Rendezvous with Vaccinia Virus in the Post-smallpox Era: R&D Advances
Abstract
:1. Introduction
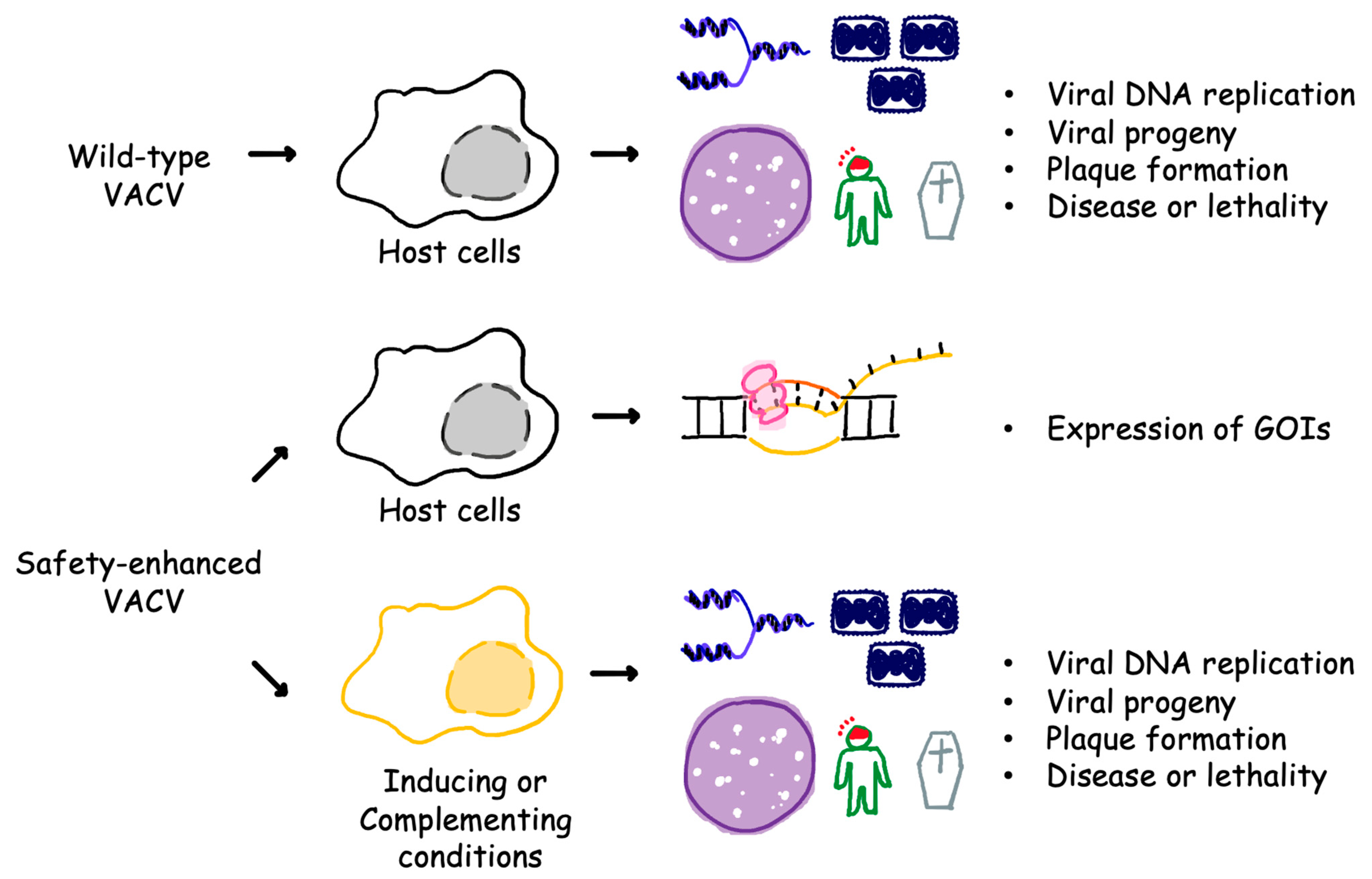
2. Enhanced Safety Mechanisms
3. Rapid Generation and Purification of Recombinant VACV
4. Modification in Viral Immunomodulatory Genes
5. Other Aspects of Innovation
6. Future Perspectives
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fenner, F.; Henderson, D.A.; Arita, I.; Ježek, Z.; Ladnyi, I.D. Smallpox and Its Eradication; World Health Organization: Geneva, Switzerland, 1988. Available online: https://apps.who.int/iris/handle/10665/39485 (accessed on 8 October 2022).
- Wehrle, P.F. A reality in our time—Certification of the global eradication of smallpox. J. Infect. Dis. 1980, 142, 636–638. [Google Scholar] [CrossRef] [PubMed]
- Esparza, J.; Lederman, S.; Nitsche, A.; Damaso, C.R. Early smallpox vaccine manufacturing in the United States: Introduction of the “animal vaccine” in 1870, establishment of “vaccine farms”, and the beginnings of the vaccine industry. Vaccine 2020, 38, 4773. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.M.; Ruben, F.L.; Neff, J.M.; Millar, J.D. Complications of smallpox vaccination, 1968: Results of ten statewide surveys. J. Infect. Dis. 1970, 122, 303–309. [Google Scholar] [CrossRef]
- Lane, J.M.; Goldstein, J. Evaluation of 21st-century risks of smallpox vaccination and policy options. Ann. Intern. Med. 2003, 138, 488–493. [Google Scholar] [CrossRef] [Green Version]
- Kemper, A.R.; Davis, M.M.; Freed, G.L. Expected adverse events in a mass smallpox vaccination campaign. Eff. Clin. Pract. 2002, 5, 84–90. [Google Scholar]
- Weltzin, R.; Liu, J.; Pugachev, K.V.; Myers, G.A.; Coughlin, B.; Blum, P.S.; Nichols, R.; Johnson, C.; Cruz, J.; Kennedy, J.S.; et al. Clonal vaccinia virus grown in cell culture as a new smallpox vaccine. Nat. Med. 2003, 9, 1125–1130. [Google Scholar] [CrossRef]
- Monath, T.P.; Caldwell, J.R.; Mundt, W.; Fusco, J.; Johnson, C.S.; Buller, M.; Liu, J.; Gardner, B.; Downing, G.; Blum, P.S.; et al. ACAM2000 clonal Vero cell culture vaccinia virus (New York City Board of Health strain)—A second-generation smallpox vaccine for biological defense. Int. J. Infect. Dis. 2004, 8 (Suppl. S2), 31–44. [Google Scholar] [CrossRef] [Green Version]
- Frey, S.E.; Newman, F.K.; Kennedy, J.S.; Ennis, F.; Abate, G.; Hoft, D.F.; Monath, T.P. Comparison of the safety and immunogenicity of ACAM1000, ACAM2000 and Dryvax in healthy vaccinia-naive adults. Vaccine 2009, 27, 1637–1644. [Google Scholar] [CrossRef]
- Greenberg, R.N.; Kennedy, J.S. ACAM2000: A newly licensed cell culture-based live vaccinia smallpox vaccine. Expert. Opin. Investig. Drugs 2008, 17, 555–564. [Google Scholar] [CrossRef]
- Stittelaar, K.J.; Amerongen, G.; van Kondova, I.; Kuiken, T.; Lavieren, R.F.; van Pistoor, F.H.M.; Niesters, H.G.M.; van Doornum, G.; van der Zeijst, B.A.M.; Mateo, L.; et al. Modified Vaccinia Virus Ankara Protects Macaques against Respiratory Challenge with Monkeypox Virus. J. Virol. 2005, 79, 7845. [Google Scholar] [CrossRef] [Green Version]
- Greenberg, R.N.; Kennedy, J.S.; Clanton, D.J.; Plummer, E.A.; Hague, L.; Cruz, J.; Ennis, F.A.; Blackwelder, W.C.; Hopkins, R.J. Safety and immunogenicity of new cell-cultured smallpox vaccine compared with calf-lymph derived vaccine: A blind, single-centre, randomised controlled trial. Lancet 2005, 365, 398–409. [Google Scholar] [CrossRef] [PubMed]
- von Krempelhuber, A.; Vollmar, J.; Pokorny, R.; Rapp, P.; Wulff, N.; Petzold, B.; Handley, A.; Mateo, L.; Siersbol, H.; Kollaritsch, H.; et al. A randomized, double-blind, dose-finding Phase II study to evaluate immunogenicity and safety of the third generation smallpox vaccine candidate IMVAMUNE. Vaccine 2010, 28, 1209–1216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vollmar, J.; Arndtz, N.; Eckl, K.M.; Thomsen, T.; Petzold, B.; Mateo, L.; Schlereth, B.; Handley, A.; King, L.; Hülsemann, V.; et al. Safety and immunogenicity of IMVAMUNE, a promising candidate as a third generation smallpox vaccine. Vaccine 2006, 24, 2065–2070. [Google Scholar] [CrossRef] [PubMed]
- Drexler, I.; Heller, K.; Wahren, B.; Erfle, V.; Sutter, G. Highly attenuated modified vaccinia virus Ankara replicates in baby hamster kidney cells, a potential host for virus propagation, but not in various human transformed and primary cells. J. Gen. Virol. 1998, 79 Pt 2, 347–352. [Google Scholar] [CrossRef]
- Mayr, A.; Stickl, H.; Müller, H.K.; Danner, K.; Singer, H. The smallpox vaccination strain MVA: Marker, genetic structure, experience gained with the parenteral vaccination and behavior in organisms with a debilitated defence mechanism (author’s transl). Zentralbl. Bakteriol. B 1978, 167, 375–390. [Google Scholar] [PubMed]
- Midgley, C.M.; Putz, M.M.; Weber, J.N.; Smith, G.L. Vaccinia virus strain NYVAC induces substantially lower and qualitatively different human antibody responses compared with strains Lister and Dryvax. J. Gen. Virol. 2008, 89 Pt 12, 2992–2997. [Google Scholar] [CrossRef]
- Paoletti, E.; Tartaglia, J.; Taylor, J. Safe and effective poxvirus vectors—NYVAC and ALVAC. Dev. Biol. Stand. 1994, 82, 65–69. [Google Scholar]
- Tartaglia, J.; Perkus, M.E.; Taylor, J.; Norton, E.K.; Audonnet, J.C.; Cox, W.I.; Davis, S.W.; Van Der Hoeven, J.; Meignier, B.; Riviere, M.; et al. NYVAC: A highly attenuated strain of vaccinia virus. Virology 1992, 188, 217–232. [Google Scholar] [CrossRef]
- Johnson, B.F.; Kanatani, Y.; Fujii, T.; Saito, T.; Yokote, H.; Smith, G.L. Serological responses in humans to the smallpox vaccine LC16m8. J. Gen. Virol. 2011, 92 Pt 10, 2405. [Google Scholar] [CrossRef]
- Kenner, J.; Cameron, F.; Empig, C.; Jobes, D.V.; Gurwith, M. LC16m8: An attenuated smallpox vaccine. Vaccine 2006, 24, 7009. [Google Scholar] [CrossRef]
- Takahashi-Nishimaki, F.; Funahashi, S.I.; Miki, K.; Hashizume, S.; Sugimoto, M. Regulation of plaque size and host range by a vaccinia virus gene related to complement system proteins. Virology 1991, 181, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J.S.; Gurwith, M.; Dekker, C.L.; Frey, S.E.; Edwards, K.M.; Kenner, J.; Lock, M.; Empig, C.; Morikawa, S.; Saijo, M.; et al. Safety and Immunogenicity of LC16m8, an Attenuated Smallpox Vaccine in Vaccinia-Naive Adults. J. Infect. Dis. 2011, 204, 1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saito, T.; Fujii, T.; Kanatani, Y.; Saijo, M.; Morikawa, S.; Yokote, H.; Takeuchi, T.; Kuwabara, N. Clinical and Immunological Response to Attenuated Tissue-Cultured Smallpox Vaccine LC16m8. JAMA 2009, 301, 1025–1033. [Google Scholar] [CrossRef] [Green Version]
- Hirao, L.A.; Draghia-Akli, R.; Prigge, J.T.; Yang, M.; Satishchandran, A.; Wu, L.; Hammarlund, E.; Khan, A.S.; Babas, T.; Rhodes, L.; et al. Multivalent Smallpox DNA Vaccine Delivered by Intradermal Electroporation Drives Protective Immunity in Nonhuman Primates Against Lethal Monkeypox Challenge. J. Infect. Dis. 2011, 203, 95. [Google Scholar] [CrossRef] [Green Version]
- Pulford, D.J.; Gates, A.; Bridge, S.H.; Robinson, J.H.; Ulaeto, D. Differential efficacy of vaccinia virus envelope proteins administered by DNA immunisation in protection of BALB/c mice from a lethal intranasal poxvirus challenge. Vaccine 2004, 22, 3358–3366. [Google Scholar] [CrossRef]
