritz, J.V.; Vallar, L.; Balling, R.; Del Sol, A.; Michelucci, A. Gene regulatory network inference of immunoresponsive gene 1 (irg1) identifies interferon regulatory factor 1 (irf1) as its transcriptional regulator in mammalian macrophages. PLoS ONE 2016, 11, e0149050. [Google Scholar] [CrossRef] [Green Version]
- Labzin, L.I.; Schmidt, S.V.; Masters, S.L.; Beyer, M.; Krebs, W.; Klee, K.; Stahl, R.; Lutjohann, D.; Schultze, J.L.; Latz, E.; et al. Atf3 is a key regulator of macrophage ifn responses. J. Immunol. 2015, 195, 4446–4455. [Google Scholar] [CrossRef] [Green Version]
- Pasick, J.; Diederich, S.; Berhane, Y.; Embury-Hyatt, C.; Xu, W. Imbalance between innate antiviral and pro-inflammatory immune responses may contribute to different outcomes involving low- and highly pathogenic avian influenza h5n3 infections in chickens. J. Gen. Virol. 2017, 98, 1245–1258. [Google Scholar] [CrossRef]
- Cheng, H.H.; Kaiser, P.; Lamont, S.J. Integrated genomic approaches to enhance genetic resistance in chickens. Annu. Rev. Anim. Biosci. 2013, 1, 239–260. [Google Scholar] [CrossRef] [Green Version]
- Vermijlen, D.; Gatti, D.; Kouzeli, A.; Rus, T.; Eberl, M. Gammadelta t cell responses: How many ligands will it take till we know? Semin. Cell Dev. Biol. 2018, 84, 75–86. [Google Scholar] [CrossRef]
- Holderness, J.; Hedges, J.F.; Ramstead, A.; Jutila, M.A. Comparative biology of gammadelta t cell function in humans, mice, and domestic animals. Annu. Rev. Anim. Biosci. 2013, 1, 99–124. [Google Scholar] [CrossRef] [PubMed]
- Sowder, J.T.; Chen, C.L.; Ager, L.L.; Chan, M.M.; Cooper, M.D. A large subpopulation of avian t cells express a homologue of the mammalian t gamma/delta receptor. J. Exp. Med. 1988, 167, 315–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arstila, T.P.; Lassila, O. Androgen-induced expression of the peripheral blood gamma delta t cell population in the chicken. J. Immunol. 1993, 151, 6627–6633. [Google Scholar] [CrossRef] [PubMed]
- Pieper, J.; Methner, U.; Berndt, A. Heterogeneity of avian gammadelta t cells. Vet. Immunol. Immunopathol. 2008, 124, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Walliser, I.; Gobel, T.W. Chicken il-17a is expressed in alphabeta and gammadelta t cell subsets and binds to a receptor present on macrophages, and t cells. Dev. Comp. Immunol. 2018, 81, 44–53. [Google Scholar] [CrossRef]
- Laursen, A.M.S.; Kulkarni, R.R.; Taha-Abdelaziz, K.; Plattner, B.L.; Read, L.R.; Sharif, S. Characterizaton of gamma delta t cells in marek’s disease virus (gallid herpesvirus 2) infection of chickens. Virology 2018, 522, 56–64. [Google Scholar] [CrossRef]
- Fenzl, L.; Gobel, T.W.; Neulen, M.L. Gammadelta t cells represent a major spontaneously cytotoxic cell population in the chicken. Dev. Comp. Immunol. 2017, 73, 175–183. [Google Scholar] [CrossRef]
- Zhong, W.; Reinherz, E.L. Cd8 alpha alpha homodimer expression and role in cd8 t cell memory generation during influenza virus a infection in mice. Eur. J. Immunol. 2005, 35, 3103–3110. [Google Scholar] [CrossRef]
- Cheroutre, H.; Lambolez, F. Doubting the tcr coreceptor function of cd8alphaalpha. Immunity 2008, 28, 149–159. [Google Scholar] [CrossRef] [Green Version]
- Goodall, K.J.; Nguyen, A.; McKenzie, C.; Eckle, S.B.G.; Sullivan, L.C.; Andrews, D.M. The murine cd94/nkg2 ligand, qa-1(b), is a high-affinity, functional ligand for the cd8alphaalpha homodimer. J. Biol. Chem. 2020, 295, 3239–3246. [Google Scholar] [CrossRef]
- Van Campen, H.; Easterday, B.C.; Hinshaw, V.S. Virulent avian influenza a viruses: Their effect on avian lymphocytes and macrophages in vivo and in vitro. J. Gen. Virol. 1989, 70, 2887–2895. [Google Scholar] [CrossRef]
- Xing, Z.; Cardona, C.J.; Adams, S.; Yang, Z.; Li, J.; Perez, D.; Woolcock, P.R. Differential regulation of antiviral and proinflammatory cytokines and suppression of fas-mediated apoptosis by ns1 of h9n2 avian influenza virus in chicken macrophages. J. Gen. Virol. 2009, 90, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Xing, Z.; Cardona, C.J.; Li, J.; Dao, N.; Tran, T.; Andrada, J. Modulation of the immune responses in chickens by low-pathogenicity avian influenza virus h9n2. J. Gen. Virol. 2008, 89, 1288–1299. [Google Scholar] [CrossRef] [PubMed]
