Pediatric Respiratory Hospitalizations in the Pre-COVID-19 Era: The Contribution of Viral Pathogens and Comorbidities to Clinical Outcomes, Valencia, Spain
Abstract
1. Introduction
2. Materials and Methods
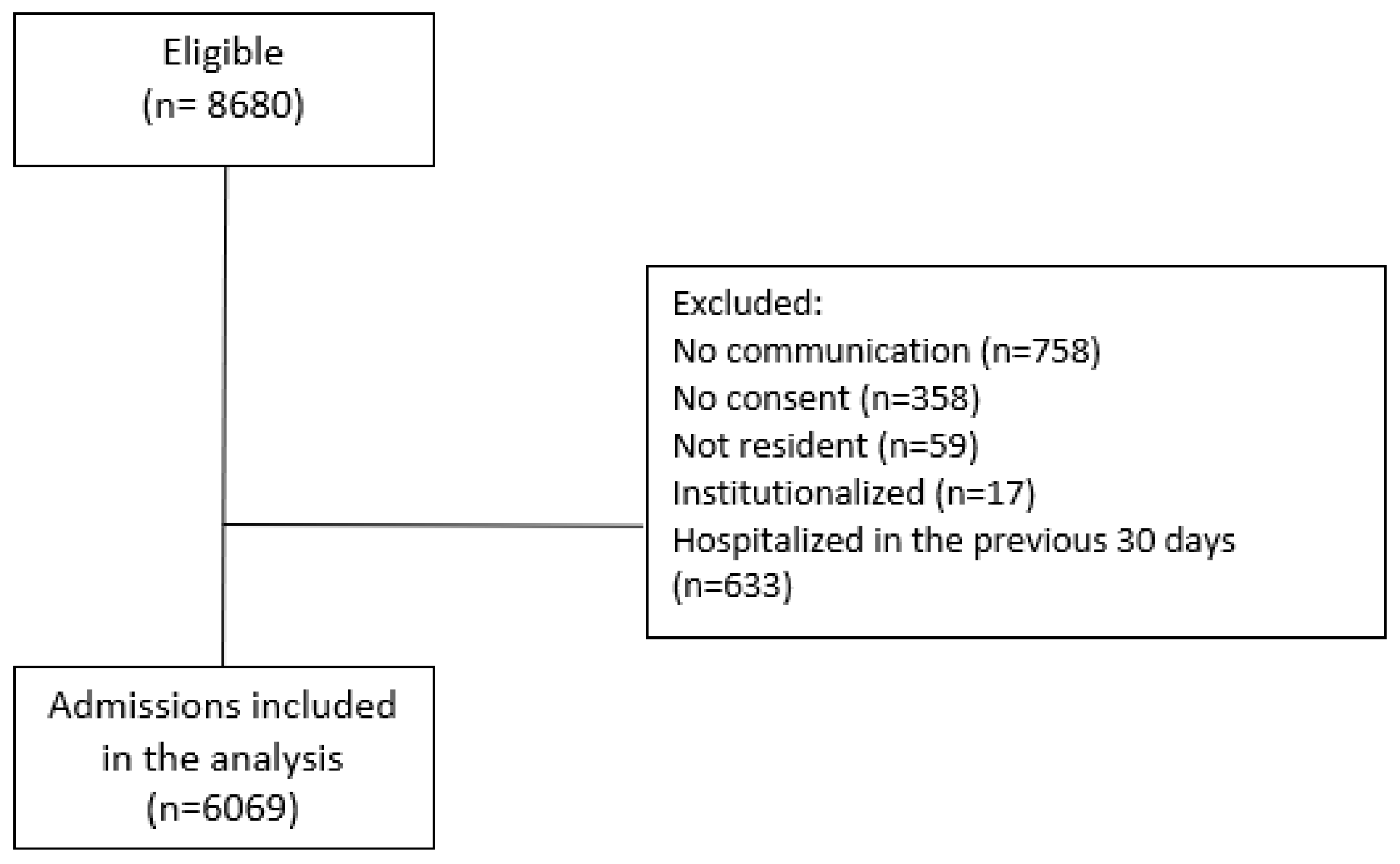
2.1. Population
2.2. Inclusion Criteria
2.3. Laboratory Methods
2.4. Data Sources and Categorization
2.5. Statistical Method
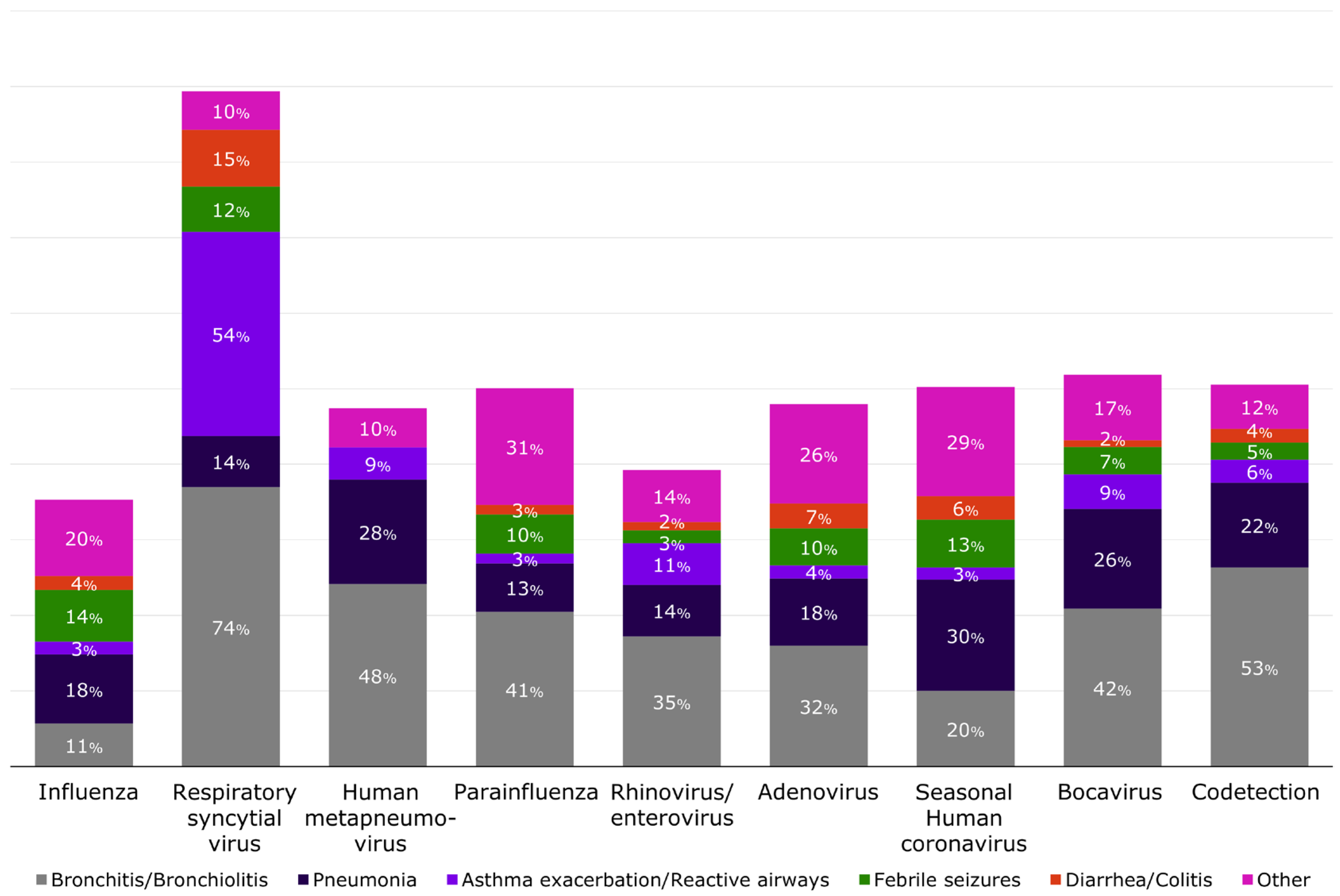
3. Results
3.1. Demographic Characteristics and Underlying Health Status of Hospitalized Children
3.2. Impact of Comorbidities on the Presence of Complications and Disease Severity
3.3. Impact of Comorbidities Associated with Selected Viral Pathogens
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Collaborators GLRI. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect. Dis. 2017, 17, 1133–1161. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Williams, D.J.; Arnold, S.R.; Ampofo, K.; Bramley, A.M.; Reed, C.; Stockmann, C.; Anderson, E.J.; Grijalva, C.G.; Self, W.H.; et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N. Engl. J. Med. 2015, 372, 835–845. [Google Scholar] [CrossRef] [PubMed]
- Derqui, N.; Nealon, J.; Mira-Iglesias, A.; Díez-Domingo, J.; Mahé, C.; Chaves, S.S. Predictors of influenza severity among hospitalized adults with laboratory confirmed influenza: Analysis of nine influenza seasons from the Valencia region, Spain. Influenza Other Respir. Viruses 2022, 16, 862–872. [Google Scholar] [CrossRef] [PubMed]
- Simon, T.D.; Mahant, S.; Cohen, E. Pediatric Hospital Medicine and Children with Medical Complexity: Past, Present, and Future. Curr. Probl. Pediatr. Adolesc. Health Care 2012, 42, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Keren, R. Flu-related hospitalization in children. LDI Issue Brief 2006, 12, 1–4. [Google Scholar] [PubMed]
- American Academy of Pediatrics Committee on Infectious Diseases; American Academy of Pediatrics Bronchiolitis Guidelines Committee. Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 2014, 134, e620–e638. [Google Scholar] [CrossRef]
- Gov.UK. Available online: https://www.gov.uk/government/publications/covid-19-vaccination-resources-for-children-aged-5-to-11-years (accessed on 28 March 2022).
