An Outbred Guinea Pig Disease Model for Lassa Fever Using a Host-Adapted Clade III Nigerian Lassa Virus
Abstract
1. Introduction
2. Methods
2.1. Ethics and Biosafety
2.2. Animal
2.3. LASV Isolate
2.4. In Vivo Challenge and Passaging
2.5. Determination of 50% Lethal Dose (LD50)
2.6. Temporal Infection Kinetics of NML-61/GPA
2.7. Viral Titrations (TCID50)
2.8. Hematology, Biochemistry and Coagulation
2.9. Cytokine Responses
2.10. Histopathology
2.11. Illumina Sequencing
3. Results
3.1. Generation of a Guinea Pig Adapted Clade III LASV
3.2. Determination of the 50% Lethal Dose
3.3. Full Genome Sequence Analysis
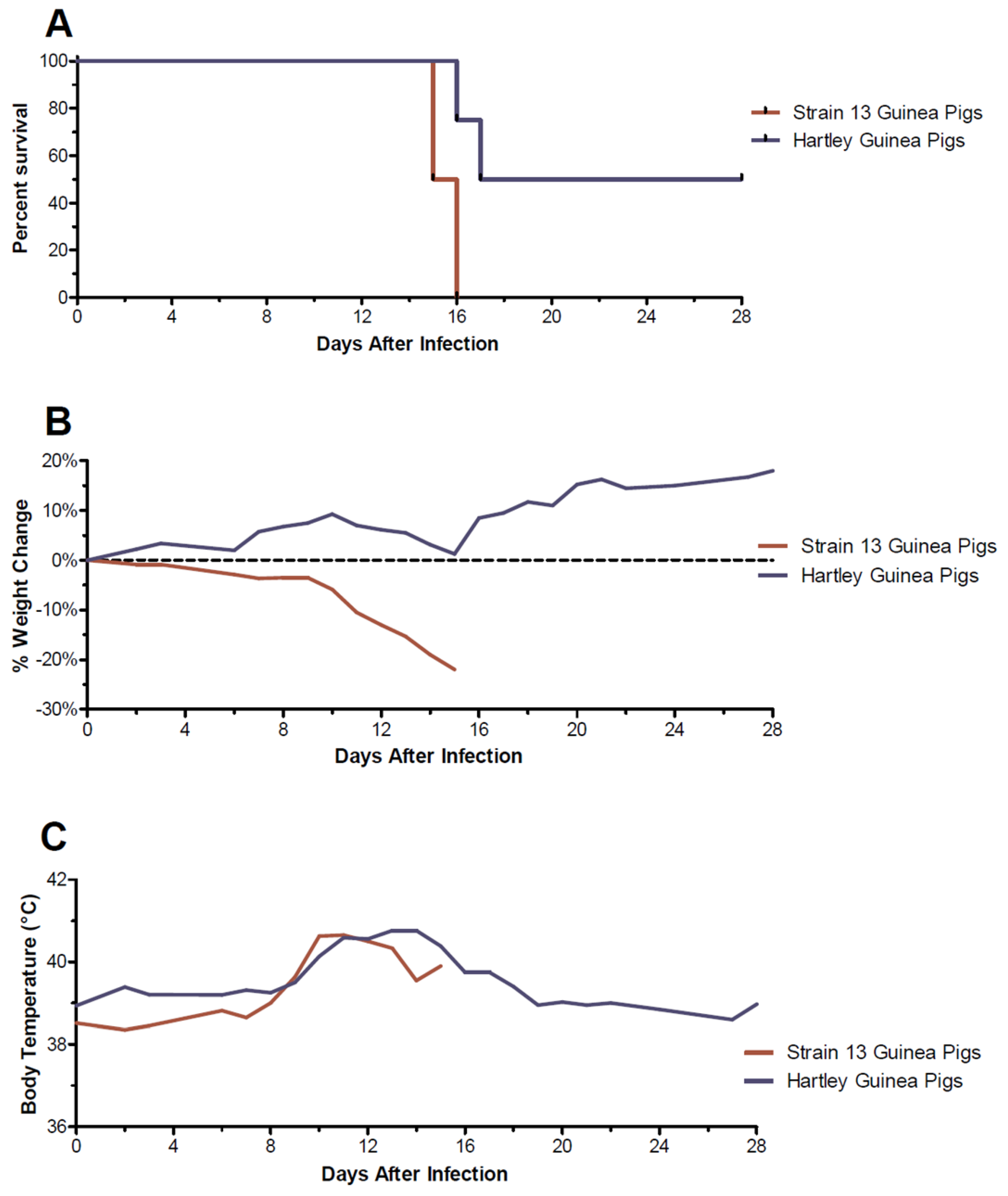
3.4. Clinical Observations in Guinea Pigs Infected with NML-61/GPA
3.5. Viral Titers in Solid Organs
3.6. Hematology, Serum Biochemistries, and Coagulation Parameters
3.7. Host Immune Responses
3.8. Pathology and Histopathological Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Frame, J.D.; Baldwin, J.M.; Gocke, D.J.; Troup, J.M. Lassa fever, a new virus disease of man from West Africa. I. Clinical description and pathological findings. Am. J. Trop. Med. Hyg. 1970, 19, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Ogbu, O.; Ajuluchukwu, E.; Uneke, C.J. Lassa fever in West African sub-region: An overview. J. Vector Borne Dis. 2007, 44, 1–11. [Google Scholar] [PubMed]
- McCormick, J.B.; Webb, P.A.; Krebs, J.W.; Johnson, K.M.; Smith, E.S. A Prospective Study of the Epidemiology and Ecology of Lassa Fever. J. Infect. Dis. 1987, 155, 437–444. [Google Scholar] [CrossRef]
- Bell-Kareem, A.R.; Smither, A.R. Epidemiology of Lassa Fever; Springer Nature: Berlin, Germany, 2021. [Google Scholar] [CrossRef]
- Monath, T.P.; Newhouse, V.F.; Kemp, G.E.; Setzer, H.W.; Cacciapuoti, A. Lassa virus isolation from Mastomys natalensis rodents during an epidemic in Sierra Leone. Science 1974, 185, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Sogoba, N.; Feldmann, H.; Safronetz, D. Lassa Fever in West Africa: Evidence for an Expanded Region of Endemicity. Zoonoses Public Health 2012, 59, 43–47. [Google Scholar] [CrossRef]
- Monath, T.P. A short history of Lassa fever: The first 10–15 years after discovery. Curr. Opin. Virol. 2019, 37, 77–83. [Google Scholar] [CrossRef]
