Ebolavirus Species-Specific Interferon Antagonism Mediated by VP24
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cells
2.2. Generation of Mutated Viruses
2.3. EBOV Tetracistronic Minigenome Reporter Assay
2.4. ISG54 Luciferase Assay
2.5. STAT1 Nuclear Translocation Assays
2.6. Viral Replication Kinetics in U3A Cells
2.7. RNA Isolation
2.8. Quantification of gRNA in Supernatants
2.9. Quantification of gRNA and mRNA in Cell Lysates
2.10. Quantification of IFNλ1 Expression in 769-P Cells
2.11. Quantification of IFNβ and ISG15 Expression in 769-P cells
2.12. Analysis of VP24 by Western Blotting
2.13. Statistical Methods
3. Results
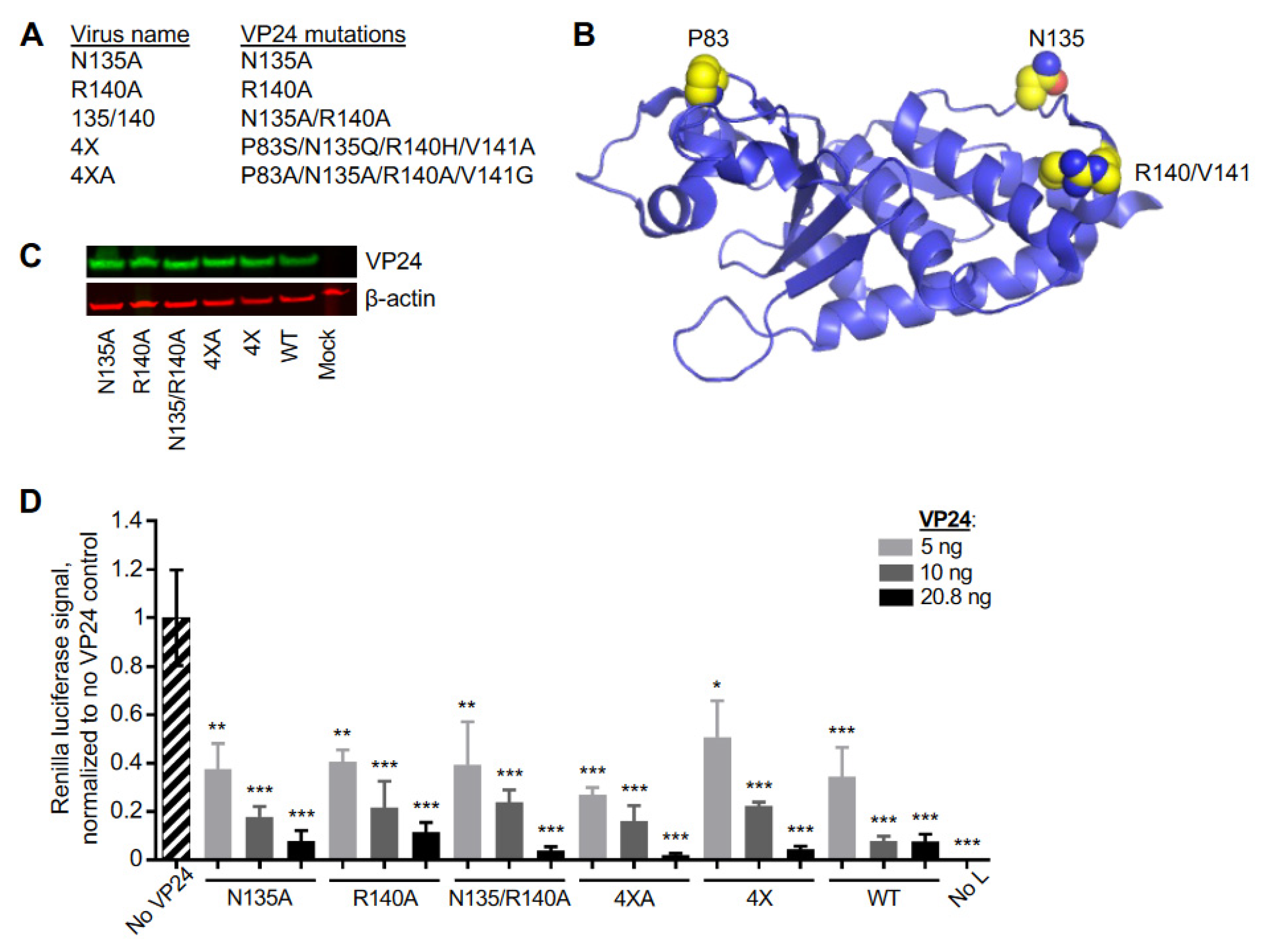
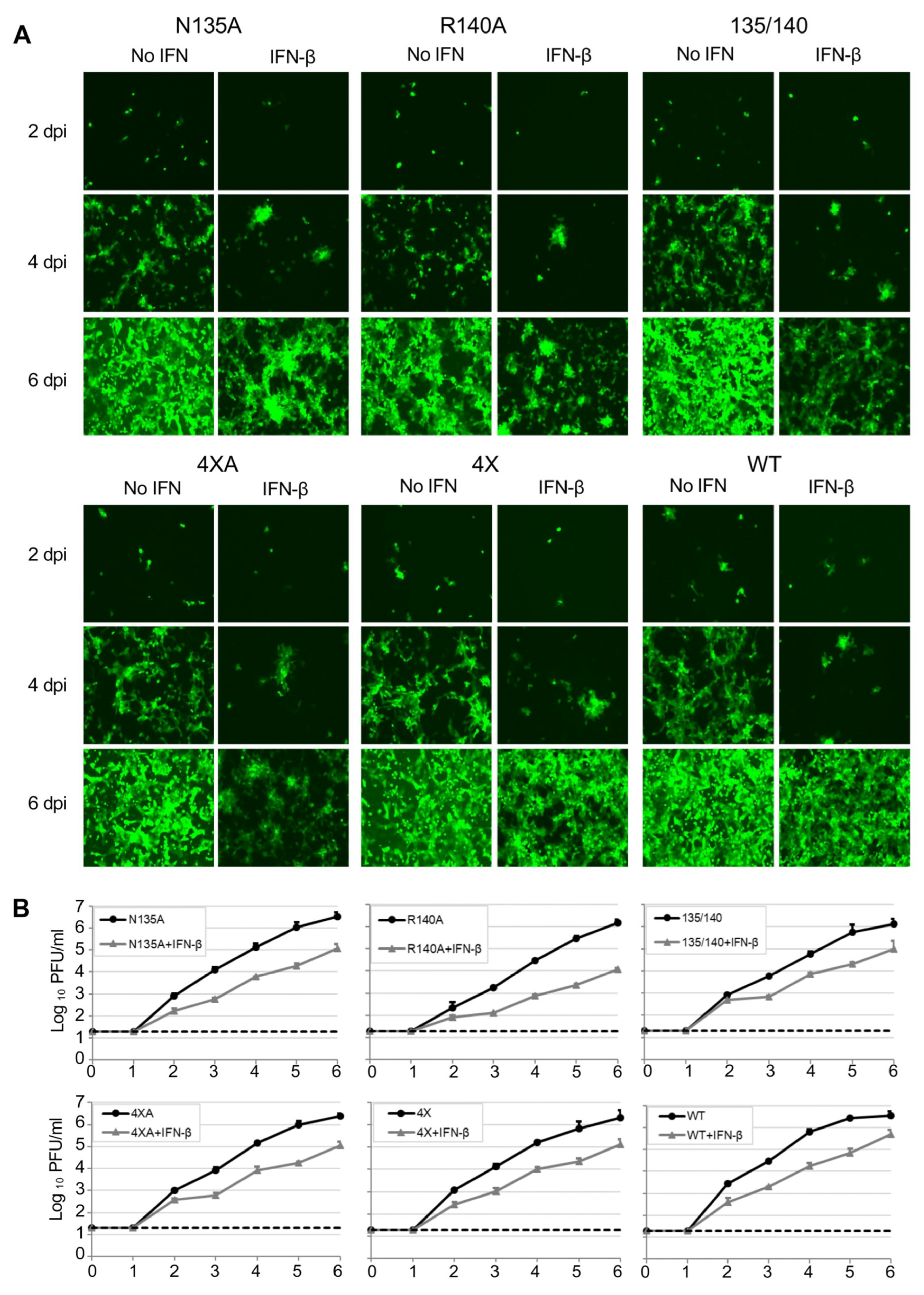
3.1. eVP24 KPNA Interface Amino Acids Are Required for Effective Replication of the Virus
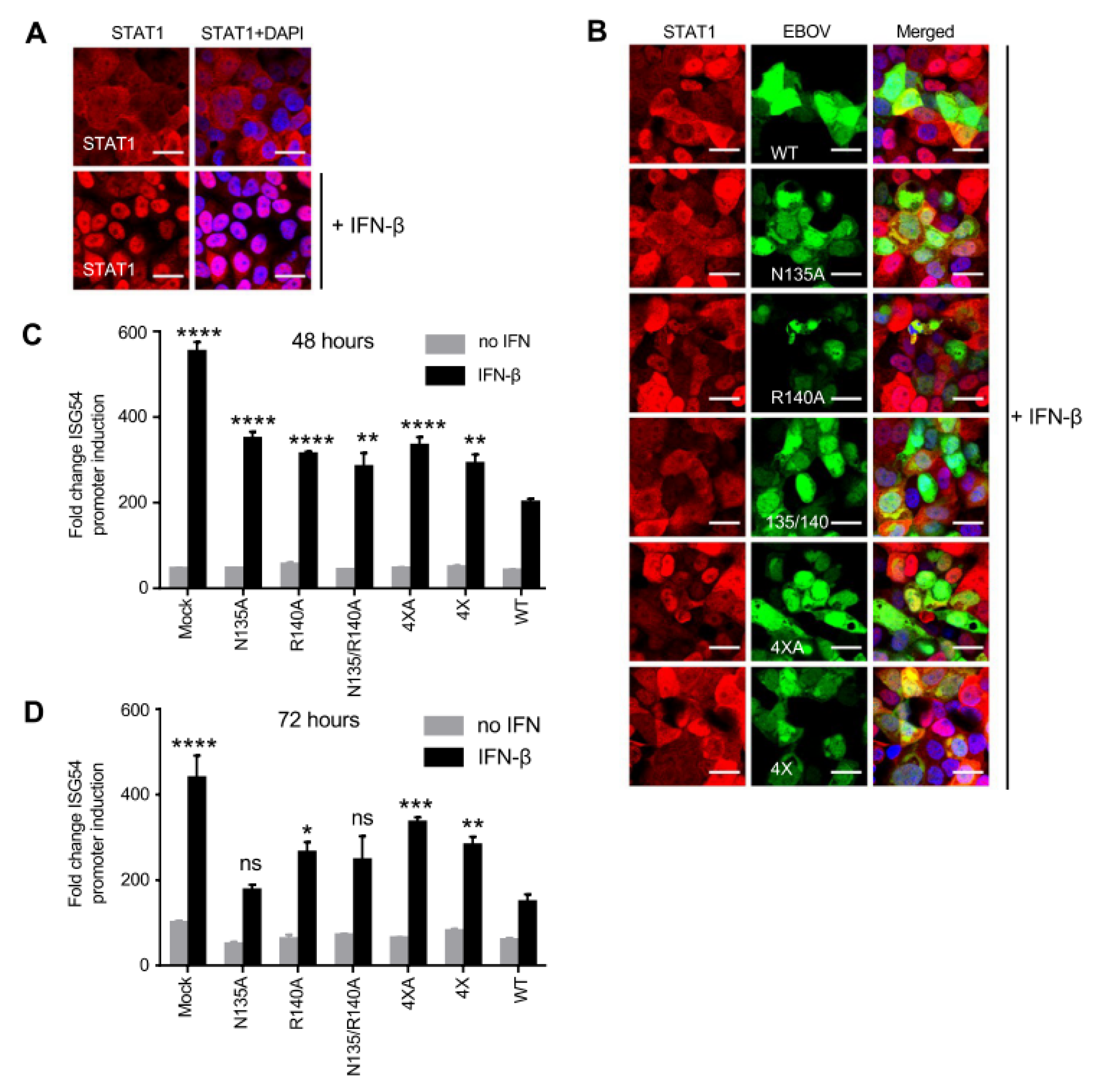
3.2. eVP24 KPNA Interface Amino Acids Inhibit IFN-mediated STAT1 Nuclear Translocation
3.3. eVP24 R140 Is Required for Effective EBOV Replication Independent of IFN-I Antagonism
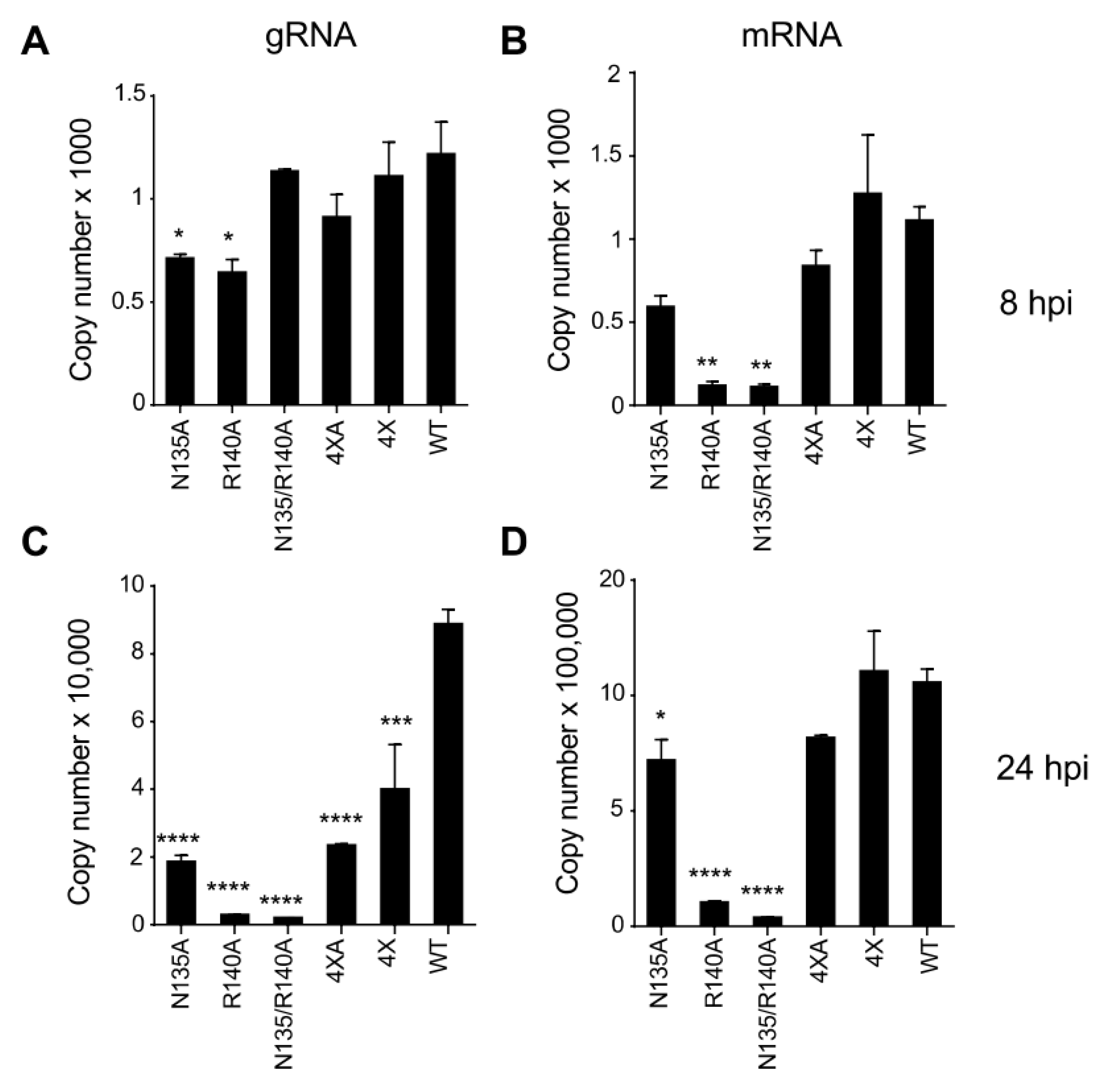
3.4. Mutations in eVP24 KPNA Interface Reduce the Amounts of Both Viral Genome and mRNA
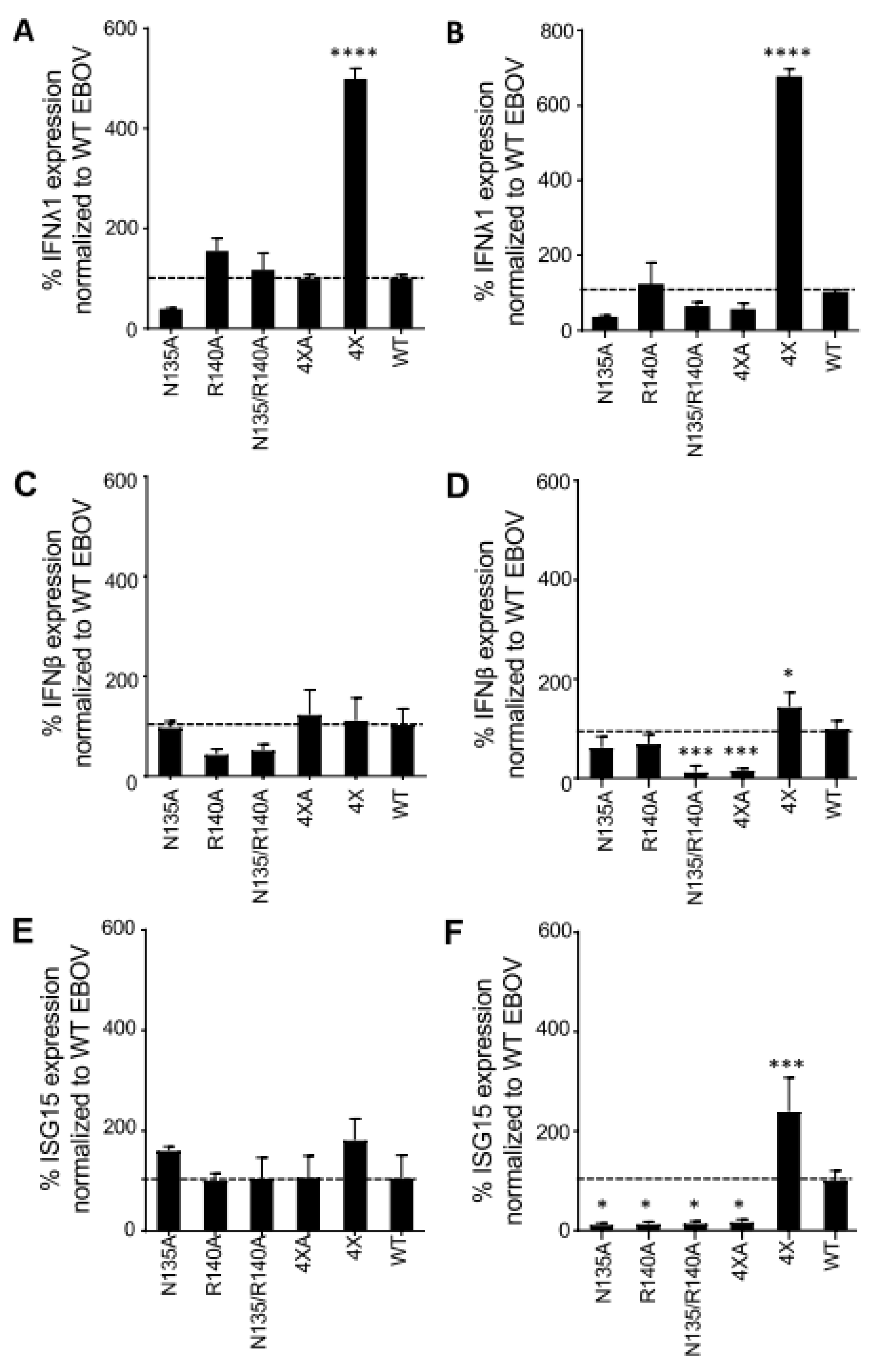
3.5. Unlike WT eVP24, eVP24 with bVP24 Interface Residues Does Not Inhibit IFNλ1 or IFNβ Expression
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goldstein, T.; Anthony, S.J.; Gbakima, A.; Bird, B.H.; Bangura, J.; Tremeau-Bravard, A.; Belaganahalli, M.N.; Wells, H.L.; Dhanota, J.K.; Liang, E.; et al. The discovery of Bombali virus adds further support for bats as hosts of ebolaviruses. Nat. Microbiol. 2018, 3, 1084–1089. [Google Scholar] [CrossRef] [PubMed]