- Rha, B.; Curns, A.T.; Lively, J.Y.; Campbell, A.P.; Englund, J.A.; Boom, J.A.; Azimi, P.H.; Weinberg, G.A.; Staat, M.A.; Selvarangan, R.; et al. Respiratory Syncytial Virus-Associated Hospitalizations Among Young Children: 2015–2016. Pediatrics 2020, 146, e20193611. [Google Scholar] [CrossRef]
- Arriola, C.S.; Kim, L.; Langley, G.; Anderson, E.J.; Openo, K.; Martin, A.M.; Lynfield, R.; Bye, E.; Como-Sabetti, K.; Reingold, A.; et al. Estimated Burden of Community-Onset Respiratory Syncytial Virus–Associated Hospitalizations among Children Aged <2 Years in the United States, 2014–2015. J. Pediatr. Infect. Dis. Soc. 2020, 9, 587–595. [Google Scholar] [CrossRef]
- Hall, C.B.; Weinberg, G.A.; Blumkin, A.K.; Edwards, K.M.; Staat, M.A.; Schultz, A.F.; Poehling, K.A.; Szilagyi, P.G.; Griffin, M.R.; Williams, J.V.; et al. Respiratory Syncytial Virus–Associated Hospitalizations Among Children Less Than 24 Months of Age. Pediatrics 2013, 132, e341–e348. [Google Scholar] [CrossRef]
- Hauge, S.H.; Bakken, I.J.; de Blasio, B.F.; Håberg, S.E. Risk conditions in children hospitalized with influenza in Norway, 2017–2019. BMC Infect. Dis. 2020, 20, 769. [Google Scholar] [CrossRef]
- Tsankov, B.K.; Allaire, J.M.; Irvine, M.A.; Lopez, A.A.; Sauvé, L.J.; Vallance, B.A.; Jacobson, K. Severe COVID-19 Infection and Pediatric Comorbidities: A Systematic Review and Meta-Analysis. Int. J. Infect. Dis. 2021, 103, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Farrar, D.S.; Drouin, O.; Hepburn, C.M.; Baerg, K.; Chan, K.; Cyr, C.; Donner, E.J.; Embree, J.E.; Farrell, C.; Forgie, S.; et al. Risk factors for severe COVID-19 in hospitalized children in Canada: A national prospective study from March 2020–May 2021. Lancet Reg. Health Am. 2022, 15, 100337. [Google Scholar] [CrossRef] [PubMed]
- Neuzil, K.M.; Mellen, B.G.; Wright, P.F.; Mitchel, E.F.J.; Griffin, M.R. The Effect of Influenza on Hospitalizations, Outpatient Visits, and Courses of Antibiotics in Children. N. Engl. J. Med. 2000, 342, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Demont, C.; Petrica, N.; Bardoulat, I.; Duret, S.; Watier, L.; Chosidow, A.; Lorrot, M.; Kieffer, A.; Lemaitre, M. Economic and disease burden of RSV-associated hospitalizations in young children in France, from 2010 through 2018. BMC Infect. Dis. 2021, 21, 730. [Google Scholar] [CrossRef]
- Zipkin, M. New Vaccine Approaches Present New Possibilities, But New Challenges. Nat. Biopharma Deal. Mak. News Feature 2021. [Google Scholar] [CrossRef]
- Focosi, D. From Co-Administration to Co-Formulation: The Race for New Vaccines against COVID-19 and Other Respiratory Viruses. Vaccines 2023, 11, 109. [Google Scholar] [CrossRef]
- Belshe, R.B.; Newman, F.K.; Anderson, E.L.; Wright, P.F.; Karron, R.A.; Tollefson, S.; Henderson, F.W.; Meissner, H.C.; Madhi, S.; Roberton, D.; et al. Evaluation of Combined Live, Attenuated Respiratory Syncytial Virus and Parainfluenza 3 Virus Vaccines in Infants and Young Children. J. Infect. Dis. 2004, 190, 2096–2103. [Google Scholar] [CrossRef]
