High-Quality Colonoscopy: A Review of Quality Indicators and Best Practices
Abstract
:1. Introduction
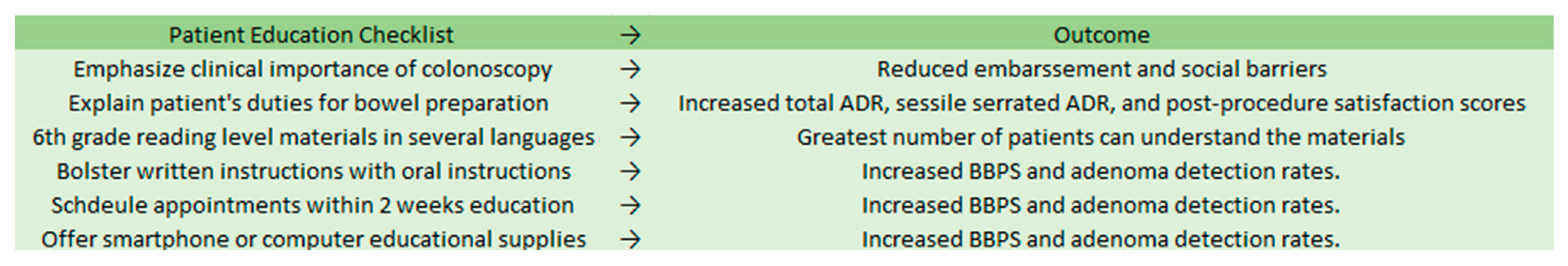
2. High-Quality Colonoscopy Component 1: Patient Education
3. High-Quality Colonoscopy Component 2: Bowel Preparation
4. High-Quality Colonoscopy Component 3: Proper Scoping Equipment and Contrast
5. High-Quality Colonoscopy Component 4: Improving Cecal Intubation
6. High-Quality Colonoscopy Component 5: Second Look into the Right Colon
7. High-Quality Colonoscopy Component 6: Lesion Detection Rate
8. High-Quality Colonoscopy Component 7: Proper Resection
9. High-Quality Colonoscopy Component 8: Documentation, Self-Analysis, and Quality Metrics
10. High-Quality Colonoscopy Component 9: Proper Screening Timelines for Patients in the US
11. Other Considerations and Utilizations
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Colorectal Cancer Statistics. C. f. D. C. a. Prevention. Available online: https://www.cdc.gov/cancer/colorectal/statistics/index.htm (accessed on 1 April 2022).
- Winawer, S.J.; Zauber, A.G.; Ho, M.N.; O’Brien, M.J.; Gottlieb, L.S.; Sternberg, S.S.; Waye, J.D.; Schapiro, M.; Bond, J.H.; Panish, J.F.; et al. Prevention of colorectal cancer by colonoscopic polypectomy. The national polyp study workgroup. N. Engl. J. Med. 1993, 329, 1977–1981. [Google Scholar] [CrossRef] [PubMed]
- Chokshi, R.V.; Hovis, C.E.; Hollander, T.; Early, D.S.; Wang, J.S. Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest. Endosc. 2012, 75, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Rex, D.K.; Cutler, C.S.; Lemmel, G.T.; Rahmani, E.Y.; Clark, D.W.; Helper, D.J.; Lehman, G.A.; Mark, D.G. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology 1997, 112, 24–28. [Google Scholar] [CrossRef]
- Lee, R.H. Quality colonoscopy: A matter of time, technique or technology? World J. Gastroenterol. 2013, 19, 1517–1522. [Google Scholar] [CrossRef]
- Cost-Effectiveness of Colorectal Cancer Interventions. 2021. Available online: https://www.cdc.gov/chronicdisease/programs-impact/pop/colorectal-cancer.htm#:~:text=The%20High%20Cost%20of%20Colorectal%20Cancer&text=Average%20Medicare%20health%20care%20spending,b)%20depending%20on%20the%20stage (accessed on 27 February 2022).
- Sullivan, K. AGA Offers Bundled Payment Model for Gastroenterologists. The American Journal of Managed Care. 2014. Available online: https://www.ajmc.com/view/aga-offers-bundled-payment-model-for-gastroenterologists (accessed on 1 April 2022).
