Abstract
Background/Objectives: Although newborn hearing screening (NHS) programs have been successfully implemented in many countries worldwide, challenges to these programs have been reported in the literature, such as a lack of awareness among families and healthcare professionals and limited funding. Challenges to the NHS programs in Saudi Arabia have not been systematically reported. This study aimed to assess the level and quality of evidence supporting the existing challenges of the NHS programs in Saudi Arabia. Methods: A systematic review of all peer-reviewed literature on Saudi NHS programs published between 2016 and 2024 was conducted according to the PRISMA guidelines. Search strategies were executed in seven databases. Data were collected from studies that met the inclusion criteria. Results: A total of 37 records were reviewed, and 13 peer-reviewed publications met the inclusion criteria. Characteristics of included studies were classified by study language, study sample, sample size, location of the study sample, study purpose, and study method via evidence tables. Each study was critically appraised according to the quality. Results revealed that cross-sectional prospective description was the main research design with low strength of evidence. Six main challenges were identified and described: lack of awareness and gaps in knowledge, lost to follow-up, inadequate data entry, management, and tracking system, limited or absence of services in some residential areas, insufficient training and frequent changes of NHS personnel, and absence of a standardized NHS protocol. Conclusions: This review may assist in overcoming these challenges and improving the NHS programs in Saudi Arabia. There is a need to establish national education campaigns about the NHS programs, improve documentation by using database management and tracking systems, and expand the early hearing detection and intervention (EHDI) services for children in all Saudi regions.
1. Introduction
Hearing plays an important role in learning spoken language. The development of language is strongly related to cognitive, social, and emotional development [1,2]. Hearing loss can have significant negative effects on language development, speech, and cognition. These effects can then have an impact on future academic and career opportunities, as well as mental health and social interactions [3,4,5]. According to the World Health Organization (WHO), approximately 430 million people worldwide, including 34 million children, have disabling hearing loss and require rehabilitation [6]. Congenital hearing loss is one of the most chronic conditions in children that affects 2–3 in every 1000 births [7]. Varying prevalences of both permanent and fluctuating hearing loss among Saudi children were reported in the literature ranging from 1.75% to 13% [8,9,10]. Saudi children commonly suffer from both conductive hearing loss and sensorineural hearing loss (SNHL) [11,12]. Without appropriate intervention, the negative impact of hearing loss in children continues into later life [13].
Early hearing detection and intervention (EHDI) programs have been established to ensure adequate access to linguistic stimulation and intervention services as quickly as possible by screening newborns before one month of age, completing audiologic diagnosis before three months of age, and providing early intervention before six months of age (i.e., the 1–3–6 EHDI timeline) [14]. The Joint Committee on Infants Hearing (JCIH) recommends the EHDI programs that have met this timeline set a new target of 1–2–3 months (screen hearing of newborns before one month of age, diagnose before two months of age, and provide early intervention before three months of age) [14]. The positive outcomes of the EHDI program have been well documented in the literature [3,15]. The first critical step of the EHDI program is newborn or neonatal hearing screening (NHS).
The process of NHS involves simple and non-invasive tests to assess the auditory system of newborns. By detecting hearing loss early, audiologists and other healthcare professionals can initiate timely interventions and provide appropriate support to maximize a child’s communication and language development. There has been a growing recognition of the importance of NHS [16]. The WHO recommends all countries adopt NHS protocols and establish appropriate rehabilitation services [17], so several countries have taken significant steps to implement universal NHS programs [16].
In Saudi Arabia, the collaboration between the Ministry of Health (MOH) and the Saudi Association for Hearing Impairment led to the launching of the first NHS program in two hospitals located in Riyadh in 2007 [18]. Before that, hospitals that were not under the MOH administration, such as military hospitals and private hospitals, had implemented their own NHS programs. In 2014, the government legislated hearing screenings for all newborns in Saudi Arabia that are covered either by the government or insurance companies [18,19]. In 2016, the MOH started the first phase of the NHS program, covering more than 60% of newborns in 30 referral hospitals to screen every newborn within 72 h of birth [20]. The current coverage rate of NHS is more than 96% with a refer rate of 0.7% in the MOH hospitals across Saudi Arabia [19]. Despite these efforts, challenges, and barriers, such as lack of awareness among parents and healthcare professionals, lack of infrastructure, inadequate funding, and scarcity of qualified professionals may hinder the effective implementation of NHS programs [21]. Unfortunately, there has been no research specifically designed to explore the up-to-date challenges to the NHS programs in Saudi Arabia. Therefore, this systematic review asked the following question: what are the challenges faced by the NHS programs in Saudi Arabia? Our study aimed to explore these challenges and provide recommendations for improvement.
2. Materials and Methods
This systematic review was approved by the Institutional Review Board (IRB) of King Saud bin Abdulaziz University for Health Sciences protocol number (IRB/NRR24/017/4).
2.1. Search Strategy
The procedure for Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) is recommended to report the methods and findings of systematic reviews [22]. Our study adheres to the PRISMA guidelines to maintain transparency, comprehensiveness, and methodological rigor in reporting our systematic review. We have utilized the PRISMA checklist and flow diagram to outline the processes of study identification, screening, eligibility assessment, and inclusion, thereby strengthening the reproducibility and reliability of our findings. The following electronic databases, PubMed, ScienceDirect, CINAHL via EBSCOhost, Cochrane Central, Embase, and Arab World Research Source, were searched in November 2024. The bibliographies of recent literature reviews and currently reviewed articles, as well as Google Scholar, were used to find relevant publications. The search results include all relevant citations that were found. Keywords, syntax terms, and Boolean phrases, such as (newborn hearing screening OR neonatal hearing screening OR infant hearing screening) AND (Saudi Arabia) AND (challenges OR difficulties OR threats) were used to retrieve available articles from these databases. Appendix A shows an example of PubMed search terms and strings.
2.2. Inclusion and Exclusion Criteria
Research studies conducted to investigate NHS and its related aspects including challenges in Saudi Arabia were included. The inclusion criteria contained all study designs. Studies that were available electronically in peer-reviewed journals and published in both Arabic and English were included. Studies that were published before 2016 were excluded because the MOH, which oversees the NHS programs in the MOH birth hospitals in Saudi Arabia, started the first phase of the NHS program in 2016. Therefore, this systematic review included studies published between 2016 and 2024, ensuring a comprehensive analysis of recent research within this timeframe.