- Jacob, S.T.; Crozier, I.; Fischer, W.A., 2nd; Hewlett, A.; Kraft, C.S.; Vega, M.A.; Soka, M.J.; Wahl, V.; Griffiths, A.; Bollinger, L.; et al. Ebola virus disease. Nat. Rev. Dis. Prim. 2020, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Martell, H.J.; Masterson, S.G.; McGreig, J.E.; Michaelis, M.; Wass, M.N. Is the Bombali virus pathogenic in humans? Bioinformatics 2019, 35, 3553–3558. [Google Scholar] [CrossRef] [PubMed]
- Yamaoka, S.; Ebihara, H. Pathogenicity and Virulence of Ebolaviruses with Species- and Variant-specificity. Virulence 2021, 12, 885–901. [Google Scholar] [CrossRef]
- Messaoudi, I.; Amarasinghe, G.K.; Basler, C.F. Filovirus pathogenesis and immune evasion: Insights from Ebola virus and Marburg virus. Nat. Rev. Microbiol. 2015, 13, 663–676. [Google Scholar] [CrossRef]
- Basler, C.F.; Mikulasova, A.; Martinez-Sobrido, L.; Paragas, J.; Muhlberger, E.; Bray, M.; Klenk, H.D.; Palese, P.; Garcia-Sastre, A. The Ebola virus VP35 protein inhibits activation of interferon regulatory factor 3. J. Virol. 2003, 77, 7945–7956. [Google Scholar] [CrossRef]
- Cardenas, W.B.; Loo, Y.M.; Gale, M., Jr.; Hartman, A.L.; Kimberlin, C.R.; Martinez-Sobrido, L.; Saphire, E.O.; Basler, C.F. Ebola Virus VP35 Protein Binds Double-Stranded RNA and Inhibits Alpha/Beta Interferon Production Induced by RIG-I Signaling. J. Virol. 2006, 80, 5168–5178. [Google Scholar] [CrossRef]
- Prins, K.C.; Cardenas, W.B.; Basler, C.F. Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. J. Virol. 2009, 83, 3069–3077. [Google Scholar] [CrossRef]
- Leung, D.W.; Ginder, N.D.; Fulton, D.B.; Nix, J.; Basler, C.F.; Honzatko, R.B.; Amarasinghe, G.K. Structure of the Ebola VP35 interferon inhibitory domain. Proc. Natl. Acad. Sci. USA 2009, 106, 411–416. [Google Scholar] [CrossRef]
- Leung, D.W.; Prins, K.C.; Borek, D.M.; Farahbakhsh, M.; Tufariello, J.M.; Ramanan, P.; Nix, J.C.; Helgeson, L.A.; Otwinowski, Z.; Honzatko, R.B.; et al. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat. Struct. Mol. Biol. 2010, 17, 165–172. [Google Scholar] [CrossRef]