- Puig-Barberà, J.; Tormos, A.; Sominina, A.; Burtseva, E.; Launay, O.; Ciblak, M.A.; Natividad-Sancho, A.; Buigues-Vila, A.; Martínez-Úbeda, S.; Mahé, C. First-year results of the Global Influenza Hospital Surveillance Network: 2012–2013 Northern hemisphere influenza season. BMC Public Health 2014, 14, 564. [Google Scholar] [CrossRef]
- Puig-Barberà, J.; Tormos, A.; Trushakova, S.; Sominina, A.; Pisareva, M.; Ciblak, M.A.; Badur, S.; Yu, H.; Cowling, B.J.; Burtseva, E.; et al. The Global Influenza Hospital Surveillance Network (GIHSN): A new platform to describe the epidemiology of severe influenza. Influ. Other Respir. Viruses 2015, 9, 277–286. [Google Scholar] [CrossRef]
- Mira-Iglesias, A.; López-Labrador, F.X.; García-Rubio, J.; Mengual-Chuliá, B.; Tortajada-Girbés, M.; Mollar-Maseres, J.; Carballido-Fernández, M.; Schwarz-Chavarri, G.; Puig-Barberà, J.; Díez-Domingo, J. Influenza Vaccine Effectiveness and Waning Effect in Hospitalized Older Adults. Valencia Region, Spain, 2018/2019 Season. Int. J. Environ. Res. Public Health 2021, 18, 1129. [Google Scholar] [CrossRef]
- Mira-Iglesias, A.; López-Labrador, F.X.; Baselga-Moreno, V.; Tortajada-Girbés, M.; Mollar-Maseres, J.; Carballido-Fernández, M.; Schwarz-Chavarri, G.; Puig-Barberà, J.; Díez-Domingo, J. Influenza vaccine effectiveness against laboratory-confirmed influenza in hospitalised adults aged 60 years or older, Valencia Region, Spain, 2017/18 influenza season. Euro Surveill. 2019, 24. [Google Scholar] [CrossRef] [PubMed]
- Mira-Iglesias, A.; López-Labrador, F.X.; Guglieri-López, B.; Tortajada-Girbés, M.; Baselga-Moreno, V.; Cano, L.; Mollar-Maseres, J.; Carballido-Fernández, M.; Schwarz-Chavarri, G.; Díez-Domingo, J.; et al. Influenza vaccine effectiveness in preventing hospitalisa-tion of individuals 60 years of age and over with laboratory-confirmed influenza, Valencia Region, Spain, influenza season 2016/17. Euro Surveill 2018, 23. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R.; Rybak, A.; Werner, A.; Béchet, S.; Desandes, R.; Hassid, F.; André, J.M.; Gelbert, N.; Thiebault, G.; Kochert, F.; et al. Trends in pediatric ambulatory community acquired infections before and during COVID-19 pandemic: A prospective multicentric sur-veillance study in France. Lancet Reg. Health Eur. 2022, 22, 100497. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.E.; Park, S.W.; Yang, W.; Vecchi, G.A.; Metcalf, C.J.E.; Grenfell, B.T. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc. Natl. Acad. Sci. USA 2020, 117, 30547–30553. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Commission Implementing Decision (EU) 2018/945 of 22 June 2018 on the Communicable Diseases and Related Health Issues to Be Covered by Epidemiological Surveillance As Well As Relevant Case Definitions; European Centre for Disease Prevention and Control: Solna, Sweden, 2018; Volume 1–74, Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32018D0945 (accessed on 1 July 2024).