- Sakhatskyy, P.; Wang, S.; Zhang, C.; Chou, T.H.; Kishko, M.; Lu, S. Immunogenicity and Protection Efficacy of Subunit-based Smallpox Vaccines Using Variola Major Antigens. Virology 2008, 371, 98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hooper, J.W.; Custer, D.M.; Thompson, E. Four-gene-combination DNA vaccine protects mice against a lethal vaccinia virus challenge and elicits appropriate antibody responses in nonhuman primates. Virology 2003, 306, 181–195. [Google Scholar] [CrossRef]
- Buchman, G.W.; Cohen, M.E.; Xiao, Y.; Richardson-Harman, N.; Silvera, P.; DeTolla, L.J.; Davis, H.L.; Eisenberg, R.J.; Cohen, G.H.; Isaacs, S.N. A protein-based smallpox vaccine protects non-human primates from a lethal monkeypox virus challenge. Vaccine 2010, 28, 6627. [Google Scholar] [CrossRef] [Green Version]
- Davies, D.H.; McCausland, M.M.; Valdez, C.; Huynh, D.; Hernandez, J.E.; Mu, Y.; Hirst, S.; Villarreal, L.; Felgner, P.L.; Crotty, S. Vaccinia virus H3L envelope protein is a major target of neutralizing antibodies in humans and elicits protection against lethal challenge in mice. J. Virol. 2005, 79, 11724–11733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogg, C.; Lustig, S.; Whitbeck, J.C.; Eisenberg, R.J.; Cohen, G.H.; Moss, B. Protective immunity to vaccinia virus induced by vaccination with multiple recombinant outer membrane proteins of intracellular and extracellular virions. J. Virol. 2004, 78, 10230–10237. [Google Scholar] [CrossRef] [Green Version]
- Moise, L.; Buller, R.M.; Schriewer, J.; Lee, J.; Frey, S.E.; Weiner, D.B.; Martin, W.; De Groot, A.S. VennVax, a DNA-prime, peptide-boost multi-T-cell epitope poxvirus vaccine, induces protective immunity against vaccinia infection by T cell response alone. Vaccine 2011, 29, 501–511. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verardi, P.H.; Titong, A.; Hagen, C.J. A vaccinia virus renaissance: New vaccine and immunotherapeutic uses after smallpox eradication. Hum. Vaccin. Immunother. 2012, 8, 961–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. 2022 Outbreak Cases and Data|Mpox|Poxvirus. Available online: https://www.cdc.gov/poxvirus/mpox/response/2022/index.html (accessed on 22 March 2023).
- Liu, B.; Panda, D.; Mendez-Rios, J.D.; Ganesan, S.; Wyatt, L.S.; Moss, B. Identification of Poxvirus Genome Uncoating and DNA Replication Factors with Mutually Redundant Roles. J. Virol. 2018, 92, 2152–2169. [Google Scholar] [CrossRef] [Green Version]
- O’Connell, C.M.; Jasperse, B.; Hagen, C.J.; Titong, A.; Verardi, P.H. Replication-inducible vaccinia virus vectors with enhanced safety in vivo. PLoS ONE 2020, 15, e0230711. [Google Scholar] [CrossRef] [PubMed]
- Hillen, W.; Berens, C. Mechanisms underlying expression of Tn10 encoded tetracycline resistance. Annu. Rev. Microbiol. 1994, 48, 345–369. [Google Scholar] [CrossRef]
- Zhu, Z.; Zheng, T.; Lee, C.G.; Homer, R.J.; Elias, J.A. Tetracycline-controlled transcriptional regulation systems: Advances and application in transgenic animal modeling. Semin. Cell Dev. Biol. 2002, 13, 121–128. [Google Scholar] [CrossRef]
- Yao, F.; Svensjö, T.; Winkler, T.; Lu, M.; Eriksson, C.; Eriksson, E. Tetracycline repressor, tetR, rather than the tetR-mammalian cell transcription factor fusion derivatives, regulates inducible gene expression in mammalian cells. Hum. Gene Ther. 1998, 9, 1939–1950. [Google Scholar] [CrossRef]
- Stieger, K.; Belbellaa, B.; le Guiner, C.; Moullier, P.; Rolling, F. In vivo gene regulation using tetracycline-regulatable systems. Adv. Drug Deliv. Rev. 2009, 61, 527–541. [Google Scholar] [CrossRef]
- Stebbins, M.J.; Urlinger, S.; Byrne, G.; Bello, B.; Hillen, W.; Yin, J.C.P. Tetracycline-inducible systems for Drosophila. Proc. Natl. Acad. Sci. USA 2001, 98, 10775–10780. [Google Scholar] [CrossRef]
- Gatz, C.; Quail, P.H. Tn10-encoded tet repressor can regulate an operator-containing plant promoter. Proc. Natl. Acad. Sci. USA 1988, 85, 1394–1397. [Google Scholar] [CrossRef]
- Faryar, K.; Gatz, C. Construction of a tetracycline-inducible promoter in Schizosaccharomyces pombe. Curr. Genet. 1992, 21, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Bertram, R.; Hillen, W. The application of Tet repressor in prokaryotic gene regulation and expression. Microb. Biotechnol. 2008, 1, 2–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tolonen, N.; Doglio, L.; Schleich, S.; Krijnse Locker, J. Vaccinia virus DNA replication occurs in endoplasmic reticulum-enclosed cytoplasmic mini-nuclei. Mol. Biol. Cell 2001, 12, 2031–2046. [Google Scholar] [CrossRef] [Green Version]
- Doglio, L.; de Marco, A.; Schleich, S.; Roos, N.; Krijnse Locker, J. The Vaccinia virus E8R gene product: A viral membrane protein that is made early in infection and packaged into the virions’ core. J. Virol. 2002, 76, 9773–9786. [Google Scholar] [CrossRef] [Green Version]
- Kato, S.E.M.; Condit, R.C.; Moussatché, N. The vaccinia virus E8R gene product is required for formation of transcriptionally active virions. Virology 2007, 367, 398–412. [Google Scholar] [CrossRef] [Green Version]
- Kato, S.E.M.; Strahl, A.L.; Moussatche, N.; Condit, R.C. Temperature-sensitive mutants in the vaccinia virus 4b virion structural protein assemble malformed, transcriptionally inactive intracellular mature virions. Virology 2004, 330, 127–146. [Google Scholar] [CrossRef] [Green Version]
- Moss, B. Poxvirus membrane biogenesis. Virology 2015, 479–480, 619–626. [Google Scholar] [CrossRef]
- Jasperse, B.; O’Connell, C.M.; Wang, Y.; Verardi, P.H. Single dose of a replication-defective vaccinia virus expressing Zika virus-like particles is protective in mice. Sci. Rep. 2021, 11, 6492. [Google Scholar] [CrossRef]
- Wyatt, L.S.; Xiao, W.; Americo, J.L.; Earl, P.L.; Moss, B. Novel Nonreplicating Vaccinia Virus Vector Enhances Expression of Heterologous Genes and Suppresses Synthesis of Endogenous Viral Proteins. MBio 2017, 8, e00790-17. [Google Scholar] [CrossRef] [Green Version]
- Sanz, P.; Moss, B. Identification of a transcription factor, encoded by two vaccinia virus early genes, that regulates the intermediate stage of viral gene expression. Proc. Natl. Acad. Sci. USA 1999, 96, 2692. [Google Scholar] [CrossRef]
- Warren, R.D.; Cotter, C.A.; Moss, B. Reverse Genetics Analysis of Poxvirus Intermediate Transcription Factors. J. Virol. 2012, 86, 9514. [Google Scholar] [PubMed] [Green Version]
- Eldi, P.; Cooper, T.H.; Liu, L.; Prow, N.A.; Diener, K.R.; Howley, P.M.; Suhrbier, A.; Hayball, J.D. Production of a Chikungunya Vaccine Using a CHO Cell and Attenuated Viral-Based Platform Technology. Mol. Ther. 2017, 25, 2332–2344. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Cooper, T.; Howley, P.M.; Hayball, J.D. From crescent to mature virion: Vaccinia virus assembly and maturation. Viruses 2014, 6, 3787–3808. [Google Scholar] [PubMed] [Green Version]
- Zhang, Y.; Moss, B. Immature viral envelope formation is interrupted at the same stage by lac operator-mediated repression of the vaccinia virus D13L gene and by the drug rifampicin. Virology 1992, 187, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, J.C.; Chao, C.C.; Young, M.J.; Chang, Y.T.; Cho, E.C.; Chang, W. A poxvirus host range protein, CP77, binds to a cellular protein, HMG20A, and regulates its dissociation from the vaccinia virus genome in CHO-K1 cells. J. Virol. 2006, 80, 7714–7728. [Google Scholar]
