Determinants of Vaccination and Willingness to Vaccinate against COVID-19 among Pregnant and Postpartum Women during the Third Wave of the Pandemic: A European Multinational Cross-Sectional Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Primary Outcome
2.4. Covariates
2.5. The Studied Determinants
2.6. Statistical Analyses
2.7. Sensitivity Analyses
2.7.1. Vaccination Willingness Alone in Pregnant Women
2.7.2. Vaccination Status or Willingness to Be Vaccinated in Breastfeeding Women
2.8. Ethical Approval
3. Results
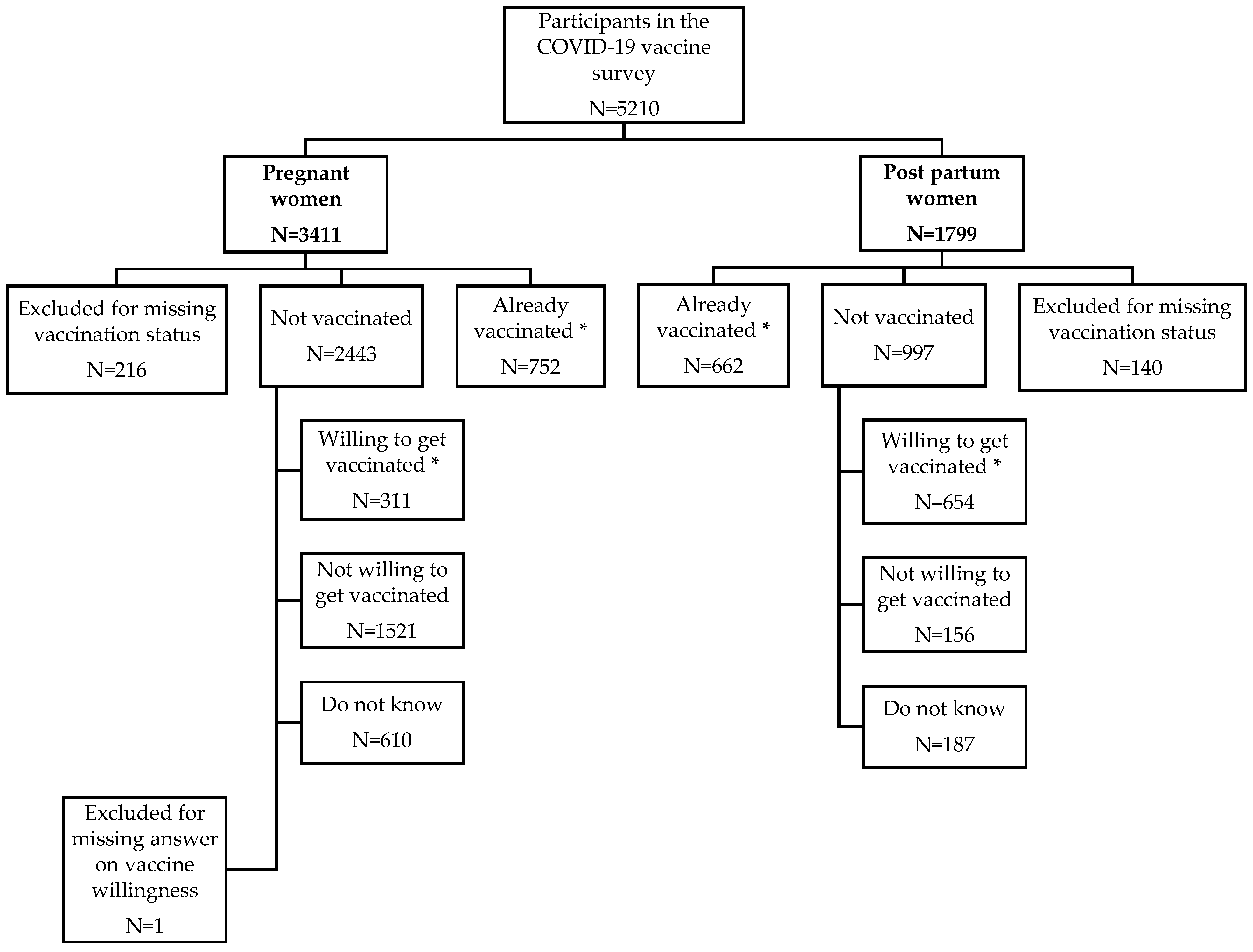
3.1. Participants
3.2. COVID-19 Vaccination Status and Vaccine Willingness
3.3. Determinants Associated with COVID-19 Vaccine Willingness
3.4. Sensitivity Analyses
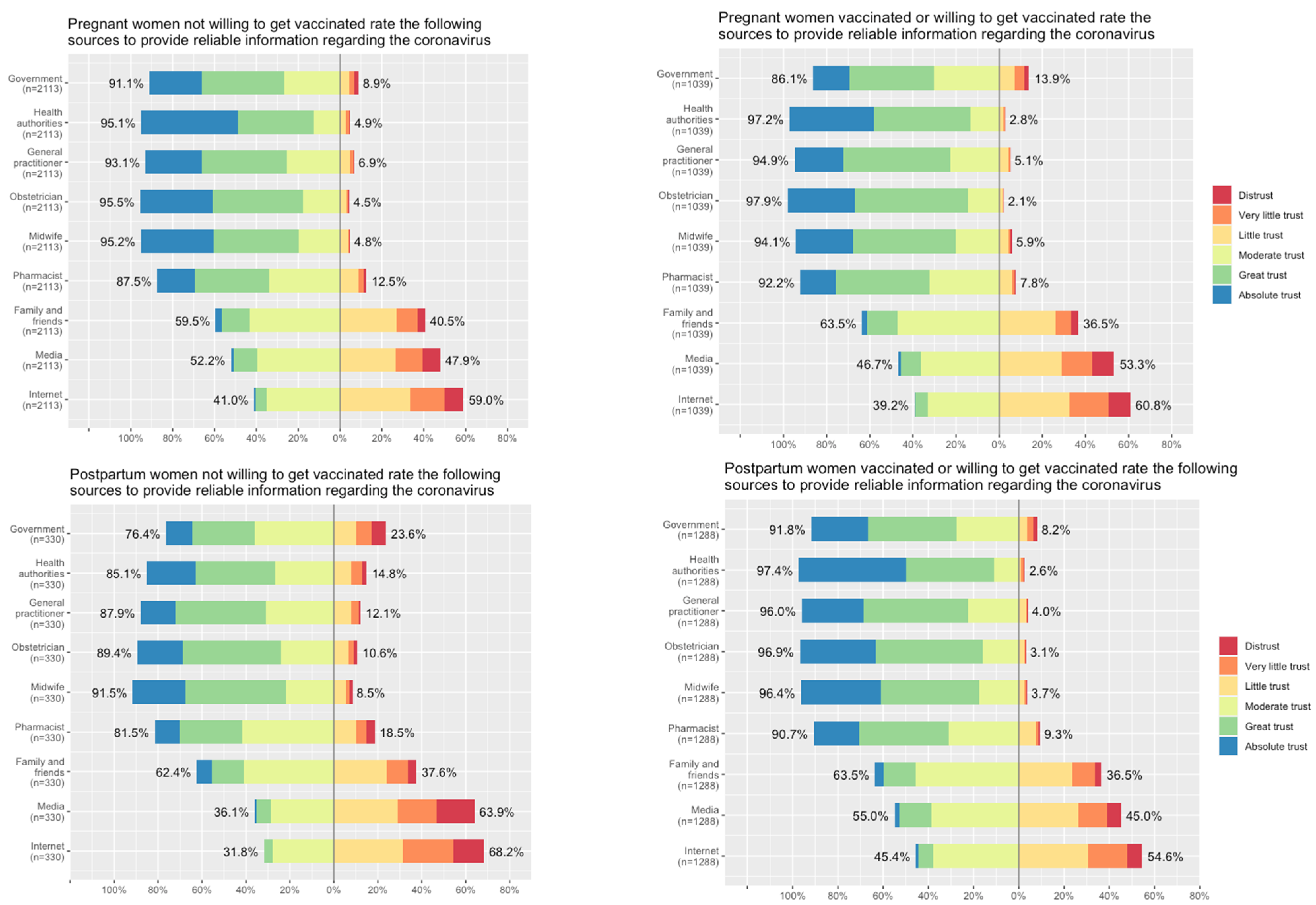
3.5. Women’s Beliefs about COVID-19 Infection, Measures to Prevent the Pandemic Spread and Their Trust in the Different Sources of Information regarding COVID-19
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Favre, G.; Maisonneuve, E.; Pomar, L.; Daire, C.; Poncelet, C.; Quibel, T.; Monod, C.; Martinez de Tejada, B.; Schaffer, L.; Papadia, A.; et al. Maternal and perinatal outcomes following pre-Delta, Delta, and Omicron SARS-CoV-2 variants infection among unvaccinated pregnant women in France and Switzerland: A prospective cohort study using the COVI-PREG registry. Lancet Reg. Health Eur. 2023, 26, 100569. [Google Scholar] [CrossRef]
- Smith, E.R.; Oakley, E.; Grandner, G.W.; Rukundo, G.; Farooq, F.; Ferguson, K.; Baumann, S.; Waldorf, K.M.A.; Afshar, Y.; Ahlberg, M.; et al. Clinical risk factors of adverse outcomes among women with COVID-19 in the pregnancy and postpartum period: A sequential, prospective meta-analysis. Am. J. Obstet. Gynecol. 2023, 228, 161–177. [Google Scholar] [CrossRef]