2.3. Eligibility and Selection
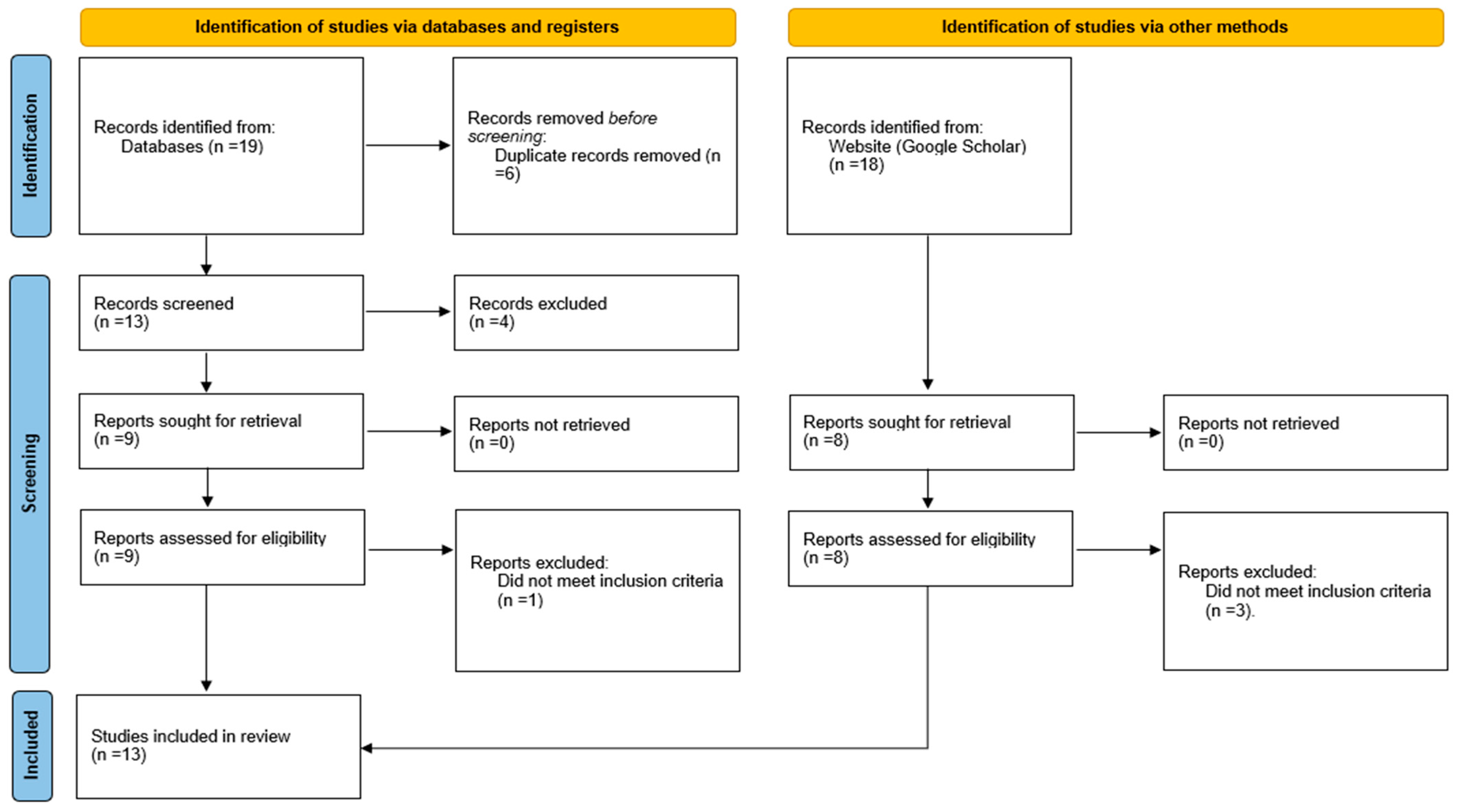
A detailed description of the systematic review’s search plan and selection criteria was developed. Initially, the search strategy was implemented and completed. Second, the papers’ titles were checked for relevancy; any research judged irrelevant did not receive further consideration. Third, the abstracts of the remaining papers were retrieved electronically, and their applicability was evaluated. The studies that met the requirements for inclusion were subsequently downloaded and printed out for careful examination. The authors assessed each study’s eligibility and methodological quality twice to ensure no bias in the publications they chose to include or reject. The PRISMA flow diagram was used to guide this procedure (Figure 1).
Figure 1.
PRISMA flow diagram demonstrates the search process. Adapted from Page et al. [22].
2.4. Critical Appraisal
Two authors evaluated the studies that were chosen for retrieval independently. Every author scored every study on their own. Critical assessment ratings were compared, and disagreements were discussed and resolved. Following the establishment of consensus, the strength of evidence of the included studies was evaluated.
2.5. Strength of Evidence
Each of the studies meeting the inclusion criteria was also rated for quality (strength) of evidence and included three categories (High, Moderate, Low). The strength of evidence classification does not mean that studies rated as having moderate or low strength of evidence are not useful, but it is essential for guiding decisions in evidence-based practices.
- High: Random assignment studies with low attrition of sample members and no reassignment of sample members after the original random assignments.
- Moderate: Random assignment studies that, because of flaws in the study design, execution, or analysis, do not meet all the criteria for the high rating; matched comparison group designs that establish baseline equivalence on selected measures; and single case and regression discontinuity designs.
- Low: Impact studies that do not meet the criteria for high or moderate.
2.6. Data Extraction and Synthesis
Data extraction and synthesis were performed on all studies, regardless of the quality of their methodology. An Excel spreadsheet was developed by the authors to extract data. The data extraction contained details on the included studies and their findings that were relevant to this review. The data were organized into evidence summary tables, and a narrative explanation of the outcomes was provided.
3. Results
The identification and selection of the studies included in this systematic review were represented by the PRISMA flow diagram (Figure 1). The initial search strategy identified 37 publications from databases and other sources. Ten duplicates were removed, leaving 27 publications for title and abstract review. The number of publications for each source after duplicate removal is shown in Table 1. Ten publications were excluded due to irrelevance based on the title and abstract review. A full study review was undertaken on the remaining 17 publications to determine eligibility based on inclusion and exclusion criteria. This process identified 13 studies meeting the study criteria. These publications were subjected to data extraction and analysis of results.

Table 1.
Number of hits for each database after duplicate removal.
3.1. Study Characteristics
The study language, study sample, sample size, location of study sample, study purpose, and study method varied among the included studies (Table 2). In this systematic review, all the studies (N = 13) were published in the English language [18,19,23,24,25,26,27,28,29,30,31,32,33] The study sample involved newborns (n = 5) [18,19,23,25,31], parents/caregivers (n = 7) [24,25,26,29,30,31,33], pediatricians (n = 2) [27,32], and family physicians (n = 1) [28]. The range of sample size in the current systematic review was 1166 to more than one million for newborns, 60 to 1533 for parents, and 67 to 216 for healthcare professionals. The variation in ranges depended on the study method and what data registry was searched. Most studies included samples from all Saudi regions (6 of 13 studies) [19,23,24,26,28,32]. The remaining studies were conducted in Riyadh (n = 3) [18,25,33], Jeddah (n = 1) [27], Riyadh and Dammam (n = 1) [31], Qassim (n = 1) [29], and AlAhsa (n = 1) [30]. Based on the type of sample, most of the studies reported the sample characteristics, such as gender, age, educational level of parents, number of children, monthly income, and years of experience for healthcare professionals. The purpose of conducting the included studies was to examine knowledge, attitudes, and perceptions regarding NHS programs, EHDI services, and hearing loss risk factors (n = 7) [24,26,27,28,29,30,32], investigate rates, such as coverage rate, lost to follow-up (i.e., it indicates that the infant did not receive the recommended diagnosis or treatment) rate, and age of hearing loss identification rate (n = 4) [18,23,25,31], and generally evaluate the status of NHS and early intervention services (n = 2) [19,23]. Data were collected by searching the registries (n = 4) [18,23,25,31], distributing validated questionnaires (n = 8) [24,26,27,28,29,30,32,33], interviewing the target population (n = 2) [25,31], and reviewing the scientific evidence (n = 1) [19].

