The Effect of Hearing Aid Amplification on Gait Parameters: A Pilot Study Using Ear-Worn Motion Sensors
Abstract
1. Introduction
2. Data Collection
2.1. Participants
2.2. Hearing Aid Fitting
2.3. Inertial Sensors
2.4. Recording Procedure
- BaseSpeech: single-task listening—performing the Freiburger monosyllabic word recognition test while sitting in a quiet environment;
- BaseWalk: single-task walking;
- DTCalc: arithmetic dual task—continuously subtract 3 starting from 100 while walking;
- DTListen: listening dual task—performing the Freiburger monosyllabic word recognition test while walking.
| Characteristic | Mean ± Std | ||
|---|---|---|---|
| Total | 25 | ||
| Gender (m/f) | 20% female | ||
| Age (years) | 68.2 ± 16.0 | ||
| Height (cm) | 176.5 ± 7.7 | ||
| Weight (kg) | 78.2 ± 13.1 | ||
| PTA4 (dB) | 39.9 ± 11.3 | ||
| Assessments | Mean ± Std | [Min, Max] | Category |
| TUG (s) | 9.0 ± 1.2 | [6.9, 11.7] | 0 fall risk [32] |
| MoCA | 26.0 ± 2.1 | [22, 30] | 15 no impairment 10 MCI * [33] |
| FES-I | 18.7 ± 2.7 | [16, 26] | 24 no fall risk 1 fall risk [34] |
| SPPB | 10.5 ± 1.23 | [8, 12] | 20 no DIS 5 mild DIS ** [28] |
3. Methods
3.1. Gait Parameter Estimation
3.1.1. Ear-Worn Sensors
3.1.2. Foot-Worn Sensors
3.2. Statistics
3.3. Evaluation
4. Results
4.1. Effects on Speech Intelligibility
4.2. Effects on Gait
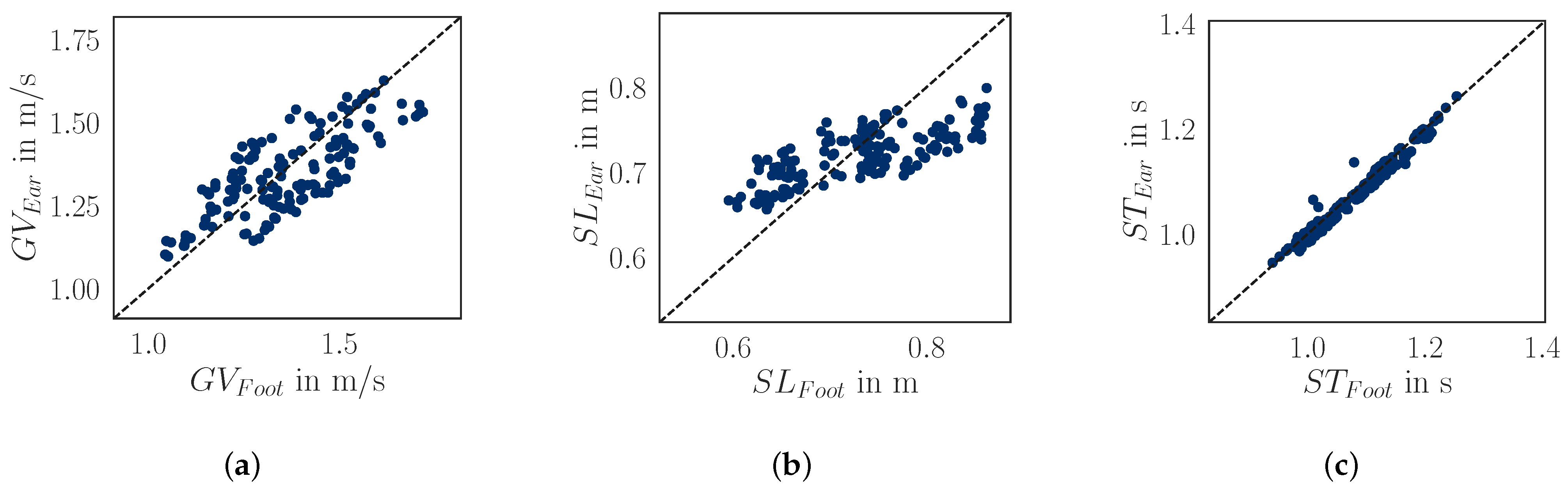
4.3. Ear vs. Foot Sensors
5. Discussion
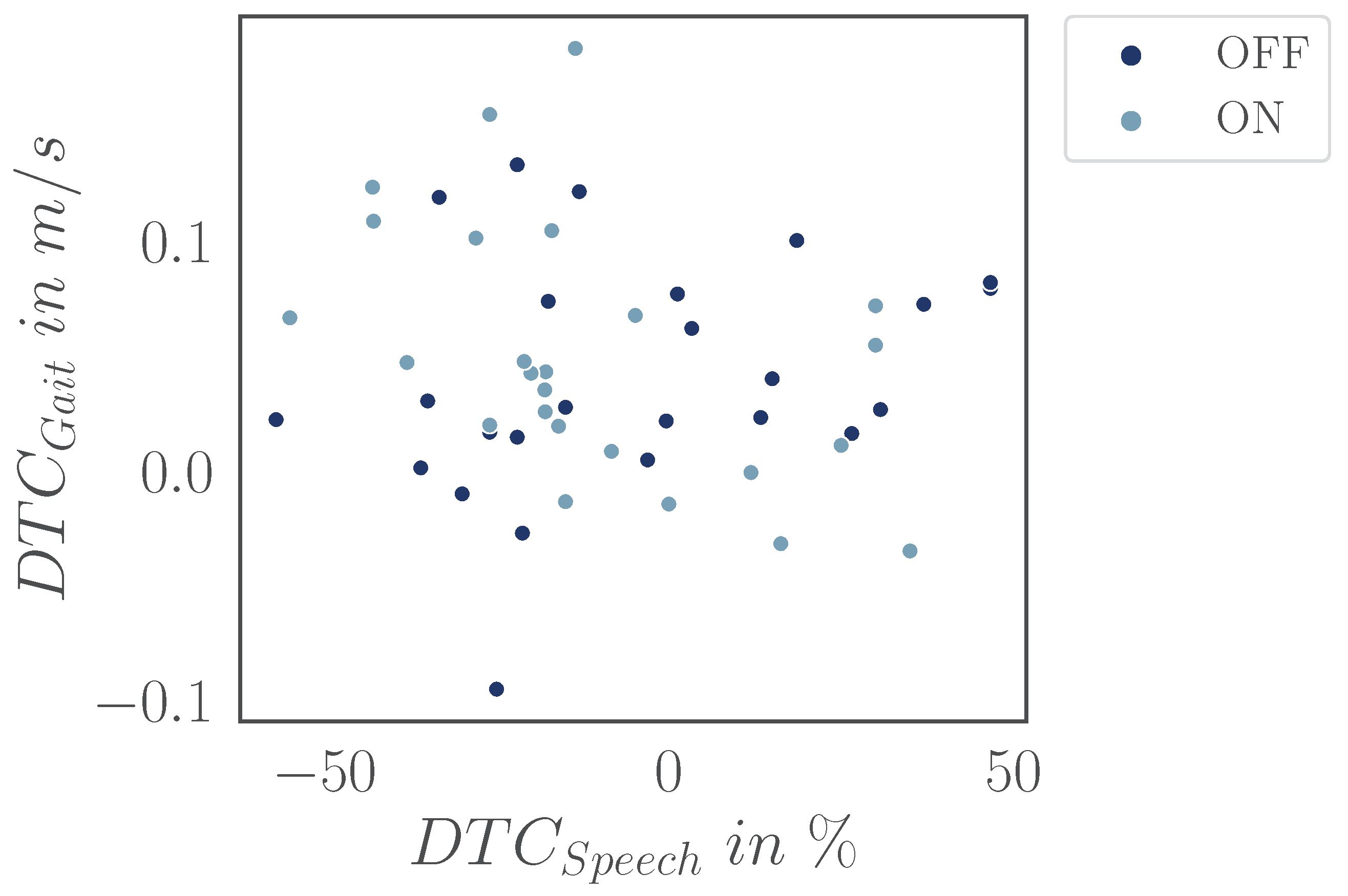
5.1. DTCs—Always Check Your DTCs