- Lassi, Z.S.; Ali, A.; Das, J.K.; Salam, R.A.; Padhani, Z.A.; Irfan, O.; Bhutta, Z.A. A systematic review and meta-analysis of data on pregnant women with confirmed COVID-19: Clinical presentation, and pregnancy and perinatal outcomes based on COVID-19 severity. J. Glob. Health 2021, 11, 05018. [Google Scholar] [CrossRef]
- Prasad, S.; Kalafat, E.; Blakeway, H.; Townsend, R.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; Le Doare, K.; Ladhani, S.; et al. Systematic review and meta-analysis of the effectiveness and perinatal outcomes of COVID-19 vaccination in pregnancy. Nat. Commun. 2022, 13, 2414. [Google Scholar] [CrossRef]
- Halasa, N.B.; Olson, S.M.; Staat, M.A.; Newhams, M.M.; Price, A.M.; Pannaraj, P.S.; Boom, J.A.; Sahni, L.C.; Chiotos, K.; Cameron, M.A.; et al. Maternal Vaccination and Risk of Hospitalization for COVID-19 among Infants. N. Engl. J. Med. 2022, 387, 109–119. [Google Scholar] [CrossRef]
- Low, J.M.; Gu, Y.; Ng, M.S.F.; Wang, L.W.; Amin, Z.; Zhong, Y.; MacAry, P.A. Human Milk Antibodies after BNT162b2 Vaccination Exhibit Reduced Binding against SARS-CoV-2 Variants of Concern. Vaccines 2022, 10, 225. [Google Scholar] [CrossRef] [PubMed]
- Shook, L.L.; Edlow, A.G. Safety and Efficacy of Coronavirus Disease 2019 (COVID-19) mRNA Vaccines During Lactation. Obstet. Gynecol. 2023, 141, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.P.; Stefanizzi, P.; Di Gioia, M.C.; Brescia, N.; Lattanzio, S.; Tafuri, S. COVID-19 vaccination hesitancy in pregnant and breastfeeding women and strategies to increase vaccination compliance: A systematic review and meta-analysis. Expert Rev. Vaccines 2022, 21, 1443–1454. [Google Scholar] [CrossRef] [PubMed]