- Reid, S.P.; Leung, L.W.; Hartman, A.L.; Martinez, O.; Shaw, M.L.; Carbonnelle, C.; Volchkov, V.E.; Nichol, S.T.; Basler, C.F. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J. Virol. 2006, 80, 5156–5167. [Google Scholar] [CrossRef] [PubMed]
- Mateo, M.; Reid, S.P.; Leung, L.W.; Basler, C.F.; Volchkov, V.E. Ebolavirus VP24 Binding to Karyopherins Is Required for Inhibition of Interferon Signaling. J. Virol. 2010, 84, 1169–1175. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.P.; Valmas, C.; Martinez, O.; Sanchez, F.M.; Basler, C.F. Ebola virus VP24 proteins inhibit the interaction of NPI-1 subfamily karyopherin alpha proteins with activated STAT1. J. Virol. 2007, 81, 13469–13477. [Google Scholar] [CrossRef]
- Xu, W.; Edwards, M.R.; Borek, D.M.; Feagins, A.R.; Mittal, A.; Alinger, J.B.; Berry, K.N.; Yen, B.; Hamilton, J.; Brett, T.J.; et al. Ebola virus VP24 targets a unique NLS binding site on karyopherin alpha 5 to selectively compete with nuclear import of phosphorylated STAT1. Cell Host Microbe 2014, 16, 187–200. [Google Scholar] [CrossRef]
- Ebihara, H.; Takada, A.; Kobasa, D.; Jones, S.; Neumann, G.; Theriault, S.; Bray, M.; Feldmann, H.; Kawaoka, Y. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2006, 2, e73. [Google Scholar] [CrossRef] [PubMed]
- Hartman, A.L.; Bird, B.H.; Towner, J.S.; Antoniadou, Z.A.; Zaki, S.R.; Nichol, S.T. Inhibition of IRF-3 activation by VP35 is critical for the high level of virulence of ebola virus. J. Virol. 2008, 82, 2699–2704. [Google Scholar] [CrossRef] [PubMed]
- Prins, K.C.; Delpeut, S.; Leung, D.W.; Reynard, O.; Volchkova, V.A.; Reid, S.P.; Ramanan, P.; Cardenas, W.B.; Amarasinghe, G.K.; Volchkov, V.E.; et al. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J. Virol. 2010, 84, 3004–3015. [Google Scholar] [CrossRef]