- Lyon, J.A.; Hinshaw, V.S. Replication of influenza a viruses in an avian macrophage cell line. J. Gen. Virol. 1991, 72, 2011–2013. [Google Scholar] [CrossRef] [PubMed]
- Perrone, L.A.; Plowden, J.K.; Garcia-Sastre, A.; Katz, J.M.; Tumpey, T.M. H5n1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 2008, 4, e1000115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ariaans, M.P.; van de Haar, P.M.; Lowenthal, J.W.; van Eden, W.; Hensen, E.J.; Vervelde, L. Elispot and intracellular cytokine staining: Novel assays for quantifying t cell responses in the chicken. Dev. Comp. Immunol. 2008, 32, 1398–1404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, S.E.; Gibson, M.S.; Wash, R.S.; Ferrara, F.; Wright, E.; Temperton, N.; Kellam, P.; Fife, M. Chicken interferon-inducible transmembrane protein 3 restricts influenza viruses and lyssaviruses in vitro. J. Virol. 2013, 87, 12957–12966. [Google Scholar] [CrossRef] [Green Version]
- Reemers, S.S.; Groot Koerkamp, M.J.; Holstege, F.C.; van Eden, W.; Vervelde, L. Cellular host transcriptional responses to influenza a virus in chicken tracheal organ cultures differ from responses in in vivo infected trachea. Vet. Immunol. Immunopathol. 2009, 132, 91–100. [Google Scholar] [CrossRef] [Green Version]
- Liu, H.; Tian, J.; Lu, K.; Li, Y.; Guan, Z.; Cao, X.; Li, X.; Chang, Z.; Wang, X.; Sa, X.; et al. Chicken isg12(2) attenuates newcastle disease virus and enhances the efficiency of newcastle disease vaccine via activating immune pathways. Transbound. Emerg. Dis. 2022, 69, 2634–2648. [Google Scholar] [CrossRef]
- Smith, J.; Sadeyen, J.R.; Cavanagh, D.; Kaiser, P.; Burt, D.W. The early immune response to infection of chickens with infectious bronchitis virus (ibv) in susceptible and resistant birds. BMC Vet. Res. 2015, 11, 256. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.; Sadeyen, J.R.; Butter, C.; Kaiser, P.; Burt, D.W. Analysis of the early immune response to infection by infectious bursal disease virus in chickens differing in their resistance to the disease. J. Virol. 2015, 89, 2469–2482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bremner, A.; Kim, S.; Morris, K.M.; Nolan, M.J.; Borowska, D.; Wu, Z.; Tomley, F.; Blake, D.P.; Hawken, R.; Kaiser, P.; et al. Kinetics of the cellular and transcriptomic response to eimeria maxima in relatively resistant and susceptible chicken lines. Front. Immunol. 2021, 12, 653085. [Google Scholar] [CrossRef] [PubMed]
- Russell, K.M.; Smith, J.; Bremner, A.; Chintoan-Uta, C.; Vervelde, L.; Psifidi, A.; Stevens, M.P. Transcriptomic analysis of caecal tissue in inbred chicken lines that exhibit heritable differences in resistance to campylobacter jejuni. BMC Genom. 2021, 22, 411. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, P.; Kuo, R.; Vervelde, L.; Dutia, B.M.; Kaiser, P.; Smith, J. Macrophages from susceptible and resistant chicken lines have different transcriptomes following marek’s disease virus infection. Genes 2019, 10, 74. [Google Scholar] [CrossRef] [Green Version]
- Zamperin, G.; Bianco, A.; Smith, J.; Bortolami, A.; Vervelde, L.; Schivo, A.; Fortin, A.; Marciano, S.; Panzarin, V.; Mazzetto, E.; et al. Heterogeneity of early host response to infection with four low-pathogenic h7 viruses with a different evolutionary history in the field. Viruses 2021, 13, 2323. [Google Scholar] [CrossRef]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bryson, K.J.; Sives, S.; Lee, H.-M.; Borowska, D.; Smith, J.; Digard, P.; Vervelde, L. Comparative Analysis of Different Inbred Chicken Lines Highlights How a Hereditary Inflammatory State Affects Susceptibility to Avian Influenza Virus. Viruses 2023, 15, 591. https://doi.org/10.3390/v15030591
Bryson KJ, Sives S, Lee H-M, Borowska D, Smith J, Digard P, Vervelde L. Comparative Analysis of Different Inbred Chicken Lines Highlights How a Hereditary Inflammatory State Affects Susceptibility to Avian Influenza Virus. Viruses. 2023; 15(3):591. https://doi.org/10.3390/v15030591
Chicago/Turabian StyleBryson, Karen J., Samantha Sives, Hui-Min Lee, Dominika Borowska, Jacqueline Smith, Paul Digard, and Lonneke Vervelde. 2023. "Comparative Analysis of Different Inbred Chicken Lines Highlights How a Hereditary Inflammatory State Affects Susceptibility to Avian Influenza Virus" Viruses 15, no. 3: 591. https://doi.org/10.3390/v15030591