- Shamshirsaz, A.A.; Hessami, K.; Morain, S.; Afshar, Y.; Nassr, A.A.; Arian, S.E.; Asl, N.M.; Aagaard, K. Intention to Receive COVID-19 Vaccine during Pregnancy: A Systematic Review and Meta-analysis. Am. J. Perinatol. 2022, 39, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Nindrea, R.D.; Djanas, D.; Warsiti; Darma, I.Y.; Hendriyani, H.; Sari, N.P. The risk factors and pregnant women’s willingness toward the SARS-CoV-2 vaccination in various countries: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2022, 14, 100982. [Google Scholar] [CrossRef] [PubMed]
- Azami, M.; Nasirkandy, M.P.; Esmaeili Gouvarchin Ghaleh, H.; Ranjbar, R. COVID-19 vaccine acceptance among pregnant women worldwide: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0272273. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, O.; Siddiquea, B.N.; Shetty, A.; Afroz, A.; Billah, B. COVID-19 vaccine hesitancy among pregnant women: A systematic review and meta-analysis. BMJ Open 2022, 12, e061477. [Google Scholar] [CrossRef] [PubMed]
- Badell, M.L.; Dude, C.M.; Rasmussen, S.A.; Jamieson, D.J. COVID-19 vaccination in pregnancy. BMJ 2022, 378, e069741. [Google Scholar] [CrossRef]
- Gerbier, E.; Favre, G.; Tauqeer, F.; Winterfeld, U.; Stojanov, M.; Oliver, A.; Passier, A.; Nordeng, H.; Pomar, L.; Baud, D.; et al. Self-Reported Medication Use among Pregnant and Postpartum Women during the Third Wave of the COVID-19 Pandemic: A European Multinational Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 5335. [Google Scholar] [CrossRef] [PubMed]
- Tauqeer, F.; Ceulemans, M.; Gerbier, E.; Passier, A.; Oliver, A.; Foulon, V.; Panchaud, A.; Lupattelli, A.; Nordeng, H. Mental health of pregnant and postpartum women during the third wave of the COVID-19 pandemic: A European cross-sectional study. BMJ Open 2023, 13, e063391. [Google Scholar] [CrossRef]
