Evaluation and Determination of a Suitable Passage Number of Codon Pair Deoptimized PRRSV-1 Vaccine Candidate in Pigs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Vaccine and Challenge Virus
2.3. Passages Limits of Attenuated E38-ORF7 CPD
2.4. Experimental Design
2.5. Serology
2.6. Quantification of the Virus in Serum and Lung Tissue
2.7. Histopathology
2.8. Statistical Analysis
3. Results
3.1. Genetic Variation via Passage Analysis
3.2. Evaluation of the Efficacy of the CPD Virus Various Passages
3.2.1. Clinical Evaluation
3.2.2. PRRSV-Specific Antibodies
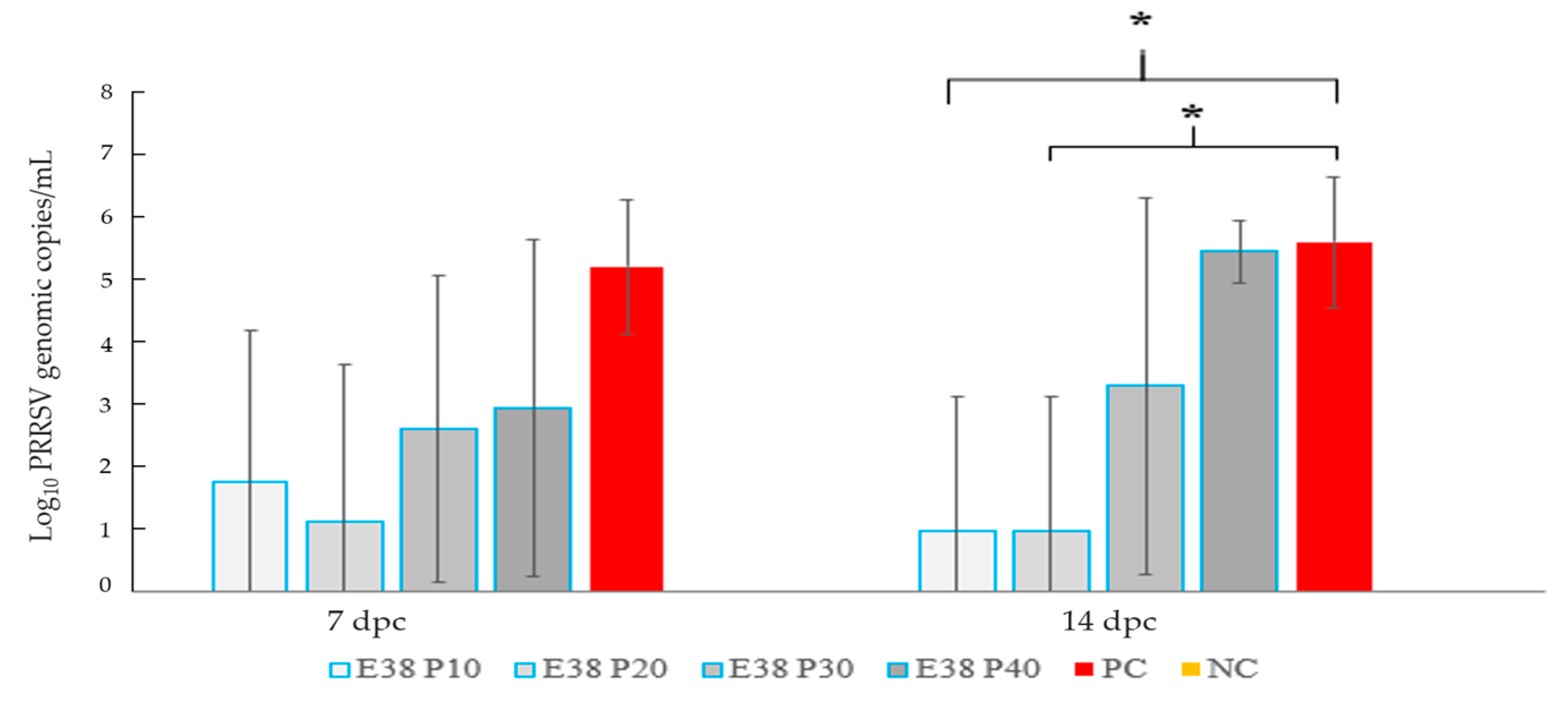
3.2.3. Quantification of PRRSV RNA in Serum
3.2.4. Microscopic Lesions Viral Load in Lung
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chae, C. Commercial PRRS modified Live virus vaccines. Vaccines 2021, 9, 185. [Google Scholar] [CrossRef]
- Kang, H.; Yu, J.E.; Shin, J.E.; Kang, A.; Kim, W.I.; Lee, C.; Lee, J.; Cho, I.S.; Choe, S.E.; Cha, S.H. Geographic distribution and molecular analysis of porcine reproductive and respiratory syndrome viruses circulating in swine farms in the Republic of Korea between 2013 and 2016. BMC Vet. Res. 2018, 14, 160. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Moon, S.H.; Jeong, C.G.; Park, G.S.; Park, J.Y.; Jeoung, H.Y.; Shin, G.E.; Ko, M.K.; Kim, S.H.; Lee, K.K.; et al. Whole-genome sequencing and genetic characteristics of representative porcine reproductive and respiratory syndrome virus (PRRSV) isolates in Korea. Virol. J. 2022, 19, 66. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.Y.; Campler, M.R.; Schroeder, D.C.; Yang, M.; Mor, S.K.; Ferreira, J.B.; Arruda, A.G. Detection of Multiple Lineages of PRRSV in Breeding and Growing Swine Farms. Front. Vet. Sci. 2022, 9, 884733. [Google Scholar] [CrossRef]
- Kuhn, J.H.; Lauck, M.; Bailey, A.L.; Shchetinin, A.M.; Vishnevskaya, T.V.; Bào, Y.; Ng, T.F.; LeBreton, M.; Schneider, B.S.; Gillis, A.; et al. Reorganization and expansion of the nidoviral family Arteriviridae. Arch. Virol. 2016, 161, 755–768. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Lam, T.T.; Hon, C.C.; Hui, R.K.; Faaberg, K.S.; Wennblom, T.; Murtaugh, M.P.; Stadejek, T.; Leung, F.C. Molecular epidemiology of PRRSV: A phylogenetic perspective. Virus. Res. 2010, 154, 7–17. [Google Scholar] [CrossRef]
- Stadejek, T.; Stankevicius, A.; Murtaugh, M.P.; Oleksiewicz, M.B. Molecular evolution of PRRSV in Europe: Current state of play. Vet. Microbiol. 2013, 165, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Lunney, J.K.; Fang, Y.; Ladinig, A.; Chen, N.; Li, Y.; Rowland, B.; Renukaradhya, G.J. Porcine reproductive and respiratory syndrome virus (PRRSV): Pathogenesis and interaction with the immune system. Annu. Rev. Anim. Biosci. 2016, 4, 129–154. [Google Scholar] [CrossRef]