Table 2.
Characteristics of included studies.
3.2. Strength of Evidence
The research design and the strength of evidence are shown in Table 3. The common study designs used for achieving the aims of the included studies were cross-sectional descriptive study designs that were either prospective (n = 8), retrospective (n = 2), or combining both (n = 2). The strength of evidence for all the included studies was classified as low.

Table 3.
Research design and strength of evidence of included studies.
3.3. Challenges of the NHS Programs
Table 4 summarizes several challenges reported by the included studies that may negatively affect the effectiveness of the NHS programs in Saudi Arabia. It is worth mentioning that not all the included studies directly examined the challenges of the NHS programs; however, some of these challenges were reported as recommendations for improving the NHS programs. The challenges of the NHS programs were as follows: (a) lack of awareness and gaps in knowledge, (b) lost to follow-up, (c) inadequate data entry, management, and tracking system, (d) limited or absence of services in some residential areas, (e) insufficient training and frequent changes of NHS personnel, and (f) absence of a standardized NHS protocol.

Table 4.
Challenges of the NHS programs in Saudi Arabia.
Lack of awareness and gaps in knowledge among parents (n = 10) and healthcare professionals (n = 3) were the main reported challenges [18,19,23,24,25,26,27,28,29,30,31,32,33]. Lost to follow-up was also reported as a major challenge (n = 4) because of several parental and logistic reasons (e.g., failure to remember and unavailable transportation) [18,19,23,25]. Inadequate data entry, management, and tracking system (n = 4), such as not including the diagnostic stage and NHS data of non-MOH and private hospitals in the NHS national registry and the absence of automated data entry, is another challenge [18,19,23,25]. Lack of services in some residential areas that may delay meeting the recommended EHDI timeline (n = 4) was stated as a challenge in the included studies [18,19,31,33]. The other challenge is insufficient training for NHS personnel (n = 3), particularly for effective counseling [18,19,33], and frequent changes in the NHS team, especially trained nurses [19]. Another included study showed that the absence of a standardized NHS protocol among all governmental and non-governmental hospitals was a challenge [18].
4. Discussion
The NHS programs were successfully implemented in Saudi Arabia because of careful planning before the program began and the use of advanced technologies [19]. However, this systematic review showed some challenges of the NHS programs in Saudi Arabia.
4.1. Challenges
4.1.1. Lack of Awareness and Gaps in Knowledge
Ten studies in the current systematic review showed that the lack of parental awareness of NHS and EHDI is a challenge to the NHS programs [18,19,23,24,25,26,29,30,31,33], while three studies revealed that the existing gap in knowledge among healthcare providers (pediatricians and family physicians) is another challenge to the NHS programs [27,28,32]. Scheepers et al. reported that the most common causes for refusing hearing screening are the caregiver’s knowledge of the screening, healthcare professionals’ knowledge and team collaboration, and costs [34]. Pynnonen et al. identified the absence of parental awareness of NHS across the United States [35]. Deficiencies in knowledge about NHS and hearing loss among physicians were also reported in the literature [36,37].
Parental awareness is a major factor in determining the NHS performance and has a direct association with the lost to follow-up rate [18]. Collaborative relationships between parents and healthcare professionals are essential. Parents and families are important team members. The role of parents in the 1–3–6 EHDI timeline is considered a critical component in the family-centered care approach, in which healthcare professionals address the needs of both the patient and his or her family members [38]. Since the patient is an infant, the parents are the family members who are involved in all aspects of clinical care. Hanft et al. reported that this care model requires professionals to inform and support families to make adequate decisions for their children [38]. The family-centered care philosophy and practice improves intervention services, patient’s health condition, patient satisfaction, and family behavior [39,40].
In the United States, the majority of children who are deaf (90–95%) are born to hearing parents [41]. In Saudi Arabia, consanguineous marriage causes a variety of hereditary progressive cochleovestibular malformations, which are linked to both syndromic and non-syndromic hereditary hearing loss [18]. Hearing parents may have different negative emotions (e.g., guilt, anger, confusion, disappointment, and stress) once their child is identified with hearing loss [42,43]. They may also know little or nothing about hearing loss and its consequences and have little to no experience making decisions regarding the choice of communication methods (e.g., spoken language versus signed language), amplification devices, and educational environments [41,43].
The success of children with hearing loss is affected by parents’ education, attitudes (e.g., reactions and acceptance), and encouragement of their child [44]. Parents should be well informed and included in this collaborative work to help them make knowledgeable decisions about their child’s hearing loss. Furthermore, the education about NHS should be extended to include healthcare professionals who have much misinformation regarding the ability to test infant hearing loss and the importance of NHS and follow-up appointments [45]. This misunderstanding could be more pronounced or apparent when there is insufficient equipment, weak training, and a scarcity of qualified personnel [46]. Healthcare professionals should be aware of the NHS program, knowledgeable about the technology used to screen infant hearing, and mindful of the 1–3–6 EHDI timeline.
4.1.2. Lost to Follow-Up
A total of 4 out of 13 included studies reported that lost to follow-up is a challenge to the NHS [18,19,23,25]. Poor follow-up return rate was reported as a challenge to the NHS programs in both developed and less developed countries [34,47,48]. In Saudi Arabia, the lost to follow-up rate is varied. One study estimated the lost to the system (i.e., the combination of lost to follow-up and lost to documentation) at 34.9% [18], while another study estimated the lost to follow-up rate at 18% [25]. As reported earlier, lost to follow-up indicates that the infant did not receive or complete the recommended diagnostic or intervention process [18], while lost to documentation means “infants who did not pass their hearing screening and whose diagnostic or intervention status has not been reported to the EHDI program; thus, their status remains unknown by the EHDI program despite the fact that they may have received services” [49].
According to the Centers for Disease Control and Prevention (CDC), approximately 27.5% of newborns referred for diagnosis following delivery of hearing screen results were lost to follow-up [47]. Parental awareness of the importance of NHS-subsequent follow-up appointments is critical. The primary cause of missing follow-up appointments in Saudi Arabia was stated to be the parental lack of awareness of NHS and follow-up appointments [18,25]. This necessitates rigorous monitoring and follow-up procedures after the first stage of NHS [14]. Increased costs and lack of parental knowledge of the next step following NHS were reported to be the reasons for NHS refusal in South Africa [34]. Parents are not required to pay for NHS because it is covered by the government or medical insurance in Saudi Arabia [19]. Other parental reasons may increase the lost to follow-up rate in Saudi Arabia, such as the lack of awareness, failure to remember, parental health conditions, absence of transportation, and work commitments [25]. Lack of adequate tracking technology may make it difficult to monitor all newborns’ hearing screening data and follow those who did not pass the initial NHS or who have risk factors [50].
