Distinct Pathological Changes in Preweaning Mice Infected with Live-Attenuated Rift Valley Fever Virus Strains
Abstract
1. Introduction
2. Materials and Methods
2.1. Media, Cells, and Viruses
2.2. Mouse Challenge Experiment Using Live-Attenuated Rift Valley Fever Viruses
2.3. RT-qPCR Measurement of Viral RNA Loads in Tissues
2.4. Histological Examination
2.5. Statistical Analysis
2.6. Ethics Statement
3. Results
3.1. Susceptibility of 19-Day-Old C57BL/6 Mice to Live-Attenuated Rift Valley Fever Viruses
3.2. Viral Load of 19-Day-Old C57BL/6 Mice Succumbed to Live-Attenuated Rift Valley Fever Virus Infections
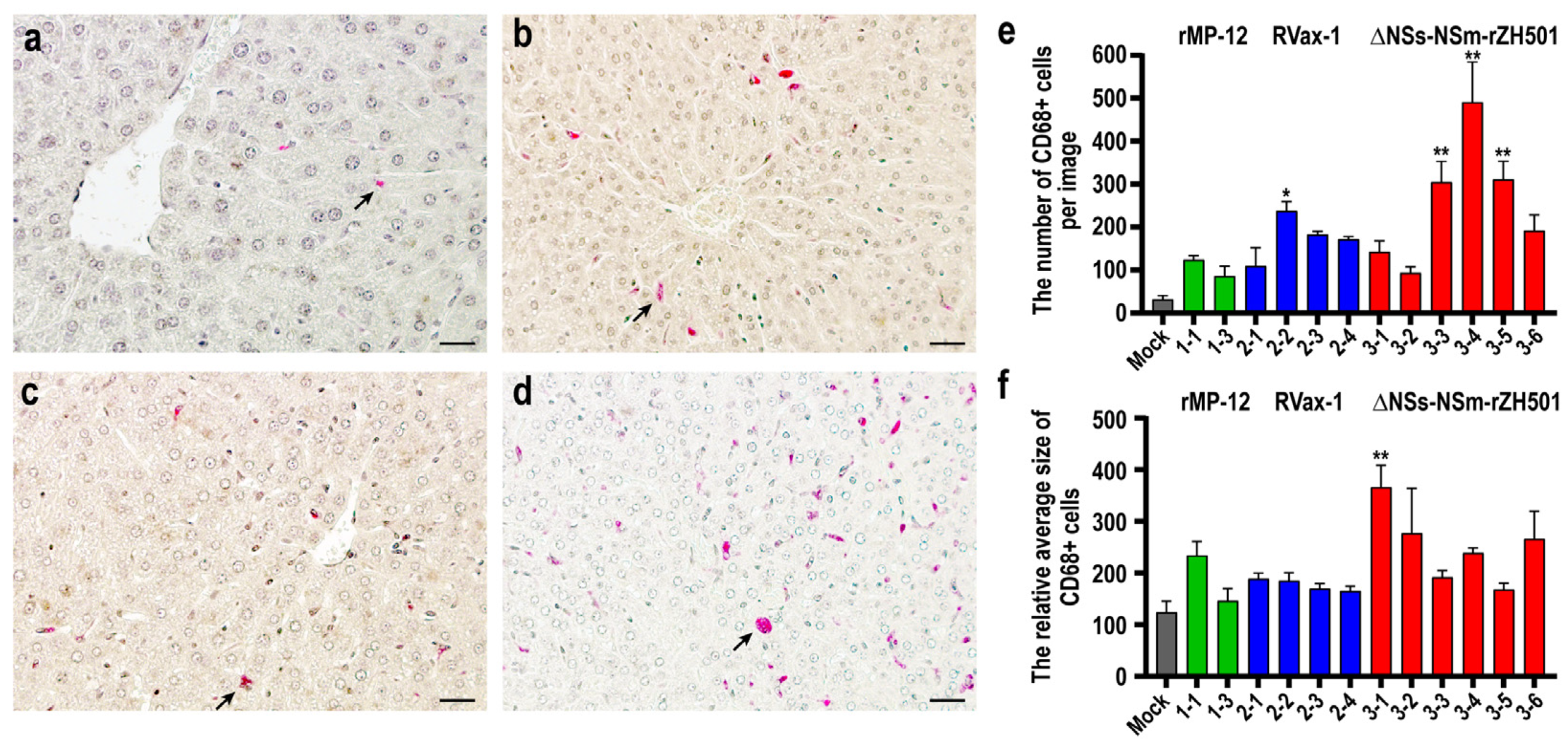
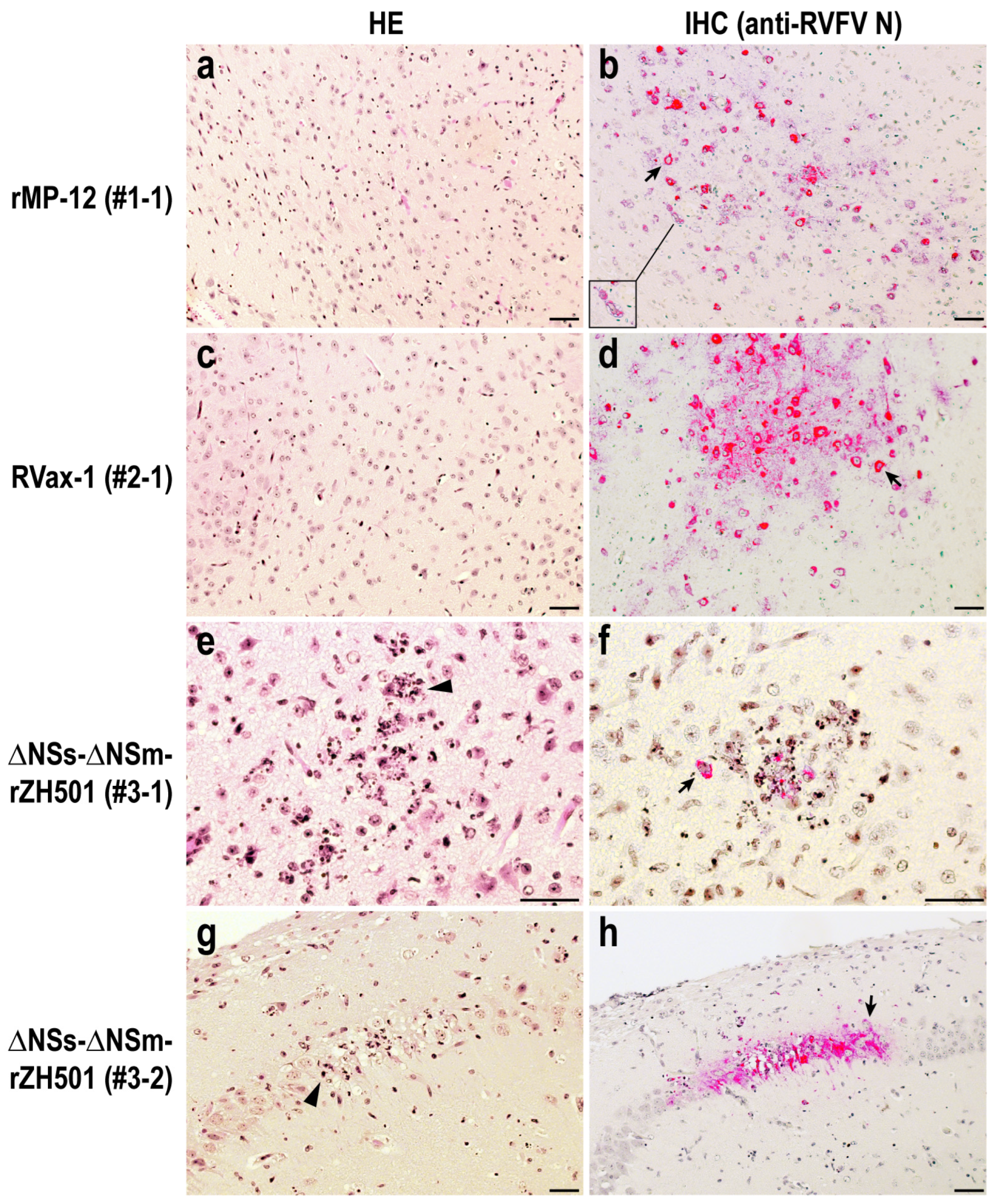
3.3. Histopathological Analysis of 19-Day-Old C57BL/6 Mice Succumbed to Live-Attenuated Rift Valley Fever Virus Infections
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Linthicum, K.J.; Britch, S.C.; Anyamba, A. Rift Valley Fever: An Emerging Mosquito-Borne Disease. Annu. Rev. Entomol. 2016, 61, 395–415. [Google Scholar] [CrossRef] [PubMed]
- Phoenix, I.; Lokugamage, N.; Nishiyama, S.; Ikegami, T. Mutational Analysis of the Rift Valley Fever Virus Glycoprotein Precursor Proteins for Gn Protein Expression. Viruses 2016, 8, 151. [Google Scholar] [CrossRef] [PubMed]
- Kreher, F.; Tamietti, C.; Gommet, C.; Guillemot, L.; Ermonval, M.; Failloux, A.B.; Panthier, J.J.; Bouloy, M.; Flamand, M. The Rift Valley fever accessory proteins NSm and P78/NSm-GN are distinct determinants of virus propagation in vertebrate and invertebrate hosts. Emerg. Microbes Infect. 2014, 3, e71. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, T.; Makino, S. The Pathogenesis of Rift Valley Fever. Viruses 2011, 3, 493–519. [Google Scholar] [CrossRef] [PubMed]
- Alkan, C.; Jurado-Cobena, E.; Ikegami, T. Advancements in Rift Valley fever vaccines: A historical overview and prospects for next generation candidates. NPJ Vaccines 2023, 8, 171. [Google Scholar] [CrossRef] [PubMed]
