Investigation of the Correlation between Enterovirus Infection and the Climate Factor Complex Including the Ping-Year Factor and El Niño-Southern Oscillation in Taiwan
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.1.1. Clinical Criteria: Any One of the Following Three Criteria
- Typical symptoms of hand, foot, and mouth disease or herpangina, with the presence of myoclonic jerks, or complications such as encephalitis, acute flaccid paralysis syndrome, acute hepatitis, myocarditis, acute cardiomyopathy, heart and lung failure, and other severe conditions.
- Absence of hand, foot, and mouth disease or herpangina, but with respiratory infection symptoms and suspected enterovirus infection accompanied by brainstem encephalitis or acute flaccid myelitis.
- Infants under three months of age who presented with symptoms of sepsis, such as myocarditis, hepatitis, encephalitis, thrombocytopenia, and multiple organ failure, excluding other common bacterial infections.
2.1.2. Laboratory Criteria: Any One of the Following Three Criteria
- Clinical specimens (throat swabs or throat washes, feces or rectal swabs, cerebrospinal fluid or vesicle fluid, etc.) were isolated and identified as enterovirus.
- Molecular biological nucleic acid testing of clinical specimens was positive.
- Serological antibody testing was positive (referring to specific IgM antibodies against enterovirus type 71 in serum)
2.2. Incidence Rate Calculation
- 1.
- Incidence rate of enterovirus infection
- 2.
- Incidence rate of EVSC
- 3.
- Ratio of EVSC
2.3. Grouping
2.3.1. Ping-Year Factor (PYF)
2.3.2. ENSO
2.4. Statistical Analysis
3. Results
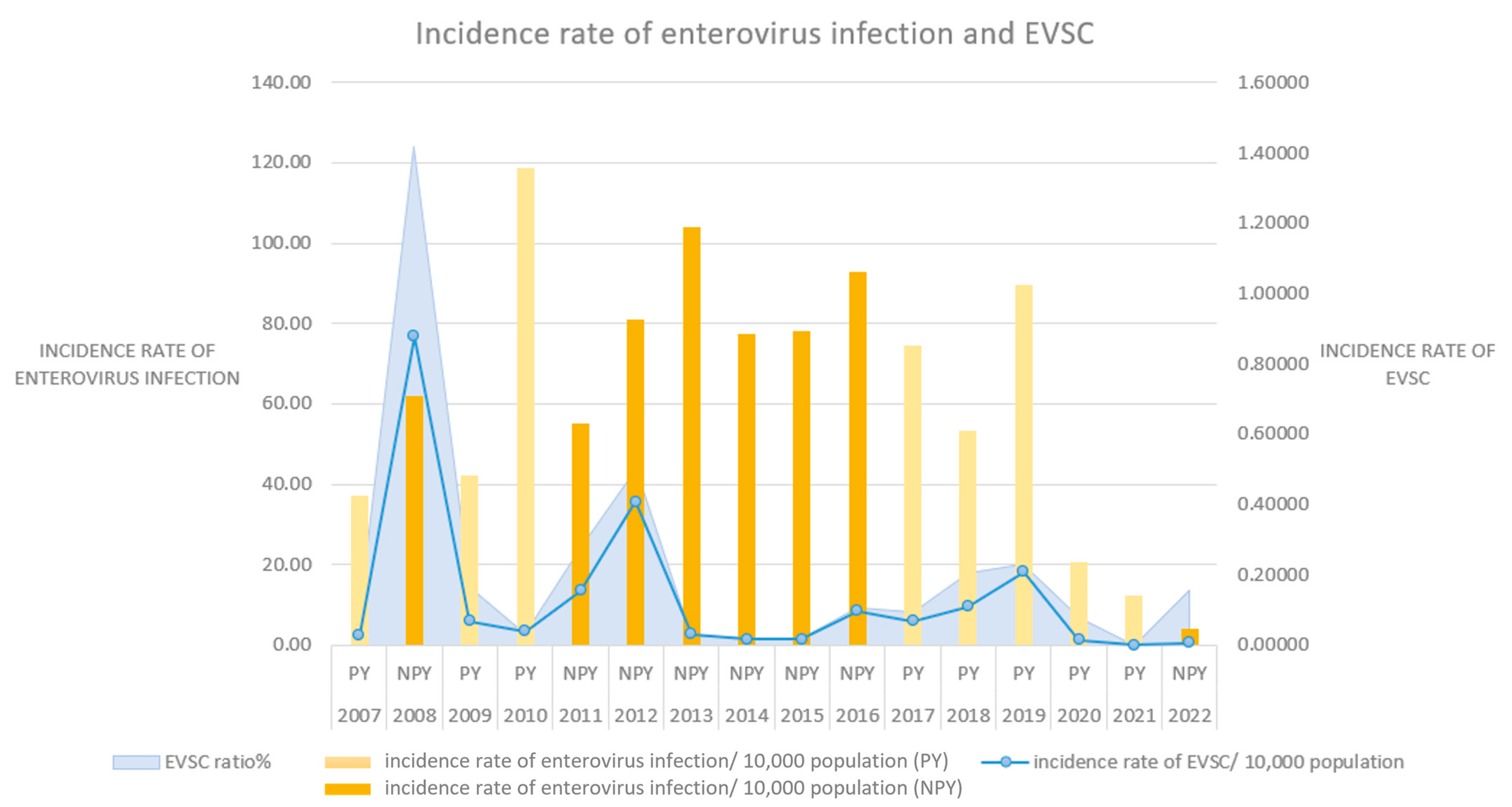
3.1. The PYF and Enterovirus Infection
3.2. ENSO and Enterovirus Infection
3.3. The PYF, ENSO, and Enterovirus Infection
4. Discussion
5. Conclusions
- ✓
- Enterovirus infection with severe complications (EVSC): Instead of the typical presentation of enterovirus infection like hand, foot, and mouth disease or herpangina, cases of EVSC show severe signs and symptoms. All cases of EVSC meet both clinical and laboratory criteria.
- ✓