- Mateo, M.; Carbonnelle, C.; Reynard, O.; Kolesnikova, L.; Nemirov, K.; Page, A.; Volchkova, V.A.; Volchkov, V.E. VP24 is a molecular determinant of Ebola virus virulence in guinea pigs. J. Infect. Dis. 2011, 204 (Suppl. S3), S1011–S1020. [Google Scholar] [CrossRef]
- Woolsey, C.; Menicucci, A.R.; Cross, R.W.; Luthra, P.; Agans, K.N.; Borisevich, V.; Geisbert, J.B.; Mire, C.E.; Fenton, K.A.; Jankeel, A.; et al. A VP35 Mutant Ebola Virus Lacks Virulence but Can Elicit Protective Immunity to Wild-Type Virus Challenge. Cell. Rep. 2019, 28, 3032–3046.e6. [Google Scholar] [CrossRef]
- Vidal, S.; Sánchez-Aparicio, M.; Seoane, R.; El Motiam, A.; Nelson, E.V.; Bouzaher, Y.H.; Baz-Martínez, M.; García-Dorival, I.; Gonzalo, S.; Vázquez, E.; et al. Expression of the Ebola Virus VP24 Protein Compromises the Integrity of the Nuclear Envelope and Induces a Laminopathy-like Cellular Phenotype. mBio 2021, 12, e0097221. [Google Scholar] [CrossRef]
- Zhang, A.P.; Bornholdt, Z.A.; Liu, T.; Abelson, D.M.; Lee, D.E.; Li, S.; Woods, V.L., Jr.; Saphire, E.O. The Ebola Virus Interferon Antagonist VP24 Directly Binds STAT1 and Has a Novel, Pyramidal Fold. PLoS Pathog. 2012, 8, e1002550. [Google Scholar] [CrossRef]
- Schwarz, T.M.; Edwards, M.R.; Diederichs, A.; Alinger, J.B.; Leung, D.W.; Amarasinghe, G.K.; Basler, C.F. VP24-Karyopherin Alpha Binding Affinities Differ between Ebolavirus Species, Influencing Interferon Inhibition and VP24 Stability. J. Virol. 2017, 91, e01715-16. [Google Scholar] [CrossRef]
- McKendry, R.; John, J.; Flavell, D.; Muller, M.; Kerr, I.M.; Stark, G.R. High-frequency mutagenesis of human cells and characterization of a mutant unresponsive to both alpha and gamma interferons. Proc. Natl. Acad. Sci. USA 1991, 88, 11455–11459. [Google Scholar] [CrossRef]
