Relevant Day/Night Temperatures Simulating Belgian Summer Conditions Reduce Japanese Encephalitis Virus Dissemination and Transmission in Belgian Field-Collected Culex pipiens Mosquitoes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Mosquito Collection
2.2. Virus Production and Titration
2.3. Oral Infection of Mosquitoes
2.4. Mosquito Salivation and Dissection
2.5. JEV Detection
2.5.1. RT-qPCR Analysis
2.5.2. Virus Isolation
2.6. Biotype Identification by qPCR
2.7. Statistical Analysis
3. Results
3.1. Infection, Dissemination and Transmission Rates
3.1.1. Incubation at a Constant 25 °C Temperature
3.1.2. Incubation at a 25/15 °C Day/Night Temperature Gradient
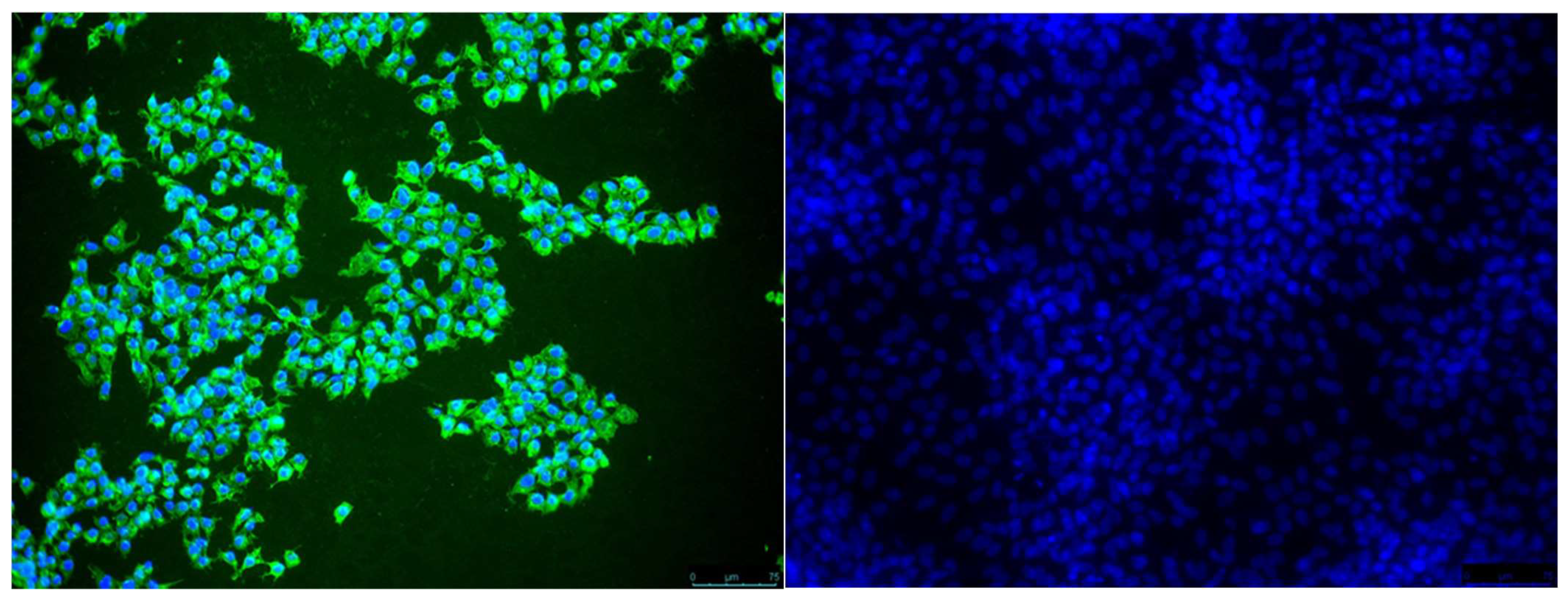
3.2. Virus Isolation
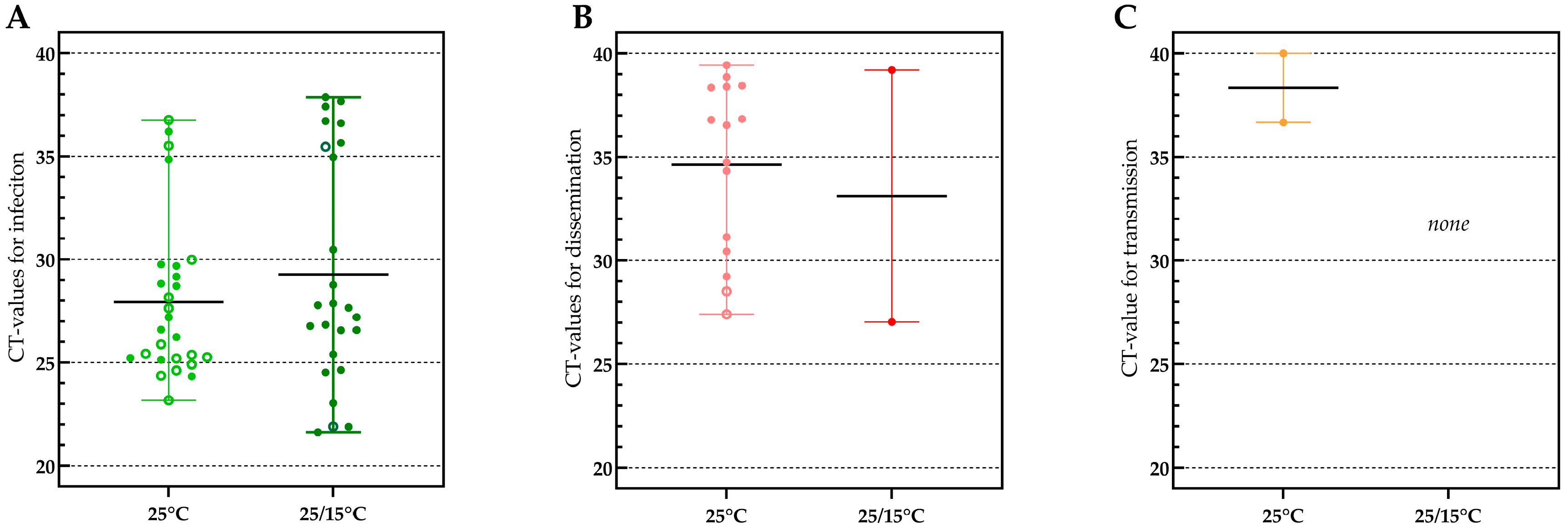
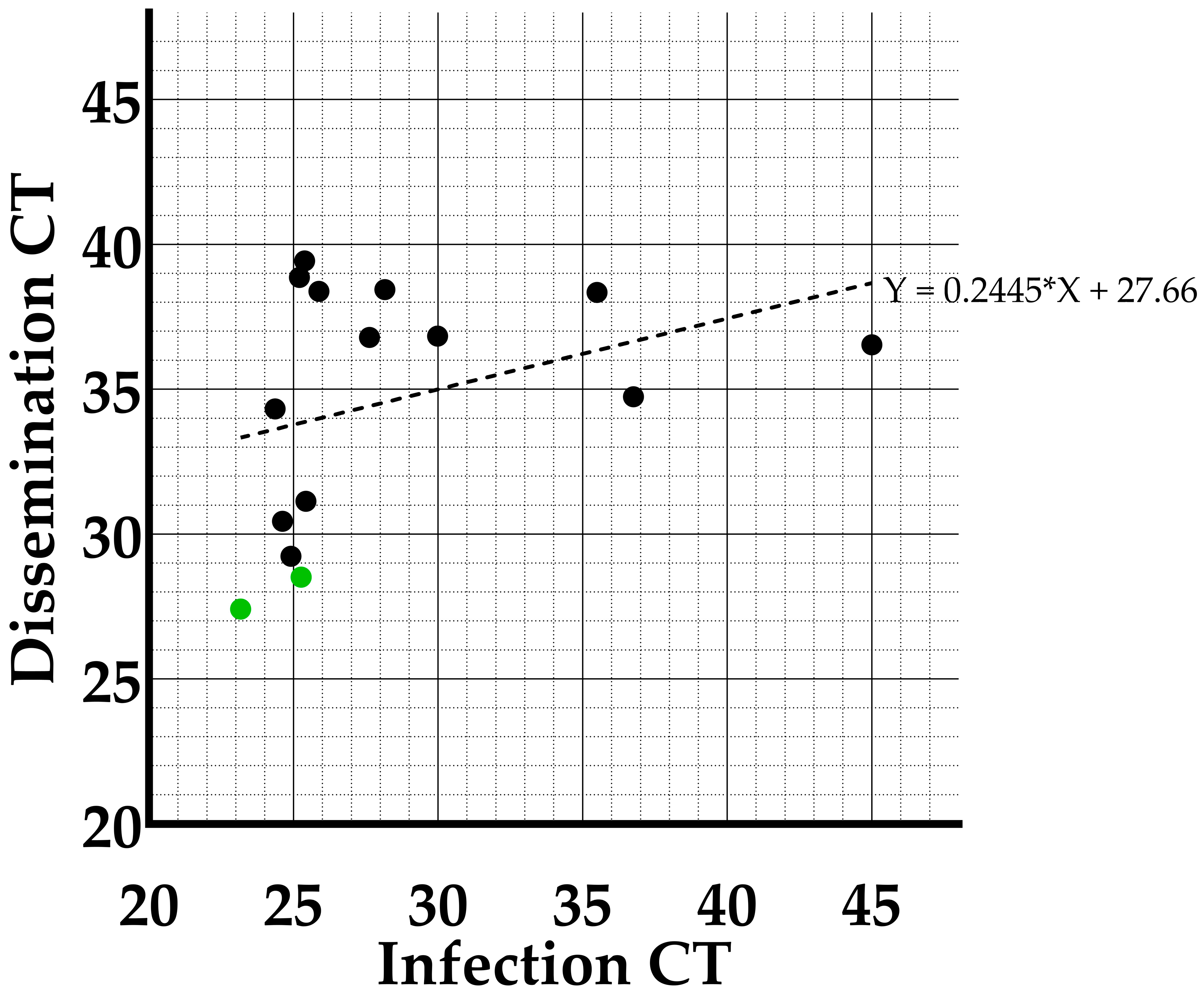
3.3. Viral Loads Found in Infection, Dissemination and Transmission
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Calisher, C.H.; Gould, E.A. Taxonomy of the virus family Flaviviridae. Adv. Virus Res. 2003, 59, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Hubálek, Z.; Rudolf, I.; Nowotny, N. Arboviruses pathogenic for domestic and wild animals. Adv. Virus Res. 2014, 89, 201–275. [Google Scholar] [CrossRef] [PubMed]
- Simon, L.; Sandhu, D.; Goyal, A.; Kruse, B. Japanese Encephalitis. StatPearls (Treasure Island, FL, USA). 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470423/ (accessed on 15 January 2023).
- Spickler, A.R. Japanese Encephalitis. Center for Food Security and Public Health; Ames, IA, USA, 2016. Available online: https://www.cfsph.iastate.edu/Factsheets/pdfs/japanese_encephalitis.pdf (accessed on 15 January 2023).
- European Center of Disease Control. Facts about Japanese encephalitis. Factsheet. 2017. Available online: https://www.ecdc.europa.eu/en/japanese-encephalitis/facts (accessed on 9 February 2021).