- Fisher-Hoch, S.P.; Perez-Oronoz, G.; Tomori, O.; Perez-Oronoz, G.I.; Fakile, Y.; Hutwagner, L.; McCormick, J.B. Review of cases of nosocomial Lassa fever in Nigeria: The high price of poor medical practice. BMJ 1995, 311, 857–859. [Google Scholar] [CrossRef]
- Okokhere, P.; Colubri, A.; Azubike, C.; Iruolagbe, C.; Osazuwa, O.; Tabrizi, S.; Chin, E.; Asad, S.; Ediale, E.; Rafiu, M.; et al. Clinical and laboratory predictors of Lassa fever outcome in a dedicated treatment facility in Nigeria: A retrospective, observational cohort study. Lancet Infect. Dis. 2018, 18, 684–695. [Google Scholar] [CrossRef]
- Akpede, G.O.; Asogun, D.A.; Akogbenin, S.A.; Dawodu, S.O.; Momoh, M.O.; Dongo, A.E.; Ike, C.; Tobin, E.; Akpede, N.; Ogbaini-Emovon, E.; et al. Corrigendum: Caseload and Case Fatality of Lassa Fever in Nigeria, 2001–2018: A Specialist Center’s Experience and Its Implications. Front. Public Health 2019, 7, 170. [Google Scholar] [CrossRef]
- Kayem, N.D.; Benson, C.; Aye, C.Y.L.; Barker, S.; Tome, M.; Kennedy, S.; Ariana, P.; Horby, P. Lassa fever in pregnancy: A systematic review and meta-analysis. Trans. R. Soc. Trop. Med. Hyg. 2020, 114, 385–396. [Google Scholar] [CrossRef]
- Ilori, E.A.; Furuse, Y.; Ipadeola, O.B.; Dan-Nwafor, C.C.; Abubakaer, A.; Womi-Eteng, O.E.; Ogbani-Emovon, E.; Okogbenin, S.; Unigwe, U.; Ogah, E.; et al. Epidemiologic and clinical features of lassa fever outbreak in Nigeria, January 1–May 6, 2018. Emerg. Infect. Dis. 2019, 25, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Chika-Igwenyi, N.M.; Harrison, R.E.; Psarra, C.; Gil-Cuesta, J.; Gulamhusein, M.; Onwe, E.O.; Onoh, R.C.; Unigwe, U.S.; Ajayi, N.A.; Nnadozie, U.U.; et al. Early onset of neurological features differentiates two outbreaks of lassa fever in Ebonyi state, Nigeria during 2017–2018. PLoS Negl. Trop. Dis. 2021, 15, e0009169. [Google Scholar] [CrossRef] [PubMed]
- Babalola, S.O.; Babatunde, J.A.; Remilekun, O.M.; Amaobuchikwu, A.R.; Abiodun, A.M.; Jide, I.; Adeshina, A.S.I.; Chikwe, I.; Aremu, O.S. Lassa virus RNA detection from suspected cases in Nigeria, 2011–2017. Pan Afr. Med. J. 2019, 34, 76. [Google Scholar] [CrossRef] [PubMed]