- Climate factor complex (CFC): A combination of several climate factors including temperature, humidity, rainfall, wind speed, sunshine, air pressure, or more. CFC can affect the environment in a large-scale way.
- ✓
- ✓
- Ping-year factor (PYF): A certain combination of Celestial Stems and Terrestrial Branches used to determine whether a year is a ping-year (PY) or a non-ping-year (NPY). There is a total of 28 PYs and 32 NPYs in a cycle of 60 years (Table 3).
- ✓
- El Niño-Southern Oscillation (ENSO): A phenomenon presents alternating El Niño and La Niña conditions. During the El Niño phase, the sea surface temperature and rainfall increase in the eastern Pacific region, while in the western Pacific region, the sea surface temperature and rainfall decrease. The La Niña phase exhibits a trend opposite to that of the El Niño phase.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pons-Salort, M.; Parker, E.P.; Grassly, N.C. The epidemiology of non-polio enteroviruses: Recent advances and outstanding questions. Curr. Opin. Infect. Dis. 2015, 28, 479–487. [Google Scholar] [CrossRef]
- Hu, Y.L.; Chang, L.Y. Current status of enterovirus D68 worldwide and in Taiwan. Pediatr. Neonatol. 2020, 61, 9–15. [Google Scholar] [CrossRef]
- Lai, C.C.; Jiang, D.S.; Wu, H.M.; Chen, H.H. A dynamic model for the outbreaks of hand, foot, and mouth disease in Taiwan. Epidemiol. Infect. 2016, 144, 1500–1511. [Google Scholar] [CrossRef]
- Chiu, M.L.; Luo, S.T.; Chen, Y.Y.; Chung, W.Y.; Duong, V.; Dussart, P.; Chan, Y.F.; Perera, D.; Ooi, M.H.; Thao, N.T.T.; et al. Establishment of Asia-Pacific Network for Enterovirus Surveillance. Vaccine 2020, 38, 1–9. [Google Scholar] [CrossRef]
- Zhuang, R.-X.; Wu, F.-Z.; Huang, W.-T.; Guo, H.-W. Epidemiological Spatiotemporal Analysis of Infectious Disease. Commissioned Technological Research Plan of Centers for Disease Control, Ministry of Health and Welfare. 2011. Available online: https://www.grb.gov.tw/search/planDetail?id=2267733 (accessed on 15 March 2024).
- Zhang, X.-L.; Chen, G.-D. The Sequelae and Medical Cost of Enterovirus Infections in Taiwan. Commissioned Technological Research Plan of Centers for Disease Control, Ministry of Health and Welfare. 2012. Available online: https://www.grb.gov.tw/search/planDetail?id=2375044 (accessed on 15 March 2024).