- Nielsen, H.S.; Oleksiewicz, M.B.; Forsberg, R.; Stadejek, T.; Bøtner, A.; Storgaard, T. Reversion of a live porcine reproductive and respiratory syndrome virus vaccine investigated by parallel mutations. J. Gen. Virol. 2001, 82, 1263–1272. [Google Scholar] [CrossRef]
- Bian, T.; Sun, Y.; Hao, M.; Zhou, L.; Ge, X.; Guo, X.; Han, J.; Yang, H.A. A recombinant type 2 porcine reproductive and respiratory syndrome virus between NADC30-like and a MLV-like: Genetic characterization and pathogenicity of piglets. Infect. Genet. Evol. 2017, 54, 279–286. [Google Scholar] [CrossRef]
- Eclercy, J.; Renson, P.; Lebret, A.; Hirchaud, E.; Normand, V.; Andraud, M.; Paboeuf, F.; Blanchard, Y.; Rose, N.; Bourry, O.A. Field recombinant strain derived from two type1 porcine reproductive and respiratory syndrome virus (PRRSV-1) modified live vaccines show increased viremia and transmission in SPF pigs. Viruses 2019, 11, 296. [Google Scholar] [CrossRef] [PubMed]
- Franzo, G.; Cecchinato, M.; Martini, M.; Ceglie, L.; Gigli, A.; Drigo, M. Observation of high recombination occurrence of porcine reproductive and respiratory syndrome virus in field condition. Virus Res. 2014, 194, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Fang, L.; Xu, Z.; Liu, S.; Gao, J.; Jiang, Y.; Chen, H.; Xiao, S. Recombination in vaccine and circulating strains of porcine reproductive and respiratory syndrome viruses. Emerg. Infect. Dis. 2009, 15, 2032–2035. [Google Scholar] [CrossRef]
- Liu, J.; Zhou, X.; Zhai, J.; Wei, C.; Dai, A.; Yang, X.; Luo, M. Recombination in JXA1-R vaccine and NADC30-like strain of porcine reproductive and respiratory syndrome viruses. Vet. Microbiol. 2017, 204, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Shin, G.E.; Park, J.Y.; Lee, K.K.; Ko, M.K.; Ku, B.K.; Park, C.K.; Jeoung, H.Y. Genetic diversity of porcine reproductive and respiratory syndrome virus and evaluation of three one-step real-time RT-PCR assays in Korea. BMC Vet. Res. 2022, 18, 327. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Kang, R.; Yu, J.; Xie, B.; Chen, C.; Li, X.; Xie, J.; Ye, Y.; Xiao, L.; Zhang, J.; et al. Genetic characterization and pathogenicity of a novel recombined porcine reproductive and respiratory syndrome virus 2 among Nadc30-like, Jxa1-like and Mlv-like strains. Viruses 2018, 10, 551. [Google Scholar] [CrossRef]