4.1.3. Inadequate Data Entry, Management, and Tracking System
Four included studies reported the existence of inadequate data entry, management, and tracking systems as challenges to the NHS programs [18,19,23,25]. The quality of many NHS programs is compromised by the absence of structured and organized databases and data gathering. According to the survey data of individuals involved with the NHS programs in 196 countries, there were no tracking procedures in place for babies who were not screened or for those who did not pass the screening and would need to be sent for audiological diagnosis and treatment services [51]. The lost to follow-up rate is typically high or unknowable in the absence of tracking [51]. The absence of tracking and data collection methods is one factor contributing to the ineffectiveness of follow-up procedures that can be avoided by using appropriate data management systems [52]. Furthermore, frequent data analysis on screening coverage and failure rates should be used as process indicators for the NHS program quality control [53].
In the United States, the EHDI Information System (EHDI-IS) is a tool available in every state and territory used to (a) assist programs in ensuring that all infants receive follow-up services in compliance with the 1–3–6 EHDI timeline, (b) gather data on the prevalence of infants with hearing loss, and (c) provide a variety of relevant data analysis that assists in tracking, surveillance, and assessment of program performance [54]. Alanazi recommended establishing a follow-up center and computer tracking system in Saudi Arabia to reach and notify parents a few days before the recommended visit and use automatic transfer of data from the screeners to the database without being manually inputted [18]. The NHS programs are also recommended to include all data of NHS that is conducted in all hospitals, governmental (whether MOH or non-MOH hospitals) and private, under one national registry [23]. Also, this registry is advised to include the results of the diagnostic stage. The integration of telemedicine components and bidirectional data flow between NHS centers and decentralized screening devices should be considered [51].
4.1.4. Lack of Services in Some Residential Areas
A total of 4 out of 13 included studies reported the absence of services in some Saudi residential areas which may delay meeting the recommended EHDI timeline [18,19,31,33]. The extent to which the EHDI programs are implemented and covered varies widely between countries and even within the regions of the same country [55]. The NHS program has not been implemented for all newborns in the world, particularly in rural areas of poor nations where the required equipment is lacking [56]. For example, half of the European countries have implemented the EHDI programs nationwide, whereas almost all the countries in the Southeast Asia region have not established any NHS programs [55].
The national NHS program has been legislated by the government for all newborns in Saudi Arabia, and the coverage rate of NHS has increased since 2014 [19]. Alkahtani et al. stated no nationwide covering of the NHS program in Saudi Arabia [31]. Alaql reported that the coverage rate of NHS is more than 96% in the MOH hospitals across Saudi Arabia [19]. Alothman et al. estimated the coverage rate of NHS at 92.6% in Saudi Arabia [23]. According to the CDC, the coverage rate of NHS was reported to be 98.4% in the United States [47]. Alyami et al. attributed the delay of EHDI services to the distribution of these services mainly in metropolitan areas, such as Riyadh [33]. The average age of cochlear implantation is 45.7 months in Saudi Arabia, while it is 21.5 months in the United States [57]. Traveling long distances to hospitals where the EHDI services exist is costly for some families, who may need financial assistance [35]. Such challenges were reported in the literature where families face transportation and financial difficulties to reach the EHDI services that existed in only some hospitals [58,59]. Alanazi recommended the expansion of the EHDI services, not only NHS, in all Saudi cities [18].
4.1.5. Insufficient Training and Frequent Changes in the NHS Personnel
Three studies identified the existing insufficient training, particularly effective counseling, for NHS personnel and the frequent change in NHS staff [18,19,33]. The success of the NHS program and the EHDI services generally depends on training healthcare professionals on both technical and communication skills. Healthcare professionals are responsible for guiding parents regarding the outcomes and the following steps in the process. There are a limited number of professionals with knowledge and experience in this field [48]. One factor that affects the standard of patient care in audiology is informational counseling for parents and/or patients [60]. Revealing to parents that their child has hearing loss is a part of the counseling process that depends on breaking bad news. The clinicians must be able to handle this type of situation and provide parents with emotional support.
NHS is mainly performed by nurses who work in well-baby nurseries and neonatal intensive care units; therefore, they play a crucial role as the point of contact for promoting hearing screening, providing parental counseling, and ensuring follow-up care [61]. However, several studies evaluating nurses’ attitudes, knowledge, and behaviors on NHS and early intervention found that nurses often did not know about the various screening protocols, phases of referral, risk factors for hearing loss, or the availability of resources [62,63,64]. This systematic review revealed the existing gaps in knowledge about the NHS programs and the EHDI services among pediatricians and family physicians [27,28,32]. Several studies showed a low level of knowledge about NHS among physicians [65,66]. This gap in knowledge among healthcare professionals could be a result of the lack of appropriate training. Besides audiologists, family physicians, pediatricians, and nurses are on the frontline in dealing with hearing-impaired children and their families. They are responsible for helping parents when breaking bad news if the child did not pass NHS, informing them about the diagnosis and next-step recommendations, and providing take-home information. Through the use of simulation, Alanazi et al. created a curriculum for training on technical and counseling skills related to NHS [67]. Training healthcare professionals is crucial in the process of successfully employing and implementing the NHS program and the 1–3–6 EHDI timeline.
One of the included studies reported that frequent changes in the NHS team, especially trained nurses, may affect the success of the NHS program [19]. Two main barriers to maintaining effective teamwork are the instability of teams and changing roles [68]. The NHS team must be stable because it is not like other healthcare teams, such as trauma teams that are formed for a temporary task. If a new team member joins the NHS program, proper training should be provided. Furthermore, the roles and responsibilities of the NHS team should be clear without any overlap to achieve the effectiveness of the NHS program.
4.1.6. Absence of a Standardized NHS Protocol
One of the included studies reported no unification of the test protocol between governmental and non-governmental hospitals [18]. Typically, the NHS program is a two-phase approach. Before being discharged from the hospital, a newborn is screened in the first few days of life utilizing automated auditory brainstem response (AABR) and/or otoacoustic emissions (OAEs). Both AABR and OAE technologies were recognized as optimal tools for NHS and hearing loss diagnosis. AABR and OAE screeners do not require behavioral responses from the infant or demand interpretation by the hearing screening personnel. This means both hearing screening technologies show either pass or fail/refer, which is ideal for non-audiologist personnel, such as nurses. The newborns will be referred for rescreening (second stage) if they do not pass the initial round within a few days or weeks [18]. This screening includes either one or two phases of OAEs testing, or both OAEs and AABR testing in high-risk cases [69]. The NHS program may follow a three-stage screening strategy, which was suggested to reduce the referral rate [19,25]. The NHS programs at the MOH adopted three AABR screenings for all newborns in Saudi Arabia [18]. While the NHS programs funded by the MOH implements the AABR screening [19], some private hospitals still utilize OAEs. It is recommended to use tympanometry, OAEs, and frequency-specific ABR testing to evaluate the infant’s hearing [18,49].