- Jiang, J.-R.; Feng, Y.; Hung, C.-L.; Chang, H.-H.; Yang, S.-H.; Kuo, J.-J.; Chen, Y.-S. A Comparison of Statistical Analysis between the Epidemics in Ming and Qing Dynasties and the “Unharmed-Year” Hypothesis in Yun-Qi Theory. J. Chin. Med. 2004, 15, 231–239. [Google Scholar]
- Cheng, Q.; Bai, L.; Zhang, Y.; Zhang, H.; Wang, S.; Xie, M.; Zhao, D.; Su, H. Ambient temperature, humidity and hand, foot, and mouth disease: A systematic review and meta-analysis. Sci. Total Environ. 2018, 625, 828–836. [Google Scholar] [CrossRef]
- Nguyen, H.X.; Chu, C.; Nguyen, H.L.T.; Nguyen, H.T.; Do, C.M.; Rutherford, S.; Phung, D. Temporal and spatial analysis of hand, foot, and mouth disease in relation to climate factors: A study in the Mekong Delta region, Vietnam. Sci. Total Environ. 2017, 581–582, 766–772. [Google Scholar] [CrossRef]
- Abdul Wahid, N.A.; Suhaila, J.; Rahman, H.A. Effect of climate factors on the incidence of hand, foot, and mouth disease in Malaysia: A generalized additive mixed model. Infect. Dis. Model. 2021, 6, 997–1008. [Google Scholar] [CrossRef]
- Chang, H.L.; Chio, C.P.; Su, H.J.; Liao, C.M.; Lin, C.Y.; Shau, W.Y.; Chi, Y.C.; Cheng, Y.T.; Chou, Y.L.; Li, C.Y.; et al. The association between enterovirus 71 infections and meteorological parameters in Taiwan. PLoS ONE 2012, 7, e46845. [Google Scholar] [CrossRef]
- Hii, Y.L.; Rocklov, J.; Ng, N. Short term effects of weather on hand, foot and mouth disease. PLoS ONE 2011, 6, e16796. [Google Scholar] [CrossRef]
- Xiao, X.; Gasparrini, A.; Huang, J.; Liao, Q.; Liu, F.; Yin, F.; Yu, H.; Li, X. The exposure-response relationship between temperature and childhood hand, foot and mouth disease: A multicity study from mainland China. Environ. Int. 2017, 100, 102–109. [Google Scholar] [CrossRef]
- Chen, S.; Liu, X.; Wu, Y.; Xu, G.; Zhang, X.; Mei, S.; Zhang, Z.; O’Meara, M.; O’Gara, M.C.; Tan, X.; et al. The application of meteorological data and search index data in improving the prediction of HFMD: A study of two cities in Guangdong Province, China. Sci. Total Environ. 2019, 652, 1013–1021. [Google Scholar] [CrossRef]
- Song, C.; He, Y.; Bo, Y.; Wang, J.; Ren, Z.; Yang, H. Risk Assessment and Mapping of Hand, Foot, and Mouth Disease at the County Level in Mainland China Using Spatiotemporal Zero-Inflated Bayesian Hierarchical Models. Int. J. Environ. Res. Public Health 2018, 15, 1476. [Google Scholar] [CrossRef]
- Xing, W.; Liao, Q.; Viboud, C.; Zhang, J.; Sun, J.; Wu, J.T.; Chang, Z.; Liu, F.; Fang, V.J.; Zheng, Y.; et al. Hand, foot, and mouth disease in China, 2008–2012: An epidemiological study. Lancet Infect Dis 2014, 14, 308–318. [Google Scholar] [CrossRef]
- Onozuka, D.; Hashizume, M. The influence of temperature and humidity on the incidence of hand, foot, and mouth disease in Japan. Sci. Total Environ. 2011, 410–411, 119–125. [Google Scholar] [CrossRef]
- Zhang, D.S.; He, J.; Gao, S.H.; Hu, B.K.; Ma, S.L. Correlation analysis for the attack of respiratory diseases and meteorological factors. Chin. J. Integr. Med. 2011, 17, 600–606. [Google Scholar] [CrossRef]
- Zhang, D.S.; Zhang, X.; Ouyang, Y.H.; Zhang, L.; Ma, S.L.; He, J. Incidence of allergic rhinitis and meteorological variables: Non-linear correlation and non-linear regression analysis based on Yunqi theory of chinese medicine. Chin. J. Integr. Med. 2016. [Google Scholar] [CrossRef]
- Zhang, X.; Ma, S.L.; Liu, Z.D.; He, J. Correlation Analysis of Rubella Incidence and Meteorological Variables Based on Chinese Medicine Theory of Yunqi. Chin. J. Integr. Med. 2019, 25, 911–916. [Google Scholar] [CrossRef]