- Charerntantanakul, W. Porcine reproductive and respiratory syndrome virus vaccines: Immunogenicity, efficacy and safety aspects. World J. Virol. 2012, 1, 23–30. [Google Scholar] [CrossRef]
- Renukaradhya, G.J.; Meng, X.J.; Calvert, J.G.; Roof, M.; Lager, K.M. Inactivated and subunit vaccines against porcine reproductive and respiratory syndrome: Current status and future direction. Vaccine 2015, 33, 3065–3072. [Google Scholar] [CrossRef]
- Coleman, J.R.; Papamichail, D.; Skiena, S.; Futcher, B.; Wimmer, E.; Mueller, S. Virus attenuation by Genome-scale Changes in Codon pair Bias. Science 2008, 320, 1784–1787. [Google Scholar] [CrossRef] [PubMed]
- Diaz-San Segundo, F.; Medina, G.N.; Spinard, E.; Kloc, A.; Ramirez-Medina, E.; Azzinaro, P.; Muller, S.; Rieder, E.; de Los Santos, T. Use of synonymous deoptimization of derived modified live attenuated strains of foot and mouth disease virus. Front. Microbiol. 2021, 11, 610286. [Google Scholar] [CrossRef]
- Evenson, D.; Gerber, P.F.; Xiao, C.T.; Halbur, P.G.; Wang, C.; Tian, D.; Ni, Y.Y.; Meng, X.J.; Opriessnig, T. A porcine reproductive and respiratory syndrome virus candidate vaccine based on the synthetic attenuated virus engineering approach is attenuated and effective in protecting against homologous virus challenge. Vaccine 2016, 34, 5546–5553. [Google Scholar] [CrossRef]
- Gao, L.; Wang, L.; Huang, C.; Yang, L.; Guo, X.K.; Yu, Z.; Liu, Y.; Yang, P.; Feng, W.H. HP-PRRSV is attenuated by de-optimization of codon pair bias in its RNA-dependent RNA polymerase nsp9 gene. Virology 2015, 485, 135–144. [Google Scholar] [CrossRef]
- LeNouen, C.; McCarty, T.; Brown, M.; Smith, M.L.; Lleras, R.; Dolan, M.A.; Mehedi, M.; Yang, L.; Luongo, C.; Liang, B.; et al. Genetic stability of genome scale deoptimized RNA virus vaccine candidates under selective pressure. Proc. Natl. Acad. Sci. USA 2017, 114, E386–E395. [Google Scholar] [CrossRef]
- Li, P.; Ke, X.; Wang, T.; Tan, Z.; Luo, D.; Miao, Y.; Sun, J.; Zhang, Y.; Liu, Y.; Hu, Q.; et al. Zika virus attenuation by codon pair deoptimization induces sterilizing immunity in Mouse models. J. Virol. 2018, 92, e00701-18. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo, M.M.; Nogales, A.; Chiem, K.; Blasco, R.; Martinez-Sobrido, L. Vaccinia virus attenuation by codon pair deoptimization of the A24R gene for vaccine development. Microbiol. Spectr. 2022, 10, e00272-22. [Google Scholar] [CrossRef] [PubMed]
- Martrus, G.; Nevot, M.; Andres, C.; Clotet, B.; Martinez, M.A. Changes in codon-pair bias of human immunodeficiency virus type 1 have profound effects on virus replication in cell culture. Retrovirology 2013, 10, 78. [Google Scholar] [CrossRef]
