Comparison of Dual Monoclonal Antibody Therapies for COVID-19 Evolution: A Multicentric Retrospective Study †
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Viral Load, Variant Identification, and SARS-CoV-2 Spike Gene Sequencing
2.3. Data Management
2.4. Data Analysis
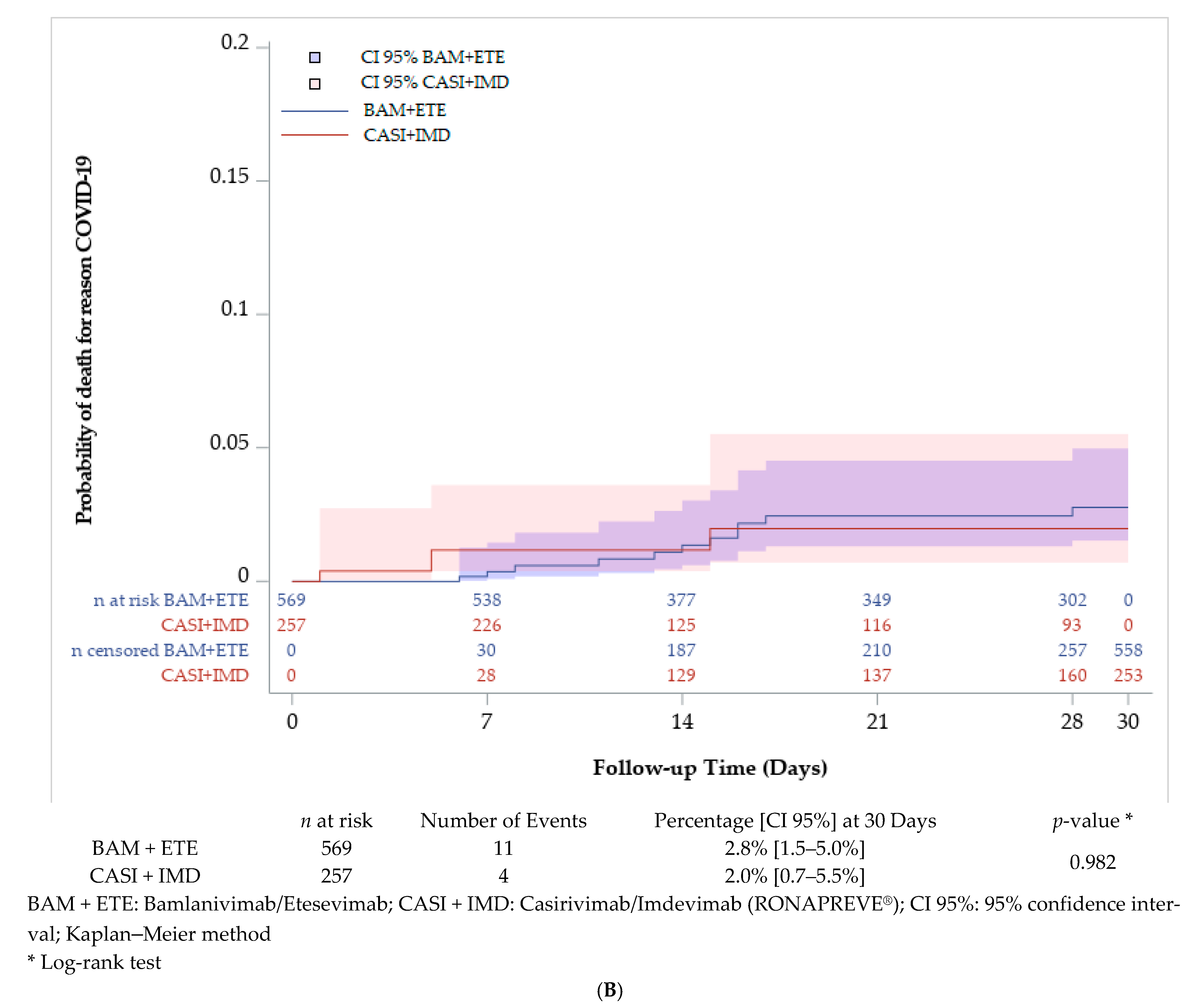
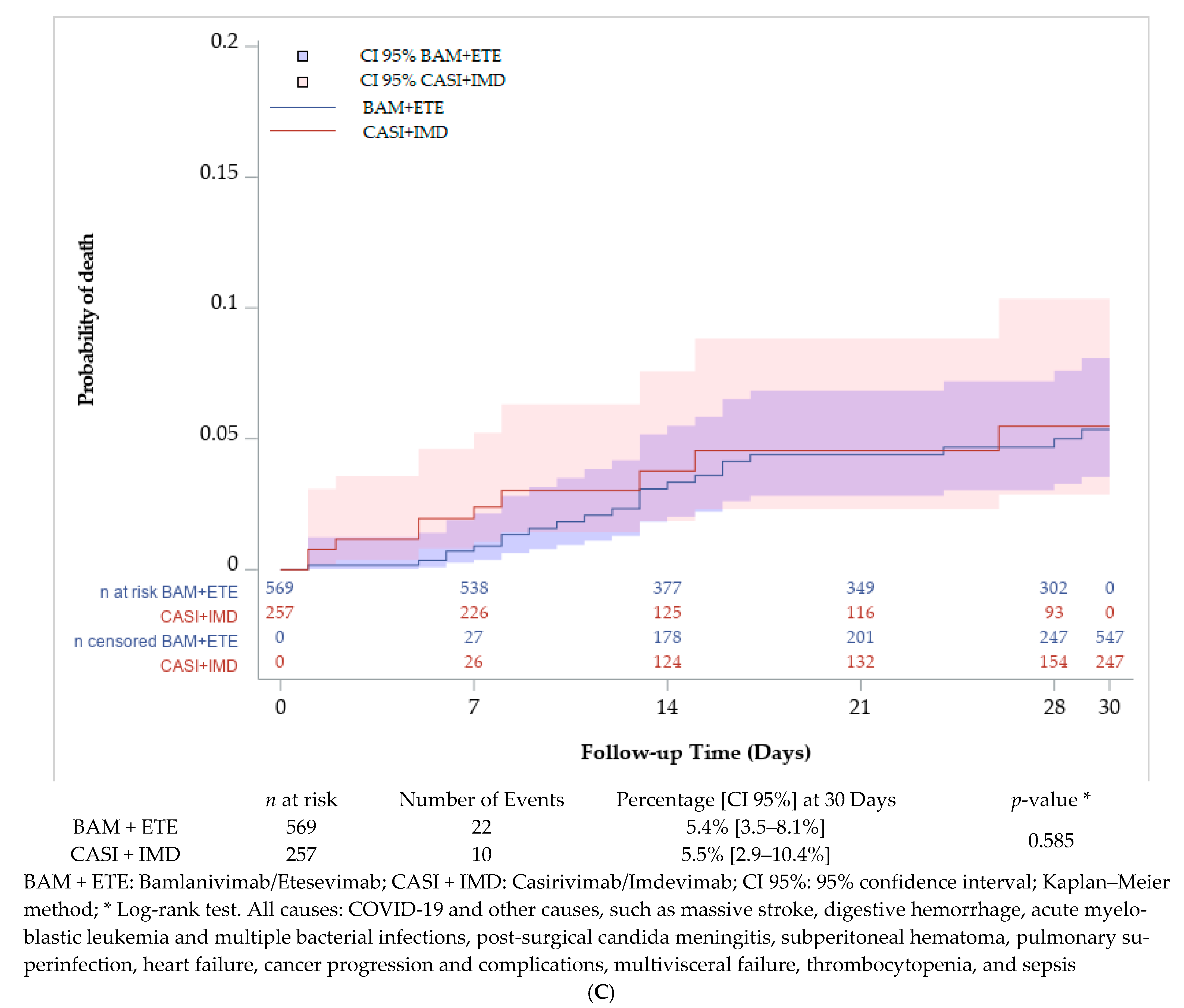
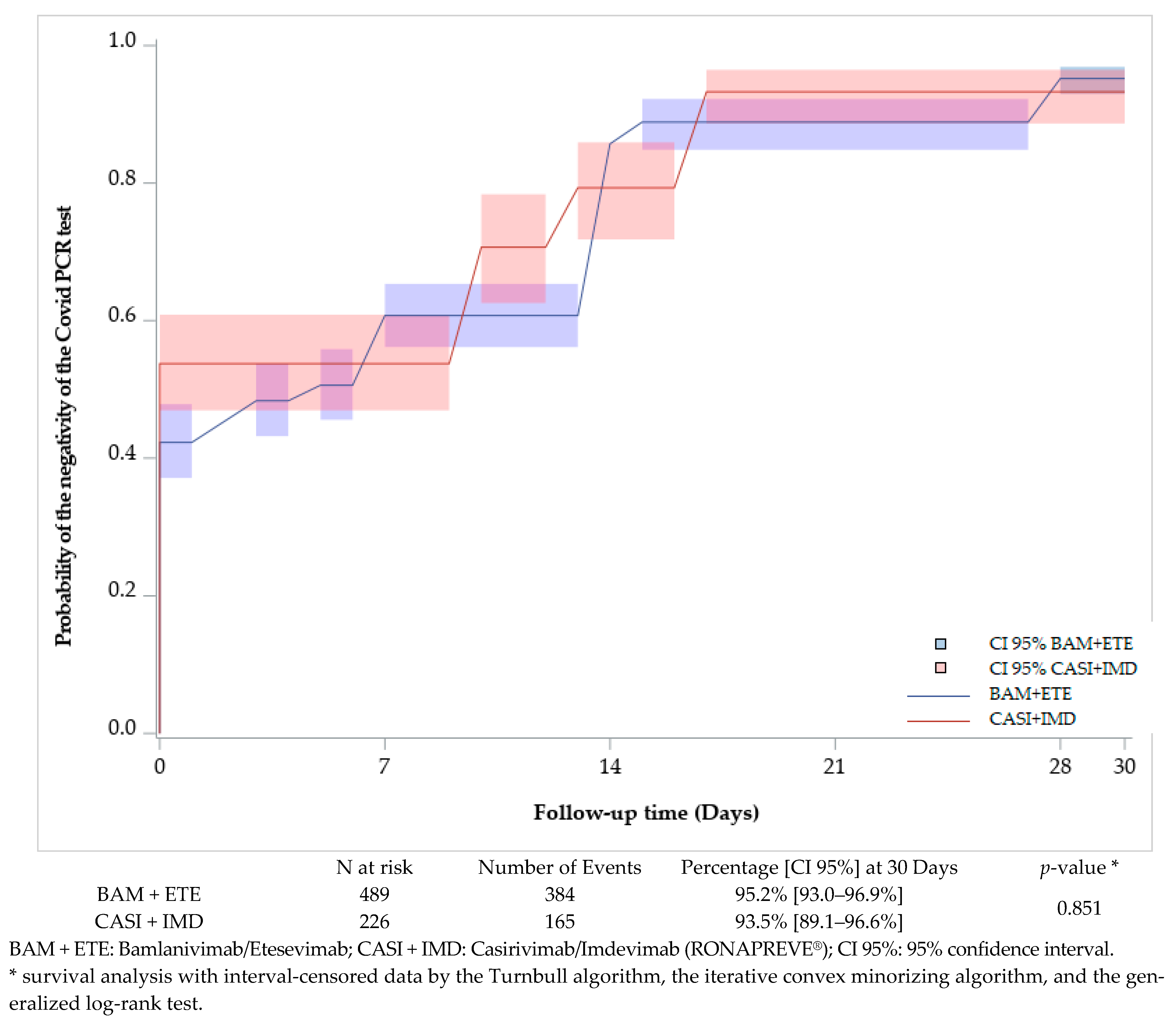
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Focosi, D.; McConnell, S.; Casadevall, A.; Cappello, E.; Valdiserra, G.; Tuccori, M. Monoclonal Antibody Therapies against SARS-CoV-2. Lancet Infect. Dis. 2022, 22, e311–e326. [Google Scholar] [CrossRef] [PubMed]
- Dougan, M.; Nirula, A.; Azizad, M.; Mocherla, B.; Gottlieb, R.L.; Chen, P.; Hebert, C.; Perry, R.; Boscia, J.; Heller, B.; et al. Bamlanivimab plus Etesevimab in Mild or Moderate COVID-19. N. Engl. J. Med. 2021, 385, 1382–1392. [Google Scholar] [CrossRef] [PubMed]
- Dougan, M.; Azizad, M.; Mocherla, B.; Gottlieb, R.L.; Chen, P.; Hebert, C.; Perry, R.; Boscia, J.; Heller, B.; Morris, J.; et al. A Randomized, Placebo-Controlled Clinical Trial of Bamlanivimab and Etesevimab Together in High-Risk Ambulatory Patients With COVID-19 and Validation of the Prognostic Value of Persistently High Viral Load. Clin. Infect. Dis. 2022, 75, e440–e449. [Google Scholar] [CrossRef] [PubMed]
- Abani, O.; Abani, O.; Abbas, A.; Abbas, A.; Abbas, F.; Abbas, F.; Abbas, M.; Abbas, M.; Abbasi, S.; Abbasi, S.; et al. Casirivimab and Imdevimab in Patients Admitted to Hospital with COVID-19 (RECOVERY): A Randomised, Controlled, Open-Label, Platform Trial. Lancet 2022, 399, 665–676. [Google Scholar] [CrossRef]