- Amlani, B.; Radaelli, F.; Bhandari, P. A survey on colonoscopy shows poor understanding of its protective value and widespread misconceptions across Europe. PLoS ONE 2020, 15, e0233490. [Google Scholar] [CrossRef]
- Tian, X.; Xu, L.-L.; Liu, X.-L.; Chen, W.-Q. Enhanced patient education for colonic polyp and adenoma detection: Meta-analysis of randomized controlled trials. JMIR mHealth uHealth 2020, 8, e17372. [Google Scholar] [CrossRef]
- Stossel, L.M.; Segar, N.; Gliatto, P.; Fallar, R.; Karani, R. Readability of patient education materials available at the point of care. J. Gen. Intern. Med. 2012, 27, 1165–1170. [Google Scholar] [CrossRef] [Green Version]
- Janahiraman, S.; Tay, C.Y.; Lee, J.M.; Lim, W.L.; Khiew, C.H.; Ishak, I.; Onn, Z.Y.; Ibrahim, M.R.; Chew, C.K. Effect of an intensive patient educational programme on the quality of bowel preparation for colonoscopy: A single-blind randomised controlled trial. BMJ Open Gastroenterol. 2020, 7, e000376. [Google Scholar] [CrossRef]
- Lee, J.; Kim, T.O.; Seo, J.W.; Choi, J.H.; Heo, N.-Y.; Park, J.; Park, S.H.; Yang, S.Y.; Moon, Y.S. Shorter waiting times from education to colonoscopy can improve the quality of bowel preparation: A randomized controlled trial. Turk. J. Gastroenterol. 2018, 29, 75–81. [Google Scholar] [CrossRef] [Green Version]
- Back, S.Y.; Kim, H.G.; Ahn, E.M.; Park, S.; Jeon, S.R.; Im, H.H.; Kim, J.-O.; Ko, B.M.; Lee, J.S.; Lee, T.H.; et al. Impact of patient audiovisual re-education via a smartphone on the quality of bowel preparation before colonoscopy: A single-blinded randomized study. Gastrointest. Endosc. 2018, 87, 789–799.e4. [Google Scholar] [CrossRef]
- Zander, Q.E.W.v.d.; Reumkens, A.; van de Valk, B.; Winkens, B.; Masclee, A.A.M.; de Ridder, R.J.J. Effects of a personalized smartphone app on bowel preparation quality: Randomized controlled trial. JMIR mHealth uHealth 2021, 9, e26703. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.-C.; Kau, K.; Huang, S.-S.; Huang, W.-H.; Tsai, L.-Y.; Tsai, T.-Y.; Tsay, S.-L. Smartphone education improves embarrassment, bowel preparation, and satisfaction with care in patients receiving colonoscopy: A randomized controlled trail. Medicine 2020, 99, e23102. [Google Scholar] [CrossRef] [PubMed]
- Veldhuijzen, G.; Klemt-Kropp, M.; Droste, J.S.T.S.; van Balkom, B.; van Esch, A.A.J.; Drenth, J.P.H. Computer-based patient education is non-inferior to nurse counselling prior to colonoscopy: A multicenter randomized controlled trial. Endoscopy 2020, 53, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Kastenberg, D.; Bertiger, G.; Brogadir, S. Bowel preparation quality scales for colonoscopy. World J. Gastroenterol. 2018, 24, 2833–2843. [Google Scholar] [CrossRef] [PubMed]
- Calderwood, A.H.; Jacobson, B. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest. Endosc. 2010, 72, 686–692. [Google Scholar] [CrossRef] [Green Version]
- Stolpman, D.R.; Solem, C.A.; Eastlick, D.; Adlis, S.; Shaw, M.J. A randomized controlled trial comparing a low-residue diet versus clear liquids for colonoscopy preparation: Impact on tolerance, procedure time, and adenoma detection rate. J. Clin. Gastroenterol. 2014, 48, 851–855. [Google Scholar] [CrossRef]
- Alvarez-Gonzalez, M.A.; Pantaleon, M.; Roux, J.A.F.-L.; Zaffalon, D.; Amorós, J.; Bessa, X.; Seoane, A.; Pedro-Botet, J. Randomized clinical trial: A normocaloric low-fiber diet the day before colonoscopy is the most effective approach to bowel preparation in colorectal cancer screening colonoscopy. Dis. Colon Rectum 2019, 62, 491–497. [Google Scholar] [CrossRef]