- Wichgers Schreur, P.J.; Bird, B.H.; Ikegami, T.; Bermudez-Mendez, E.; Kortekaas, J. Perspectives of Next-Generation Live-Attenuated Rift Valley Fever Vaccines for Animal and Human Use. Vaccines 2023, 11, 707. [Google Scholar] [CrossRef]
- Caplen, H.; Peters, C.J.; Bishop, D.H. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J. Gen. Virol. 1985, 66 Pt 10, 2271–2277. [Google Scholar] [CrossRef]
- Hills, R.E. Issuance of a Conditional License for Rift Valley Fever Vaccine, Modified Live Virus; Notice no. 13-12; Center for Veterinary Biologics: Ames, IA, USA, 2013. [Google Scholar]
- Pittman, P.R.; McClain, D.; Quinn, X.; Coonan, K.M.; Mangiafico, J.; Makuch, R.S.; Morrill, J.; Peters, C.J. Safety and immunogenicity of a mutagenized, live attenuated Rift Valley fever vaccine, MP-12, in a Phase 1 dose escalation and route comparison study in humans. Vaccine 2016, 34, 424–429. [Google Scholar] [CrossRef]
- Pittman, P.R.; Norris, S.L.; Brown, E.S.; Ranadive, M.V.; Schibly, B.A.; Bettinger, G.E.; Lokugamage, N.; Korman, L.; Morrill, J.C.; Peters, C.J. Rift Valley fever MP-12 vaccine Phase 2 clinical trial: Safety, immunogenicity, and genetic characterization of virus isolates. Vaccine 2016, 34, 523–530. [Google Scholar] [CrossRef]
- Ikegami, T.; Hill, T.E.; Smith, J.K.; Zhang, L.; Juelich, T.L.; Gong, B.; Slack, O.A.; Ly, H.J.; Lokugamage, N.; Freiberg, A.N. Rift Valley Fever Virus MP-12 Vaccine Is Fully Attenuated by a Combination of Partial Attenuations in the S, M, and L Segments. J. Virol. 2015, 89, 7262–7276. [Google Scholar] [CrossRef]
- Nishiyama, S.; Lokugamage, N.; Ikegami, T. The L-, M- and S-segments of Rift Valley fever virus MP-12 vaccine independently contribute to a temperature-sensitive phenotype. J. Virol. 2016, 90, 3735–3744. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, T.; Jurado-Cobena, E.; Alkan, C.; Smith, J.K.; Zhang, L.; Kalveram, B.; Juelich, T.L.; Esterly, A.T.; Bhaskar, J.R.; Thangamani, S.; et al. Evaluations of rationally designed rift valley fever vaccine candidate RVax-1 in mosquito and rodent models. NPJ Vaccines 2022, 7, 109. [Google Scholar] [CrossRef] [PubMed]