- Timmermann, A.; An, S.I.; Kug, J.S.; Jin, F.F.; Cai, W.; Capotondi, A.; Cobb, K.M.; Lengaigne, M.; McPhaden, M.J.; Stuecker, M.F.; et al. El Nino-Southern Oscillation complexity. Nature 2018, 559, 535–545. [Google Scholar] [CrossRef]
- Lin, H.; Zou, H.; Wang, Q.; Liu, C.; Lang, L.; Hou, X.; Li, Z. Short-term effect of El Nino-Southern Oscillation on pediatric hand, foot and mouth disease in Shenzhen, China. PLoS ONE 2013, 8, e65585. [Google Scholar] [CrossRef]
- Ramirez, I.J.; Lee, J.; Grady, S.C. Mapping Multi-Disease Risk during El Nino: An Ecosyndemic Approach. Int. J. Environ. Res. Public Health 2018, 15, 2639. [Google Scholar] [CrossRef]
- Anyamba, A.; Chretien, J.P.; Britch, S.C.; Soebiyanto, R.P.; Small, J.L.; Jepsen, R.; Forshey, B.M.; Sanchez, J.L.; Smith, R.D.; Harris, R.; et al. Global Disease Outbreaks Associated with the 2015–2016 El Nino Event. Sci. Rep. 2019, 9, 1930. [Google Scholar] [CrossRef]
- Andersen, L.K.; Davis, M.D. The effects of the El Nino Southern Oscillation on skin and skin-related diseases: A message from the International Society of Dermatology Climate Change Task Force. Int. J. Dermatol. 2015, 54, 1343–1351. [Google Scholar] [CrossRef]
- Iyer, V.; Sharma, A.; Nair, D.; Solanki, B.; Umrigar, P.; Murtugudde, R.; Jiang, C.; Mavalankar, D.; Sapkota, A. Role of extreme weather events and El Nino Southern Oscillation on incidence of Enteric Fever in Ahmedabad and Surat, Gujarat, India. Environ. Res. 2021, 196, 110417. [Google Scholar] [CrossRef] [PubMed]
- Adams, N.; Dhimal, M.; Mathews, S.; Iyer, V.; Murtugudde, R.; Liang, X.Z.; Haider, M.; Cruz-Cano, R.; Thu, D.T.A.; Hashim, J.H.; et al. El Nino Southern Oscillation, monsoon anomaly, and childhood diarrheal disease morbidity in Nepal. PNAS Nexus 2022, 1, pgac032. [Google Scholar] [CrossRef] [PubMed]
- Kovats, R.S.; Bouma, M.J.; Hajat, S.; Worrall, E.; Haines, A. El Nino and health. Lancet 2003, 362, 1481–1489. [Google Scholar] [CrossRef] [PubMed]
- Kuo, S.C.; Tsou, H.H.; Wu, H.Y.; Hsu, Y.T.; Lee, F.J.; Shih, S.M.; Hsiung, C.A.; Chen, W.J. Nonpolio Enterovirus Activity during the COVID-19 Pandemic, Taiwan, 2020. Emerg. Infect. Dis. 2021, 27, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.T.; Chang, H.L.; Wang, S.T.; Cheng, Y.T.; Yang, J.Y. Epidemiologic features of hand-foot-mouth disease and herpangina caused by enterovirus 71 in Taiwan, 1998–2005. Pediatrics 2007, 120, e244–e252. [Google Scholar] [CrossRef] [PubMed]
- Tseng, F.C.; Huang, H.C.; Chi, C.Y.; Lin, T.L.; Liu, C.C.; Jian, J.W.; Hsu, L.C.; Wu, H.S.; Yang, J.Y.; Chang, Y.W.; et al. Epidemiological survey of enterovirus infections occurring in Taiwan between 2000 and 2005: Analysis of sentinel physician surveillance data. J. Med. Virol. 2007, 79, 1850–1860. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.M.; Mulkey, S.B.; Campos, J.M.; DeBiasi, R.L. Laboratory diagnosis of CNS infections in children due to emerging and re-emerging neurotropic viruses. Pediatr. Res. 2024, 95, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Cheng, H.B.; Chen, H.H.; Liu, C.M.; Chou, C.H.; Sung, F.C. Circulating viruses associated with severe complicated enterovirus infection in Taiwan: A multi-year analysis. Pediatr. Infect. Dis. J. 2010, 29, 334–339. [Google Scholar] [CrossRef]
- Yang, J.Y.L.C. Development of Reagent Kits for Enterovirus Molecular Diagnosis. Department of Disease Control and Prevention, Ministry of Health and Welfare. 2020. Available online: https://www.grb.gov.tw/search/planDetail?id=12878301 (accessed on 15 March 2024).