- Jiao, L.; Wang, J.; Zhao, W.; Zhu, X.; Meng, X.; Zhao, L. Comparison of the effect of 1-day and 2-day low residue diets on the quality of bowel preparation before colonoscopy. Saudi J. Gastroenterol. 2020, 26, 137. [Google Scholar] [CrossRef]
- Mohamed, R.; Hilsden, R.J.; Dube, C.; Rostom, A. Split-Dose Polyethylene glycol is superior to single dose for colonoscopy preparation: Results of a randomized controlled trial. Can. J. Gastroenterol. Hepatol. 2016, 2016, 3181459. [Google Scholar] [CrossRef] [Green Version]
- Kmochova, K.; Grega, T.; Ngo, O.; Vojtechova, G.; Majek, O.; Urbanek, P.; Zavoral, M.; Suchanek, S. Comparison of four bowel cleansing agents for colonoscopy and the factors affecting their efficacy. A prospective, randomized study. J. Gastrointest. Liver Dis. 2021, 30, 213–220. [Google Scholar] [CrossRef]
- Di Palma, J.A.; Bhandari, R.; Cleveland, M.V.; Mishkin, D.S.; Tesoriero, J.; Hall, S.; McGowan, J. A safety and efficacy comparison of a new sulfate-based tablet bowel preparation versus a peg and ascorbate comparator in adult subjects undergoing colonoscopy. Am. J. Gastroenterol. 2020, 116, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Shi, X.; Kang, X.; Luo, H.; Wang, X.; Jia, H.; Tao, Q.; Wang, J.; Zhang, M.; Wang, J.; et al. Risk factors associated with inadequate bowel preparation in patients with functional constipation. Dig. Dis. Sci. 2019, 65, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, V.; Ragunath, K. Advanced endoscopic imaging: A review of commercially available technologies. Clin. Gastroenterol. Hepatol. 2014, 12, 368–376.e361. [Google Scholar] [CrossRef] [PubMed]
- Roelandt, P.; Demedts, I.; Willekens, H.; Bessissow, T.; Braeye, L.; Coremans, G.; Cuyle, P.-J.; Ferrante, M.; Gevers, A.-M.; Hiele, M.; et al. Impact of endoscopy system, high definition, and virtual chromoendoscopy in daily routine colonoscopy: A randomized trial. Endoscopy 2019, 51, 237–243. [Google Scholar] [CrossRef]
- Pohl, J.; Schneider, A.; Vogell, H.; Mayer, G.; Kaiser, G.; Ell, C. Pancolonic chromoendoscopy with indigo carmine versus standard colonoscopy for detection of neoplastic lesions: A randomised two-centre trial. Gut 2010, 60, 485–490. [Google Scholar] [CrossRef]
- Iacucci, M.; Kaplan, G.G.; Panaccione, R.; Akinola, O.; Lethebe, B.C.; Lowerison, M.; Leung, Y.; Novak, K.L.; Seow, C.H.; Urbanski, S.; et al. A randomized trial comparing high definition colonoscopy alone with high definition dye spraying and electronic virtual chromoendoscopy for detection of colonic neoplastic lesions during IBD surveillance colonoscopy. Am. J. Gastroenterol. 2018, 113, 225–234. [Google Scholar] [CrossRef]
- Spadaccini, M.; Iannone, A.; Maselli, R.; Badalamenti, M.; Desai, M.; Chandrasekar, V.T.; Patel, H.K.; Fugazza, A.; Pellegatta, G.; Galtieri, P.A.; et al. Computer-aided detection versus advanced imaging for detection of colorectal neoplasia: A systematic review and network meta-analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 793–802. [Google Scholar] [CrossRef]
- Hoff, G.; Holme, Ø.; Bretthauer, M.; Sandvei, P.; Darre-Næss, O.; Stallemo, A.; Wiig, H.; Høie, O.; Noraberg, G.; Moritz, V.; et al. Cecum intubation rate as quality indicator in clinical versus screening colonoscopy. Endosc. Int. Open 2017, 5, E489–E495. [Google Scholar] [CrossRef] [Green Version]
- Baxter, N.N.; Sutradhar, R.; Forbes, S.; Paszat, L.F.; Saskin, R.; Rabeneck, L. Analysis of administrative data finds endoscopist quality measures associated with postcolonoscopy colorectal cancer. Gastroenterology 2011, 140, 65–72. [Google Scholar] [CrossRef]
- European Guidelines for Quality Assurance in Colorectal Cancer Screening and Diagnosis; Publications Office of the European Union: Luxembourg, 2013.