- Towner, J.S.; Paragas, J.; Dover, J.E.; Gupta, M.; Goldsmith, C.S.; Huggins, J.W.; Nichol, S.T. Generation of eGFP expressing recombinant Zaire ebolavirus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology 2005, 332, 20–27. [Google Scholar] [CrossRef]
- Neumann, G.; Feldmann, H.; Watanabe, S.; Lukashevich, I.; Kawaoka, Y. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J. Virol. 2002, 76, 406–410. [Google Scholar] [CrossRef]
- Wang, G.P.; Bushman, F.D. A statistical method for comparing viral growth curves. J. Virol. Methods 2006, 135, 118–123. [Google Scholar] [CrossRef]
- El-Sayed, N.S.; Jureka, A.S.; Edwards, M.R.; Lohan, S.; Williams, C.G.; Keiser, P.T.; Davey, R.A.; Totonchy, J.; Tiwari, R.K.; Basler, C.F.; et al. Synthesis and antiviral activity of fatty acyl conjugates of remdesivir against severe acute respiratory syndrome coronavirus 2 and Ebola virus. Eur. J. Med. Chem. 2021, 226, 113862. [Google Scholar] [CrossRef]
- Meyer, M.; Garron, T.; Lubaki, N.M.; Mire, C.E.; Fenton, K.A.; Klages, C.; Olinger, G.G.; Geisbert, T.W.; Collins, P.L.; Bukreyev, A. Aerosolized Ebola vaccine protects primates and elicits lung-resident T cell responses. J. Clin. Investig. 2015, 125, 3241–3255. [Google Scholar] [CrossRef]
- Prasad, A.N.; Ronk, A.J.; Widen, S.G.; Wood, T.G.; Basler, C.F.; Bukreyev, A. Ebola Virus Produces Discrete Small Noncoding RNAs Independently of the Host MicroRNA Pathway Which Lack RNA Interference Activity in Bat and Human Cells. J. Virol. 2020, 94, e01441-19. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Watanabe, S.; Noda, T.; Halfmann, P.; Jasenosky, L.; Kawaoka, Y. Ebola virus (EBOV) VP24 inhibits transcription and replication of the EBOV genome. J. Infect. Dis. 2007, 196 (Suppl. S2), S284–S290. [Google Scholar] [CrossRef] [PubMed]