- Ni, Y.Y.; Zhao, Z.; Opriessnig, T.; Subramaniam, S.; Zhou, L.; Cao, D.; Cao, Q.; Yang, H.; Meng, X.J. Codon aided codon pairs deoptimization of the major envelope GP5 gene attenuates porcine reproductive and respiratory syndrome virus. Virology 2014, 450–451, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Nogales, A.; Baker, S.F.; Ortiz-Riaño, E.; Dewhurst, S.; Topham, D.J.; Martínez-Sobrido, L. Influenza A virus attenuation by codon deoptimization of the NS gene for vaccine development. J. Virol. 2014, 88, 10525–10540. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Baek, J.H.; Cho, S.H.; Jeong, J.; Chae, C.; You, S.H.; Cha, S.H. Field porcine reproductive and respiratory syndrome viruses (PRRSV) attenuated by codon pair deoptimization (CPD) in NSP1 protected pigs from heterologous challenge. Virology 2020, 540, 172–183. [Google Scholar] [CrossRef]
- Park, C.; Lee, M.S.; Baek, J.H.; Cho, S.H.; Hyun, B.H.; You, S.H.; Cha, S.H. Intradermal co-inoculation of codon pair deoptimization (CPD)- attenuated chimeric porcine reproductive and respiratory syndrome virus (PRRSV) with Toll like receptor (TLR) agonists enhanced the protective effects in pigs against heterologous challenge. Vet. Microbiol. 2021, 256, 109048. [Google Scholar] [CrossRef]
- Lee, M.A.; You, S.H.; Jayaramaiah, U.; Shin, E.G.; Song, S.M.; Ju, L.; Kang, S.J.; Cho, S.H.; Huyn, B.H.; Lee, H.S. Codon Pair Deoptimization (CPD)-atteanuated PRRSV-2 Vaccination exhibit immunity to virulent PRRSV challenge in Pigs. Vaccines 2023, 11, 777. [Google Scholar] [CrossRef]
- Bull, J.J. Evolutionary reversion of live viral vaccines: Can genetic engineering subdue it? Virus Evol. 2015, 1, vev005. [Google Scholar] [CrossRef]
- Tsai, H.J.; Saif, Y.M. Effect of cell-culture passage on the pathogenicity and immunogenicity of the two variant strains of the Infectious Bursal disease virus. Avian Dis. 1992, 36, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Kwang, J.; Yoon, I.J.; Joo, H.S.; Frey, M.L. Enhanced replication of porcine reproductive and respiratory syndrome (PRRS) virus in a homogenous subpopulation of MA-104 cell line. Arch. Virol. 1993, 133, 477–483. [Google Scholar] [CrossRef]
- Park, C.; Seo, H.W.; Han, K.; Kang, I.; Chae, C. Efficacy of a new modified live porcine reproductive and respiratory syndrome virus (PRRSV) vaccine (Fostera PRRS) against heterologous PRRSV challenge. Vet. Microbiol. 2014, 172, 432–442. [Google Scholar] [CrossRef]