- Weinreich, D.M.; Sivapalasingam, S.; Norton, T.; Ali, S.; Gao, H.; Bhore, R.; Xiao, J.; Hooper, A.T.; Hamilton, J.D.; Musser, B.J.; et al. REGEN-COV Antibody Combination and Outcomes in Outpatients with COVID-19. N. Engl. J. Med. 2021, 385, e81. [Google Scholar] [CrossRef]
- Dutta, D.; Naiyer, S.; Mansuri, S.; Soni, N.; Singh, V.; Bhat, K.H.; Singh, N.; Arora, G.; Mansuri, M.S. COVID-19 Diagnosis: A Comprehensive Review of the RT-qPCR Method for Detection of SARS-CoV-2. Diagnostics 2022, 12, 1503. [Google Scholar] [CrossRef] [PubMed]
- Leducq, V.; Zafilaza, K.; Fauchois, A.; Ghidaoui, E.; Sayon, S.; Dorival, C.; Meledje, M.-L.; Lusivika-Nzinga, C.; Yordanov, Y.; Martin-Blondel, G.; et al. Spike Protein Genetic Evolution in Patients at High Risk of Severe Coronavirus Disease 2019 Treated by Monoclonal Antibodies. J. Infect. Dis. 2023, 229, 1341–1351. [Google Scholar] [CrossRef]
- Laurini, E.; Marson, D.; Aulic, S.; Fermeglia, A.; Pricl, S. Molecular Rationale for SARS-CoV-2 Spike Circulating Mutations Able to Escape Bamlanivimab and Etesevimab Monoclonal Antibodies. Sci. Rep. 2021, 11, 20274. [Google Scholar] [CrossRef] [PubMed]
- Peiffer-Smadja, N.; Bridier-Nahmias, A.; Ferré, V.M.; Charpentier, C.; Garé, M.; Rioux, C.; Allemand, A.; Lavallée, P.; Ghosn, J.; Kramer, L.; et al. Emergence of E484K Mutation Following Bamlanivimab Monotherapy among High-Risk Patients Infected with the Alpha Variant of SARS-CoV-2. Viruses 2021, 13, 1642. [Google Scholar] [CrossRef]