- Wyatt, L.S.; Earl, P.L.; Moss, B. Generation of Recombinant Vaccinia Viruses. Curr. Protoc. Protein Sci. 2017, 89, 5.13.1–5.13.18. [Google Scholar]
- Falkner, F.G.; Moss, B. Transient dominant selection of recombinant vaccinia viruses. J. Virol. 1990, 64, 3108–3111. [Google Scholar] [CrossRef]
- Siciliano, N.A.; Huang, L.; Eisenlohr, L.C. Recombinant poxviruses: Versatile tools for immunological assays. Methods Mol. Biol. 2013, 960, 219–245. [Google Scholar]
- Cao, J.; Layne, C.; Varga, J.; Deschambault, Y. Application of poxvirus K3 ortholog as a positive selection marker for constructing recombinant vaccinia viruses with modified host range. MethodsX 2020, 7, 100918. [Google Scholar] [CrossRef]
- Jasperse, B.; O’Connell, C.M.; Wang, Y.; Verardi, P.H. EPPIC (Efficient Purification by Parental Inducer Constraint) Platform for Rapid Generation of Recombinant Vaccinia Viruses. Mol. Ther. Methods Clin. Dev. 2020, 17, 731–738. [Google Scholar] [CrossRef]
- White, S.D.; Conwell, K.; Langland, J.O.; Jacobs, B.L. Use of a negative selectable marker for rapid selection of recombinant vaccinia virus. Biotechniques 2011, 50, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ung, T.L.; Cao, C.; Lu, J.; Ozato, K.; Dever, T.E. Heterologous dimerization domains functionally substitute for the double-stranded RNA binding domains of the kinase PKR. EMBO J. 2001, 20, 3728–3737. [Google Scholar] [CrossRef] [Green Version]
- Sternberg, N.; Hamilton, D. Bacteriophage P1 site-specific recombination. I. Recombination between loxP sites. J. Mol. Biol. 1981, 150, 467–486. [Google Scholar] [CrossRef]
- Sauer, B.; Henderson, N. Site-specific DNA recombination in mammalian cells by the Cre recombinase of bacteriophage P1. Proc. Natl. Acad. Sci. USA 1988, 85, 5166–5170. [Google Scholar] [CrossRef] [PubMed]
- Rintoul, J.L.; Wang, J.; Gammon, D.B.; van Buuren, N.J.; Garson, K.; Jardine, K.; Barry, M.; Evans, D.H.; Bell, J.C. A selectable and excisable marker system for the rapid creation of recombinant poxviruses. PLoS ONE 2011, 6, e24643. [Google Scholar] [CrossRef]
- Guo, Z.S.; Liu, Z.; Sathaiah, M.; Wang, J.; Ravindranathan, R.; Kim, E.; Huang, S.; Kenniston, T.W.; Bell, J.C.; Zeh, H.J.; et al. Rapid Generation of Multiple Loci-Engineered Marker-free Poxvirus and Characterization of a Clinical-Grade Oncolytic Vaccinia Virus. Mol. Ther. Methods Clin. Dev. 2017, 7, 112–122. [Google Scholar] [CrossRef] [Green Version]
- Yuan, M.; Zhang, W.; Wang, J.; Al Yaghchi, C.; Ahmed, J.; Chard, L.; Lemoine, N.R.; Wang, Y. Efficiently Editing the Vaccinia Virus Genome by Using the CRISPR-Cas9 System. J. Virol. 2015, 89, 5176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gowripalan, A.; Smith, S.; Stefanovic, T.; Tscharke, D.C. Rapid poxvirus engineering using CRISPR/Cas9 as a selection tool. Commun. Biol. 2020, 3, 643. [Google Scholar] [CrossRef] [PubMed]
- Yuan, M.; Gao, X.; Chard, L.S.; Ali, Z.; Ahmed, J.; Li, Y.; Liu, P.; Lemoine, N.R.; Wang, Y. A marker-free system for highly efficient construction of vaccinia virus vectors using CRISPR Cas9. Mol. Ther. Methods Clin. Dev. 2015, 2, 15035. [Google Scholar] [CrossRef]
- Laudermilch, E.; Chandran, K. MAVERICC: Marker-free vaccinia virus engineering of recombinants through in vitro CRISPR/Cas9 cleavage. J. Mol. Biol. 2021, 433, 166896. [Google Scholar] [CrossRef]
- Borca, M.V.; Holinka, L.G.; Berggren, K.A.; Gladue, D.P. CRISPR-Cas9, a tool to efficiently increase the development of recombinant African swine fever viruses. Sci. Rep. 2018, 8, 3154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bi, Y.; Sun, L.; Gao, D.; Ding, C.; Li, Z.; Li, Y.; Cun, W.; Li, Q. High-efficiency targeted editing of large viral genomes by RNA-guided nucleases. PLoS Pathog. 2014, 10, e1004090. [Google Scholar] [CrossRef] [PubMed]
- Russell, T.A.; Stefanovic, T.; Tscharke, D.C. Engineering herpes simplex viruses by infection-transfection methods including recombination site targeting by CRISPR/Cas9 nucleases. J. Virol. Methods 2015, 213, 18–25. [Google Scholar] [CrossRef]
- Yang, H.; Wang, H.; Shivalila, C.S.; Cheng, A.W.; Shi, L.; Jaenisch, R. One-step generation of mice carrying reporter and conditional alleles by CRISPR/Cas-mediated genome engineering. Cell 2013, 154, 1370. [Google Scholar] [CrossRef] [Green Version]
- Jiang, W.; Bikard, D.; Cox, D.; Zhang, F.; Marraffini, L.A. RNA-guided editing of bacterial genomes using CRISPR-Cas systems. Nat. Biotechnol. 2013, 31, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Shi, T.Q.; Liu, G.N.; Ji, R.Y.; Shi, K.; Song, P.; Ren, L.J.; Huang, H.; Ji, X.-J. CRISPR/Cas9-based genome editing of the filamentous fungi: The state of the art. Appl. Microbiol. Biotechnol. 2017, 101, 7435–7443. [Google Scholar] [CrossRef] [PubMed]
- Lander, N.; Chiurillo, M.A.; Docampo, R. Genome Editing by CRISPR/Cas9: A Game Change in the Genetic Manipulation of Protists. J. Eukaryot. Microbiol. 2016, 63, 679–690. [Google Scholar] [CrossRef] [Green Version]
- Ebrahimi, S.; Teimoori, A.; Khanbabaei, H.; Tabasi, M. Harnessing CRISPR/Cas 9 System for manipulation of DNA virus genome. Rev. Med. Virol. 2019, 29, e2009. [Google Scholar] [CrossRef] [Green Version]
- Smith, E.S.; Shi, S.; Zauderer, M. Construction of cDNA libraries in vaccinia virus. Methods Mol. Biol. 2004, 269, 65–76. [Google Scholar]
- Smith, G.L.; Benfield, C.T.O.; Maluquer de Motes, C.; Mazzon, M.; Ember, S.W.J.; Ferguson, B.J.; Sumner, R.P. Vaccinia virus immune evasion: Mechanisms, virulence and immunogenicity. J. Gen. Virol. 2013, 94 Pt 11, 2367–2392. [Google Scholar] [CrossRef]
- Albarnaz, J.D.; Torres, A.A.; Smith, G.L. Modulating Vaccinia Virus Immunomodulators to Improve Immunological Memory. Viruses 2018, 10, 101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotwal, G.J.; Moss, B. Vaccinia virus encodes a secretory polypeptide structurally related to complement control proteins. Nature 1988, 335, 176–178. [Google Scholar] [CrossRef] [Green Version]
- McKenzie, R.; Kotwal, G.J.; Moss, B.; Hammer, C.H.; Frank, M.M. Regulation of complement activity by vaccinia virus complement-control protein. J. Infect. Dis. 1992, 166, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Tscharke, D.C.; Reading, P.C.; Smith, G.L. Dermal infection with vaccinia virus reveals roles for virus proteins not seen using other inoculation routes. J. Gen. Virol. 2002, 83 Pt 8, 1977–1986. [Google Scholar] [CrossRef] [PubMed]
- Palacios, S.; Perez, L.H.; Welsch, S.; Schleich, S.; Chmielarska, K.; Melchior, F.; Krijnse Locker, J. Quantitative SUMO-1 modification of a vaccinia virus protein is required for its specific localization and prevents its self-association. Mol. Biol. Cell 2005, 16, 2822–2835. [Google Scholar] [CrossRef] [Green Version]
- Wilcock, D.; Duncan, S.A.; Traktman, P.; Zhang, W.H.; Smith, G.L. The vaccinia virus A4OR gene product is a nonstructural, type II membrane glycoprotein that is expressed at the cell surface. J. Gen. Virol. 1999, 80 Pt 8, 2137–2148. [Google Scholar] [CrossRef]
- Stack, J.; Haga, I.R.; Schröder, M.; Bartlett, N.W.; Maloney, G.; Reading, P.C.; Fitzgerald, K.A.; Smith, G.L.; Bowie, A.G. Vaccinia virus protein A46R targets multiple Toll-like–interleukin-1 receptor adaptors and contributes to virulence. J. Exp. Med. 2005, 201, 1007. [Google Scholar] [CrossRef]