- Turtle, L.; Solomon, T. Japanese encephalitis — the prospects for new treatments. Nat. Rev. Neurol. 2018, 14, 298–313. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Zhang, Y.; Zhou, Z.-B.; Xia, S.; Shi, W.-Q.; Xue, J.-B.; Li, Y.-Y.; Wu, J.-T. New strains of Japanese encephalitis virus circulating in Shanghai, China after a ten-year hiatus in local mosquito surveillance. Parasites Vectors 2019, 12, 1–14. [Google Scholar] [CrossRef]
- Eynde, C.V.D.; Sohier, C.; Matthijs, S.; De Regge, N. Japanese Encephalitis Virus Interaction with Mosquitoes: A Review of Vector Competence, Vector Capacity and Mosquito Immunity. Pathogens 2022, 11, 317. [Google Scholar] [CrossRef]
- Erlanger, T.E.; Weiss, S.; Keiser, J.; Utzinger, J.; Wiedenmayer, K. Past, Present, and Future of Japanese Encephalitis. Emerg. Infect. Dis. 2009, 15, 1–7. [Google Scholar] [CrossRef]
- Furuya-Kanamori, L.; Gyawali, N.; Mills, D.J.; Hugo, L.E.; Devine, G.J.; Lau, C.L. The Emergence of Japanese Encephalitis in Australia and the Implications for a Vaccination Strategy. Trop. Med. Infect. Dis. 2022, 7, 85. [Google Scholar] [CrossRef]
- Simon-Loriere, E.; Faye, O.; Prot, M.; Casademont, I.; Fall, G.; Kipela, J.-M.; Fall, I.S.; Holmes, E.C.; Sakuntabhai, A.; Sall, A.A. Autochthonous Japanese Encephalitis with Yellow Fever Coinfection in Africa. N. Engl. J. Med. 2017, 376, 1483–1485. [Google Scholar] [CrossRef]
- Ravanini, P.; Huhtamo, E.; Ilaria, V.; Crobu, M.G.; Nicosia, A.M.; Servino, L.; Rivasi, F.; Allegrini, S.; Miglio, U.; Magri, A.; et al. Japanese encephalitis virus RNA detected in Culex pipiens mosquitoes in Italy. Eurosurveillance 2012, 17, 20221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Wispelaere, M.; Desprès, P.; Choumet, V. European Aedes albopictus and Culex pipiens Are Competent Vectors for Japanese Encephalitis Virus. PLOS Neglected Trop. Dis. 2017, 11, e0005294. [Google Scholar] [CrossRef] [Green Version]
- Chapman, G.E.; Sherlock, K.; Hesson, J.C.; Blagrove, M.S.C.; Lycett, G.J.; Archer, D.; Solomon, T.; Baylis, M. Laboratory transmission potential of British mosquitoes for equine arboviruses. Parasites Vectors 2020, 13, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Folly, A.J.; Dorey-Robinson, D.; Hernández-Triana, L.M.; Ackroyd, S.; Vidana, B.; Lean, F.Z.X.; Hicks, D.; Nuñez, A.; Johnson, N. Temperate conditions restrict Japanese encephalitis virus infection to the mid-gut and prevents systemic dissemination in Culex pipiens mosquitoes. Sci. Rep. 2021, 11, 6133. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie-Impoinvil, L.; Impoinvil, D.E.; Galbraith, S.E.; Dillon, R.J.; Ranson, H.; Johnson, N.; Fooks, A.R.; Solomon, T.; Baylis, M. Evaluation of a temperate climate mosquito, Ochlerotatus detritus(=Aedes detritus), as a potential vector of Japanese encephalitis virus. Med Veter-Èntomol. 2014, 29, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.-J.; Kim, H.C.; Klein, T.A.; Ramey, A.M.; Lee, J.-H.; Kyung, S.-G.; Park, J.-Y.; Cho, Y.S.; Cho, I.-S.; Yeh, J.-Y. Molecular Detection and Genotyping of Japanese Encephalitis Virus in Mosquitoes during a 2010 Outbreak in the Republic of Korea. PLoS ONE 2013, 8, e55165. [Google Scholar] [CrossRef]
- Kim, H.C.; Takhampunya, R.; Tippayachai, B.; Chong, S.-T.; Park, J.-Y.; Kim, M.-S.; Seo, H.-J.; Yeh, J.-Y.; Lee, W.-J.; Lee, D.-K.; et al. Japanese Encephalitis Virus in Culicine Mosquitoes (Diptera: Culicidae) of the Republic of Korea, 2008–2010. Mil. Med. 2015, 180, 158–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Cha, G.-W.; Jeong, Y.E.; Lee, W.-G.; Chang, K.S.; Roh, J.Y.; Yang, S.C.; Park, M.Y.; Park, C.; Shin, E.-H. Detection of Japanese Encephalitis Virus Genotype V in Culex orientalis and Culex pipiens (Diptera: Culicidae) in Korea. PLoS ONE 2015, 10, e0116547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Versteirt, V.; Boyer, S.; Damiens, D.; De Clercq, E.; Dekoninck, W.; Ducheyne, E.; Grootaert, P.; Garros, C.; Hance, T.; Hendrickx, G.; et al. Nationwide inventory of mosquito biodiversity (Diptera: Culicidae) in Belgium, Europe. Bull. Èntomol. Res. 2012, 103, 193–203. [Google Scholar] [CrossRef] [Green Version]
- Fritz, M.L.; Walker, E.D.; Miller, J.R.; Severson, D.W.; Dworkin, I. Divergent host preferences of above- and below-ground Culex pipiens mosquitoes and their hybrid offspring. Med Veter- Èntomol. 2015, 29, 115–123. [Google Scholar] [CrossRef]
- Beerntsen, B.T.; James, A.A.; Christensen, B.M. Genetics of Mosquito Vector Competence. Microbiol. Mol. Biol. Rev. 2000, 64, 115–137. [Google Scholar] [CrossRef] [Green Version]
- KMI. Climatic Overviews of 2020. p. 2020. Available online: https://www.meteo.be/nl/klimaat/klimaat-van-belgie/klimatologisch-overzicht/2016-2020/2020/juli (accessed on 18 July 2022).