- Lohr, B.; Niemann, D.; Verheyen, J. Bamlanivimab Treatment Leads to Rapid Selection of Immune Escape Variant Carrying the E484K Mutation in a B.1.1.7-Infected and Immunosuppressed Patient. Clin. Infect. Dis. 2021, 73, 2144–2145. [Google Scholar] [CrossRef]
- Focosi, D.; Novazzi, F.; Genoni, A.; Dentali, F.; Gasperina, D.D.; Baj, A.; Maggi, F. Emergence of SARS-CoV-2 Spike Protein Escape Mutation Q493R after Treatment for COVID-19. Emerg. Infect. Dis. 2021, 27, 2728–2731. [Google Scholar] [CrossRef] [PubMed]
- Jensen, B.; Luebke, N.; Feldt, T.; Keitel, V.; Brandenburger, T.; Kindgen-Milles, D.; Lutterbeck, M.; Freise, N.F.; Schoeler, D.; Haas, R.; et al. Emergence of the E484K Mutation in SARS-CoV-2-Infected Immunocompromised Patients Treated with Bamlanivimab in Germany. Lancet Reg. Health Eur. 2021, 8, 100164. [Google Scholar] [CrossRef] [PubMed]
- Guigon, A.; Faure, E.; Lemaire, C.; Chopin, M.-C.; Tinez, C.; Assaf, A.; Lazrek, M.; Hober, D.; Bocket, L.; Engelmann, I.; et al. Emergence of Q493R Mutation in SARS-CoV-2 Spike Protein during Bamlanivimab/Etesevimab Treatment and Resistance to Viral Clearance. J. Infect. 2022, 84, 248–288. [Google Scholar] [CrossRef]
- Kim, Y.; Gaudreault, N.N.; Meekins, D.A.; Perera, K.D.; Bold, D.; Trujillo, J.D.; Morozov, I.; McDowell, C.D.; Chang, K.-O.; Richt, J.A. Effects of Spike Mutations in SARS-CoV-2 Variants of Concern on Human or Animal ACE2-Mediated Virus Entry and Neutralization. Microbiol. Spectr. 2022, 10, e01789-21. [Google Scholar] [CrossRef]