- Bahar, M.W.; Kenyon, J.C.; Putz, M.M.; Abrescia, N.G.A.; Pease, J.E.; Wise, E.L.; Stuart, D.I.; Smith, G.L.; Grimes, J.M. Structure and function of A41, a vaccinia virus chemokine binding protein. PLoS Pathog. 2008, 4, e5. [Google Scholar] [CrossRef] [Green Version]
- Harte, M.T.; Haga, I.R.; Maloney, G.; Gray, P.; Reading, P.C.; Bartlett, N.W.; Smith, G.L.; Bowie, A.; O’Neill, L.A.J. The Poxvirus Protein A52R Targets Toll-like Receptor Signaling Complexes to Suppress Host Defense. J. Exp. Med. 2003, 197, 343. [Google Scholar] [CrossRef]
- Eaglesham, J.B.; Pan, Y.; Kupper, T.S.; Kranzusch, P.J. Viral and metazoan poxins are cGAMP-specific nucleases that restrict cGAS-STING signaling. Nature 2019, 566, 259. [Google Scholar] [CrossRef]
- Alejo, A.; Ruiz-Argüello, M.B.; Ho, Y.; Smith, V.P.; Saraiva, M.; Alcami, A. A chemokine-binding domain in the tumor necrosis factor receptor from variola (smallpox) virus. Proc. Natl. Acad. Sci. USA 2006, 103, 5995–6000. [Google Scholar] [CrossRef] [PubMed]
- Symons, J.A.; Tscharke, D.C.; Price, N.; Smith, G.L. A study of the vaccinia virus interferon-gamma receptor and its contribution to virus virulence. J. Gen. Virol. 2002, 83 Pt 8, 1953–1964. [Google Scholar] [CrossRef] [PubMed]
- Price, N.; Tscharke, D.C.; Smith, G.L. The vaccinia virus B9R protein is a 6 kDa intracellular protein that is non-essential for virus replication and virulence. J. Gen. Virol. 2002, 83, 873–878. [Google Scholar] [CrossRef]
- Dobbelstein, M.; Shenk, T. Protection against apoptosis by the vaccinia virus SPI-2 (B13R) gene product. J. Virol. 1996, 70, 6479. [Google Scholar] [CrossRef]
- Chen, R.A.J.; Ryzhakov, G.; Cooray, S.; Randow, F.; Smith, G.L. Inhibition of IκB Kinase by Vaccinia Virus Virulence Factor B14. PLoS Pathog. 2008, 4, e22. [Google Scholar] [CrossRef] [Green Version]
- Staib, C.; Kisling, S.; Erfle, V.; Sutter, G. Inactivation of the viral interleukin 1beta receptor improves CD8+ T-cell memory responses elicited upon immunization with modified vaccinia virus Ankara. J. Gen. Virol. 2005, 86 Pt 7, 1997–2006. [Google Scholar] [CrossRef]
- Symons, J.A.; Alcamí, A.; Smith, G.L. Vaccinia virus encodes a soluble type I interferon receptor of novel structure and broad species specificity. Cell 1995, 81, 551–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unterholzner, L.; Sumner, R.P.; Baran, M.; Ren, H.; Mansur, D.S.; Bourke, N.M.; Randow, F.; Smith, G.L.; Bowie, A.G. Vaccinia Virus Protein C6 Is a Virulence Factor that Binds TBK-1 Adaptor Proteins and Inhibits Activation of IRF3 and IRF7. PLoS Pathog. 2011, 7, e1002247. [Google Scholar] [CrossRef]
- Perkus, M.E.; Goebel, S.J.; Davis, S.W.; Johnson, G.P.; Limbach, K.; Norton, E.K.; Paoletti, E. Vaccinia virus host range genes. Virology 1990, 179, 276–286. [Google Scholar] [CrossRef]
- Nájera, J.L.; Gómez, C.E.; Domingo-Gil, E.; Gherardi, M.M.; Esteban, M. Cellular and biochemical differences between two attenuated poxvirus vaccine candidates (MVA and NYVAC) and role of the C7L gene. J. Virol. 2006, 80, 6033–6047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, X.; Jiang, C.; Arsenio, J.; Dick, K.; Cao, J.; Xiang, Y. Vaccinia virus K1L and C7L inhibit antiviral activities induced by type I interferons. J. Virol. 2009, 83, 10627–10636. [Google Scholar] [CrossRef] [Green Version]
- Smith, V.P.; Bryant, N.A.; Alcamí, A. Ectromelia, vaccinia and cowpox viruses encode secreted interleu-kin-18-binding proteins. J. Gen. Virol. 2000, 81 Pt 5, 1223–1230. [Google Scholar] [PubMed]
- Yang, N.; Wang, Y.; Dai, P.; Li, T.; Zierhut, C.; Tan, A.; Zhang, T.; Xiang, J.Z.; Ordureau, A.; Funabiki, H.; et al. Vaccinia E5 is a major inhibitor of the DNA sensor cGAS. Nat. Commun. 2023, 14, 2898. [Google Scholar] [CrossRef] [PubMed]
- Schröder, M.; Baran, M.; Bowie, A.G. Viral targeting of DEAD box protein 3 reveals its role in TBK1/IKKɛ-mediated IRF activation. EMBO J. 2008, 27, 2147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teferi, W.M.; Desaulniers, M.A.; Noyce, R.S.; Shenouda, M.; Umer, B.; Evans, D.H. The vaccinia virus K7 protein promotes histone methylation associated with heterochromatin formation. PLoS ONE 2017, 12, e0173056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzlez, J.M.; Esteban, M. A poxvirus Bcl-2-like gene family involved in regulation of host immune response: Sequence similarity and evolutionary history. Virol. J. 2010, 7, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferguson, B.J.; Benfield, C.T.O.; Ren, H.; Lee, V.H.; Frazer, G.L.; Strnadova, P.; Sumner, R.P.; Smith, G.L. Vaccinia virus protein N2 is a nuclear IRF3 inhibitor that promotes virulence. J. Gen. Virol. 2013, 94 Pt 9, 2070–2081. [Google Scholar] [CrossRef] [PubMed]
- Pérez, P.; Marín, M.Q.; Lázaro-Frías, A.; Sorzano, C.Ó.S.; Gómez, C.E.; Esteban, M.; García-Arriaza, J. Deletion of Vaccinia Virus A40R Gene Improves the Immunogenicity of the HIV-1 Vaccine Candidate MVA-B. Vaccines 2020, 8, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marín, M.Q.; Pérez, P.; Gómez, C.E.; Sorzano, C.Ó.S.; Esteban, M.; García-Arriaza, J. Removal of the C6 Vaccinia Virus Interferon-β Inhibitor in the Hepatitis C Vaccine Candidate MVA-HCV Elicited in Mice High Immunogenicity in Spite of Reduced Host Gene Expression. Viruses 2018, 10, 414. [Google Scholar] [CrossRef] [Green Version]
- García-Arriaza, J.; Nájera, J.L.; Gómez, C.E.; Sorzano, C.O.S.; Esteban, M. Immunogenic Profiling in Mice of a HIV/AIDS Vaccine Candidate (MVA-B) Expressing Four HIV-1 Antigens and Potentiation by Specific Gene Deletions. PLoS ONE 2010, 5, e12395. [Google Scholar] [CrossRef]
- Garber, D.A.; O’Mara, L.A.; Gangadhara, S.; McQuoid, M.; Zhang, X.; Zheng, R.; Gill, K.; Verma, M.; Yu, T.; Johnson, B.; et al. Deletion of Specific Immune-Modulatory Genes from Modified Vaccinia Virus Ankara-Based HIV Vaccines Engenders Improved Immunogenicity in Rhesus Macaques. J. Virol. 2012, 86, 12605–12615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perdiguero, B.; Gómez, C.E.; Di Pilato, M.; Sorzano, C.O.S.; Delaloye, J.; Roger, T.; Calandra, T.; Pantaleo, G.; Esteban, M. Deletion of the Vaccinia Virus Gene A46R, Encoding for an Inhibitor of TLR Signalling, Is an Effective Approach to Enhance the Immunogenicity in Mice of the HIV/AIDS Vaccine Candidate NYVAC-C. PLoS ONE 2013, 8, e74831. [Google Scholar] [CrossRef] [PubMed]
- Holgado, M.P.; Falivene, J.; Maeto, C.; Amigo, M.; Pascutti, M.F.; Vecchione, M.B.; Bruttomesso, A.; Calamante, G.; Del Médico-Zajac, M.P.; Gherardi, M.M. Deletion of A44L, A46R and C12L Vaccinia Virus Genes from the MVA Genome Improved the Vector Immunogenicity by Modifying the Innate Immune Response Generating Enhanced and Optimized Specific T-Cell Responses. Viruses 2016, 8, 139. [Google Scholar] [CrossRef] [Green Version]
- Gómez, C.E.; Perdiguero, B.; Sánchez-Corzo, C.; Sorzano, C.O.S.; Esteban, M. Immune Modulation of NYVAC-Based HIV Vaccines by Combined Deletion of Viral Genes that Act on Several Signalling Pathways. Viruses 2018, 10, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Pilato, M.; Mejías-Pérez, E.; Zonca, M.; Perdiguero, B.; Gómez, C.E.; Trakala, M.; Nieto, J.; Nájera, J.L.; SSorzano, C.O.; Combadière, C.; et al. NFκB activation by modified vaccinia virus as a novel strategy to enhance neutrophil migration and HIV-specific T-cell responses. Proc. Natl. Acad. Sci. USA 2015, 112, E1333–E1342. [Google Scholar] [CrossRef]