4.2. Alignment with Global NHS Challenges and Future Research Directions
The NHS programs in Saudi Arabia encounter some challenges that are consistent with global experiences. A significant barrier to the success of NHS programs is the lack of awareness and knowledge among parents. In Saudi Arabia, the included studies in the current systematic review have shown that there are still gaps in knowledge that require further investigation and intervention [18,19,23,24,25,26,29,30,31,33]. Globally, lack of awareness about early identification of hearing loss poses challenges to effective NHS implementation. For example, only 22% of parents in the United States are aware of the appropriate next steps after their child receives a hearing loss diagnosis [70]. Investigating effective methods to educate parents about the importance of early hearing screening and the potential consequences of delayed intervention is necessary. This could include developing culturally appropriate educational materials and community outreach programs. Healthcare providers’ knowledge is also limited as reported by Saudi studies [27,28,32]. For example, nurses are the primary healthcare practitioners who perform NHS [71]; however, they do not receive training on hearing loss, its prevention, its impact on speech and language development, or the importance of referring patients for diagnostic testing [72,73]. The current knowledge gaps among healthcare providers regarding NHS require developing targeted training programs to enhance their understanding and engagement in the screening process.
Both in Saudi Arabia and worldwide, ensuring that infants who fail initial screenings receive timely follow-up assessments is a significant hurdle. In Saudi Arabia, the lack of parental knowledge about follow-up recommendations and the importance of NHS is a common reason for defaults [18,25]. Similarly, global reports indicate that delays and loss to follow-up are prevalent issues, raising concerns about achieving acceptable screening coverage [34,74]. High rates of lost to follow-up significantly compromise the effectiveness of NHS programs. Conducting qualitative studies to understand the specific reasons for lost to follow-up in different populations, considering factors such as cultural beliefs, socioeconomic status, and healthcare accessibility, is important. Interventions aimed at reducing lost to follow-up, such as reminder systems, transportation assistance, and flexible scheduling of follow-up appointments, require development and evaluation.
Effective data management is crucial for monitoring the progress of infants through the NHS process. Inadequate data entry and tracking systems can lead to infants being lost to follow-up and documentation, where their screening status becomes unknown, undermining the program’s effectiveness. In Saudi Arabia, studies have shown deficiencies in data entry, management, and tracking systems which pose significant challenges to the NHS programs [18,19,23,25]. Globally, no tracking systems for infants who were either not screened or did not pass the screening and required audiological evaluation and treatment were reported [51]. The current data management systems used in NHS programs need assessments to identify weaknesses and areas for improvement and explore the development and implementation of robust, user-friendly electronic health record systems that facilitate accurate data entry and real-time tracking of patients through the screening and follow-up process.
Disparities in healthcare infrastructure can result in limited access to NHS services in certain residential areas, particularly in rural or underserved regions. The coverage rate of NHS programs in Saudi Arabia was reported between 92.6 and 96% across Saudi [19,23]. Different coverage rates were reported worldwide. For instance, half of the European countries have implemented nationwide EHDI programs, while nearly all countries in the Southeast Asia region have yet to establish NHS programs [51]. This lack of access can lead to delays in screening and intervention, adversely affecting child development. Studies to map the availability of NHS services, identify regions with limited access, and evaluate the feasibility and effectiveness of deploying mobile hearing screening units to reach underserved areas are suggested.
The quality of NHS programs heavily relies on the expertise of the personnel conducting the screenings. Insufficient training and high staff turnover can lead to inconsistencies in screening practices and affect program outcomes. The included studies recognized the prevailing lack of adequate training, especially in effective counseling for NHS personnel, along with the frequent turnover of NHS staff [18,19,33]. This is consistent with frequently lacking awareness of different screening protocols, referral procedures, hearing loss risk factors, and available resources among healthcare practitioners worldwide, which may stem from insufficient training [62,63,64,65,66]. Developing and assessing standardized training curricula for NHS personnel to ensure consistent and high-quality screenings are recommended. Furthermore, it is advised to investigate factors contributing to staff turnover in NHS programs and develop strategies to improve job satisfaction and retention.
Both in Saudi Arabia and worldwide, variations in screening protocols can lead to inconsistencies in identifying and managing hearing impairments [18,19,75]. The absence of standardized guidelines may result in disparities in care and outcomes. Collaboration with stakeholders should be carried out to develop evidence-based, standardized NHS protocols that can be adapted to different healthcare settings. The effectiveness of standardized protocols in various contexts should be studied and barriers to their adoption identified. By addressing these challenges through targeted research and interventions, NHS programs can be optimized to ensure early detection and intervention for all infants, thereby supporting their developmental potential.
4.3. The Main Limitations of the Included Studies
The main limitations of all included studies in this review were related to not specifically investigating the challenges of the NHS programs. Furthermore, specific limitations to each included study were identified. For example, parents were asked to provide information about their child’s hearing and neonatal hearing screening which may introduce recall bias [26]. Seven studies gathered data through self-administered questionnaires, relying primarily on the participants’ honesty and personal perceptions, which could have led to inaccurate responses [24,26,27,28,29,30,32]. The small sample size was one of the limitations of the included studies [27,28,29,32,33]. The quality of all included studies was low based on their study designs; however, the variation between studies based on study sample, sample size, location of the study sample, study purpose, and study method plays a more significant role in shaping the conclusions than the strength of evidence alone. Specifically, those studies categorized as having lower strength of evidence did not systematically introduce bias in a way that would undermine the overall findings. That said, study designs of the included studies highlight the need for more rigorous, higher-quality studies with strong methodologies and research designs to be implemented in future research. Research is also needed to further investigate the challenges that face the NHS programs in governmental and non-governmental hospitals in Saudi Arabia.
4.4. Limitations of the Current Review
Despite our best efforts, some study limitations were inevitable. Not all databases were accessible for searching for eligible studies. However, additional sources were checked for any research that the first search strategy might have overlooked. The inclusion criteria were open to all types of evidence, so weak study design studies were included in the review. Another drawback of the inclusion criteria was the inclusion of only studies published in and after 2016. The authors provided relevant research findings for each challenge factor; however, the study did not include an analysis of correlations between these factors.
5. Conclusions
The current systematic review explored the challenges of the NHS programs in Saudi Arabia. The included studies were either expert opinion, survey, or database studies. Several challenges were identified. The most common challenge was the lack of awareness and gap in knowledge among parents and healthcare professionals. National education campaigns about the NHS program and the EHDI services are critically needed. Lost to follow-up is a major challenge that requires a dedicated multidisciplinary team, a focus on public awareness, and improved documentation by using suitable database management and tracking systems. This review also identified the need for expanding the EHDI services for children in all regions of Saudi Arabia. The results obtained from the present review may assist in overcoming these challenges and improving the NHS programs in Saudi Arabia.