- Bharucha, T.; Sengvilaipaseuth, O.; Vongsouvath, M.; Davong, V.; Panyanouvong, P.; Piorkowski, G.; Garson, J.; Newton, P.; De Lamballerie, X.; Dubot-Pérès, A. Development of an improved RT-qPCR Assay for detection of Japanese encephalitis virus (JEV) RNA including a systematic review and comprehensive comparison with published methods. PLoS ONE 2018, 13, e0194412. [Google Scholar] [CrossRef]
- Vogels, C.B.F. The role of Culex Pipiens Mosquitoes in Transmission of West Nile Virus in Europe; Wageningen University: Wageningen, The Netherlands, 2017. [Google Scholar]
- Boukraa, S.; Dekoninck, W.; Versteirt, V.; Schaffner, F.; Coosemans, M.; Haubruge, E.; Francis, F. Updated checklist of the mosquitoes (Diptera: Culicidae) of Belgium. J. Vector Ecol. 2015, 40, 398–407. [Google Scholar] [CrossRef] [PubMed]
- Tyler-Julian, K.; Darrisaw, C.; Lloyd, A.; Hoel, D. The Use of Frozen, Food-Grade Blood to Successfully Maintain Colonies of Four Species of Mosquitoes (Diptera: Culicidae). J. Insect Sci. 2021, 21. [Google Scholar] [CrossRef] [PubMed]
- Ross, P.A.; Endersby-Harshman, N.M.; Hoffmann, A.A. A comprehensive assessment of inbreeding and laboratory adaptation in Aedes aegypti mosquitoes. Evol. Appl. 2018, 12, 572–586. [Google Scholar] [CrossRef] [Green Version]
- Tuanudom, R.; Yurayart, N.; Rodkhum, C.; Tiawsirisup, S. Diversity of midgut microbiota in laboratory-colonized and field-collected Aedes albopictus (Diptera: Culicidae): A preliminary study. Heliyon 2021, 7, e08259. [Google Scholar] [CrossRef]
- Gloria-Soria, A.; Soghigian, J.; Kellner, D.; Powell, J.R. Genetic diversity of laboratory strains and implications for research: The case of Aedes aegypti. PLOS Neglected Trop. Dis. 2019, 13, e0007930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richards, S.L.; Mores, C.N.; Lord, C.C.; Tabachnick, W.J. Impact of Extrinsic Incubation Temperature and Virus Exposure on Vector Competence of Culex pipiens quinquefasciatus Say (Diptera: Culicidae) for West Nile Virus. Vector-Borne Zoonotic Dis. 2007, 7, 629–636. [Google Scholar] [CrossRef] [Green Version]