- Watt, A.; Moukambi, F.; Banadyga, L.; Groseth, A.; Callison, J.; Herwig, A.; Ebihara, H.; Feldmann, H.; Hoenen, T. A novel life cycle modeling system for Ebola virus shows a genome length-dependent role of VP24 in virus infectivity. J. Virol. 2014, 88, 10511–10524. [Google Scholar] [CrossRef] [PubMed]
- Desmyter, J.; Melnick, J.L.; Rawls, W.E. Defectiveness of interferon production and of rubella virus interference in a line of African green monkey kidney cells (Vero). J. Virol. 1968, 2, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Kato, A.; Kiyotani, K.; Kubota, T.; Yoshida, T.; Tashiro, M.; Nagai, Y. Importance of the anti-interferon capacity of Sendai virus C protein for pathogenicity in mice. J. Virol. 2007, 81, 3264–3271. [Google Scholar] [CrossRef]
- Cuevas, R.A.; Ghosh, A.; Wallerath, C.; Hornung, V.; Coyne, C.B.; Sarkar, S.N. MOV10 Provides Antiviral Activity against RNA Viruses by Enhancing RIG-I-MAVS-Independent IFN Induction. J. Immunol. 2016, 196, 3877–3886. [Google Scholar] [CrossRef]
- Hoenen, T.; Jung, S.; Herwig, A.; Groseth, A.; Becker, S. Both matrix proteins of Ebola virus contribute to the regulation of viral genome replication and transcription. Virology 2010, 403, 56–66. [Google Scholar] [CrossRef]
- Mateo, M.; Carbonnelle, C.; Martinez, M.J.; Reynard, O.; Page, A.; Volchkova, V.A.; Volchkov, V.E. Knockdown of Ebola virus VP24 impairs viral nucleocapsid assembly and prevents virus replication. J. Infect. Dis. 2011, 204 (Suppl. S3), S892–S896. [Google Scholar] [CrossRef]
- Olejnik, J.; Hume, A.J.; Leung, D.W.; Amarasinghe, G.K.; Basler, C.F.; Mühlberger, E. Filovirus Strategies to Escape Antiviral Responses. Curr. Top. Microbiol. Immunol. 2017, 411, 293–322. [Google Scholar]
- He, F.; Melén, K.; Maljanen, S.; Lundberg, R.; Jiang, M.; Österlund, P.; Kakkola, L.; Julkunen, I. Ebolavirus protein VP24 interferes with innate immune responses by inhibiting interferon-λ1 gene expression. Virology 2017, 509, 23–34. [Google Scholar] [CrossRef]