- Araya, R.A.; Tauqeer, F.; Ceulemans, M.; Gerbier, E.; Maisonneuve, E.; Passier, A.; Oliver, A.; Panchaud, A.; Lupattelli, A.; Nordeng, H. Pregnancy- and Birth-Related Experiences among Postpartum Women during the Third Wave of the COVID-19 Pandemic—A Multinational European Study. Pharmacoepidemiology 2023, 2, 54–67. [Google Scholar] [CrossRef]
- Ceulemans, M.; Foulon, V.; Panchaud, A.; Winterfeld, U.; Pomar, L.; Lambelet, V.; Cleary, B.; O’Shaughnessy, F.; Passier, A.; Richardson, J.L.; et al. Vaccine Willingness and Impact of the COVID-19 Pandemic on Women’s Perinatal Experiences and Practices-A Multinational, Cross-Sectional Study Covering the First Wave of the Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3367. [Google Scholar] [CrossRef]
- Ceulemans, M.; Foulon, V.; Ngo, E.; Panchaud, A.; Winterfeld, U.; Pomar, L.; Lambelet, V.; Cleary, B.; O’Shaughnessy, F.; Passier, A.; et al. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-A multinational cross-sectional study. Acta Obstet. Gynecol. Scand. 2021, 100, 1219–1229. [Google Scholar] [CrossRef]
- Superior Health Council Belgium. Recommendations for the Vaccination against SARS-CoV-2 with Messenger RNA Vaccines of Pregnant Women, Women Willing to Get Pregnant and Breastfeeding Women. 21 May 2021. Available online: https://www.health.belgium.be/sites/default/files/uploads/fields/fpshealth_theme_file/20210623_hgr-9622_vaccinatie_zwangere_en_lacterende_vrouwen_vweb.pdf (accessed on 18 April 2023).
- Norwegian Institute of Public Health. Advice and Information for Women Who Are Pregnant or Breastfeeding, Published 14 March 2020, Updated 25 March 2022. Available online: https://www.fhi.no/en/op/novel-coronavirus-facts-advice/facts-and-general-advice/advice-and-information-for-pregnant-women/#vaccination-of-pregnant-women (accessed on 18 April 2023).