- Ly, H.J.; Nishiyama, S.; Lokugamage, N.; Smith, J.K.; Zhang, L.; Perez, D.; Juelich, T.L.; Freiberg, A.N.; Ikegami, T. Attenuation and protective efficacy of Rift Valley fever phlebovirus rMP12-GM50 strain. Vaccine 2017, 35 Pt B, 6634–6642. [Google Scholar] [CrossRef]
- Bird, B.H.; Albarino, C.G.; Hartman, A.L.; Erickson, B.R.; Ksiazek, T.G.; Nichol, S.T. Rift valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J. Virol. 2008, 82, 2681–2691. [Google Scholar] [CrossRef] [PubMed]
- Bird, B.H.; Maartens, L.H.; Campbell, S.; Erasmus, B.J.; Erickson, B.R.; Dodd, K.A.; Spiropoulou, C.F.; Cannon, D.; Drew, C.P.; Knust, B.; et al. Rift Valley Fever Virus Vaccine Lacking the NSs and NSm Genes Is Safe, Nonteratogenic, and Confers Protection from Viremia, Pyrexia, and Abortion following Challenge in Adult and Pregnant Sheep. J. Virol. 2011, 85, 12901–12909. [Google Scholar] [CrossRef] [PubMed]
- Billecocq, A.; Spiegel, M.; Vialat, P.; Kohl, A.; Weber, F.; Bouloy, M.; Haller, O. NSs protein of Rift Valley fever virus blocks interferon production by inhibiting host gene transcription. J. Virol. 2004, 78, 9798–9806. [Google Scholar] [CrossRef] [PubMed]
- Bouloy, M.; Janzen, C.; Vialat, P.; Khun, H.; Pavlovic, J.; Huerre, M.; Haller, O. Genetic evidence for an interferon-antagonistic function of rift valley fever virus nonstructural protein NSs. J. Virol. 2001, 75, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, T.; Narayanan, K.; Won, S.; Kamitani, W.; Peters, C.J.; Makino, S. Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog. 2009, 5, e1000287. [Google Scholar] [CrossRef] [PubMed]
- Kalveram, B.; Lihoradova, O.; Ikegami, T. NSs Protein of Rift Valley Fever Virus Promotes Post-Translational Downregulation of the TFIIH Subunit p62. J. Virol. 2011, 85, 6234–6243. [Google Scholar] [CrossRef]
- Mudhasani, R.; Tran, J.P.; Retterer, C.; Kota, K.P.; Whitehouse, C.A.; Bavari, S. Protein Kinase R Degradation Is Essential for Rift Valley Fever Virus Infection and Is Regulated by SKP1-CUL1-F-box (SCF)FBXW11-NSs E3 Ligase. PLoS Pathog. 2016, 12, e1005437. [Google Scholar] [CrossRef]