- Pappalardo, M.; Collu, F.; Macpherson, J.; Michaelis, M.; Fraternali, F.; Wass, M.N. Investigating Ebola virus pathogenicity using molecular dynamics. BMC Genom. 2017, 18, 566. [Google Scholar] [CrossRef]
- Chakraborty, S.; Rao, B.; Asgeirsson, B.; Dandekar, A. Correlating the ability of VP24 protein from Ebola and Marburg viruses to bind human karyopherin to their immune suppression mechanism and pathogenicity using computational methods [version 2; peer review: 2 approved with reservations]. F1000Research 2014, 3. [Google Scholar] [CrossRef]
- Pappalardo, M.; Juliá, M.; Howard, M.J.; Rossman, J.S.; Michaelis, M.; Wass, M.N. Conserved differences in protein sequence determine the human pathogenicity of Ebolaviruses. Sci. Rep. 2016, 6, 23743. [Google Scholar] [CrossRef]
- Ding, J.N.; Zhang, Y.J.; Zhong, H.; Ao, C.C.; Li, J.; Han, J.G. An all-atom molecular dynamics study of the anti-interferon signaling of Ebola virus: Interaction mechanisms of EBOV VP24 binding to Karyopherin alpha5. Mol. Biosyst. 2017, 13, 1031–1045. [Google Scholar] [CrossRef]
- Lubaki, N.M.; Ilinykh, P.; Pietzsch, C.; Tigabu, B.; Freiberg, A.N.; Koup, R.A.; Bukreyev, A. The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J. Virol. 2013, 87, 7471–7485. [Google Scholar] [CrossRef]
- Takamatsu, Y.; Kolesnikova, L.; Schauflinger, M.; Noda, T.; Becker, S. The Integrity of the YxxL Motif of Ebola Virus VP24 Is Important for the Transport of Nucleocapsid-Like Structures and for the Regulation of Viral RNA Synthesis. J. Virol. 2020, 94, e02170-19. [Google Scholar] [CrossRef]
- He, F.B.; Khan, H.; Huttunen, M.; Kolehmainen, P.; Melen, K.; Maljanen, S.; Qu, M.; Jiang, M.; Kakkola, L.; Julkunen, I. Filovirus VP24 Proteins Differentially Regulate RIG-I and MDA5-Dependent Type I and III Interferon Promoter Activation. Front. Immunol. 2021, 12, 694105. [Google Scholar] [CrossRef]