- Federal Office of Public Health. Recommendations of Federal Office of Public Health on Coronavirus Vaccination in Pregnant Women. Available online: https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/impfen.html#-1430125092 (accessed on 18 April 2023).
- Government of The Netherlands; National Institute for Public Health and the Environment. Pregnancy and the COVID-19 Vaccine. Available online: https://www.government.nl/topics/coronavirus-covid-19/dutch-vaccination-programme/safety-and-development-of-vaccines (accessed on 18 April 2023).
- Royal College of Obstetricians and Gynecologists. COVID-19 Vaccines, Pregnancy and Breastfeeding. Available online: https://www.rcog.org.uk/guidance/coronavirus-covid-19-pregnancy-and-women-s-health/vaccination/covid-19-vaccines-pregnancy-and-breastfeeding-faqs/ (accessed on 18 April 2023).
- Our World in Data. COVID-19 Data Explorer. Available online: https://ourworldindata.org/covid-vaccinations?country=OWID_WRL (accessed on 18 April 2023).
- Ortqvist, A.K.; Dahlqwist, E.; Magnus, M.C.; Ljung, R.; Jonsson, J.; Aronsson, B.; Pasternak, B.; Haberg, S.E.; Stephansson, O. COVID-19 vaccination in pregnant women in Sweden and Norway. Vaccine 2022, 40, 4686–4692. [Google Scholar] [CrossRef]
- National Institute for Public Health and the Environment. Archief Wekelijkse Update Vaccinatiecijfers July 2021. Available online: https://www.rivm.nl/covid-19-vaccinatie/archief-wekelijkse-update-vaccinatiecijfers-2021 (accessed on 18 April 2023).
- Zhang, Z.; Murtagh, F.; Van Poucke, S.; Lin, S.; Lan, P. Hierarchical cluster analysis in clinical research with heterogeneous study population: Highlighting its visualization with R. Ann. Transl. Med. 2017, 5, 75. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Su, X.; Lu, H.; Li, X.; Luo, M.; Li, F.; Zhang, Q. COVID-19 vaccine hesitancy in periconceptional and lactating women: A systematic review and meta-analysis protocol. BMJ Open 2022, 12, e059514. [Google Scholar] [CrossRef] [PubMed]
- Schaal, N.K.; Zollkau, J.; Hepp, P.; Fehm, T.; Hagenbeck, C. Pregnant and breastfeeding women’s attitudes and fears regarding the COVID-19 vaccination. Arch. Gynecol. Obstet. 2022, 306, 365–372. [Google Scholar] [CrossRef]
- Fajar, J.K.; Sallam, M.; Soegiarto, G.; Sugiri, Y.J.; Anshory, M.; Wulandari, L.; Kosasih, S.A.P.; Ilmawan, M.; Kusnaeni, K.; Fikri, M.; et al. Global Prevalence and Potential Influencing Factors of COVID-19 Vaccination Hesitancy: A Meta-Analysis. Vaccines 2022, 10, 1356. [Google Scholar] [CrossRef] [PubMed]
- Egloff, C.; Couffignal, C.; Cordier, A.G.; Deruelle, P.; Sibiude, J.; Anselem, O.; Benachi, A.; Luton, D.; Mandelbrot, L.; Vauloup-Fellous, C.; et al. Pregnant women’s perceptions of the COVID-19 vaccine: A French survey. PLoS ONE 2022, 17, e0263512. [Google Scholar] [CrossRef] [PubMed]
- Marban-Castro, E.; Nedic, I.; Ferrari, M.; Crespo-Mirasol, E.; Ferrer, L.; Noya, B.; Marin, A.; Fumado, V.; Lopez, M.; Menendez, C.; et al. Perceptions of COVID-19 Maternal Vaccination among Pregnant Women and Healthcare Workers and Factors That Influence Vaccine Acceptance: A Cross-Sectional Study in Barcelona, Spain. Vaccines 2022, 10, 1930. [Google Scholar] [CrossRef]