- Tambo, E.; Adetunde, O.T.; Olalubi, O.A. Re-emerging Lassa fever outbreaks in Nigeria: Re-enforcing ‘One Health’ community surveillance and emergency response practice. Infect. Dis. Poverty 2018, 7, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-Y.; French, C.E.; Salam, A.P.; Dawson, S.; McAleenan, A.; McGuinness, L.A.; Savović, J.; Hornby, P.W.; Sterne, J.A.C. Lack of Evidence for Ribavirin Treatment of Lassa Fever in Systematic Review of Published and Unpublished Studies. Emerg. Infect. Dis. 2022, 28, 1559–1568. [Google Scholar] [CrossRef]
- Schmaljohn, C.; Safronetz, D. Editorial overview: Lassa virus. Curr. Opin. Virol. 2019, 37, vii–ix. [Google Scholar] [CrossRef]
- Sattler, R.A.; Paessler, S.; Ly, H.; Huang, C. Animal models of lassa fever. Pathogens 2020, 9, 197. [Google Scholar] [CrossRef]
- Safronetz, D.; Rosenke, K.; Westover, J.B.; Martellaro, C.; Okumura, A.; Furuta, Y.; Geisbert, J.; Saturday, G.; Komeno, T.; Geisbert, T.W.; et al. The broad-spectrum antiviral favipiravir protects Guinea pigs from lethal Lassa virus infection post-disease onset. Sci. Rep. 2015, 5, 14775. [Google Scholar] [CrossRef]
- Stein, D.R.; Warner, B.M.; Audet, J.; Soule, G.; Siragam, V.; Sroga, P.; Griffin, B.D.; Leung, A.; Grolla, A.; Tierney, K.; et al. Differential pathogenesis of closely related 2018 Nigerian outbreak clade III Lassa virus isolates. PLoS Pathog. 2021, 17, e1009966. [Google Scholar] [CrossRef]
- Safronetz, D.; Strong, J.E.; Feldmann, F.; Haddock, E.; Sogoba, N.; Brining, D.; Geisbert, T.W.; Scott, D.P.; Feldmann, H. A recently isolated Lassa virus from Mali demonstrates atypical clinical disease manifestations and decreased virulence in cynomolgus macaques. J. Infect. Dis. 2013, 207, 1316–1327. [Google Scholar] [CrossRef]
- Gowen, B.B.; Holbrook, M.R. Animal models of highly pathogenic RNA viral infections: Hemorrhagic fever viruses. Antivir. Res. 2008, 78, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Holbrook, M.R.; Gowen, B.B. Animal models of viral hemorrhagic fever. Antivir. Res. 2014, 112, 59–79. [Google Scholar] [CrossRef] [PubMed]
- Safronetz, D.; Feldmann, H.; Falzarano, D. Arenaviruses and filoviruses: Viral haemorrhagic fevers. In Medical Microbiology, 18th ed.; Churchill Livingstone: London, UK, 2012; pp. 546–558. ISBN 978-0-7020-4089-4. [Google Scholar]