Author Contributions
A.A.A. conceptualized the study, conducted the literature search and selection process, designed the methodology, validated the results, extracted the data, appraised the studies included in this systematic review, wrote the initial draft, reviewed and edited multiple versions of the draft, provided oversight of the team, and administered the project. N.N. consented to the concept of the study, participated in the literature search and selection process, participated in the methodology design, validated the results, extracted the data, appraised the studies included in this systematic review, co-wrote the initial draft, and reviewed and edited multiple versions of the draft. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Institutional Review Board (IRB) of King Saud bin Abdulaziz University for Health Sciences (KSAU-HS) protocol number (IRB/NRR24/017/4) on 01 May 2024.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Search terms, databases, and search strings.
Table A1.
Search terms, databases, and search strings.
| Search Terms | Database | Search Strings |
|---|---|---|
| Population: newborns, neonates, infants Type: hearing screening in Saudi Arabia Outcomes: challenges, difficulties, threats | PubMed and CINAHL® database searches consisted of MeSH term/CINAHL | Heading newborns (OR) neonates (OR) infants is a major topic combined (AND) with the terms hearing screening (AND) Saudi Arabia. The citations retrieved from this search were further narrowed using the terms (challenges (OR) difficulties (OR) threats). |
Note. CINAHL = Cumulative Index to Nursing and Allied Health Literature; MeSH = Medical Subject Heading.
References
- Cole, E.B.; Flexer, C. Children with Hearing Loss: Developing Listening and Talking: Birth to Six, 4th ed.; Plural: San Diego, CA, USA, 2020. [Google Scholar]
- Grau-Husarikova, E.; Sánchez Pedroche, A.; Mumbardó-Adam, C.; Sanz-Torrent, M. How language affects social cognition and emotional competence in typical and atypical development: A systematic review. Int. J. Lang. Commun. Disord. 2024, 59, 1788–1816. [Google Scholar] [CrossRef] [PubMed]
- Pimperton, H.; Kennedy, C.R. The impact of early identification of permanent childhood hearing impairment on speech and language outcomes. Arch. Dis. Child. 2012, 97, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Hintermair, M. Executive functions and behavioral problems in deaf and hard-of-hearing students at general and special schools. J. Deaf. Stud. Deaf. Educ. 2013, 18, 344–359. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.; Harper, M.; Pedersen, E.; Goman, A.; Suen, J.J.; Price, C.; Applebaum, J.; Hoyer, M.; Lin, F.R.; Reed, N.S. Hearing loss, loneliness, and social isolation: A systematic review. Otolaryngol. Head Neck Surg. 2020, 162, 622–633. [Google Scholar] [CrossRef]
- World Health Organization. Deafness and Hearing Loss. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss (accessed on 19 August 2024).
- Renauld, J.M.; Basch, M.L. Congenital deafness and recent advances towards restoring hearing loss. Curr. Protoc. 2021, 1, e76. [Google Scholar] [CrossRef] [PubMed]
- Abolfotouh, M.; Ghieth, M.M.; Badawi, I.A. Hearing loss and other ear problems among schoolboys in Abha, Saudi Arabia. Ann. Saudi Med. 1995, 15, 323–326. [Google Scholar] [CrossRef]
- Al-Rowaily, M.A.; Alfayez, A.I.; AlJomiey, M.S.; Albadr, A.M.; Abolfotouh, M. Hearing impairments among Saudi preschool children. Int. J. Pediatr. Otorhinolaryngol. 2021, 76, 1674–1677. [Google Scholar] [CrossRef]
- Daghistani, K.J.; Jamal, T.S.; Zakzouk, S.M. The management of hearing impaired Saudi children: An epidemiological survey. Bahrain Med. Bull. 2002, 24, 7–12. Available online: https://www.bahrainmedicalbulletin.com/march_2002/management.pdf (accessed on 3 February 2025).
- Al-Abdiljawad, K.A. Hearing screening of primary school children. Saudi J. Otorhinolaryngol. Head Neck Surg. 2007, 9, 50–52. [Google Scholar]
- Elmalik, S.; Alshawi, S.; AlQahtani, A.M.; AlShammasi, H.S.; Alruwaili, A.; Aldughaim, A.; Alkhalifa, S.A. Descriptive patterns of deafness among pre-school Saudi children aged two to five years visiting neurology clinic from 2012 to 2017. Cureus 2020, 12, e10893. [Google Scholar] [CrossRef]
- Podury, A.; Jiam, N.T.; Kim, M.; Donnenfield, J.I.; Dhand, A. Hearing and sociality: The implications of hearing loss on social life. Front. Neurosci. 2023, 17, 1245434. [Google Scholar] [CrossRef] [PubMed]
- Joint Committee on Infants Hearing. Year 2019 position statement: Principles and guidelines for early hearing detection and intervention programs. J. Early Hear. Detect. Interv. 2019, 4, 1–44. [Google Scholar] [CrossRef]
- Ching, T.Y.; Dillon, H.; Marnane, V.; Hou, S.; Day, J.; Seeto, M.; Crowe, K.; Street, L.; Thomson, J.; Van Buynder, P.; et al. Outcomes of early- and late-identified children at 3 years of age: Findings from a prospective population-based study. Ear Hear. 2013, 34, 535–552. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, B.O.; Luxon, L.M.; Wirz, S.L. Benefits and challenges of newborn hearing screening for developing countries. Int. J. Pediatr. Otorhinolaryngol. 2004, 68, 287–305. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Future programme developments for prevention of deafness and hearing impairment. In Proceedings of the Report of the 4th Informal Consultation, Geneva, Switzerland, 17–18 February 2000. Available online: https://iris.who.int/bitstream/handle/10665/67888/WHO_PDH_02.1.pdf?isAllowed=y&sequence=1 (accessed on 19 August 2024).
- Alanazi, A.A. Referral and lost to system rates of two newborn hearing screening programs in Saudi Arabia. Int. J. Neonatal Screen. 2020, 6, 50. [Google Scholar] [CrossRef]
- Alaql, F.A.M. Realization of successful universal newborn hearing screening program in Saudi Arabia. J. Pediatr. Neonatal Med. 2021, 3, 147. [Google Scholar] [CrossRef]
- Ministry of Health. MOH News: MOH Launches the 1st Phase of Newborn Screening for Hearing Loss and CCHD Program. Available online: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2016-10-09-001.aspx (accessed on 19 August 2024).