- Mannocci, A.; Scaglione, C.; Casella, G.; Lanzone, A.; La Torre, G. COVID-19 in Pregnancy: Knowledge about the Vaccine and the Effect of the Virus. Reliability and Results of the MAMA-19 Questionnaire. Int. J. Environ. Res. Public Health 2022, 19, 14886. [Google Scholar] [CrossRef]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarethsson, V.O.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef]
- Roghani, A. The relationship between macro-socioeconomics determinants and COVID-19 vaccine distribution. AIMS Public Health 2021, 8, 655–664. [Google Scholar] [CrossRef]
- Kirbiš, A. The Impact of Socioeconomic Status, Perceived Threat and Healthism on Vaccine Hesitancy. Sustainability 2023, 15, 6107. [Google Scholar] [CrossRef]
- Villar, J.; Soto Conti, C.P.; Gunier, R.B.; Ariff, S.; Craik, R.; Cavoretto, P.I.; Rauch, S.; Gandino, S.; Nieto, R.; Winsey, A.; et al. Pregnancy outcomes and vaccine effectiveness during the period of omicron as the variant of concern, INTERCOVID-2022: A multinational, observational study. Lancet 2023, 401, 447–457. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Pregnant Women N = 3194 N (%) | Postpartum Women N = 1659 N (%) | |
|---|---|---|---|
| Country | Belgium | 298 (9.3) | 196 (11.8) |
| Norway | 2376 (74.4) | 1113 (67.1) | |
| Switzerland | 165 (5.2) | 140 (8.4) | |
| The Netherlands | 123 (3.9) | 124 (7.5) | |
| United Kingdom | 232 (7.3) | 86 (5.2) | |
| Maternal age (years) | 18–25 | 224 (7.0) | 94 (5.7) |
| 26–30 | 1150 (36.0) | 581 (35.0) | |
| 31–35 | 1301 (40.7) | 684 (41.2) | |
| 36–40 | 406 (12.7) | 213 (12.8) | |
| >40 | 68 (2.1) | 44 (2.7) | |
| Missing data | 45 (1.4) | 183 (2.6) | |
| Relationship status | Partner | 3092 (96.8) | 1595 (96.1) |
| No partner | 57 (1.8) | 21 (1.3) | |
| Missing data | 45 (1.4) | 43 (2.6) | |
| Professional status * | Inactive | 348 (10.9) | 176 (9.8) |
| Active | 2799 (87.6) | 1430 (79.5) | |
| Missing data | 47 (1.5) | 53 (3.2) | |
| Working in healthcare | No | 1879 (58.8) | 947 (57.1) |
| Yes | 906 (28.8) | 486 (29.3) | |
| Missing data | 409 (12.8) | 226 (13.6) | |
| Educational Level ** | Low | 73 (2.3) | 34 (2.0) |
| Medium | 540 (16.9) | 290 (17.5) | |
| High | 2516 (78.7) | 1279 (77.1) | |
| Missing data | 65 (2.0) | 56 (3.4) | |
| Smoking during pregnancy *** | Yes | 43 (1.3) | 19 (1.1) |
| No | 3106 (97.2) | 1597 (88.8) | |
| Missing data | 45 (1.4) | 43 (2.6) | |
| History of positive SARS-CoV-2 test | Yes | 142 (4.4) | 83 (5.0) |
| No | 3051 (95.5) | 1576 (95.0) | |
| Missing data | 1 (0.0) | 0 (0.0) | |
| Chronic illness requiring medication | Yes | 1174 (36.8) | 470 (26.1) |
| No | 1416 (44.3) | 790 (43.9) | |
| Missing data | 604 (18.9) | 399 (24.1) | |
| Gravidity | Primigravida | 1607 (50.3) | NA |
| Multigravida | 1587 (49.7) | NA | |
| Gestational trimester | 1st trimester | 351 (11.0) | NA |
| 2nd trimester | 1102 (34.5) | NA | |
| 3rd trimester | 1741 (54.5) | NA | |
| Breastfeeding at the time of survey completion | Yes | NA | 1523 (91.8) |