- Chung, W.B.; Chan, W.H.; Chaung, H.C.; Lien, Y.; Wu, C.C.; Huang, Y.L. Real-time PCR for quantitation of porcine reproductive and respiratory syndrome virus and porcine circovirus type 2 in naturally-infected and challenged pigs. J. Virol. Methods 2005, 124, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Halbur, P.G.; Paul, P.S.; Frey, M.L.; Landgraf, J.; Eernisse, K.; Meng, X.J.; Lum, M.A.; Andrews, J.J.; Rathje, J.A. Comparison of the pathogenicity of two US porcine reproductive and respiratory syndrome virus isolates with that of the Lelystad virus. Vet. Pathol. 1995, 32, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Nelsen, C.J.; Murtaugh, M.P.; Schmitt, B.J.; Faaberg, K.S. Recombination between North American Strains of Porcine reproductive and respiratory syndrome virus. Virus Res. 1999, 61, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Chen, Q.; Wang, L.; Madson, D.; Harmon, K.; Gauger, P.; Zhang, J.; Li, G. Recombination between vaccine and field strains of Porcine reproductive and Respiratory syndrome virus. Emerg. Infect. Dis. 2019, 25, 2335–2337. [Google Scholar] [CrossRef]
- Martínez, M.A.; Jordan-Paiz, A.; Franco, S.; Nevot, M. Synonymous virus genome recoding as a tool to impact viral fitness. Trends Microbiol. 2016, 24, 134–147. [Google Scholar] [CrossRef]
- Stauft, C.B.; Song, Y.; Gorbatsevych, O.; Pantoja, P.; Rodriguez, I.V.; Futcher, B.; Sariol, C.A.; Wimmer, E. Extensive genomic recoding by Codon-pair deoptimization selective for mammals is a flexible tool to generate attenuated vaccine candidates for dengue virus 2. Virology 2019, 537, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Trus, I.; Oh, D.Y.; Kvisgaard, L.K.; Rappe, J.C.F.; Ruggli, N.; Vanderheijden, N.; Larsen, L.E.; Lefevre, F.; Nauwynck, H.J. A triple Amino acid substitution at position 88/94/95 in glycoproten GP2a of Type 1 porcine reproductive and respiratory syndrome virus (PRRSV1) is responsible for adaptation to MARC-145 cells. Viruses 2019, 11, 36. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Setiyono, A.; Kobayashi, M.; Takigami, S.; Fukushi, H.; Hirai, K. Infectious bursal disease live vaccines: Changes in the virus population during serial passage in chickens and chicken embryo fibroblast cells. Avian Dis. 2000, 44, 284–290. [Google Scholar] [CrossRef] [PubMed]


| Passage 10 | Passage 20 | Passage 30 | Passage 40 | |
|---|---|---|---|---|
| Number of nt change | 7 | 10 | 16 | 19 |
| nucleotide | ORF1a (2941nt, C->T) ORF1a (6778nt, G->A) ORF1b (4090nt, T->C) ORF2a (509nt, T->C) ORF3 (214nt, A->G) ORF5 (50nt, T->C) ORF7 (327nt, C->T) | ORF1a(2613nt, C->A) ORF1a(4990nt, A->G) ORF4(529nt, T->G) | ORF1a (5814nt, A->G) ORF2a (282nt, G->A) ORF2a (591nt, G->A) ORF4 (519nt, C->T) ORF5 (109nt, A->G) ORF7 (204nt, T->C) | ORF1a (721nt, C->T) ORF1a (2981nt, A->G) ORF1a (3624nt, T->C) |