- Kainulainen, M.; Habjan, M.; Hubel, P.; Busch, L.; Lau, S.; Colinge, J.; Superti-Furga, G.; Pichlmair, A.; Weber, F. Virulence factor NSs of rift valley fever virus recruits the F-box protein FBXO3 to degrade subunit p62 of general transcription factor TFIIH. J. Virol. 2014, 88, 3464–3473. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, M.B.; Kent Crockett, R.J.; Bird, B.H.; Nichol, S.T.; Erickson, B.R.; Biggerstaff, B.J.; Horiuchi, K.; Miller, B.R. Infection and transmission of Rift Valley fever viruses lacking the NSs and/or NSm genes in mosquitoes: Potential role for NSm in mosquito infection. PLoS Negl. Trop. Dis. 2012, 6, e1639. [Google Scholar] [CrossRef] [PubMed]
- Cartwright, H.N.; Barbeau, D.J.; McElroy, A.K. Rift Valley Fever Virus Is Lethal in Different Inbred Mouse Strains Independent of Sex. Front. Microbiol. 2020, 11, 1962. [Google Scholar] [CrossRef] [PubMed]
- Ito, N.; Takayama-Ito, M.; Yamada, K.; Hosokawa, J.; Sugiyama, M.; Minamoto, N. Improved recovery of rabies virus from cloned cDNA using a vaccinia virus-free reverse genetics system. Microbiol. Immunol. 2003, 47, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, T. Development of a Simian RNA Polymerase I Promoter-Driven Reverse Genetics for the Rescue of Recombinant Rift Valley Fever Virus from Vero Cells. J. Virol. 2021, 95, e02004-20. [Google Scholar] [CrossRef]
- Ikegami, T.; Won, S.; Peters, C.J.; Makino, S. Rescue of infectious rift valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J. Virol. 2006, 80, 2933–2940. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, S.; Slack, O.A.; Lokugamage, N.; Hill, T.E.; Juelich, T.L.; Zhang, L.; Smith, J.K.; Perez, D.; Gong, B.; Freiberg, A.N.; et al. Attenuation of pathogenic Rift Valley fever virus strain through the chimeric S-segment encoding sandfly fever phlebovirus NSs or a dominant-negative PKR. Virulence 2016, 7, 871–881. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morrill, J.C.; Ikegami, T.; Yoshikawa-Iwata, N.; Lokugamage, N.; Won, S.; Terasaki, K.; Zamoto-Niikura, A.; Peters, C.J.; Makino, S. Rapid accumulation of virulent rift valley Fever virus in mice from an attenuated virus carrying a single nucleotide substitution in the m RNA. PLoS ONE 2010, 5, e9986. [Google Scholar] [CrossRef]