- Dohm, D.J.; O’Guinn, M.L.; Turell, M.J. Effect of Environmental Temperature on the Ability of Culex pipiens (Diptera: Culicidae) to Transmit West Nile Virus. J. Med Èntomol. 2002, 39, 221–225. [Google Scholar] [CrossRef]
- Cansado-Utrilla, C.; Zhao, S.Y.; McCall, P.J.; Coon, K.L.; Hughes, G.L. The microbiome and mosquito vectorial capacity: Rich potential for discovery and translation. Microbiome 2021, 9, 111. [Google Scholar] [CrossRef]
- Samuel, G.H.; Adelman, Z.N.; Myles, K.M. Temperature-dependent effects on the replication and transmission of arthropod-borne viruses in their insect hosts. Curr. Opin. Insect Sci. 2016, 16, 108–113. [Google Scholar] [CrossRef] [Green Version]
- Breslin, J.J.; Smith, L.G.; Barnes, H.J.; Guy, J.S. Comparison of virus isolation, immunohistochemistry, and reverse transcriptase-polymerase chain reaction procedures for detection of turkey coronavirus. Avian Dis. 2000, 44, 624. [Google Scholar] [CrossRef]
- Knüsel, R.; Bergmann, S.M.; Casey, J.; Segner, H.; Wahli, T.; Einer-Jensen, K. Virus isolation vs RT-PCR: Which method is more successful in detecting VHSV and IHNV in fish tissue sampled under field conditions? J. Fish Dis. 2007, 30, 559–568. [Google Scholar] [CrossRef]
- Carpenter, A.; Clem, R.J. Factors Affecting Arbovirus Midgut Escape in Mosquitoes. Pathogens 2023, 12, 220. [Google Scholar] [CrossRef]
- Boorman, J. Observations on the amount of virus present in the haemolymph of Aedes aegypti infected with Uganda S, yellow fever and Semliki Forest viruses. Trans R Soc Trop Med Hyg 1960, 54, 362–365. [Google Scholar] [CrossRef] [PubMed]
- Miles, J.A.R.; Pillai, J.S.; Maguire, T. Multiplication of Whataroa Virus in Mosquitoes. J. Med Èntomol. 1973, 10, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L.D.; Houk, E.J.; Hardy, J.L.; Presser, S.B. Dissemination Barriers for Western Equine Encephalomyelitis Virus in Culex Tarsalis Infected after Ingestion of Low Viral Doses *. Am. J. Trop. Med. Hyg. 1981, 30, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Vazeille, M.; Madec, Y.; Mousson, L.; Bellone, R.; Barré-Cardi, H.; Sousa, C.A.; Jiolle, D.; Yébakima, A.; de Lamballerie, X.; Failloux, A.-B. Zika virus threshold determines transmission by European Aedes albopictus mosquitoes. Emerg. Microbes Infect. 2019, 8, 1668–1678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Vargas, I.; Olson, K.; Black, W. The Genetic Basis for Salivary Gland Barriers to Arboviral Transmission. Insects 2021, 12, 73. [Google Scholar] [CrossRef]