- Li, Q.; Nie, J.; Wu, J.; Zhang, L.; Ding, R.; Wang, H.; Zhang, Y.; Li, T.; Liu, S.; Zhang, M.; et al. SARS-CoV-2 501Y.V2 Variants Lack Higher Infectivity but Do Have Immune Escape. Cell 2021, 184, 2362–2371.e9. [Google Scholar] [CrossRef] [PubMed]
- Jangra, S.; Ye, C.; Rathnasinghe, R.; Stadlbauer, D.; Personalized Virology Initiative study group; Krammer, F.; Simon, V.; Martinez-Sobrido, L.; García-Sastre, A.; Schotsaert, M. SARS-CoV-2 Spike E484K Mutation Reduces Antibody Neutralisation. Lancet Microbe 2021, 2, e283–e284. [Google Scholar] [CrossRef]
- Chen, P.; Nirula, A.; Heller, B.; Gottlieb, R.L.; Boscia, J.; Morris, J.; Huhn, G.; Cardona, J.; Mocherla, B.; Stosor, V.; et al. SARS-CoV-2 Neutralizing Antibody LY-CoV555 in Outpatients with COVID-19. N. Engl. J. Med. 2021, 384, 229–237. [Google Scholar] [CrossRef]
- Balasundaram, P.; Morgan-Joseph, T. Etesevimab. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Mader, A.-L.; Tydykov, L.; Glück, V.; Bertok, M.; Weidlich, T.; Gottwald, C.; Stefl, A.; Vogel, M.; Plentz, A.; Köstler, J.; et al. Omicron’s Binding to Sotrovimab, Casirivimab, Imdevimab, CR3022, and Sera from Previously Infected or Vaccinated Individuals. iScience 2022, 25, 104076. [Google Scholar] [CrossRef]
- Weinreich, D.M.; Sivapalasingam, S.; Norton, T.; Ali, S.; Gao, H.; Bhore, R.; Musser, B.J.; Soo, Y.; Rofail, D.; Im, J.; et al. REGN-COV2, a Neutralizing Antibody Cocktail, in Outpatients with COVID-19. N. Engl. J. Med. 2021, 384, 238–251. [Google Scholar] [CrossRef]