- Hallam, H.J.; Lokugamage, N.; Ikegami, T. Rescue of infectious Arumowot virus from cloned cDNA: Posttranslational degradation of Arumowot virus NSs protein in human cells. PLoS Negl. Trop. Dis. 2019, 13, e0007904. [Google Scholar] [CrossRef]
- Lihoradova, O.A.; Indran, S.V.; Kalveram, B.; Lokugamage, N.; Head, J.A.; Gong, B.; Tigabu, B.; Juelich, T.L.; Freiberg, A.N.; Ikegami, T. Characterization of Rift Valley Fever Virus MP-12 Strain Encoding NSs of Punta Toro Virus or Sandfly Fever Sicilian Virus. PLoS Negl. Trop. Dis. 2013, 7, e2181. [Google Scholar] [CrossRef]
- Won, S.; Ikegami, T.; Peters, C.J.; Makino, S. NSm and 78-kilodalton proteins of Rift Valley fever virus are nonessential for viral replication in cell culture. J. Virol. 2006, 80, 8274–8278. [Google Scholar] [CrossRef] [PubMed]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Ly, H.J.; Ikegami, T. Rift Valley fever virus NSs protein functions and the similarity to other bunyavirus NSs proteins. Virol. J. 2016, 13, 118. [Google Scholar] [CrossRef] [PubMed]
- Wuerth, J.D.; Weber, F. Phleboviruses and the Type I Interferon Response. Viruses 2016, 8, 174. [Google Scholar] [CrossRef] [PubMed]
- Bird, B.H.; Albarino, C.G.; Nichol, S.T. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology 2007, 362, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Haddock, E.; Feldmann, H.; Marzi, A. Ebola Virus Infection in Commonly Used Laboratory Mouse Strains. J. Infect. Dis. 2018, 218 (Suppl. S5), S453–S457. [Google Scholar] [CrossRef] [PubMed]