- Cardin, F.; Minicuci, N.; Andreotti, A.; Pinetti, E.; Campigotto, F.; Donà, B.M.; Martella, B.; Terranova, O. Maximizing the general success of cecal intubation during propofol sedation in a multi-endoscopist academic centre. BMC Gastroenterol. 2010, 10, 123. [Google Scholar] [CrossRef] [Green Version]
- Garborg, K.; Bretthauer, M. Cecal intubation failure: Refer or change technique? Gastrointest. Endosc. 2016, 83, 1245–1247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garborg, K.; Wiig, H.; Hasund, A.; Matre, J.; Holme, Ø.; Noraberg, G.; Løberg, M.; Kalager, M.; Adami, H.; Bretthauer, M. Gradual stiffness versus magnetic imaging-guided variable stiffness colonoscopes: A randomized noninferiority trial. United Eur. Gastroenterol. J. 2017, 5, 128–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, S.G.; Brooker, J.C.; Williams, C.B.; Thapar, C.; Suzuki, N.; Saunders, B.P. The variable stiffness colonoscope: Assessment of efficacy by magnetic endoscope imaging. Gastrointest. Endosc. 2002, 56, 195–201. [Google Scholar] [CrossRef]
- Mark-Christensen, A.; Brandsborg, S.; Iversen, L.H. Magnetic endoscopic imaging as an adjuvant to elective colonoscopy: A systematic review and meta-analysis of randomized controlled trials. Endoscopy 2014, 47, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.S.; Lee, J.W.; Chang, L.-C.; Ong, D.E.; Chiu, H.-M.; Matsuda, T.; Kim, H.-S.; Sekiguchi, M.; Leong, R.W.; Ho, A.M.; et al. Two vs. one forward view examination of right colon on adenoma detection: An international multicenter randomized trial. Clin. Gastroenterol. Hepatol. 2020, 20, 372–380.e372. [Google Scholar] [CrossRef] [PubMed]
- Rex, D.K.; Schoenfeld, P.S.; Cohen, J.; Pike, I.M.; Adler, D.G.; Fennerty, M.B.; Lieb, J.G., II; Park, W.G.; Rizk, M.K.; Sawhney, M.S.; et al. Quality indicators for colonoscopy. Gastrointest. Endosc. 2014, 81, 31–53. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, P.; Liu, X.; Li, L.; Xiao, X.; Liu, P.; Zhang, D.; Li, Y.; Xu, G.; Tu, M.; et al. Factors predicting the colorectal adenoma detection rate in colonoscopic screening of a Chinese population: A prospective study. Medicine 2019, 98, e15103. [Google Scholar] [CrossRef]
- Mangas-Sanjuan, C.; Zapater, P.; Cubiella, J.; Murcia, Ó.; Bujanda, L.; Hernández, V.; Martínez-Ares, D.; Pellisé, M.; Seoane, A.; Lanas, Á.; et al. Importance of endoscopist quality metrics for findings at surveillance colonoscopy: The detection-surveillance paradox. United Eur. Gastroenterol. J. 2018, 6, 622–629. [Google Scholar] [CrossRef]
- Pohl, H.; Srivastava, A.; Bensen, S.P.; Anderson, P.; Rothstein, R.I.; Gordon, S.R.; Levy, L.C.; Toor, A.; Mackenzie, T.A.; Rosch, T.; et al. Incomplete polyp resection during colonoscopy—Results of the Complete Adenoma Resection (CARE) study. Gastroenterology 2013, 144, 74–80.e71. [Google Scholar] [CrossRef] [Green Version]
- Wallace, M.B. New strategies to improve polypectomy during colonoscopy. Gastroenterol. Hepatol. 2017, 13, 1–12. [Google Scholar]
- Piraka, C.; Saeed, A.; Waljee, A.K.; Pillai, A.; Stidham, R.; Elmunzer, B.J. Cold snare polypectomy for non-pedunculated colon polyps greater than 1 cm. Endosc. Int. Open 2017, 5, E184–E189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choksi, N.; Elmunzer, B.J.; Stidham, R.W.; Shuster, D.; Piraka, C. Cold snare piecemeal resection of colonic and duodenal polyps ≥1 cm. Endosc. Int. Open 2015, 3, E508–E513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tutticci, N.J.; Hewett, D.G. Cold EMR of large sessile serrated polyps at colonoscopy (with video). Gastrointest. Endosc. 2018, 87, 837–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmes, I.; Friedland, S. Endoscopic mucosal resection versus endoscopic submucosal dissection for large polyps: A western colonoscopist’s view. Clin. Endosc. 2016, 49, 454–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moss, A.; Williams, S.J.; Hourigan, L.F.; Brown, G.; Tam, W.; Singh, R.; Zanati, S.; Burgess, N.; Sonson, R.; Byth, K.; et al. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: Results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut 2014, 64, 57–65. [Google Scholar] [CrossRef] [Green Version]
- Uraoka, T.; Saito, Y.; Yamamoto, K.; Fujii, T. Submucosal injection solution for gastrointestinal tract endoscopic mucosal resection and endoscopic submucosal dissection. Drug Des. Dev. Ther. 2008, 2, 131–138. [Google Scholar] [CrossRef] [Green Version]
- Rex, D.; Wallace, M.B.; Sharma, P.; Lollo, G.; Maselli, R.; Repici, A. 689 A Randomized, double-blind trial of a new injectable solution (Sic 8000) for endoscopic resection of colonic polyps larger than 2 cm: An interim report. Gastrointest. Endosc. 2017, 85, AB101. [Google Scholar] [CrossRef]
- What Should I Know About Screening? 2022. Available online: https://www.cdc.gov/cancer/colorectal/basic_info/screening/index.htm (accessed on 1 April 2022).