- Jary, A.; Marot, S.; Faycal, A.; Leon, S.; Sayon, S.; Zafilaza, K.; Ghidaoui, E.; Quoc, S.N.; Nemlaghi, S.; Choquet, S.; et al. Spike Gene Evolution and Immune Escape Mutations in Patients with Mild or Moderate Forms of COVID-19 and Treated with Monoclonal Antibodies Therapies. Viruses 2022, 14, 226. [Google Scholar] [CrossRef]
- Gupta, A.; Konnova, A.; Smet, M.; Berkell, M.; Savoldi, A.; Morra, M.; Averbeke, V.V.; Winter, F.H.R.D.; Peserico, D.; Danese, E.; et al. Host Immunological Responses Facilitate Development of SARS-CoV-2 Mutations in Patients Receiving Monoclonal Antibody Treatments. J. Clin. Investig. 2023, 133, e166032. [Google Scholar] [CrossRef]
- Focosi, D.; McConnell, S.; Sullivan, D.J.; Casadevall, A. Analysis of SARS-CoV-2 Mutations Associated with Resistance to Therapeutic Monoclonal Antibodies That Emerge after Treatment. Drug Resist. Updates 2023, 71, 100991. [Google Scholar] [CrossRef] [PubMed]
- Bruel, T.; Vrignaud, L.-L.; Porrot, F.; Staropoli, I.; Planas, D.; Guivel-Benhassine, F.; Puech, J.; Prot, M.; Munier, S.; Bolland, W.H.; et al. Sotrovimab Therapy Elicits Antiviral Activities against Omicron BQ.1.1 and XBB.1.5 in Sera of Immunocompromised Patients. Med 2023, 4, 664–667. [Google Scholar] [CrossRef] [PubMed]
- Traitement par Paxlovid® des patients à risque de Forme Grave de COVID-19. Available online: https://www.has-sante.fr/jcms/p_3310993/fr/traitement-par-paxlovid-des-patients-a-risque-de-forme-grave-de-covid-19 (accessed on 9 November 2022).