- Di Pilato, M.; Mejías-Pérez, E.; Sorzano, C.O.; Esteban, M. Distinct Roles of Vaccinia Virus NF-κB Inhibitor Proteins A52, B15, and K7 in the Immune Response. J. Virol. 2017, 91, 10–1128. [Google Scholar] [CrossRef] [Green Version]
- Riederer, S.; del Canizo, A.; Navas, J.; Peter, M.G.; Link, E.K.; Sutter, G.; Rojas, J.J. Improving poxvirus-mediated antitumor immune responses by deleting viral cGAMP-specific nuclease. Cancer Gene Ther. 2023, 30, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Gomez, C.E.; Perdiguero, B.; Najera, J.L.; Sorzano, C.O.S.; Jimenez, V.; Gonzalez-Sanz, R.; Esteban, M. Removal of Vaccinia Virus Genes That Block Interferon Type I and II Pathways Improves Adaptive and Memory Responses of the HIV/AIDS Vaccine Candidate NYVAC-C in Mice. J. Virol. 2012, 86, 5026–5038. [Google Scholar] [CrossRef] [Green Version]
- Chea, L.S.; Wyatt, L.S.; Gangadhara, S.; Moss, B.; Amara, R.R. Novel Modified Vaccinia Virus Ankara Vector Expressing Anti-apoptotic Gene B13R Delays Apoptosis and Enhances Humoral Responses. J. Virol. 2019, 93, e01648-18. [Google Scholar] [CrossRef] [Green Version]
- García-Arriaza, J.; Nájera, J.L.; Gómez, C.E.; Tewabe, N.; Sorzano, C.O.S.; Calandra, T.; Roger, T.; Esteban, M. A candidate HIV/AIDS vaccine (MVA-B) lacking vaccinia virus gene C6L enhances memory HIV-1-specific T-cell responses. PLoS ONE 2011, 6, e24244. [Google Scholar] [CrossRef] [Green Version]
- García-Arriaza, J.; Arnáez, P.; Gómez, C.E.; Sorzano, C.Ó.S.; Esteban, M. Improving Adaptive and Memory Immune Responses of an HIV/AIDS Vaccine Candidate MVA-B by Deletion of Vaccinia Virus Genes (C6L and K7R) Blocking Interferon Signaling Pathways. PLoS ONE 2013, 8, e66894. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Sampedro, L.; Mejías-Pérez, E.; SSorzano, C.Ó.; Nájera, J.L.; Esteban, M. NYVAC vector modified by C7L viral gene insertion improves T cell immune responses and effectiveness against leishmaniasis. Virus Res. 2016, 220, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Arriaza, J.; Gomez, C.E.; Sorzano, C.O.S.; Esteban, M. Deletion of the Vaccinia Virus N2L Gene Encoding an Inhibitor of IRF3 Improves the Immunogenicity of Modified Vaccinia Virus Ankara Expressing HIV-1 Antigens. J. Virol. 2014, 88, 3392–3410. [Google Scholar] [CrossRef] [Green Version]
- Deng, S.; Martin, C.; Patil, R.; Zhu, F.; Zhao, B.; Xiang, Z.; He, Y. Vaxvec: The first web-based recombinant vaccine vector database and its data analysis. Vaccine 2015, 33, 6938. [Google Scholar] [CrossRef] [Green Version]
- He, Y.; Racz, R.; Sayers, S.; Lin, Y.; Todd, T.; Hur, J.; Li, X.; Patel, M.; Zhao, B.; Chung, M.; et al. Updates on the web-based VIOLIN vaccine database and analysis system. Nucleic Acids Res. 2014, 42, D1124–D1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiang, Z.; Todd, T.; Ku, K.P.; Kovacic, B.L.; Larson, C.B.; Chen, F.; Hodges, A.P.; Tian, Y.; Olenzek, E.A.; Zhao, B.; et al. VIOLIN: Vaccine investigation and online information network. Nucleic Acids Res. 2008, 36, D923–D928. [Google Scholar] [CrossRef] [Green Version]
- Perdiguero, B.; Gómez, C.E.; Esteban, M. Bioluminescence Imaging as a Tool for Poxvirus Biology. Methods in Molecular Biology; Humana: New York, NY, USA, 2019; pp. 269–285. Available online: https://pubmed.ncbi.nlm.nih.gov/31240684/ (accessed on 17 September 2020).
- Kieser, Q.; Paszkowski, P.; Lin, J.; Evans, D.; Noyce, R. Visualizing Poxvirus Replication and Recombination Using Live-Cell Imaging. Methods Mol. Biol. 2019, 2023, 221–235. [Google Scholar]
- Gallardo, F.; Schmitt, D.; Brandely, R.; Brua, C.; Silvestre, N.; Findeli, A.; Foloppe, J.; Top, S.; Kappler-Gratias, S.; Quentin-Froignant, C.; et al. Fluorescent Tagged Vaccinia Virus Genome Allows Rapid and Efficient Measurement of Oncolytic Potential and Discovery of Oncolytic Modulators. Biomedicines 2020, 8, 543. [Google Scholar] [CrossRef]
- Mok, H.; Yakimovich, A. Click Chemistry-Based Labeling of Poxvirus Genomes. Methods Mol. Biol. 2019, 2023, 209–220. [Google Scholar]
- Jordan, I.; Vos, A.; Beilfuß, S.; Neubert, A.; Breul, S.; Sandig, V. An avian cell line designed for production of highly attenuated viruses. Vaccine 2009, 27, 748–756. [Google Scholar] [CrossRef]
- Léon, A.; David, A.L.; Madeline, B.; Guianvarc’h, L.; Dureau, E.; Champion-Arnaud, P.; Hebben, M.; Huss, T.; Chatrenet, B.; Schwamborn, K. The EB66® cell line as a valuable cell substrate for MVA-based vaccines production. Vaccine 2016, 34, 5878–5885. [Google Scholar] [CrossRef] [PubMed]
- Kraus, B.; Fircks, S.; von Feigl, S.; Koch, S.M.; Fleischanderl, D.; Terler, K.; Dersch-Pourmojib, M.; Konetschny, C.; Grillberger, L.; Reiter, M. Avian cell line—Technology for large scale vaccine production. BMC Proc. 2011, 5 (Suppl. S8), P52. [Google Scholar] [CrossRef]
- Mayr, A. Genetically Engineered Virus for Use in the Propagation of Preferential Cells. U.S. Patent 6682743 B2, 2004. [Google Scholar]
- Jordan, I.; Lohr, V.; Genzel, Y.; Reichl, U.; Sandig, V. Elements in the Development of a Production Process for Modified Vaccinia Virus Ankara. Microorganisms 2013, 1, 100. [Google Scholar] [CrossRef] [PubMed]
- Jordan, I.; Northoff, S.; Thiele, M.; Hartmann, S.; Horn, D.; Höwing, K.; Bernhardt, H.; Oehmke, S.; von Horsten, H.; Rebeski, D.; et al. A chemically defined production process for highly attenuated poxviruses. Biologicals 2011, 39, 50–58. [Google Scholar] [CrossRef]
- Chen, Y.; Liao, Q.; Chen, T.; Zhang, Y.; Yuan, W.; Xu, J.; Zhang, X. Freeze-Drying Formulations Increased the Adenovirus and Poxvirus Vaccine Storage Times and Antigen Stabilities. Virol. Sin. 2021, 36, 365. [Google Scholar] [CrossRef]
- Hou, M.M.; Barrett, J.R.; Themistocleous, Y.; Rawlinson, T.A.; Diouf, A.; Martinez, F.J.; Nielsen, C.M.; Lias, A.M.; King, L.D.W.; Edwards, N.J.; et al. Vaccination with Plasmodium vivax Duffy-binding protein inhibits parasite growth during controlled human malaria infection. Sci. Transl. Med. 2023, 15, eadf1782. [Google Scholar] [CrossRef]
- Leung-Theung-Long, S.; Gouanvic, M.; Coupet, C.A.; Ray, A.; Tupin, E.; Silvestre, N.; Marchand, J.B.; Schmitt, D.; Hoffmann, C.; Klein, M.; et al. A Novel MVA-Based Multiphasic Vaccine for Prevention or Treatment of Tuberculosis Induces Broad and Multifunctional Cell-Mediated Immunity in Mice and Primates. PLoS ONE 2015, 10, e0143552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nangpal, P.; Bahal, R.K.; Tyagi, A.K. Boosting with recombinant MVA expressing M. tuberculosis α-crystallin antigen augments the protection imparted by BCG against tuberculosis in guinea pigs. Sci. Rep. 2017, 7, 17286. [Google Scholar] [CrossRef] [Green Version]
- García-Arriaza, J.; Perdiguero, B.; Heeney, J.L.; Seaman, M.S.; Montefiori, D.C.; Yates, N.L.; Tomaras, G.D.; Ferrari, G.; Foulds, K.E.; Roederer, M.; et al. HIV/AIDS Vaccine Candidates Based on Replication-Competent Recombinant Poxvirus NYVAC-C-KC Expressing Trimeric gp140 and Gag-Derived Virus-Like Particles or Lacking the Viral Molecule B19 That Inhibits Type I Interferon Activate Relevant HIV-1-Specific B and T Cell Immune Functions in Nonhuman Primates. J. Virol. 2017, 91, e02182-16. [Google Scholar]
- Chege, G.K.; Burgers, W.A.; Müller, T.L.; Gray, C.M.; Shephard, E.G.; Barnett, S.W.; Ferrari, G.; Montefiori, D.; Williamson, C.; Williamson, A.L. DNA-MVA-protein vaccination of rhesus macaques induces HIV-specific immunity in mucosal-associated lymph nodes and functional antibodies. Vaccine 2017, 35, 929–937. [Google Scholar] [CrossRef]