- Heitmann, A.; Jansen, S.; Lühken, R.; Leggewie, M.; Schmidt-Chanasit, J.; Tannich, E. Forced Salivation As a Method to Analyze Vector Competence of Mosquitoes. J. Vis. Exp. 2018, 138, e57980. [Google Scholar] [CrossRef] [Green Version]
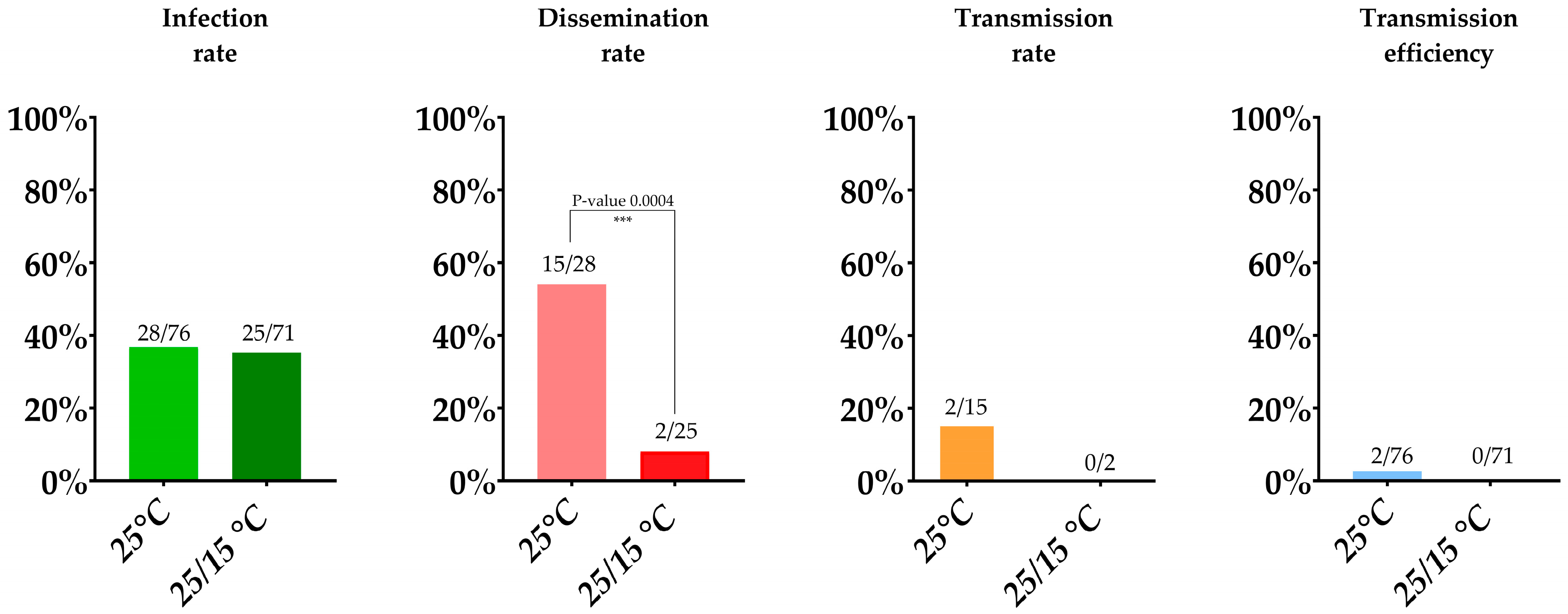
| 14 Day Survival Rate | Infection Rate | Dissemination Rate | Transmission Rate | Transmission Efficiency | |
|---|---|---|---|---|---|
| 25 °C | 80% (76/95) | 36.8% (28/76) | 53.6% (15/28) | 13.3% (2/15) | 2.6% (2/76) |
| 25/15 °C | 64% (71/111) | 35.2% (25/71) | 8% (2/25) | 0% (0/2) | 0% (0/71) |
| Infection RT-qPCR Positives Confirmed by Isolation | Dissemination RT-qPCR Positives Confirmed by Isolation | Transmission RT-qPCR Positives Confirmed by Isolation | |
|---|---|---|---|
| 25 °C | 71.4% (20/28) | 86.7% (13/15) | 50% (1/2) |
| 25/15 °C | 92% (23/25) | 100% (2/2) | No RT-qPCR positive samples |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van den Eynde, C.; Sohier, C.; Matthijs, S.; De Regge, N. Relevant Day/Night Temperatures Simulating Belgian Summer Conditions Reduce Japanese Encephalitis Virus Dissemination and Transmission in Belgian Field-Collected Culex pipiens Mosquitoes. Viruses 2023, 15, 764. https://doi.org/10.3390/v15030764
Van den Eynde C, Sohier C, Matthijs S, De Regge N. Relevant Day/Night Temperatures Simulating Belgian Summer Conditions Reduce Japanese Encephalitis Virus Dissemination and Transmission in Belgian Field-Collected Culex pipiens Mosquitoes. Viruses. 2023; 15(3):764. https://doi.org/10.3390/v15030764
Chicago/Turabian StyleVan den Eynde, Claudia, Charlotte Sohier, Severine Matthijs, and Nick De Regge. 2023. "Relevant Day/Night Temperatures Simulating Belgian Summer Conditions Reduce Japanese Encephalitis Virus Dissemination and Transmission in Belgian Field-Collected Culex pipiens Mosquitoes" Viruses 15, no. 3: 764. https://doi.org/10.3390/v15030764