| No | NA | 136 (8.2) | |
| Participated in the COVID-19 survey in 2020 # | Yes | 47 (1.5) | 18 (1.1) |
| No | 3032 (94.9) | 1574 (94.9) | |
| Can’t remember | 105 (3.3) | 67 (4.0) |
| Country | Total N (%) | Belgium N (%) | Norway N (%) | Switzerland N (%) | The Netherlands N (%) | United Kingdom N (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Status | Pregnancy | Postpartum | Pregnancy | Postpartum | Pregnancy | Postpartum | Pregnancy | Postpartum | Pregnancy | Postpartum | Pregnancy | Postpartum |
| Already vaccinated against COVID-19 | ||||||||||||
| Yes | 752 (23.5) | 662 (39.9) | 216 (72.5) | 112 (57.1) | 268 (11.3) | 365 (32.8) | 37 (22.4) | 56 (40.0) | 59 (48.0) | 62 (50.0) | 172 (74.1) | 67 (77.9) |
| No | 2442 (76.5) | 997 (60.1) | 82 (27.5) | 84 (42.9) | 2108 (88.7) | 748 (67.2) | 128 (77.6) | 84 (60.0) | 64 (52.0) | 62 (50.0) | 60 (25.9) | 19 (22.1) |
| Unvaccinated women who would be vaccinated against COVID-19 if they had had the opportunity | ||||||||||||
| Yes | 311 (12.7) | 654 (65.6) | 24 (29.3) | 56 (71.8) | 242 (11.5) | 537 (71.8) | 16 (12.5) | 26 (31.0) | 18 (28.1) | 28 (45.2) | 11 (18.3) | 7 (36.8) |
| No | 1521 (62.3) | 156 (15.6) | 42 (51.2) | 11 (11.5) | 1326 (62.9) | 86 (11.5) | 82 (64.1) | 40 (47.6) | 36 (56.2) | 15 (24.2) | 35 (58.3) | 4 (21.1) |
| Do not know | 610 (25.0) | 187 (18.8) | 16 (19.5) | 17 (20.2) | 540 (25.6) | 125 (16.7) | 30 (23.4) | 18 (21.4) | 10 (15.6) | 19 (30.6) | 14 (23.3) | 8 (42.1) |
| Composite variable: “already vaccinated or willing to get vaccinated against COVID-19” | ||||||||||||
| Yes | 1063 (33.3) | 1316 (79.3) | 240 (80.5) | 168 (85.7) | 510 (21.5) | 902 (81.0) | 53 (32.1) | 82 (58.6) | 77 (62.6) | 90 (72.6) | 183 (78.9) | 74 (86.0) |
| No | 2131 (66.7) | 343 (20.7) | 58 (19.5) | 28 (14.3) | 1866 (78.5) | 211 (19.0) | 112 (67.9) | 58 (41.4) | 46 (37.4) | 34 (27.4) | 49 (21.1) | 12 (14.0) |
| Pregnant Women | Postpartum Women | |||||
|---|---|---|---|---|---|---|
| All N (%) | 1st Trimester N (%) | 2nd Trimester N (%) | 3rd Trimester N (%) | Breastfeeding N (%) | No Breastfeeding N (%) | |
| “Please indicate why you believe COVID-19 vaccines are not (entirely) safe during pregnancy, breastfeeding or postpartum. You can indicate multiple reasons.” * | ||||||
| “I believe that the long-term effects of these vaccines are not known yet” | 1908/1958 (97.4) | 202/208 (97.1) | 653/69 (97.6) | 1053/1081 (97.4) | 651/726 (89.7) | 61/189 (32.3) |
| “I believe that some steps of the usual process of vaccine development and approval were not fully completed or bypassed” | 917/1030 (89.0) | 87/99 (87.9) | 328/369 (88.9) | 502/562 (89.3) | 313/417 (75.1) | 36/171 (21.0) |
| “I believe that it bears a potential risk for my unborn child’s growth and development” | 761/872 (87.2) | 105/118 (89) | 302/343 (88) | 354/411 (86.1) | NA | NA |
| “I believe that it bears a potential risk of malformation for my unborn” | 548/671 (81.7) | 79/91 (86.8) | 221/268 (82.5) | 248/312 (79.5) | NA | NA |