- Krishnan, L.A.; Donaldson, L.K. Newborn hearing screening in developing countries: Understanding the challenges and complexities of implementation. Perspect. Glob. Iss. Com. Sci. Relat. Dis. 2013, 3, 54–61. [Google Scholar] [CrossRef]
- Page, M.J.; Mckenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Alothman, N.; Elbeltagy, R.; Mulla, R. Universal newborn hearing screening program in Saudi Arabia: Current insight. J. Otol. 2024, 19, 35–39. [Google Scholar] [CrossRef]
- Khurayzi, T.A.; Gadi, W.H.; Alandijani, H.A.; Almutairi, A.B.; Zogel, B.A.; Akoor, A.A.; Hakami, A.M.; Alsallum, M.H. Parental knowledge and attitudes to childhood hearing loss and hearing services in the Kingdom of Saudi Arabia. Saudi. J. Otorhinolaryngol. Head Neck Surg. 2024, 26, 88–95. [Google Scholar] [CrossRef]
- Alothman, N.; Alotaibi, M.; Alshawairkh, G.; Almutairi, M.; Aldosari, R.; Alblowi, R.; Alqhtany, A. Loss to follow-up in a newborn hearing screening program in Saudi Arabia. Int. J. Pediatr. Otorhinolaryngol. 2023, 172, 111688. [Google Scholar] [CrossRef] [PubMed]
- Almatrafi, M.A.; Alsahaf, N.; Kabli, A.; Maksood, L.; Alharbi, K.; Alsharif, A.; Mujahed, R.A.; Naser, A.Y.; Assaggaf, H.M.; Mosalli, R.; et al. Predictors of parental recall of newborn hearing screening program in Saudi Arabia. Healthcare 2023, 11, 1357. [Google Scholar] [CrossRef] [PubMed]
- Malas, M.; Aboalfaraj, A.; Alamoudi, H.; Kurdi, A.; Alahmadi, T.; Zawawi, F. Pediatricians’ knowledge and attitude toward hearing loss and newborn hearing screening programs. Int. J. Pediatr. Otorhinolaryngol. 2022, 161, 111265. [Google Scholar] [CrossRef] [PubMed]
- Alqudah, O.; Alqudah, S.; Al-Bashaireh, A.M.; Alharbi, N.; Alqudah, A.M. Knowledge, attitude, and management of hearing screening in children among family physicians in the Kingdom of Saudi Arabia. PLoS ONE 2021, 16, e0256647. [Google Scholar] [CrossRef]
- Alsudays, A.M.; Alharbi, A.A.; Althunayyan, F.S.; Alsudays, A.A.; Alanazy, S.M.; Al-Wutay, O.; Alenezi, M.M. Parental knowledge and attitudes to childhood hearing loss and hearing services in Qassim, Saudi Arabia. BMC Pediatr. 2020, 20, 175. [Google Scholar] [CrossRef]
- Al-Yahya, K.; Al-Muneef, A.A.; Al-Majed, F.S.; Alhashem, F.Y.; Al-Khalifah, A.S. Maternal knowledge and awareness of neonatal hearing loss: A local survey from Saudi Arabia. Int. J. Med. Dev. Ctries 2020, 4, 124–129. [Google Scholar] [CrossRef]
- Alkahtani, R.; Rowan, D.; Kattan, N.; Alwan, N.A. Age of identification of sensorineural hearing loss and Characteristics of affected children: Findings from two cross-sectional studies in Saudi Arabia. Int. J. Pediatr. Otorhinolaryngol. 2019, 122, 27–34. [Google Scholar] [CrossRef]
- Almutairi, A.; Alosaimi, M.; Albaik, N.Z.; Abalkhail, S.A.; Al Aqili, N.S.; Sabri, R.H.; Alhiwaishil, H.M.; Baghdadi, A.A.; Alenzi, A.A.; Althobaiti, T.M.; et al. Knowledge, attitude, and practices of Saudi pediatricians regarding newborn hearing screening in Saudi Arabia. Int. J. Pharm. Res. Allied Sci. 2019, 8, 146–152. Available online: https://ijpras.com/article/knowledge-attitude-and-practices-of-saudi-pediatricians-regarding-newborn-hearing-screening-in-saudi-arabia (accessed on 3 February 2025).
- Alyami, H.; Soer, M.; Swanepoel, A.; Pottas, L. Deaf or hard of hearing children in Saudi Arabia: Status of early intervention services. Int. J. Pediatr. Otorhinolaryngol. 2016, 86, 142–149. [Google Scholar] [CrossRef]
- Scheepers, L.J.; Swanepoel, d.W.; Roux, T.l. Why parents refuse newborn hearing screening and default on follow-up rescreening: A South African perspective. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 652–658. [Google Scholar] [CrossRef]
- Pynnonen, M.A.; Handelsman, J.A.; King, E.F.; Singer, D.C.; Davis, M.M.; Lesperance, M.M. Parent perception of newborn hearing screening: Results of a US national survey. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 538–543. [Google Scholar] [CrossRef] [PubMed][Green Version]
- López-Vázquez, M.; Berruecos, P.; Lopez, L.E.; Cacho, J. Attitude and knowledge of hearing loss among medical doctors selected to initiate a residency in Mexico. Int. J. Audiol. 2009, 48, 101–107. [Google Scholar] [CrossRef]
- Moeller, M.P.; White, K.R.; Shisler, L. Primary care physicians’ knowledge, attitudes, and practices related to newborn hearing screening. Pediatrics 2006, 118, 1357–1370. [Google Scholar] [CrossRef] [PubMed]
- Hanft, B.; Shepherd, J.; Read, J. Pediatric therapy teams. In Kids Can Be Kids; Lane, S., Bundy, A., Eds.; F.A. Davis: Philadelphia, PA, USA, 2012; pp. 273–296. [Google Scholar]
- Kuhlthau, K.A.; Bloom, S.; Van Cleave, J.; Knapp, A.A.; Romm, D.; Klatka, K.; Homer, C.J.; Newacheck, P.W.; Perrin, J.M. Evidence for family-centered care for children with special health care needs: A systematic review. Acad. Pediatr. 2011, 11, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.L.; Roter, D.L. Hidden in plain sight: Medical visit companions as a resource for vulnerable older adults. Arch. Intern. Med. 2008, 168, 1409–1415. [Google Scholar] [CrossRef]
- Mitchell, R.E.; Karchmer, M.A. Chasing the mythical ten percent: Parental hearing status of deaf and hard of hearing students in the United States. Sign Lang. Stud. 2004, 4, 138–163. Available online: http://www.jstor.org/stable/26190985 (accessed on 3 February 2025).
- Luterman, D. Counseling families with a hearing-impaired child. Otolaryngol. Clin. N. Am. 1999, 32, 1037–1050. [Google Scholar] [CrossRef]
- Meadow-Orlans, K.P.; Koester, L.S.; Spencer, P.E.; MacTurk, R.H. Theoretical rationale for the longitudinal study. In The World of Deaf Infants: A Longitudinal Study; Meadow-Orlans, K.R., Spencer, P.E., Koester, L.S., Eds.; Oxford University Press: New York, NY, USA, 2004; pp. 11–23. [Google Scholar]
- Moeller, M.P. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics 2000, 106, E43. [Google Scholar] [CrossRef]
- Meyer, M.E.; Swanepoel, d.W. Newborn hearing screening in the private health care sector: A national survey. S. Afr. Med. J. 2011, 101, 665–667. [Google Scholar]
- Theunissen, M.; Swanepoel, D. Early hearing detection and intervention services in the public health sector in South Africa. Int. J. Audiol. 2008, 47, S23–S29. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. 2019 Summary of National CDC EHDI Data. 2023. Available online: https://www.cdc.gov/ncbddd/hearingloss/2019-data/01-data-summary.html (accessed on 21 August 2024).