- Thompson, M.G.; Levine, M.Z.; Bino, S.; Hunt, D.R.; Al-Sanouri, T.M.; Simões, E.A.F.; Porter, R.M.; Biggs, H.M.; Gresh, L.; Simaku, A.; et al. Underdetection of laboratory-confirmed influenza-associated hospital admissions among infants: A multicentre, prospective study. Lancet Child Adolesc. Health 2019, 3, 781–794. [Google Scholar] [CrossRef] [PubMed]
- Norman, D.A.; Cheng, A.C.; Macartney, K.K.; Moore, H.C.; Danchin, M.; Seale, H.; McRae, J.; Clark, J.E.; Marshall, H.S.; Buttery, J.; et al. Influenza hospitalizations in Australian children 2010-2019: The impact of medical comorbidities on outcomes, vaccine coverage, and effectiveness. Influenza Other Respir Viruses 2022, 16, 316–327. [Google Scholar] [CrossRef]
- Sarna, M.; Lambert, S.B.; Sloots, T.P.; Whiley, D.M.; Alsaleh, A.; Mhango, L.; Bialasiewicz, S.; Wang, D.; Nissen, M.D.; Grimwood, K.; et al. Viruses causing lower respiratory symptoms in young children: Findings from the ORChID birth cohort. Thorax 2017, 73, 969–979. [Google Scholar] [CrossRef]
- Le Corre, N.; Pérez, R.; Vizcaya, C.; Martínez-Valdebenito, C.; López, T.; Monge, M.; Alarcón, R.; Moller, F.; Martínez, M.T.; Massardo, J.M.; et al. Relevance of codetection of respiratory viruses in the severity of acute respiratory infection in hospitalized children. Andes Pediatr. 2021, 92, 349–357. [Google Scholar] [CrossRef]
- Agathis, N.T.; Patel, K.; Milucky, J.; Taylor, C.A.; Whitaker, M.; Pham, H.; Anglin, O.; Chai, S.J.; Alden, N.B.; Meek, J.; et al. Codetections of Other Respiratory Viruses Among Children Hospitalized with COVID-19. Pediatrics 2023, 151. [Google Scholar] [CrossRef]
- Lin, G.-L.; Drysdale, S.; Snape, M.; O’Connor, D.; Brown, A.; MacIntyre-Cockett, G.; Mellado-Gomez, E.; de Cesare, M.; Ansari, A.; Bonsall, D.; et al. Association between disease severity and co-detection of respiratory pathogens in infants with RSV infection. medRxiv 2023. [Google Scholar] [CrossRef]
- Samson, L.; Cooke, C.; MacDonald, N. Analysis of antibiotic use and misuse in children hospitalized with RSV infection. Paediatr. Child Health 1999, 4, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Van Houten, C.B.; Cohen, A.; Engelhard, D.; Hays, J.P.; Karlsson, R.; Moore, E.; Fernández, D.; Kreisberg, R.; Collins, L.V.; de Waal, W.; et al. Antibiotic misuse in respiratory tract infections in children and adults—A prospective, multicentre study (TAILORED Treatment). Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Han, S.B.; Shin, J.A.; Kim, S.K.; Lee, J.W.; Lee, D.-G.; Chung, N.-G.; Cho, B.; Jeong, D.C.; Kang, J.H. Respiratory viral infections in children and adolescents with hematological malignancies. Mediterr. J. Hematol. Infect. Dis. 2019, 11, e2019006. [Google Scholar] [CrossRef] [PubMed]
- Britton, P.N.; Jones, C.A.; Macartney, K.; Cheng, A.C. Parechovirus: An important emerging infection in young infants. Med. J. Aust. 2018, 208, 365–369. [Google Scholar] [CrossRef]
- Shah, M.M.; Perez, A.; Lively, J.Y.; Avadhanula, V.; Boom, J.A.; Chappell, J.; Englund, J.A.; Fregoe, W.; Halasa, N.B.; Harrison, C.J.; et al. Enterovirus D68-Associated Acute Respiratory Illness—New Vaccine Surveillance Network, United States, July–November 2018–2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1623–1628. [Google Scholar] [CrossRef]
- Monto, A.S. The seasonality of rhinovirus infections and its implications for clinical recognition. Clin. Ther. 2002, 24, 1987–1997. [Google Scholar] [CrossRef]
- Pons-Salort, M.; Oberste, M.S.; Pallansch, M.A.; Abedi, G.R.; Takahashi, S.; Grenfell, B.T.; Grassly, N.C. The seasonality of nonpolio enteroviruses in the United States: Patterns and drivers. Proc. Natl. Acad. Sci. USA 2018, 115, 3078–3083. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control; World Health Organization. Operational Considerations for Respiratory Virus Surveillance in Europe, 18 July 2022. WHO/EURO:2022-5841-45606-65427. 2022. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2022-5841-45606-65427 (accessed on 1 July 2024).