| “I believe that it bears potential risks for my own health” | 431/552 (78.1) | 54/65 (83.1) | 151/201 (75.1) | 226/286 (79) | 216/327 (66.1) | 22/161 (13.7) |
| “I believe that it could lead to a miscarriage or stillbirth” | 470/608 (77.3) | 80/194 (85.1) | 212/265 (80) | 178/249 (71.5) | NA | NA |
| “Other reason” | 399/551 (72.4) | 39/55 (70.9) | 136/204 (66.7) | 224/292 (76.7) | 70/205 (34.2) | 6/144 (4.2) |
| “I believe that other non-medical treatments for COVID-19 may be safer” | 305/464 (65.7) | 26/42 (61.9) | 97/164 (59.1) | 182/258 (70.5) | 37/174 (21.3) | 3/143 (2.1) |
| “I believe that it could negatively affect my fertility” | 235/388 (60.6) | 36/50 (72) | 88/155 (56.8) | 111/183 (60.7) | 104/230 (45.2) | 10/147 (6.8) |
| “I believe that it could cause DNA alterations” | 229/381 (60.1) | 35/50 (70) | 92/154 (59.7) | 102/177 (57.6) | 72/203 (35.5) | 6/145 (4.1) |
| “I believe that other medical treatments for COVID-19 may be safer” | 184/341 (54.0) | 18/35 (51.4) | 64/130 (49.2) | 102/176 (58) | 26/163 (16.0) | 4/144 (2.8) |
| “I could catch (/transmit) the disease through the vaccine” | 54/214 (25.2) | 105/118 (89) | 302/343 (88) | 354/411 (86.1) | 24/156 (15.4) | 5/144 (3.5) |
| “I generally do not believe vaccines are safe” | 29/190 (15.3) | 4/21 (19) | 13/82 (15.9) | 12/87 (13.8) | 17/153 (11.1) | 11/142 (7.7) |
| “I believe that it bears potential risks for my nursing infant” | NA | NA | NA | NA | 273/372 (73.4) | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maisonneuve, E.; Gerbier, E.; Tauqeer, F.; Pomar, L.; Favre, G.; Winterfeld, U.; Passier, A.; Oliver, A.; Baud, D.; Nordeng, H.; et al. Determinants of Vaccination and Willingness to Vaccinate against COVID-19 among Pregnant and Postpartum Women during the Third Wave of the Pandemic: A European Multinational Cross-Sectional Survey. Viruses 2023, 15, 1090. https://doi.org/10.3390/v15051090
Maisonneuve E, Gerbier E, Tauqeer F, Pomar L, Favre G, Winterfeld U, Passier A, Oliver A, Baud D, Nordeng H, et al. Determinants of Vaccination and Willingness to Vaccinate against COVID-19 among Pregnant and Postpartum Women during the Third Wave of the Pandemic: A European Multinational Cross-Sectional Survey. Viruses. 2023; 15(5):1090. https://doi.org/10.3390/v15051090
Chicago/Turabian StyleMaisonneuve, Emeline, Eva Gerbier, Fatima Tauqeer, Léo Pomar, Guillaume Favre, Ursula Winterfeld, Anneke Passier, Alison Oliver, David Baud, Hedvig Nordeng, and et al. 2023. "Determinants of Vaccination and Willingness to Vaccinate against COVID-19 among Pregnant and Postpartum Women during the Third Wave of the Pandemic: A European Multinational Cross-Sectional Survey" Viruses 15, no. 5: 1090. https://doi.org/10.3390/v15051090
APA StyleMaisonneuve, E., Gerbier, E., Tauqeer, F., Pomar, L., Favre, G., Winterfeld, U., Passier, A., Oliver, A., Baud, D., Nordeng, H., Ceulemans, M., & Panchaud, A. (2023). Determinants of Vaccination and Willingness to Vaccinate against COVID-19 among Pregnant and Postpartum Women during the Third Wave of the Pandemic: A European Multinational Cross-Sectional Survey. Viruses, 15(5), 1090. https://doi.org/10.3390/v15051090