- American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007, 120, 898–921. [Google Scholar] [CrossRef]
- American Speech-Language-Hearing Association. Loss to Follow-Up in Early Hearing Detection and Intervention. Available online: https://www.infanthearing.org/coordinator_toolkit/section14/46_follow_up.pdf (accessed on 21 August 2024).
- Gambacorta, V.; Orzan, E.; Molini, E.; Lapenna, R.; Paniconi, M.; Di Giovanni, A.; Faralli, M.; Ricci, G. Critical Issues in the management of newborn hearing screening in the time of COVID-19 in Umbria, Italy. Children 2022, 9, 1736. [Google Scholar] [CrossRef] [PubMed]
- Neumann, K.; Mathmann, P.; Chadha, S.; Euler, H.A.; White, K.R. Newborn hearing screening benefits children, but global disparities persist. J. Clin. Med. 2022, 11, 271. [Google Scholar] [CrossRef] [PubMed]
- Ravi, R.; Gunjawate, D.R.; Yerraguntla, K.; Lewis, L.E.; Driscoll, C.; Rajashekhar, B. Follow-up in newborn hearing screening: A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2016, 90, 29–36. [Google Scholar] [CrossRef]
- World Health Organization. Ear and Hearing Care-Planning and Monitoring of National Strategies: A Manual; World Health Organization: Geneva, Switzerland, 2015; Available online: https://www.who.int/publications/i/item/ear-and-hearing-care-planning-and-monitoring-of-national-strategies (accessed on 21 August 2024).
- Sanchez-Gomez, M.C.; Dundon, K.; Deng, X. Evaluating data quality of newborn hearing screening. J. Early Hear. Detect. Interv. 2019, 4, 26–32. [Google Scholar] [CrossRef]
- World Health Organization. Current Issues and Guiding Principles for Action. 2010. Available online: https://portaldeboaspraticas.iff.fiocruz.br/wp-content/uploads/2021/08/Newborn_and_Infant_Hearing_Screening_Report.pdf (accessed on 22 August 2024).
- Lawrensia, S.; Pomar, E.G. Newborn Hearing Screening; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560930/ (accessed on 22 August 2024).
- Al-Sayed, A.A.; AlSanosi, A. Cochlear implants in children: A cross-sectional investigation on the influence of geographic location in Saudi Arabia. J. Fam. Community Med. 2017, 24, 118–121. [Google Scholar] [CrossRef]
- Limb, S.J.; McManus, M.A.; Fox, H.B.; White, K.R.; Forsman, I. Ensuring financial access to hearing AIDS for infants and young children. Pediatrics 2010, 126, S43–S51. [Google Scholar] [CrossRef]
- Olusanya, B.O.; Wirz, S.L.; Luxon, L.M. Community-based infant hearing screening for early detection of permanent hearing loss in Lagos, Nigeria: A cross-sectional study. Bull. World Health Organ. 2008, 86, 956–963. [Google Scholar] [CrossRef]
- English, K. Informing parents of their child’s hearing loss: Breaking bad news guidelines for audiologists. Schol. Spee. Lang. Pathol. Audiol. 2004, 16, 185. Available online: http://ideaexchange.uakron.edu/speech_ideas/185 (accessed on 3 February 2025).
- Sharma, R.; Gu, Y.; Ching, T.Y.C.; Marnane, V.; Parkinson, B. Economic evaluations of childhood hearing loss screening programmes: A systematic review and critique. Appl. Health Econ. Health Policy 2019, 17, 331–357. [Google Scholar] [CrossRef]
- Barbosa, C.P.; Aires, J.B.; Farias, I.Y.; Linhares, F.M.; Griz, S.M. Newborn and infant hearing health education for nursing professionals. Brazil. J. Otorhinolaryngol. 2013, 79, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Goedert, M.H.; Moeller, M.P.; White, K.R. Midwives’ knowledge, attitudes, and practices related to newborn hearing screening. J. Midwifery Women Health 2011, 56, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Sanju, K.H.; Aggarwal, K.; Choudhary, M.; Yadav, K.A. Knowledge and attitude of nurses towards infant hearing impairment in North India. Indian J. Anat. Surg. Head Neck Brain 2018, 4, 9–13. [Google Scholar] [CrossRef]
- Ross, D.S.; Visser, S.N. Pediatric primary care physicians’ practices regarding newborn hearing screening. J. Prim. Care Community Health 2012, 3, 256–263. [Google Scholar] [CrossRef]
- Zaitoun, M.; Rawashdeh, M.; AlQudah, S.; ALMohammad, H.; Nuseir, A.; Al-Tamimi, F. Knowledge and practice of hearing screening and hearing loss management among ear, nose, and throat physicians in Jordan. Int. Arch. Otorhinolaryngol. 2021, 25, e98–e107. [Google Scholar] [CrossRef]
- Alanazi, A.A.; Nicholson, N.; Atcherson, S.R.; Franklin, C.; Anders, M.; Nagaraj, N.; Franklin, J.; Highley, P. Use of baby Isao simulator and standardized parents in hearing screening and parent counseling education. Am. J. Audiol. 2016, 25, 211–223. [Google Scholar] [CrossRef]
- Babiker, A.; El Husseini, M.; Al Nemri, A.; Al Frayh, A.; Al Juryyan, N.; Faki, M.O.; Assiri, A.; Al Saadi, M.; Shaikh, F.; Al Zamil, F. Health care professional development: Working as a team to improve patient care. Sudan. J. Paediatr. 2014, 14, 9–16. [Google Scholar]
- Wroblewska-Seniuk, K.E.; Dabrowski, P.; Szyfter, W.; Mazela, J. Universal newborn hearing screening: Methods and results, obstacles, and benefits. Pediatr. Res. 2017, 81, 415–422. [Google Scholar] [CrossRef]
- White, K.R. Early hearing detection and intervention programs: Opportunities for genetic services. Am. J. Med. Genet. 2004, 130, 29–36. [Google Scholar] [CrossRef]
- Alanazi, A.A.; Alothman, N.I.; AlHarbi, M.F.; Alkhalaf, A.; Almsened, A.; Alzahrani, M.; Alsawaji, H. Evaluation of newborn hearing screening programs in Riyadh, Saudi Arabia: A mixed methods study. J. Nat. Sci. Med. 2025, 8, 81–92. [Google Scholar] [CrossRef]
- Barbosa, C.P.; Griz, S.M.S. Health education regarding newborn screening: An integrative review. Rev. CEFAC 2014, 16, 643–650. [Google Scholar] [CrossRef][Green Version]
- Van der Linde, J.; Kritzinger, A. Perceptions of rural primary health care personnel about expansion of early communication intervention. Afr. J. Prim. Health Care Fam. Med. 2013, 5, 553–564. [Google Scholar] [CrossRef]
- Juarez, J.M.; Shaffer, A.D.; Chi, D.H. Follow-up after failed newborn hearing screening: Parental and primary care provider awareness. Am. J. Otolaryngol. 2020, 41, 102614. [Google Scholar] [CrossRef]
- Kanji, A.; Khoza-Shangase, K.; Moroe, N. Newborn hearing screening protocols and their outcomes: A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2018, 115, 104–109. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).