| Number of a.a change | 6 | +3 (9) | +2 (11) | +2 (13) |
| a.a | ORF1a (981a.a, Arg->Cys) ORF1a (2226a.a, Asp->Asn) ORF1b (1364a.a, Tyr->His) ORF2a (170a.a, Val->Ala) ORF3 (72a.a, Ser->Gly) ORF5 (17a.a, Phe->Ser) | ORF1a (871a.a, Ser->Arg) ORF1a (1664a.a, Thr->Ala) ORF4 (177a.a, Phe->Val) | ORF2a (94a.a, Met->Ile) ORF5 (37a.a, Asn->Asp) | ORF1a (241a.a, Leu->Phe) ORF1a (994a.a, Gln->Arg) |
| 0 dpi | 7 dpi | 14 dpi | 21 dpi | 28 dpi | 35 dpi | 42 dpi | |
|---|---|---|---|---|---|---|---|
| Passage 10 | 0 0% | 0 0% | 0.46 80% | 0.68 100% | 0.73 100% | 1.07 100% | 1.15 100% |
| Passage 20 | 0 0% | 0 0% | 0.41 80% | 0.59 100% | 0.71 100% | 0.91 100% | 1.16 100% |
| Passage 30 | 0 0% | 0 0% | 0 0% | 0.3 60% | 0.31 60% | 0.58 80% | 1.48 100% |
| Passage 40 | 0 0% | 0 0% | 0 0% | 0.23 40% | 0.28 40% | 0.44 80% | 1.24 100% |
| PC | 0 0% | 0 0% | 0 0% | 0 0% | 0 0% | 0.08 20% | 1.14 100% |
| NC | 0 0% | 0 0% | 0 0% | 0 0% | 0 0% | 0 0% | 0 0% |
| Passage 10 | Passage 20 | Passage 30 | Passage 40 | PC | NC | |
|---|---|---|---|---|---|---|
| Lung lesion score | 0.46 ± 0.29 * | 0.53 ± 0.18 * | 1.33 ± 0.33 | 1.6 ± 0.27 | 1.73 ± 0.27 | 0.1 3± 0.18 * |
| Log10 PRRSV genomic copies/g | 0 ± 0 * | 0 ± 0 * | 1.66 ± 2.28 * | 2.94 ± 2.69 | 5.46 ± 0.62 | 0 ± 0 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-A.; You, S.-H.; Jayaramaiah, U.; Shin, E.-G.; Song, S.-M.; Ju, L.; Kang, S.-J.; Cho, S.-H.; Hyun, B.-H.; Lee, H.-S. Evaluation and Determination of a Suitable Passage Number of Codon Pair Deoptimized PRRSV-1 Vaccine Candidate in Pigs. Viruses 2023, 15, 1071. https://doi.org/10.3390/v15051071
Lee M-A, You S-H, Jayaramaiah U, Shin E-G, Song S-M, Ju L, Kang S-J, Cho S-H, Hyun B-H, Lee H-S. Evaluation and Determination of a Suitable Passage Number of Codon Pair Deoptimized PRRSV-1 Vaccine Candidate in Pigs. Viruses. 2023; 15(5):1071. https://doi.org/10.3390/v15051071
Chicago/Turabian StyleLee, Min-A, Su-Hwa You, Usharani Jayaramaiah, Eun-Gyeong Shin, Seung-Min Song, Lanjeong Ju, Seok-Jin Kang, Sun-Hee Cho, Bang-Hun Hyun, and Hyang-Sim Lee. 2023. "Evaluation and Determination of a Suitable Passage Number of Codon Pair Deoptimized PRRSV-1 Vaccine Candidate in Pigs" Viruses 15, no. 5: 1071. https://doi.org/10.3390/v15051071
APA StyleLee, M.-A., You, S.-H., Jayaramaiah, U., Shin, E.-G., Song, S.-M., Ju, L., Kang, S.-J., Cho, S.-H., Hyun, B.-H., & Lee, H.-S. (2023). Evaluation and Determination of a Suitable Passage Number of Codon Pair Deoptimized PRRSV-1 Vaccine Candidate in Pigs. Viruses, 15(5), 1071. https://doi.org/10.3390/v15051071