- Bresky, E.; Bresky, G.; Lancellotti, D.; Madariaga, J.; Licuime, S.; Palma, P.; Saez, F.; Rojas, M.J.; Seijas, L. Should the endoscopic restrictions during COVID-19 pandemic remain unchanged? Gastroenterol. Insights 2021, 12, 34. [Google Scholar] [CrossRef]
- Magi, L.; Rinzivillo, M.; Panzuto, F. What gastroenterologists should know about carcinoid syndrome. Gastroenterol. Insights 2022, 13, 14. [Google Scholar] [CrossRef]


| Quality Metrics | Description |
|---|---|
| Patient Education | Emphasis on importance of colonoscopy Explanation of need for bowel preparation Simple language, 6th-grade reading level materials Materials available in different languages Scheduling of appointments within 2 weeks of education |
| Bowel Preparation | Use of validated scales to document bowel preparation Adherence to low-residue or clear liquid diet Adjustment of bowel preparation dose for patients with chronic constipation or diabetes, patients who use opioids, and the elderly. |
| Proper Scoping Equipment and Contrast | Using the best available modality for diagnostic purposes |
| Improving Cecal Intubation | Endoscopists improvement of skills, as it is a technically challenging maneuver Improvement of modifiable factors (bowel preparation) Application of variable stiffness colonoscopes |
| Second Look into the Right Colon | Repeat forward view upon reaching hepatic flexure |
| Lesion Detection Rate | Endoscopists should aim for an adenoma detection rate of 25% in males and 15% in females |
| Proper Resection | Complete removal with proper margin while minimizing damage to surrounding mucosa Removal technique guided by size and shape of polyp |
| Documentation, Self-Analysis, and Quality Metrics | Tracking of validated quality metrics Comparison of quality metrics amongst peers, ongoing review of new medical literature |
| Proper Screening Timelines for Patients in the US | For average patients, CRC screening should be started at age 45 and continued every 10 years until age 75 Screening beyond that age is based on a combination of factors and is individualized Patients with family history of CRC and patients with inflammatory bowel, familial adenomatous polyposis, and Lynch syndrome should start screening before age 45 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soeder, M.; Turshudzhyan, A.; Rosenberg, L.; Tadros, M. High-Quality Colonoscopy: A Review of Quality Indicators and Best Practices. Gastroenterol. Insights 2022, 13, 162-172. https://doi.org/10.3390/gastroent13020017
Soeder M, Turshudzhyan A, Rosenberg L, Tadros M. High-Quality Colonoscopy: A Review of Quality Indicators and Best Practices. Gastroenterology Insights. 2022; 13(2):162-172. https://doi.org/10.3390/gastroent13020017
Chicago/Turabian StyleSoeder, Mason, Alla Turshudzhyan, Lisa Rosenberg, and Micheal Tadros. 2022. "High-Quality Colonoscopy: A Review of Quality Indicators and Best Practices" Gastroenterology Insights 13, no. 2: 162-172. https://doi.org/10.3390/gastroent13020017
APA StyleSoeder, M., Turshudzhyan, A., Rosenberg, L., & Tadros, M. (2022). High-Quality Colonoscopy: A Review of Quality Indicators and Best Practices. Gastroenterology Insights, 13(2), 162-172. https://doi.org/10.3390/gastroent13020017