| Characteristics before Monoclonal Antibody Treatment | All n = 1004 | Dual Therapy Bamlanivimab+ Etesevimab n = 691 | Dual Therapy Casirivimab+ Imdevimab (RONAPREVE®) n = 313 | p-Value |
|---|---|---|---|---|
| Age categories, n (%) | 0.116 | |||
| - Under 60 years old | 287 (28.6) | 184 (26.6) | 103 (32.9) | |
| - between 60 and 80 years old | 405 (40.3) | 284 (41.1) | 121 (38.7) | |
| - 80 years and more | 312 (31.1) | 223 (32.3) | 89 (28.4) | |
| Sex, n (%) | 0.748 | |||
| - Female | 524 (52.2) | 363 (52.5) | 161 (51.4) | |
| - Male | 480 (47.8) | 328 (47.5) | 152 (48.6) | |
| Weight, kg, median (IQR) | 73 (61–84) | 73 (61–84) | 71 (61–85) | 0.341 |
| Form of the COVID-19, n (%) | 0.577 | |||
| - Mild | 853 (85.0) | 590 (85.4) | 263 (84.0) | |
| - Moderated | 151 (15.0) | 101 (14.6) | 50 (16.0) | |
| Immune deficiency related to a pathology or treatments, n (%) | <0.001 | |||
| - Yes | 545 (54.3) | 339 (49.1) | 206 (65.8) | |
| - No | 459 (45.7) | 352 (50.9) | 107 (34.2) | |
| Chemotherapy on-going, n (%) | 185 (18.4) | 119 (17.2) | 66 (21.1) | 0.143 |
| Solid organ transplantation, n (%) | 150 (14.9) | 87 (12.6) | 63 (20.1) | 0.002 |
| Immunosuppressive treatments *, n (%) | 150 (14.9) | 101 (14.6) | 49 (15.7) | 0.669 |
| Corticosteroid treatment > 10 mg/day prednisone equivalent for more than 2 weeks, n (%) | 67 (6.7) | 47 (6.8) | 20 (6.4) | 0.809 |
| Systemic lupus or vasculitis with immunosuppressive therapy, n (%) | 20 (2.0) | 13 (1.9) | 7 (2.2) | 0.709 |
| Patients with comorbidities, n (%) | <0.001 | |||
| - Yes | 304 (30.3) | 251 (36.3) | 53 (16.9) | |
| - No | 700 (69.7) | 440 (63.7) | 260 (83.1) | |
| Idiopathic pulmonary fibrosis, n (%) | 6 (0.6) | 3 (0.4) | 3 (1.0) | 0.383 |
| Myopathy with a forced vital capacity, n (%) | 3 (0.3) | 2 (3.0) | 1 (0.3) | 1.000 |
| Amyotrophic lateral sclerosis, n (%) | 5 (0.5) | 5 (0.7) | 0 (0.0) | 0.332 |
| Trisomy 21, n (%) | 3 (0.3) | 3 (0.4) | 0 (0.0) | 0.556 |
| Rare liver diseases including autoimmune hepatitis, n (%) | 11 (1.1) | 7 (1.0) | 4 (1.3) | 0.747 |
| Other rare diseases defined by the FSMR, n (%) | 23 (2.3) | 14 (2.0) | 9 (2.9) | 0.405 |
| Obesity, n (%) | 102 (10.2) | 85 (12.3) | 17 (5.4) | <0.001 |
| Diabetes, n (%) | 120 (12.0) | 102 (14.8) | 18 (5.8) | <0.001 |
| Heart failure, n (%) | 65 (6.5) | 57 (8.2) | 8 (2.6) | <0.001 |
| COPD and chronic respiratory failure, n (%) | 44 (4.4) | 39 (5.6) | 5 (1.6) | 0.004 |
| Chronic renal failure | 51 (5.1) | 46 (6.7) | 5 (1.6) | <0.001 |
| Complicated high blood pressure, n (%) | 68 (6.8) | 59 (8.5) | 9 (2.9) | <0.001 |