- Fiore, A.E.; Uyeki, T.M.; Broder, K.; Finelli, L.; Euler, G.L.; Singleton, J.A.; Iskander, J.K.; Wortley, P.M.; Shay, D.K.; Bresee, J.S.; et al. Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm. Rep. 2010, 59, 1–62. [Google Scholar]
- Mak, T.K.; Mangtani, P.; Leese, J.; Watson, J.M.; Pfeifer, D. Influenza vaccination in pregnancy: Current evidence and selected national policies. Lancet Infect. Dis. 2008, 8, 44–52. [Google Scholar] [CrossRef]
- Morales, K.F.; Brown, D.W.; Dumolard, L.; Steulet, C.; Vilajeliu, A.; Alvarez, A.M.R.; Moen, A.; Friede, M.; Lambach, P. Seasonal influenza vaccination policies in the 194 WHO Member States: The evolution of global influenza pandemic preparedness and the challenge of sustaining equitable vaccine access. Vaccine X 2021, 8, 100097. [Google Scholar] [CrossRef]
- Cohen, S.A.; Chui, K.K.; Naumova, E.N. Influenza Vaccination in Young Children Reduces Influenza-Associated Hospitalizations in Older Adults, 2002–2006. J. Am. Geriatr. Soc. 2011, 59, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Dbaibo, G.; Amanullah, A.; Claeys, C.; Izu, A.; Jain, V.K.; Kosalaraksa, P.; Rivera, L.; Soni, J.; Yanni, E.; Zaman, K.; et al. Quadrivalent Influenza Vaccine Prevents Illness and Reduces Healthcare Utilization Across Diverse Geographic Regions During Five Influenza Seasons: A Randomized Clinical Trial. Pediatr. Infect Dis. J. 2020, 39, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- King, J.C.J.; Stoddard, J.J.; Gaglani, M.J.; Moore, K.A.; Magder, L.; McClure, E.; Rubin, J.D.; Englund, J.A.; Neuzil, K. Effectiveness of School-Based Influenza Vaccination. N. Engl. J. Med. 2006, 355, 2523–2532. [Google Scholar] [CrossRef] [PubMed]
- Gantenberg, J.R.; van Aalst, R.; Zimmerman, N.; Limone, B.; Chaves, S.S.; La Via, W.V.; Nelson, C.B.; Rizzo, C.; Savitz, D.A.; Zullo, A.R. Medically Attended Illness due to Respiratory Syncytial Virus Infection Among Infants Born in the United States Between 2016 and 2020. J. Infect. Dis. 2022, 226 (Suppl. S2), S164–S174. [Google Scholar] [CrossRef] [PubMed]
- Wildenbeest, J.G.; Billard, M.-N.; Zuurbier, R.P.; Korsten, K.; Langedijk, A.C.; van de Ven, P.M.; Snape, M.D.; Drysdale, S.B.; Pollard, A.J.; Robinson, H.; et al. The burden of respiratory syncytial virus in healthy term-born infants in Europe: A prospective birth cohort study. Lancet Respir. Med. 2022, 11, 341–353. [Google Scholar] [CrossRef]
- Domachowske, J.B.; Anderson, E.J.; Goldstein, M. The Future of Respiratory Syncytial Virus Disease Prevention and Treatment. Infect. Dis. Ther. 2021, 10 (Suppl. S1), 47–60. [Google Scholar] [CrossRef]
- Mazur, N.I.; Terstappen, J.; Baral, R.; Bardají, A.; Beutels, P.; Buchholz, U.J.; Cohen, C.; Crowe, J.E.; Cutland, C.L.; Eckert, L.; et al. Respiratory syncytial virus prevention within reach: The vaccine and monoclonal antibody landscape. Lancet Infect. Dis. 2023, in press. [Google Scholar] [CrossRef]
- Hammitt, L.L.; Dagan, R.; Yuan, Y.; Cots, M.B.; Bosheva, M.; Madhi, S.A.; Muller, W.J.; Zar, H.J.; Brooks, D.; Grenham, A.; et al. Nirsevimab for Prevention of RSV in Healthy Late-Preterm and Term Infants. N. Engl. J. Med. 2022, 386, 837–846. [Google Scholar] [CrossRef]
- Griffin, M.P.; Yuan, Y.; Takas, T.; Domachowske, J.B.; Madhi, S.A.; Manzoni, P.; Simões, E.A.F.; Esser, M.T.; Khan, A.A.; Dubovsky, F.; et al. Single-Dose Nirsevimab for Prevention of RSV in Preterm Infants. N. Engl. J. Med. 2020, 383, 415–425. [Google Scholar] [CrossRef]