- Dodd, K.A.; McElroy, A.K.; Jones, M.E.; Nichol, S.T.; Spiropoulou, C.F. Rift Valley Fever Virus Clearance and Protection from Neurologic Disease Are Dependent on CD4+ T Cell and Virus-Specific Antibody Responses. J. Virol. 2013, 87, 6161–6171. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Dodd, K.A.; McElroy, A.K.; Jones, T.L.; Zaki, S.R.; Nichol, S.T.; Spiropoulou, C.F. Rift valley Fever virus encephalitis is associated with an ineffective systemic immune response and activated T cell infiltration into the CNS in an immunocompetent mouse model. PLoS Negl. Trop. Dis. 2014, 8, e2874. [Google Scholar] [CrossRef]

| Group | Sex (n 1) | Viruses | Target Doses (PFU 2) | Actual Doses (PFU) |
|---|---|---|---|---|
| 1 | M (2)/F (4) | rMP-12 | 1000 | 1680 |
| 2 | M (2)/F (4) | rMP-12 | 50 | 84 |
| 3 | M (3)/F (4) | rMP-12 | 10 | 8 |
| 4 | M (2)/F (5) | RVax-1 | 1000 | 840 |
| 5 | M (4)/F (7) | RVax-1 | 50 | 36 |
| 6 | M (3)/F (4) | RVax-1 | 10 | 9 |
| 7 | M (5)/F (2) | ∆NSs-∆NSm-rZH501 | 1000 | 567 |
| 8 | M (3)/F (4) | ∆NSs-∆NSm-rZH501 | 50 | 52 |
| 9 | M (4)/F (3) | ∆NSs-∆NSm-rZH501 | 10 | 7 |
| Viruses | Animal ID# (PFU Dose 1; Death 2) | Liver (Copies/mg) 3 | Spleen (Copies/mg) | Brain (Copies/mg) |
|---|---|---|---|---|
| [PFU/100 mg] 4 | [PFU/100 mg] | [PFU/100 mg] | ||
| rMP-12 | 1–1 (50; 5 dpc) | 5.0 × 101 | N.T. 5 | 9.7 × 106 |
| [<1.0 × 102] | [2.2 × 106] | |||
| 1–2 (50; 6 dpc) | 7.5 × 101 | N.T. | 2.4 × 109 | |
| 1–3 (50; 13 dpc) | 4.5 × 101 | 1.1 × 101 | 1.0 × 109 | |
| [<1.0 × 102] | [<1.0 × 102] | [3.2 × 106] | ||
| RVax-1 | 2–1 (50; 7 dpc) | 2.4 × 103 | N.T. | 1.8 × 108 |
| [<1.0 × 101] | N.T. | [1.4 × 106] | ||
| 2–2 (50; 7 dpc) | 2.5 × 102 | N.T. | 7.9 × 107 | |
| [3.0 × 102] | N.T. | [3.2 × 105] | ||
| 2–3 (50; 8 dpc) | 3.6 × 105 | 6.9 × 105 | 1.3 × 1011 | |
| [1.4 × 105] | [3.4 × 104] | [2.9 × 108] | ||
| 2–4 (50; 8 dpc) | 4.3 × 104 | 2.9 × 103 | 9.6 × 108 | |
| [4.0 × 102] | [1.0 × 102] | [9.7 × 106] | ||
| ∆NSs-∆NSm | 3–1 (50; 7 dpc) | 6.1 × 102 | 3.1 × 102 | 5.4 × 108 |
| -rZH501 | [<1.0 × 102] | [<1.0 × 102] | [1.2 × 105] | |
| 3–2 (50; 7 dpc) | 6.1 × 102 | 8.7 × 101 | 7.7 × 108 | |
| [<1.0 × 102] | [<1.0 × 102] | [9.0 × 104] | ||
| 3–3 (50; 7 dpc) | 9.8 × 100 | 4.5 × 102 | 2.5 × 108 | |
| [<1.0 × 102] | [<1.0 × 102] | [7.0 × 104] | ||