- Bradley, T.; Pollara, J.; Santra, S.; Vandergrift, N.; Pittala, S.; Bailey-Kellogg, C.; Shen, X.; Parks, R.; Goodman, D.; Eaton, A.; et al. Pentavalent HIV-1 vaccine protects against simian-human immunodeficiency virus challenge. Nat. Commun. 2017, 8, 15711. [Google Scholar] [CrossRef]
- Saunders, K.O.; Santra, S.; Parks, R.; Yates, N.L.; Sutherland, L.L.; Scearce, R.M.; Balachandran, H.; Bradley, T.; Goodman, D.; Eaton, A.; et al. Immunogenicity of NYVAC Prime-Protein Boost Human Immunodeficiency Virus Type 1 Envelope Vaccination and Simian-Human Immunodeficiency Virus Challenge of Nonhuman Primates. J. Virol. 2018, 92, e02035-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asbach, B.; Kibler, K.V.; Köstler, J.; Perdiguero, B.; Yates, N.L.; Stanfield-Oakley, S.; Tomaras, G.D.; Kao, S.F.; Foulds, K.E.; Roederer, M.; et al. Priming with a Potent HIV-1 DNA Vaccine Frames the Quality of Immune Responses prior to a Poxvirus and Protein Boost. J. Virol. 2019, 93, e01529-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perdiguero, B.; Gómez, C.E.; García-Arriaza, J.; Sánchez-Corzo, C.; Sorzano, C.Ó.S.; Wilmschen, S.; von Laer, D.; Asbach, B.; Schmalzl, C.; Peterhoff, D.; et al. Heterologous Combination of VSV-GP and NYVAC Vectors Expressing HIV-1 Trimeric gp145 Env as Vaccination Strategy to Induce Balanced B and T Cell Immune Responses. Front. Immunol. 2019, 10, 2941. [Google Scholar] [CrossRef] [Green Version]
- Raman, S.C.; Mejías-Pérez, E.; Gomez, C.E.; García-Arriaza, J.; Perdiguero, B.; Vijayan, A.; Pérez-Ruiz, M.; Cuervo, A.; Santiago, C.; Sorzano, C.O.S.; et al. The Envelope-Based Fusion Antigen GP120C14K Forming Hexamer-Like Structures Triggers T Cell and Neutralizing Antibody Responses Against HIV-1. Front. Immunol. 2019, 10, 2793. [Google Scholar] [CrossRef]
- Lévy, Y.; Lacabaratz, C.; Ellefsen-Lavoie, K.; Stöhr, W.; Lelièvre, J.D.; Bart, P.A.; Launay, O.; Weber, J.; Salzberger, B.; Wiedemann, A.; et al. Optimal priming of poxvirus vector (NYVAC)based HIV vaccine regimens for T cell responses requires three DNA injections. Results of the randomized multicentre EV03/ ANRS VAC20 Phase I/II Trial. PLoS Pathog. 2020, 16, e1008522. [Google Scholar] [CrossRef]
- Gómez, C.E.; Perdiguero, B.; Usero, L.; Marcos-Villar, L.; Miralles, L.; Leal, L.; Sorzano, C.Ó.S.; Sánchez-Corzo, C.; Plana, M.; García, F.; et al. Enhancement of the HIV-1-Specific Immune Response Induced by an mRNA Vaccine through Boosting with a Poxvirus MVA Vector Expressing the Same Antigen. Vaccines 2021, 9, 959. [Google Scholar] [CrossRef]
- Wee, E.G.; Moyo, N.; Hannoun, Z.; Giorgi, E.E.; Korber, B.; Hanke, T. Effect of epitope variant co-delivery on the depth of CD8 T cell responses induced by HIV-1 conserved mosaic vaccines. Mol. Ther. Methods Clin. Dev. 2021, 21, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Li, Y.; Zhong, M.; Yang, J.; Zhou, D.; Zhao, B.; Cao, Y.; Yan, H.; Zhang, E.; Yang, Y.; et al. Improved immune response against HIV-1 Env antigen by enhancing EEV production via a K151E mutation in the A34R gene of replication-competent vaccinia virus Tiantan. Antiviral Res. 2018, 153, 49–59. [Google Scholar] [CrossRef]
- Kibler, K.V.; Asbach, B.; Perdiguero, B.; García-Arriaza, J.; Yates, N.L.; Parks, R.; Stanfield-Oakley, S.; Ferrari, G.; Montefiori, D.C.; Tomaras, G.D.; et al. Replication-Competent NYVAC-KC Yields Improved Immunogenicity to HIV-1 Antigens in Rhesus Macaques Compared to Nonreplicating NYVAC. J. Virol. 2019, 93, 1513–1518. [Google Scholar] [CrossRef] [Green Version]
- Pérez, P.; Marín, M.Q.; Lázaro-Frías, A.; Sorzano, C.Ó.S.; Di Pilato, M.; Gómez, C.E.; Esteban, M.; García-Arriaza, J. An MVA Vector Expressing HIV-1 Envelope under the Control of a Potent Vaccinia Virus Promoter as a Promising Strategy in HIV/AIDS Vaccine Design. Vaccines 2019, 7, 208. [Google Scholar] [CrossRef] [Green Version]
- Bollimpelli, V.S.; Reddy, P.B.J.; Gangadhara, S.; Charles, T.P.; Burton, S.L.; Tharp, G.K.; Styles, T.M.; Labranche, C.C.; Smith, J.C.; Upadhyay, A.A.; et al. Intradermal but not intramuscular modified vaccinia Ankara immunizations protect against intravaginal tier2 simian-human immunodeficiency virus challenges in female macaques. Nat. Commun. 2023, 14, 4789. [Google Scholar] [CrossRef]
- Falqui, M.; Perdiguero, B.; Coloma, R.; Albert, M.; Marcos-Villar, L.; McGrail, J.P.; Sorzano, C.Ó.S.; Esteban, M.; Gómez, C.E.; Guerra, S. An MVA-based vector expressing cell-free ISG15 increases IFN-I production and improves HIV-1-specific CD8 T cell immune responses. Front. Cell Infect. Microbiol. 2023, 13, 1187193. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo, M.M.; Marín-López, A.; Chiem, K.; Jimenez-Cabello, L.; Ullah, I.; Utrilla-Trigo, S.; Calvo-Pinilla, E.; Lorenzo, G.; Moreno, S.; Ye, C.; et al. Vaccinia Virus Strain MVA Expressing a Prefusion-Stabilized SARS-CoV-2 Spike Glycoprotein Induces Robust Protection and Prevents Brain Infection in Mouse and Hamster Models. Vaccines 2023, 11, 1006. [Google Scholar] [CrossRef]
- Styles, T.M.; Gangadhara, S.; Reddy, P.B.J.; Sahoo, A.; Shiferaw, A.; Welbourn, S.; Kozlowski, P.A.; Derdeyn, C.A.; Velu, V.; Amara, R.R. V2 hotspot optimized MVA vaccine expressing stabilized HIV-1 Clade C envelope Gp140 delays acquisition of heterologous Clade C Tier 2 challenges in Mamu-A*01 negative Rhesus Macaques. Front. Immunol. 2022, 13, 914969. [Google Scholar] [CrossRef]
- Sahoo, A.; Jones, A.T.; Cheedarla, N.; Gangadhara, S.; Roy, V.; Styles, T.M.; Shiferaw, A.; Walter, K.L.; Williams, L.T.D.; Shen, X.; et al. A clade C HIV-1 vaccine protects against heterologous SHIV infection by modulating IgG glycosylation and T helper response in macaques. Sci. Immunol. 2022, 7, eabl4102. [Google Scholar] [CrossRef]
- Wilken, L.; Stelz, S.; Agac, A.; Sutter, G.; Prajeeth, C.K.; Rimmelzwaan, G.F. Recombinant Modified Vaccinia Virus Ankara Expressing a Glycosylation Mutant of Dengue Virus NS1 Induces Specific Antibody and T-Cell Responses in Mice. Vaccines 2023, 11, 714. [Google Scholar] [CrossRef]
- Pérez, P.; Marín, M.Q.; Lázaro-Frías, A.; Jiménez de Oya, N.; Blázquez, A.B.; Escribano-Romero, E.; Carlos, C.Ó.; Ortego, J.; Saiz, J.C.; Esteban, M.; et al. A Vaccine Based on a Modified Vaccinia Virus Ankara Vector Expressing Zika Virus Structural Proteins Controls Zika Virus Replication in Mice. Sci. Rep. 2018, 8, 17385. [Google Scholar] [CrossRef] [Green Version]
- Prow, N.A.; Liu, L.; McCarthy, M.K.; Walters, K.; Kalkeri, R.; Geiger, J.; Koide, F.; Cooper, T.H.; Eldi, P.; Nakayama, E.; et al. The vaccinia virus based Sementis Copenhagen Vector vaccine against Zika and chikungunya is immunogenic in non-human primates. npj Vaccines 2020, 5, 44. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Deng, Y.; Huang, B.; Song, Q.; Wang, W.; Yang, Y.; Dai, L.; Wang, W.; Yan, J.; Gao, G.F.; et al. Humoral and cellular immunity against both ZIKV and poxvirus is elicited by a two-dose regimen using DNA and non-replicating vaccinia virus-based vaccine candidates. Vaccine 2019, 37, 2122–2130. [Google Scholar] [CrossRef] [PubMed]