| Time between symptoms and administration of treatment (days), median (IQR) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 0.409 |
| Time between symptoms and administration of treatment (days), n (%) | 0.593 | |||
| - 0 | 40 (4.0) | 32 (4.6) | 8 (2.6) | |
| - 1 | 142 (14.1) | 102 (14.8) | 40 (12.8) | |
| - 2 | 231 (23.0) | 154 (22.3) | 77 (24.6) | |
| - 3 | 271 (27.0) | 185 (26.8) | 86 (27.5) | |
| - 4 | 253 (25.2) | 171 (24.8) | 82 (26.2) | |
| - 5 | 67 (6.7) | 47 (6.8) | 20 (6.4) | |
| Reaction at the time of administration, n (%) | 0.383 | |||
| - No | 998 (99.4) | 688 (99.6) | 310 (99.0) | |
| - Yes | 6 (0.6) | 3 (0.4) | 3 (1.0) | |
| Infusion reaction/Hypersensitivity | 3 | 1 | 2 | |
| Others: | 3 | 2 | 1 | |
| - Agitation | 1 | 1 | 0 | |
| - Malaise-like reaction or chills | 1 | 1 | 0 | |
| - Vomiting at the end of the infusion | 1 | 0 | 1 |
| Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Characteristics | N | HR [CI 95%] | p-Value | HR [CI 95%] | p-Value |
| Treatment | <0.001 | <0.001 | |||
| - BAM + ETE | 569 | 1 | 1 | ||
| - CASI + IMD | 257 | 3.1 [2.1–4.4] | 3.0 [2.1–4.3] | ||
| Immune deficiency related to a pathology or treatment | 0.178 | 0.955 | |||
| - No | 387 | 1 | 1 | ||
| - Yes | 439 | 1.3 [0.9–1.8] | 1.0 [0.7–1.5] | ||
| Comorbidities | 0.081 | 0.562 | |||
| - No | 587 | 1 | 1 | ||
| - Yes | 239 | 0.7 [0.5–1.0] | 0.9 [0.5–1.4] | ||
| Time between symptoms and treatment (days) | 826 | 1.11 [0.96–1.28] | 0.159 | 1.1 [1.0–1.3] | 0.151 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zafilaza, K.; Bellet, J.; Truffot, A.; Foulongne, V.; Onambele, M.M.; Salmona, M.; Vellas, C.; Périllaud-Dubois, C.; Mirand, A.; André-Garnier, E.; et al. Comparison of Dual Monoclonal Antibody Therapies for COVID-19 Evolution: A Multicentric Retrospective Study. Viruses 2024, 16, 1542. https://doi.org/10.3390/v16101542
Zafilaza K, Bellet J, Truffot A, Foulongne V, Onambele MM, Salmona M, Vellas C, Périllaud-Dubois C, Mirand A, André-Garnier E, et al. Comparison of Dual Monoclonal Antibody Therapies for COVID-19 Evolution: A Multicentric Retrospective Study. Viruses. 2024; 16(10):1542. https://doi.org/10.3390/v16101542
Chicago/Turabian StyleZafilaza, Karen, Jonathan Bellet, Aurélie Truffot, Vincent Foulongne, Manuela Mireille Onambele, Maud Salmona, Camille Vellas, Claire Périllaud-Dubois, Audrey Mirand, Elisabeth André-Garnier, and et al. 2024. "Comparison of Dual Monoclonal Antibody Therapies for COVID-19 Evolution: A Multicentric Retrospective Study" Viruses 16, no. 10: 1542. https://doi.org/10.3390/v16101542