- Safronetz, D.; Mire, C.; Rosenke, K.; Feldmann, F.; Haddock, E.; Geisbert, T.; Feldmann, H. A Recombinant Vesicular Stomatitis Virus-Based Lassa Fever Vaccine Protects Guinea Pigs and Macaques against Challenge with Geographically and Genetically Distinct Lassa Viruses. PLoS Negl. Trop. Dis. 2015, 9, e0003736. [Google Scholar] [CrossRef] [PubMed]







| Coding Region | Position | Mutation | Frequency | Coding Region | Position | Mutation | Frequency |
|---|---|---|---|---|---|---|---|
| L | 1221 | Asn→Asp | 58.7% | GPC | 213 | Met→Ile | 11% |
| L | 672 | Lys→Glu | 14.7% | NP | 435 | Val→Ile | 6.1% |
| L | 607 | Gly→Glu | 13.8% | NP | 228 | Ile→Val | 53.5% |
| L | 515 | Thr→fs | 6% | NP | 62 | Gly→Asp | 14.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deschambault, Y.; Soule, G.; Klassen, L.; Sloan, A.; Audet, J.; Azaransky, K.; Musa, A.S.; Ahmad, A.; Akinpelu, A.M.; Mba, N.; et al. An Outbred Guinea Pig Disease Model for Lassa Fever Using a Host-Adapted Clade III Nigerian Lassa Virus. Viruses 2023, 15, 769. https://doi.org/10.3390/v15030769
Deschambault Y, Soule G, Klassen L, Sloan A, Audet J, Azaransky K, Musa AS, Ahmad A, Akinpelu AM, Mba N, et al. An Outbred Guinea Pig Disease Model for Lassa Fever Using a Host-Adapted Clade III Nigerian Lassa Virus. Viruses. 2023; 15(3):769. https://doi.org/10.3390/v15030769
Chicago/Turabian StyleDeschambault, Yvon, Geoff Soule, Levi Klassen, Angela Sloan, Jonathan Audet, Kim Azaransky, Abdulmajid S. Musa, Adama Ahmad, Afolabi M. Akinpelu, Nwando Mba, and et al. 2023. "An Outbred Guinea Pig Disease Model for Lassa Fever Using a Host-Adapted Clade III Nigerian Lassa Virus" Viruses 15, no. 3: 769. https://doi.org/10.3390/v15030769
APA StyleDeschambault, Y., Soule, G., Klassen, L., Sloan, A., Audet, J., Azaransky, K., Musa, A. S., Ahmad, A., Akinpelu, A. M., Mba, N., Stein, D. R., Ranson, M., Almiski, M., Tierney, K., Fischer, G., Chan, M., & Safronetz, D. (2023). An Outbred Guinea Pig Disease Model for Lassa Fever Using a Host-Adapted Clade III Nigerian Lassa Virus. Viruses, 15(3), 769. https://doi.org/10.3390/v15030769