- Jiménez de Oya, N.; Pérez, P.; Blázquez, A.B.; Escribano-Romero, E.; Esteban, M.; Saiz, J.C.; García-Arriaza, J.; Mar-tín-Acebes, M.A. Low Immune Cross-Reactivity between West Nile Virus and a Zika Virus Vaccine Based on Modified Vaccinia Virus Ankara. Pharmaceuticals 2022, 15, 354. [Google Scholar] [CrossRef] [PubMed]
- Volz, A.; Lim, S.; Kaserer, M.; Lülf, A.; Marr, L.; Jany, S.; Deeg, C.A.; Pijlman, G.P.; Koraka, P.; Osterhaus, A.D.M.E.; et al. Immunogenicity and protective efficacy of recombinant Modified Vaccinia virus Ankara candidate vaccines delivering West Nile virus envelope antigens. Vaccine 2016, 34, 1915–1926. [Google Scholar] [CrossRef] [PubMed]
- Julander, J.G.; Testori, M.; Cheminay, C.; Volkmann, A. Immunogenicity and protection after vaccination with a modified vaccinia virus Ankara-vectored yellow fever vaccine in the hamster model. Front. Immunol. 2018, 9, 1756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beicht, J.; Kubinski, M.; Zdora, I.; Puff, C.; Biermann, J.; Gerlach, T.; Baumgärtner, W.; Sutter, G.; Osterhaus, A.D.M.E.; Prajeeth, C.K.; et al. Induction of humoral and cell-mediated immunity to the NS1 protein of TBEV with recombinant Influenza virus and MVA affords partial protection against lethal TBEV infection in mice. Front. Immunol. 2023, 14, 1177324. [Google Scholar] [CrossRef] [PubMed]
- Kubinski, M.; Beicht, J.; Zdora, I.; Biermann, J.; Puff, C.; Gerlach, T.; Tscherne, A.; Baumgärtner, W.; Osterhaus, A.D.M.E.; Sutter, G.; et al. A recombinant Modified Vaccinia virus Ankara expressing prME of tick-borne encephalitis virus affords mice full protection against TBEV infection. Front. Immunol. 2023, 14, 1182963. [Google Scholar] [CrossRef]
- García-Arriaza, J.; Esteban, M.; López, D. Modified Vaccinia Virus Ankara as a Viral Vector for Vaccine Candidates against Chikungunya Virus. Biomedicines 2021, 9, 1122. [Google Scholar] [CrossRef]
- Buttigieg, K.R.; Dowall, S.D.; Findlay-Wilson, S.; Miloszewska, A.; Rayner, E.; Hewson, R.; Carroll, M.W. A novel vaccine against Crimean-Congo haemorrhagic fever protects 100% of animals against lethal challenge in a mouse model. PLoS ONE 2014, 9, e91516. [Google Scholar] [CrossRef] [Green Version]
- Malherbe, D.C.; Domi, A.; Hauser, M.J.; Atyeo, C.; Fischinger, S.; Hyde, M.A.; Williams, J.M.; Alter, G.; Guirakhoo, F.; Bukreyev, A. A single immunization with a modified vaccinia Ankara vectored vaccine producing Sudan virus-like particles protects from lethal infection. NPJ Vaccines 2022, 7, 83. [Google Scholar] [CrossRef]
- Lázaro-Frías, A.; Gómez-Medina, S.; Sánchez-Sampedro, L.; Ljungberg, K.; Ustav, M.; Liljeström, P.; Muñoz-Fontela, C.; Esteban, M.; García-Arriaza, J. Distinct Immunogenicity and Efficacy of Poxvirus-Based Vaccine Candidates against Ebola Virus Expressing GP and VP40 Proteins. J. Virol. 2018, 92, 363–381. [Google Scholar] [CrossRef] [Green Version]
- Rahim, M.N.; Wee, E.G.; He, S.; Audet, J.; Tierney, K.; Moyo, N.; Hannoun, Z.; Crook, A.; Baines, A.; Korber, B.; et al. Complete protection of the BALB/c and C57BL/6J mice against Ebola and Marburg virus lethal challenges by pan-filovirus T-cell epigraph vaccine. PLoS Pathog. 2019, 15, e1007564. [Google Scholar] [CrossRef]
- Xie, L.; Zai, J.; Yi, K.; Li, Y. Intranasal immunization with recombinant Vaccinia virus Tiantan harboring Zaire Ebola virus gp elicited systemic and mucosal neutralizing antibody in mice. Vaccine 2019, 37, 3335–3342. [Google Scholar] [CrossRef] [PubMed]
- Medina-Magües, E.S.; Lopera-Madrid, J.; Lo, M.K.; Spiropoulou, C.F.; Montgomery, J.M.; Medina-Magües, L.G.; Salas-Quinchucua, C.; Jiménez-Mora, A.P.; Osorio, J.E. Immunogenicity of poxvirus-based vaccines against Nipah virus. Sci. Rep. 2023, 13, 11384. [Google Scholar] [CrossRef]
- Coughlan, L.; Sridhar, S.; Payne, R.; Edmans, M.; Milicic, A.; Venkatraman, N.; Lugonja, B.; Clifton, L.; Qi, C.; Folegatti, P.M.; et al. Heterologous Two-Dose Vaccination with Simian Adenovirus and Poxvirus Vectors Elicits Long-Lasting Cellular Immunity to Influenza Virus A in Healthy Adults. EBioMedicine 2018, 29, 146–154. [Google Scholar] [CrossRef] [Green Version]
- Langenmayer, M.C.; Luelf-Averhoff, A.T.; Marr, L.; Jany, S.; Freudenstein, A.; Adam-Neumair, S.; Tscherne, A.; Fux, R.; Rojas, J.J.; Blutke, A.; et al. Newly Designed Poxviral Promoters to Improve Immunogenicity and Efficacy of MVA-NP Candidate Vaccines against Lethal Influenza Virus Infection in Mice. Pathogens 2023, 12, 867. [Google Scholar] [CrossRef] [PubMed]
- Vatzia, E.; Feest, K.; McNee, A.; Manjegowda, T.; Carr, B.V.; Paudyal, B.; Chrun, T.; Maze, E.A.; Mccarron, A.; Morris, S.; et al. Immunization with matrix-, nucleoprotein and neuraminidase protects against H3N2 influenza challenge in pH1N1 pre-exposed pigs. NPJ Vaccines 2023, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Villadiego, J.; García-Arriaza, J.; Ramírez-Lorca, R.; García-Swinburn, R.; Cabello-Rivera, D.; Rosales-Nieves, A.E.; Álvarez-Vergara, M.I.; Cala-Fernández, F.; García-Roldán, E.; López-Ogáyar, J.L.; et al. Full protection from SARS-CoV-2 brain infection and damage in susceptible transgenic mice conferred by MVA-CoV2-S vaccine candidate. Nat. Neurosci. 2023, 26, 226–238. [Google Scholar] [CrossRef] [PubMed]
- Russell, M.S.; Thulasi Raman, S.N.; Gravel, C.; Zhang, W.; Pfeifle, A.; Chen, W.; Van Domselaar, G.; Safronetz, D.; Johnston, M.; Sauve, S.; et al. Single Immunization of a Vaccine Vectored by a Novel Recombinant Vaccinia Virus Affords Effective Protection Against Respiratory Syncytial Virus Infection in Cotton Rats. Front. Immunol. 2021, 12, 747866. [Google Scholar] [CrossRef]
- Endt, K.; Wollmann, Y.; Haug, J.; Bernig, C.; Feigl, M.; Heiseke, A.; Kalla, M.; Hochrein, H.; Suter, M.; Chaplin, P.; et al. A Recombinant MVA-Based RSV Vaccine Induces T-Cell and Antibody Responses That Cooperate in the Protection Against RSV Infection. Front. Immunol. 2022, 13, 841471. [Google Scholar] [CrossRef]
- Alharbi, N.K.; Aljamaan, F.; Aljami, H.A.; Alenazi, M.W.; Albalawi, H.; Almasoud, A.; Alharthi, F.J.; Azhar, E.I.; Barhoumi, T.; Bosaeed, M.; et al. Immunogenicity of High-Dose MVA-Based MERS Vaccine Candidate in Mice and Camels. Vaccines 2022, 10, 1330. [Google Scholar] [CrossRef]
- Weskamm, L.M.; Fathi, A.; Raadsen, M.P.; Mykytyn, A.Z.; Koch, T.; Spohn, M.; Friedrich, M.; Bartels, E.; Gundlach, S.; Hesterkamp, T.; et al. Persistence of MERS-CoV-spike-specific B cells and antibodies after late third immunization with the MVA-MERS-S vaccine. Cell Rep. Med. 2022, 3, 100685. [Google Scholar] [CrossRef]
- Chiuppesi, F.; Salazar, M.D.A.; Contreras, H.; Nguyen, V.; Martinez, J.; Park, S.; Nguyen, J.; Kha, M.; Iniguez, A.; Zhou, Q.; et al. Development of a Multi-Antigenic SARS-CoV-2 Vaccine Using a Synthetic Poxvirus Platform. Res. Sq. 2020, 3, 40198. [Google Scholar]
- Tscherne, A.; Hendrik Schwarz, J.; Rohde, C.; Kupke, A.; Kalodimou, G.; Limpinsel, L.; Okba, N.M.A.; Bošnjak, B.; Sandrock, I.; Odak, I.; et al. Immunogenicity and efficacy of the COVID-19 candidate vector vaccine MVA-SARS-2-S in preclinical vaccination. Proc. Natl. Acad. Sci. USA 2021, 118, e2026207118. [Google Scholar] [CrossRef]
- Mooij, P.; García-Arriaza, J.; Pérez, P.; Lázaro-Frías, A.; Verstrepen, B.E.; Böszörményi, K.P.; Mortier, D.; Fagrouch, Z.; Kiemenyi-Kayere, G.; Niphuis, H.; et al. Poxvirus MVA Expressing SARS-CoV-2 S Protein Induces Robust Immunity and Protects Rhesus Macaques From SARS-CoV-2. Front. Immunol. 2022, 13, 845887. [Google Scholar] [CrossRef]