- Nacher, M.; Adenis, A.; Blaizot, R.; Abboud, P.; Le Turnier, P.; Francoise, U.; Lucarelli, A.; Demar, M.; Djossou, F.; Epelboin, L.; et al. Establishing the proportion of severe/moderately severe vs mild cases of progressive disseminated histoplasmosis in patients with HIV. PLoS Negl. Trop. Dis. 2022, 16, e0010856. [Google Scholar] [CrossRef]
- Warner, P. Poisson regression. J. Fam. Plann Reprod. Health Care 2015, 41, 223–224. [Google Scholar] [CrossRef]
- Villeneuve, P.J.; Burnett, R.T.; Shi, Y.; Krewski, D.; Goldberg, M.S.; Hertzman, C.; Chen, Y.; Brook, J. A time-series study of air pollution, socioeconomic status, and mortality in Vancouver, Canada. J. Expo. Anal. Environ. Epidemiol. 2003, 13, 427–435. [Google Scholar] [CrossRef]
- Chang, S.A.; Kuan, C.H.; Hung, C.Y.; Wang, T.C.; Chen, Y.S. The outbreak of COVID-19 in Taiwan in late spring 2021: Combinations of specific weather conditions and related factors. Environ Sci Pollut Res Int 2022, 29, 85669–85675. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.Q.; Quirchmayr, G.; Winiwarter, W.; Cui, M. Influenza early warning model based on Yunqi theory. Chin. J. Integr. Med. 2012, 18, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.P.; Wang, T.A.; Huang, W.T.; Chang, L.Y.; Wang, E.T.; Cheng, S.H.; Yang, M.C. Disease burden of enterovirus infection in Taiwan: Implications for vaccination policy. Vaccine 2016, 34, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.L.; Chen, C.M.; Wang, E.T.; Kuo, H.W.; Shih, W.L.; Fang, C.T.; Liu, D.P.; Chang, L.Y. The secular trend of enterovirus A71 after the implementation of preventive measures in Taiwan. BMC Public. Health 2022, 22, 1483. [Google Scholar] [CrossRef]
- Gopalakrishnan, S.; Ebenesersdottir, S.S.; Lundstrom, I.K.C.; Turner-Walker, G.; Moore, K.H.S.; Luisi, P.; Margaryan, A.; Martin, M.D.; Ellegaard, M.R.; Magnusson, O.; et al. The population genomic legacy of the second plague pandemic. Curr. Biol. 2022, 32, 4743–4751. [Google Scholar] [CrossRef]
- Klunk, J.; Vilgalys, T.P.; Demeure, C.E.; Cheng, X.; Shiratori, M.; Madej, J.; Beau, R.; Elli, D.; Patino, M.I.; Redfern, R.; et al. Evolution of immune genes is associated with the Black Death. Nature 2022, 611, 312–319. [Google Scholar] [CrossRef]
- Bramanti, B.; Dean, K.R.; Walloe, L.; Chr Stenseth, N. The Third Plague Pandemic in Europe. Proc. Biol. Sci. 2019, 286, 20182429. [Google Scholar] [CrossRef]
- Yap, T.F.; Decker, C.J.; Preston, D.J. Effect of daily temperature fluctuations on virus lifetime. Sci. Total Environ. 2021, 789, 148004. [Google Scholar] [CrossRef]