| 3–4 (50; 7 dpc) | 1.5 × 102 | 2.0 × 102 | 8.4 × 108 | |
| [<1.0 × 102] | [<1.0 × 102] | [8.0 × 104] | ||
| 3–5 (50; 7 dpc) | 3.3 × 102 | 2.5 × 102 | 7.6 × 108 | |
| [<1.0 × 102] | [<1.0 × 102] | [1.7 × 105] | ||
| 3–6 (50; 7 dpc) | 2.8 × 102 | 1.1 × 102 | 1.2 × 108 | |
| [<1.0 × 102] | [<1.0 × 102] | [1.0 × 105] |
| Viruses 50 PFU Dose | Animal ID# (Death) | Liv | Spl | Cor | Hp | Tha | Mid | Pon | Cer |
|---|---|---|---|---|---|---|---|---|---|
| rMP-12 | 1–1 (5 dpc) | − | − | − | − | ++ | +++ | +++ | N.T. |
| 1–3 (13 dpc) | − | − | − | − | + | + | N.T. | N.T. | |
| RVax-1 | 2–1 (7 dpc) | − | − | − | − | + | +++ | +++ | + |
| 2–2 (7 dpc) | − | − | − | − | + | + | ++ | ++ | |
| 2–3 (8 dpc) | + | − | +++ | +++ | +++ | N.T. | N.T. | N.T. | |
| 2–4 (8 dpc) | − | − | − | − | ++ | + | N.T. | N.T. | |
| ∆NSs-∆NSm | 3–1 (7 dpc) | − | − | − | − | ++ | + | +++ | ++ |
| -rZH501 | 3–2 (7 dpc) | − | − | + | ++ | ++ | + | ++ | + |
| 3–3 (7 dpc) | − | − | + | − | + | ++ | +++ | − | |
| 3–4 (7 dpc) | − | − | + | − | ++ | ++ | ++ | + | |
| 3–5 (7 dpc) | − | − | − | − | − | + | + | − |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkan, C.; Jurado-Cobena, E.; Ikegami, T. Distinct Pathological Changes in Preweaning Mice Infected with Live-Attenuated Rift Valley Fever Virus Strains. Viruses 2024, 16, 999. https://doi.org/10.3390/v16070999
Alkan C, Jurado-Cobena E, Ikegami T. Distinct Pathological Changes in Preweaning Mice Infected with Live-Attenuated Rift Valley Fever Virus Strains. Viruses. 2024; 16(7):999. https://doi.org/10.3390/v16070999
Chicago/Turabian StyleAlkan, Cigdem, Eduardo Jurado-Cobena, and Tetsuro Ikegami. 2024. "Distinct Pathological Changes in Preweaning Mice Infected with Live-Attenuated Rift Valley Fever Virus Strains" Viruses 16, no. 7: 999. https://doi.org/10.3390/v16070999
APA StyleAlkan, C., Jurado-Cobena, E., & Ikegami, T. (2024). Distinct Pathological Changes in Preweaning Mice Infected with Live-Attenuated Rift Valley Fever Virus Strains. Viruses, 16(7), 999. https://doi.org/10.3390/v16070999