- Boulton, S.; Poutou, J.; Martin, N.T.; Azad, T.; Singaravelu, R.; Crupi, M.J.F.; Jamieson, T.; He, X.; Marius, R.; Petryk, J.; et al. Single-dose replicating poxvirus vector-based RBD vaccine drives robust humoral and T cell immune response against SARS-CoV-2 infection. Mol. Ther. 2022, 30, 1885–1896. [Google Scholar] [CrossRef] [PubMed]
- Pérez, P.; Lázaro-Frías, A.; Zamora, C.; Sánchez-Cordón, P.J.; Astorgano, D.; Luczkowiak, J.; Delgado, R.; Casasnovas, J.M.; Esteban, M.; García-Arriaza, J. A Single Dose of an MVA Vaccine Expressing a Prefusion-Stabilized SARS-CoV-2 Spike Protein Neutralizes Variants of Concern and Protects Mice From a Lethal SARS-CoV-2 Infection. Front. Immunol. 2022, 12, 824728. [Google Scholar] [CrossRef]
- Perdiguero, B.; Marcos-Villar, L.; López-Bravo, M.; Sánchez-Cordón, P.J.; Zamora, C.; Valverde, J.R.; Sorzano, C.Ó.S.; Sin, L.; Álvarez, E.; Ramos, M.; et al. Immunogenicity and efficacy of a novel multi-patch SARS-CoV-2/COVID-19 vaccine candidate. Front. Immunol. 2023, 14, 1160065. [Google Scholar] [CrossRef]
- Kalodimou, G.; Jany, S.; Freudenstein, A.; Schwarz, J.H.; Limpinsel, L.; Rohde, C.; Kupke, A.; Becker, S.; Volz, A.; Tscherne, A.; et al. Short- and Long-Interval Prime-Boost Vaccination with the Candidate Vaccines MVA-SARS-2-ST and MVA-SARS-2-S Induces Comparable Humoral and Cell-Mediated Immunity in Mice. Viruses 2023, 15, 1180. [Google Scholar] [CrossRef] [PubMed]
- Wussow, F.; Kha, M.; Kim, T.; Ly, M.; Yll-Pico, M.; Kar, S.; Lewis, M.G.; Chiuppesi, F.; Diamond, D.J. Synthetic multi-antigen MVA vaccine COH04S1 and variant-specific derivatives protect Syrian hamsters from SARS-CoV-2 Omicron subvariants. NPJ Vaccines 2023, 8, 41. [Google Scholar] [CrossRef]
- Ishigaki, H.; Yasui, F.; Nakayama, M.; Endo, A.; Yamamoto, N.; Yamaji, K.; Nguyen, C.T.; Kitagawa, Y.; Sanada, T.; Honda, T.; et al. An attenuated vaccinia vaccine encoding the severe acute respiratory syndrome coronavirus-2 spike protein elicits broad and durable immune responses, and protects cynomolgus macaques and human angiotensin-converting enzyme 2 transgenic mice from severe acute respiratory syndrome coronavirus-2 and its variants. Front. Microbiol. 2022, 13, 967019. [Google Scholar] [PubMed]
- Americo, J.L.; Cotter, C.A.; Earl, P.L.; Liu, R.; Moss, B. Intranasal inoculation of an MVA-based vaccine induces IgA and protects the respiratory tract of hACE2 mice from SARS-CoV-2 infection. Proc. Natl. Acad. Sci. USA 2022, 119, e2202069119. [Google Scholar] [CrossRef]
- Deschambault, Y.; Lynch, J.; Warner, B.; Tierney, K.; Huynh, D.; Vendramelli, R.; Tailor, N.; Frost, K.; Sajesh, B.; LeBlanc, K.; et al. Single Immunization with Recombinant ACAM2000 Vaccinia Viruses Expressing the Spike and the Nucleocapsid Proteins Protects Hamsters against SARS-CoV-2-Caused Clinical Disease. J. Virol. 2022, 96, e00389-22. [Google Scholar] [CrossRef]
- Richert, L.; Lelièvre, J.D.; Lacabaratz, C.; Hardel, L.; Hocini, H.; Wiedemann, A.; Lucht, F.; Poizot-Martin, I.; Bauduin, C.; Diallo, A.; et al. T Cell Immunogenicity, Gene Expression Profile, and Safety of Four Heterologous Prime-Boost Combinations of HIV Vaccine Candidates in Healthy Volunteers: Results of the Randomized Multi-Arm Phase I/II ANRS VRI01 Trial. J. Immunol. 2022, 208, 2663–2674. [Google Scholar] [CrossRef]
- Rowland, R.; Pathan, A.A.; Satti, I.; Poulton, I.D.; Matsumiya, M.M.L.; Whittaker, M.; Minassian, A.M.; O’Hara, G.A.; Hamill, M.; Scott, J.T.; et al. Safety and immunogenicity of an FP9-vectored candidate tuberculosis vaccine (FP85A), alone and with candidate vaccine MVA85A in BCG-vaccinated healthy adults: A phase i clinical trial. Hum. Vaccin. Immunother. 2013, 9, 50–62. [Google Scholar] [CrossRef] [Green Version]
- Tameris, M.D.; Hatherill, M.; Landry, B.S.; Scriba, T.J.; Snowden, M.A.; Lockhart, S.; Shea, J.E.; McClain, J.B.; Hussey, G.D.; Hanekom, W.A.; et al. Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: A randomised, placebo-controlled phase 2b trial. Lancet 2013, 381, 1021. [Google Scholar] [CrossRef] [Green Version]
- Jordan, E.; Kabir, G.; Schultz, S.; Silbernagl, G.; Schmidt, D.; Jenkins, V.A.; Weidenthaler, H.; Stroukova, D.; Martin, B.K.; De Moerlooze, L. Reduced Respiratory Syncytial Virus Load, Symptoms, and Infections: A Human Challenge Trial of MVA-BN-RSV Vaccine. J. Infect. Dis. 2023, jiad108. [Google Scholar] [CrossRef]
- Evans, T.G.; Bussey, L.; Eagling-Vose, E.; Rutkowski, K.; Ellis, C.; Argent, C.; Griffin, P.; Kim, J.; Thackwray, S.; Shakib, S.; et al. Efficacy and safety of a universal influenza A vaccine (MVA-NP+M1) in adults when given after seasonal quadrivalent influenza vaccine immunisation (FLU009): A phase 2b, randomised, double-blind trial. Lancet Infect. Dis. 2022, 22, 857–866. [Google Scholar] [CrossRef]
- Chiuppesi, F.; Zaia, J.A.; Frankel, P.H.; Stan, R.; Drake, J.; Williams, B.; Acosta, A.M.; Francis, K.; Taplitz, R.A.; Dickter, J.K.; et al. Safety and immunogenicity of a synthetic multiantigen modified vaccinia virus Ankara-based COVID-19 vaccine (COH04S1): An open-label and randomised, phase 1 trial. Lancet Microbe 2022, 3, e252–e264. [Google Scholar] [CrossRef] [PubMed]
- Hermann, J.R.; Fry, A.M.; Siev, D.; Slate, D.; Lewis, C.; Gatewood, D.M. Stability of vaccinia-vectored recombinant oral rabies vaccine under field conditions: A 3-year study. Can. J. Vet. Res. 2011, 75, 278. [Google Scholar] [PubMed]
- Tomori, O.; Kolawole, M.O. Ebola virus disease: Current vaccine solutions. Curr. Opin. Immunol. 2021, 71, 27–33. [Google Scholar] [CrossRef]
- Moss, B. Reflections on the Early Development of Poxvirus Vectors. Vaccine 2013, 31, 4220. [Google Scholar] [CrossRef] [Green Version]

| VACV Genes | Functions | Mutants Reported in Vaccine Research |
|---|---|---|
| A40R | Virulence [86] or essential gene [87,111] | [109] |
| A41L | Chemokine inhibitor [89] | [112,113] |
| A46R | NF-κB inhibitor [88] | [113,114,115,116] |
| A52R | NF-κB inhibitor [90] | [116,117,118] |
| B2R | IFN and NF-κB inhibitor [91] | [119] * |
| B6R | Unknown | [116] |
| B7R | TNF decoy [92] | [116] |
| B8R | IFN-γ inhibitor [93] | [116,120] |
| B9R | Replication in vivo [94] | [116] |
| B10R | Unknown | [116] |
| B13R | Apoptosis inhibitor [95] | [121] |
| B15R | IκB kinase inhibitor [96] | [113,116,117,118] |
| B16R | IL-1β decoy [97] | [112] |
| B19R | Type I IFN inhibitor [98] | [116,120] |
| C6L | IFN-β inhibitor [99] | [110,122,123] |
| C7L | Type I IFN inhibitor [100,101,102] | [124] |
| C12L | IL-18 inhibitor [103] | [113,115] |
| E5R | Virulence factor and IFN inhibitor [104] | [104] |
| K7R | NF-κB inhibitor [105,106,107] | [116,117,118,123] |
| N2L | IRF3 inhibitor [107,108] | [125] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y. Rendezvous with Vaccinia Virus in the Post-smallpox Era: R&D Advances. Viruses 2023, 15, 1742. https://doi.org/10.3390/v15081742
Wang Y. Rendezvous with Vaccinia Virus in the Post-smallpox Era: R&D Advances. Viruses. 2023; 15(8):1742. https://doi.org/10.3390/v15081742
Chicago/Turabian StyleWang, Yuxiang. 2023. "Rendezvous with Vaccinia Virus in the Post-smallpox Era: R&D Advances" Viruses 15, no. 8: 1742. https://doi.org/10.3390/v15081742
APA StyleWang, Y. (2023). Rendezvous with Vaccinia Virus in the Post-smallpox Era: R&D Advances. Viruses, 15(8), 1742. https://doi.org/10.3390/v15081742