- Lu, Y.C.; Tseng, L.W.; Huang, Y.C.; Yang, C.W.; Chen, Y.C.; Chen, H.Y. The Potential Complementary Role of Using Chinese Herbal Medicine with Western Medicine in Treating COVID-19 Patients: Pharmacology Network Analysis. Pharmaceuticals 2022, 15, 794. [Google Scholar] [CrossRef]
- Honein, M.A.; Barrios, L.C.; Brooks, J.T. Data and Policy to Guide Opening Schools Safely to Limit the Spread of SARS-CoV-2 Infection. JAMA 2021, 325, 823–824. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Braund, W.E.; Auerbach, J.; Chou, J.H.; Teng, J.H.; Tu, P.; Mullen, J. Policy Decisions and Use of Information Technology to Fight COVID-19, Taiwan. Emerg. Infect. Dis. 2020, 26, 1506–1512. [Google Scholar] [CrossRef] [PubMed]
- Thirumalai, K.; DiNezio, P.N.; Okumura, Y.; Deser, C. Extreme temperatures in Southeast Asia caused by El Nino and worsened by global warming. Nat. Commun. 2017, 8, 15531. [Google Scholar] [CrossRef] [PubMed]
- Chuang, T.W.; Chaves, L.F.; Chen, P.J. Effects of local and regional climatic fluctuations on dengue outbreaks in southern Taiwan. PLoS ONE 2017, 12, e0178698. [Google Scholar] [CrossRef]
| Celestial Stems | Jiǎ and Jǐ (甲, 己) | Yǐ and Gēng (乙, 庚) | Bǐng and Xīn (丙, 辛) | Dīng and Rén (丁, 壬) | Wù and Guǐ (戊, 癸) |
|---|---|---|---|---|---|
| Major Yun | Earth | Metal | Water | Wood | Fire |
| Terrestrial Branches | First Qi | Second Qi | Third Qi | Forth Qi | Fifth Qi | Sixth Qi |
|---|---|---|---|---|---|---|
| Zǐ and Wǔ (子, 午) | Greater Yang | Reverting Yin | Lesser Yin | Greater Yin | Lesser Yang | Yang Brightness |
| Chǒu and Wèi (丑, 未) | Reverting Yin | Lesser Yin | Greater Yin | Lesser Yang | Yang Brightness | Greater Yang |
| Yín and Shēn (寅, 申) | Lesser Yin | Greater Yin | Lesser Yang | Yang Brightness | Greater Yang | Reverting Yin |
| Mǎo and Yǒu (卯, 酉) | Greater Yin | Lesser Yang | Yang Brightness | Greater Yang | Reverting Yin | Lesser Yin |
| Chén and Xū (辰, 戌) | Lesser Yang | Yang Brightness | Greater Yang | Reverting Yin | Lesser Yin | Greater Yin |
| Sì and Hài (巳, 亥) | Yang Brightness | Greater Yang | Reverting Yin | Lesser Yin | Greater Yin | Lesser Yang |
| Celestial Stems (Heavenly Stems)—Terrestrial Branches (Earthly Branches) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Jiǎ-Zǐ 甲子 1984 | Yǐ-Chǒu 乙丑 1985 | Bǐng-Yín 丙寅 1986 | Dīng-Mǎo 丁卯 1987 | Wù-Chén 戊辰 1988 | Jǐ-Sì 己巳 1989 | Gēng-Wǔ 庚午 1990 | Xīn-Wèi 辛未 1991 | Rén-Shēn 壬申 1992 | Guǐ-Yǒu 癸酉 1993 |
| Jiǎ-Xū 甲戌 1994 | Yǐ-Hài 乙亥 1995 | Bǐng-Zǐ 丙子 1996 | Dīng-Chǒu 丁丑 1997 | Wù-Yín 戊寅 1998 | Jǐ-Mǎo 己卯 1999 | Gēng-Chén 庚辰 2000 | Xīn-Sì 辛巳 2001 | Rén-Wǔ 壬午 2002 | Guǐ-Wèi 癸未 2003 |
| Jiǎ-Shēn 甲申 2004 | Yǐ-Yǒu 乙酉 2005 | Bǐng-Xū 丙戌 2006 | Dīng-Hài 丁亥 2007 | Wù-Zǐ 戊子 2008 | Jǐ-Chǒu 己丑 2009 | Gēng-Yín 庚寅 2010 | Xīn-Mǎo 辛卯 2011 | Rén-Chén 壬辰 2012 | Guǐ-Sì 癸巳 2013 |