- Simões, E.A.F.; Madhi, S.A.; Muller, W.J.; Atanasova, V.; Bosheva, M.; Cabañas, F.; Cots, M.B.; Domachowske, J.B.; Garcia-Garcia, M.L.; Grantina, I.; et al. Efficacy of nirsevimab against respiratory syncytial virus lower respiratory tract infections in preterm and term infants, and pharmacokinetic extrapolation to infants with congenital heart disease and chronic lung disease: A pooled analysis of randomised controlled trials. Lancet Child Adolesc. Health 2023, 7, 180–189. [Google Scholar] [CrossRef]
- Aliprantis, A.O.; Wolford, D.; Caro, L.; Maas, B.M.; Ma, H.; Montgomery, D.L.; Sterling, L.M.; Hunt, A.; Cox, K.S.; Vora, K.A.; et al. A Phase 1 Randomized, Double-Blind, Placebo-Controlled Trial to Assess the Safety, Tolerability, and Pharmacokinetics of a Respiratory Syncytial Virus Neutralizing Monoclonal Antibody MK-1654 in Healthy Adults. Clin. Pharmacol. Drug Dev. 2021, 10, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Sah, P.; Vilches, T.N.; Pandey, A.; Schneider, E.C.; Moghadas, S.M.; Galvani, A.P. Estimating the impact of vaccination on reducing COVID-19 burden in the United States: December 2020 to March 2022. J. Glob. Health 2022, 12, 03062. [Google Scholar] [CrossRef] [PubMed]
- Dawood, F.S.; Chaves, S.S.; Pérez, A.; Reingold, A.; Meek, J.; Farley, M.M.; Ryan, P.; Lynfield, R.; Morin, C.; Baumbach, J.; et al. Emerging Infections Program Network. Complications and Associated Bacterial Coinfections Among Children Hospitalized with Seasonal or Pandemic Influenza, United States, 2003–2010. J. Infect. Dis. 2014, 209, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Reed, C.; Chaves, S.S.; Perez, A.; D’Mello, T.; Kirley, P.D.; Aragon, D.; Meek, J.I.; Farley, M.M.; Ryan, P.; Lynfield, R.; et al. Complications Among Adults Hospitalized with Influenza: A Comparison of Seasonal Influenza and the 2009 H1N1 Pandemic. Clin. Infect. Dis. 2014, 59, 166–174. [Google Scholar] [CrossRef]


| Total (N = 6069) | ||
|---|---|---|
| Characteristic | n | % |
| Age group a | ||
| <6 months of age | 2363 | 38.9 |
| 6 to 11 months of age | 677 | 11.1 |
| 1 to 4 years of age | 2339 | 38.5 |
| 5 to 17 years of age | 690 | 11.4 |
| Sex | ||
| Male | 3447 | 56.8 |
| Female | 2622 | 43.2 |
| Ratio Male/Female | 1.3 | |
| Number of comorbidities at admission | ||
| None | 4469 | 73.6 |
| At least one | 1600 | 26.4 |
| One | 1315 | 21.7 |
| Two or more | 285 | 4.7 |
| Comorbidities | ||
| Prematurity | 634 | 10.5 |
| Lung disease | 535 | 8.8 |
| Recurrent wheezing/asthma | 283 | 4.7 |
| Heart disease | 155 | 2.5 |
| Anemia | 125 | 2.1 |
| Neurological/neuromuscular diseases | 84 | 1.4 |
| Chronic renal disease | 53 | 0.9 |
| Chronic autoimmune disease | 24 | 0.4 |
| Endocrine system disease other than diabetes | 21 | 0.4 |
| Diabetes | 17 | 0.3 |
| Chronic liver disease | 9 | 0.2 |
| Neoplastic disease | 8 | 0.1 |
| Total (N = 6069) | Otherwise Healthy (N = 4469) | With at Least 1 Comorbidity (N = 1600) | ||||
|---|---|---|---|---|---|---|
| Severity | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) |
| Intensive care admission | 78 | 1.3 (1.0; 1.6) | 44 | 1.0 (0.7; 1.3) | 34 | 2.3 (1.5; 3.0) |
| Mechanical ventilation a | 21 | 0.6 (0.3; 0.9) | 12 | 0.4 (0.2; 0.7) | 9 | 1.0 (0.5; 1.9) |
| Length of hospital stay (in days) | ||||||
| Median | 4 | 4 | 4 | |||
| Q1; Q3 | 3; 6 | 3; 6 | 2; 6 | |||