| Vero-E6 Cells | 769-P Cells | |||
|---|---|---|---|---|
| Virus | No IFN-β Added | IFN-β Added | No IFN-β Added | IFN-β Added |
| N135A | 19.98 (6.5 ns) | 14.48 (5.1 ****) | 18.78 (6 ns) | 13.12 (4.2 ns) |
| R140A | 17.42 (6.2 *) | 11.32 (4.1 ****) | 14.18 (4.1 ****) | 8.9 (3.0 ****) |
| 135/140 | 18.83 (6.1 *) | 14.85 (5.0 ****) | 16.72 (5.6 ns) | 11.97 (3.4 ***) |
| 4 × A | 19.8 (6.4 ns) | 14.82 (5.1 ****) | 17.07 (5.7 ns) | 10.9 (3.2 ****) |
| 4× | 19.85 (6.3 ns) | 15.18 (5.1 ****) | 18.17 (5.6 ns) | 12.6 (3.9 ns) |
| WT | 21.68 (6.5) | 16.52 (5.7) | 19.12 (5.4) | 14.28 (4.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramanathan, P.; Tigabu, B.; Santos, R.I.; Ilinykh, P.A.; Kuzmina, N.; Vogel, O.A.; Thakur, N.; Ahmed, H.; Wu, C.; Amarasinghe, G.K.; et al. Ebolavirus Species-Specific Interferon Antagonism Mediated by VP24. Viruses 2023, 15, 1075. https://doi.org/10.3390/v15051075
Ramanathan P, Tigabu B, Santos RI, Ilinykh PA, Kuzmina N, Vogel OA, Thakur N, Ahmed H, Wu C, Amarasinghe GK, et al. Ebolavirus Species-Specific Interferon Antagonism Mediated by VP24. Viruses. 2023; 15(5):1075. https://doi.org/10.3390/v15051075
Chicago/Turabian StyleRamanathan, Palaniappan, Bersabeh Tigabu, Rodrigo I. Santos, Philipp A. Ilinykh, Natalia Kuzmina, Olivia A. Vogel, Naveen Thakur, Hamza Ahmed, Chao Wu, Gaya K. Amarasinghe, and et al. 2023. "Ebolavirus Species-Specific Interferon Antagonism Mediated by VP24" Viruses 15, no. 5: 1075. https://doi.org/10.3390/v15051075
APA StyleRamanathan, P., Tigabu, B., Santos, R. I., Ilinykh, P. A., Kuzmina, N., Vogel, O. A., Thakur, N., Ahmed, H., Wu, C., Amarasinghe, G. K., Basler, C. F., & Bukreyev, A. (2023). Ebolavirus Species-Specific Interferon Antagonism Mediated by VP24. Viruses, 15(5), 1075. https://doi.org/10.3390/v15051075