| Jiǎ-Wǔ 甲午 2014 | Yǐ-Wèi 乙未 2015 | Bǐng-Shēn 丙申 2016 | Dīng-Yǒu 丁酉 2017 | Wù-Xū 戊戌 2018 | Jǐ-Hài 己亥 2019 | Gēng-Zǐ 庚子 2020 | Xīn-Chǒu 辛丑 2021 | Rén-Yín 壬寅 2022 | Guǐ-Mǎo 癸卯 2023 |
| Jiǎ-Chén 甲辰 2024 | Yǐ-Sì 乙巳 2025 | Bǐng-Wǔ 丙午 2026 | Dīng-Wèi 丁未 2027 | Wù-Shēn 戊申 2028 | Jǐ-Yǒu 己酉 2029 | Gēng-Xū 庚戌 2030 | Xīn-Hài 辛亥 2031 | Rén-Zǐ 壬子 2032 | Guǐ-Chǒu 癸丑 2033 |
| Jiǎ-Yín 甲寅 2034 | Yǐ-Mǎo 乙卯 2035 | Bǐng-Chén 丙辰 2036 | Dīng-Sì 丁巳 2037 | Wù-Wǔ 戊午 2038 | Jǐ-Wèi 己未 2039 | Gēng-Shēn 庚申 2040 | Xīn-Yǒu 辛酉 2041 | Rén-Xū 壬戌 2042 | Guǐ-Hài 癸亥 2043 |
| Year | ONI | ENSO | Level |
|---|---|---|---|
| 2007 | −1.5~1.9 | La Niña | Strong |
| 2008 | −0.5~−0.9 | La Niña | Weak |
| 2009 | 1~1.4 | El Niño | Moderate |
| 2010 | −1.5~1.9 | La Niña | Strong |
| 2011 | −1~−1.4 | La Niña | Moderate |
| 2012 | Neutral | ||
| 2013 | Neutral | ||
| 2014 | 0.5~0.9 | El Niño | Weak |
| 2015 | >2 | El Niño | Very Strong |
| 2016 | −0.5~−0.9 | La Niña | Weak |
| 2017 | −0.5~−0.9 | La Niña | Weak |
| 2018 | 0.5~0.9 | El Niño | Weak |
| 2019 | Neutral | ||
| 2020 | −1~−1.4 | La Niña | Moderate |
| 2021 | −1~−1.4 | La Niña | Moderate |
| 2022 | −0.5~−0.9 | La Niña | Weak |
| Year | Ping-Year Factor | ENSO | ENSO Level | No. of Enterovirus Infections | No. of EVSCs | Total Population | Incidence Rate of Enterovirus Infections * | Incidence Rate of EVSCs * | Ratio of EVSCs |
|---|---|---|---|---|---|---|---|---|---|
| 2007 | PY | La Niña | Strong | 16,192 | 12 | 4,350,461 | 37.22 | 0.028 | 0.074 |
| 2008 | NPY | La Niña | Weak | 26,223 | 371 | 4,231,147 | 61.98 | 0.877 | 1.415 |
| 2009 | PY | El Niño | Moderate | 17,264 | 28 | 4,100,007 | 42.11 | 0.068 | 0.162 |
| 2010 | PY | La Niña | Strong | 46,933 | 16 | 3,948,315 | 118.87 | 0.041 | 0.034 |
| 2011 | NPY | La Niña | Moderate | 21,091 | 59 | 3,823,867 | 55.16 | 0.154 | 0.28 |
| 2012 | NPY | Neutral | 30,289 | 152 | 3,734,674 | 81.1 | 0.407 | 0.502 | |
| 2013 | NPY | Neutral | 37,560 | 11 | 3,613,842 | 103.93 | 0.03 | 0.029 | |
| 2014 | NPY | El Niño | Weak | 27,566 | 6 | 3,559,994 | 77.43 | 0.017 | 0.022 |
| 2015 | NPY | El Niño | Very Strong | 27,311 | 6 | 3,493,764 | 78.17 | 0.017 | 0.022 |
| 2016 | NPY | La Niña | Weak | 31,548 | 33 | 3,398,892 | 92.82 | 0.097 | 0.105 |
| 2017 | PY | La Niña | Weak | 24,820 | 23 | 3,338,143 | 74.35 | 0.069 | 0.093 |
| 2018 | PY | El Niño | Weak | 17,510 | 36 | 3,275,623 | 53.46 | 0.11 | 0.206 |
| 2019 | PY | Neutral | 28,967 | 67 | 3,228,875 | 89.71 | 0.208 | 0.231 | |
| 2020 | PY | La Niña | Moderate | 6546 | 5 | 3,171,193 | 20.64 | 0.016 | 0.076 |
| 2021 | PY | La Niña | Moderate | 3790 | 0 | 3,094,757 | 12.25 | 0 | 0 |