| Total a (N = 6069) | Pathogens Identified through ICD Codes as Part of Patient’s Discharge | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| RSV (N = 1093) | Influenza (N = 246) | Rotavirus (N = 66) | Streptococcus Pneumonia (N = 40) | Hemophilus Influenzae (N = 34) | Epstein-Barr Virus (N = 22) | Escherichia coli (N = 22) | Streptococcus (N = 17) | Other Pathogens b (N = 68) | No Pathogens (N = 4505) | ||
| RT-PCR Viral Panel | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| No virus detected | 2790 (46.0) | 295 (27.0) | 37 (15.0) | 53 (80.3) | 27 (67.5) | 14 (41.2) | 15 (68.2) | 16 (72.6) | 10 (58.8) | 47 (69.1) | 2290 (50.8) |
| Influenza c | 437 (7.2) | 8 (0.7) | 185 (75.2) | 1 (1.5) | 0 (0) | 4 (11.8) | 4 (18.2) | 0 (0) | 2 (11.8) | 4 (5.9) | 239 (5.3) |
| Respiratory syncytial virus | 1402 (23.1) | 644 (58.9) | 4 (1.6) | 0 (0) | 9 (22.5) | 8 (23.5) | 1 (4.5) | 0 (0) | 2 (11.8) | 6 (8.8) | 742 (16.5) |
| Human metapneumovirus | 116 (1.9) | 3 (0.3) | 2 (0.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 111 (2.5) |
| Parainfluenza | 39 (0.6) | 0 (0) | 0 (0) | 1 (1.5) | 0 (0) | 1 (2.9) | 0 (0) | 0 (0) | 0 (0) | 2 (2.9) | 36 (0.8) |
| Rhinovirus/enterovirus | 579 (9.5) | 28 (2.6) | 6 (2.4) | 1 (1.5) | 3 (7.5) | 2 (5.9) | 1 (4.5) | 0 (0) | 0 (0) | 2 (2.9) | 536 (11.9) |
| Adenovirus | 95 (1.6) | 5 (0.5) | 0 (0) | 5 (7.6) | 1 (2.5) | 0 (0) | 0 (0) | 1 (4.5) | 0 (0) | 1 (1.5) | 86 (1.9) |
| Human coronavirus | 197 (3.2) | 18 (1.6) | 0 (0) | 0 (0) | 0 (0) | 2 (5.9) | 0 (0) | 3 (13.6) | 1 (5.9 | 4 (5.9) | 165 (3.7) |
| Bocavirus | 110 (1.8) | 9 (0.8) | 3 (1.2) | 2 (3) | 0 (0) | 1 (2.9) | 0 (0) | 1 (4.5) | 1 (5.9) | 0 (0) | 95 (2.1) |
| Codetection | 281 (4.6) | 78 (7.1) | 9 (3.7) | 0 (0) | 0 (0) | 2 (5.9) | 1 (4.5) | 0 (0) | 1 (5.9) | 2 (2.9) | 188 (4.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bosch Castells, V.; Mira-Iglesias, A.; López-Labrador, F.X.; Mengual-Chuliá, B.; Carballido-Fernández, M.; Tortajada-Girbés, M.; Mollar-Maseres, J.; Puig-Barberà, J.; Díez-Domingo, J.; Chaves, S.S. Pediatric Respiratory Hospitalizations in the Pre-COVID-19 Era: The Contribution of Viral Pathogens and Comorbidities to Clinical Outcomes, Valencia, Spain. Viruses 2024, 16, 1519. https://doi.org/10.3390/v16101519
Bosch Castells V, Mira-Iglesias A, López-Labrador FX, Mengual-Chuliá B, Carballido-Fernández M, Tortajada-Girbés M, Mollar-Maseres J, Puig-Barberà J, Díez-Domingo J, Chaves SS. Pediatric Respiratory Hospitalizations in the Pre-COVID-19 Era: The Contribution of Viral Pathogens and Comorbidities to Clinical Outcomes, Valencia, Spain. Viruses. 2024; 16(10):1519. https://doi.org/10.3390/v16101519
Chicago/Turabian StyleBosch Castells, Valérie, Ainara Mira-Iglesias, Francisco Xavier López-Labrador, Beatriz Mengual-Chuliá, Mario Carballido-Fernández, Miguel Tortajada-Girbés, Joan Mollar-Maseres, Joan Puig-Barberà, Javier Díez-Domingo, and Sandra S. Chaves. 2024. "Pediatric Respiratory Hospitalizations in the Pre-COVID-19 Era: The Contribution of Viral Pathogens and Comorbidities to Clinical Outcomes, Valencia, Spain" Viruses 16, no. 10: 1519. https://doi.org/10.3390/v16101519
APA StyleBosch Castells, V., Mira-Iglesias, A., López-Labrador, F. X., Mengual-Chuliá, B., Carballido-Fernández, M., Tortajada-Girbés, M., Mollar-Maseres, J., Puig-Barberà, J., Díez-Domingo, J., & Chaves, S. S. (2024). Pediatric Respiratory Hospitalizations in the Pre-COVID-19 Era: The Contribution of Viral Pathogens and Comorbidities to Clinical Outcomes, Valencia, Spain. Viruses, 16(10), 1519. https://doi.org/10.3390/v16101519