| 2022 | NPY | La Niña | Weak | 1281 | 2 | 3,022,295 | 4.24 | 0.007 | 0.156 |
| Average | 62.72 | 0.134 | 0.213 | ||||||
| Corrected average | 74.33 | 0.163 | 0.244 | ||||||
| Separate PYF and ENSO | Combined PYF and ENSO | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors | Incidence Rate Ratio | 95% CI | p < Value | Predictors | Incidence Rate Ratio | 95% CI | p-Value | ||
| Lower | Upper | Lower | Upper | ||||||
| incidence rate of enterovirus infections | |||||||||
| PY | 1 | - | - | - | PY | 1 | - | - | - |
| NPY | 1.24 | 1.23 | 1.24 | <0.001 *** | NPY | 1.29 | 1.28 | 1.29 | <0.001 *** |
| La Niña | 0.96 | 0.96 | 0.97 | <0.001 *** | La Niña (PY) | 1.03 | 1.03 | 1.04 | <0.001 *** |
| La Niña (NPY) | 0.89 | 0.89 | 0.89 | <0.001 *** | |||||
| incidence rate of EVSCs | |||||||||
| PY | 1 | - | - | - | PY | 1 | - | - | - |
| NPY | 3.38 | 2.88 | 3.99 | <0.001 *** | NPY | 2.38 | 2.00 | 2.83 | <0.001 *** |
| La Niña | 1.02 | 0.98 | 1.06 | 0.393 | La Niña (PY) | 0.77 | 0.71 | 0.83 | <0.001 *** |
| La Niña (NPY) | 1.94 | 1.75 | 2.16 | <0.001 *** | |||||
| ratio of EVSCs | |||||||||
| PY | 1 | - | - | - | PY | 1 | - | - | - |
| NPY | 2.73 | 2.33 | 3.23 | <0.001 *** | NPY | 1.79 | 1.51 | 2.13 | <0.001 *** |
| La Niña | 1.06 | 1.01 | 1.10 | 0.008 ** | La Niña (PY) | 0.74 | 0.68 | 0.80 | <0.001 *** |
| La Niña (NPY) | 2.37 | 2.12 | 2.65 | <0.001 *** | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H.-W.; Kuan, C.-H.; Tseng, L.-W.; Chen, H.-Y.; Tsai, M.-Y.; Chen, Y.-S. Investigation of the Correlation between Enterovirus Infection and the Climate Factor Complex Including the Ping-Year Factor and El Niño-Southern Oscillation in Taiwan. Viruses 2024, 16, 471. https://doi.org/10.3390/v16030471
Yu H-W, Kuan C-H, Tseng L-W, Chen H-Y, Tsai M-Y, Chen Y-S. Investigation of the Correlation between Enterovirus Infection and the Climate Factor Complex Including the Ping-Year Factor and El Niño-Southern Oscillation in Taiwan. Viruses. 2024; 16(3):471. https://doi.org/10.3390/v16030471
Chicago/Turabian StyleYu, Hsueh-Wen, Chia-Hsuan Kuan, Liang-Wei Tseng, Hsing-Yu Chen, Meg-Yen Tsai, and Yu-Sheng Chen. 2024. "Investigation of the Correlation between Enterovirus Infection and the Climate Factor Complex Including the Ping-Year Factor and El Niño-Southern Oscillation in Taiwan" Viruses 16, no. 3: 471. https://doi.org/10.3390/v16030471
APA StyleYu, H.-W., Kuan, C.-H., Tseng, L.-W., Chen, H.-Y., Tsai, M.-Y., & Chen, Y.-S. (2024). Investigation of the Correlation between Enterovirus Infection and the Climate Factor Complex Including the Ping-Year Factor and El Niño-Southern Oscillation in Taiwan. Viruses, 16(3), 471. https://doi.org/10.3390/v16030471