5.2. Negligible Impact of HA in Simple Environments
5.3. Individuals Showing Benefits
5.4. Need for Standardized Acoustic DT
5.5. Reliable Accuracy of Gait Algorithms for Ear-Worn Devices
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AE | Absolute error |
| APE | Absolute percentage error |
| DT | Dual-task |
| DTC | Dual-task cost |
| HA | Hearing aid |
| HL | Hearing loss |
| IMU | Inertial measurement unit |
| RM ANOVA | Repeated-measures ANOVA |
| STD | Standard deviation |
| WRP | Word recognition performance |
Appendix A
Appendix A.1

| Gait Velocity in m/s | Step Length in m | Stride Time in s | |||||
|---|---|---|---|---|---|---|---|
| HA Status | Mean | Std | Mean | Std | Mean | Std | |
| All | All | 1.343 | 0.120 | 0.720 | 0.029 | 1.082 | 0.072 |
| OFF | 1.340 | 0.117 | 0.719 | 0.028 | 1.083 | 0.070 | |
| ON | 1.346 | 0.125 | 0.721 | 0.030 | 1.080 | 0.074 | |
| BaseGait | All | 1.380 | 0.120 | 0.730 | 0.029 | 1.067 | 0.068 |
| OFF | 1.374 | 0.120 | 0.730 | 0.029 | 1.074 | 0.070 | |
| ON | 1.387 | 0.122 | 0.731 | 0.030 | 1.060 | 0.068 | |
| DTCalc | All | 1.312 | 0.118 | 0.714 | 0.028 | 1.099 | 0.077 |
| OFF | 1.312 | 0.112 | 0.713 | 0.025 | 1.096 | 0.074 | |
| ON | 1.312 | 0.127 | 0.715 | 0.030 | 1.102 | 0.081 | |
| DTListen | All | 1.336 | 0.114 | 0.715 | 0.029 | 1.078 | 0.068 |
| OFF | 1.334 | 0.114 | 0.714 | 0.029 | 1.078 | 0.068 | |
| ON | 1.338 | 0.118 | 0.717 | 0.029 | 1.078 | 0.069 | |
| Gait Velocity | Step Length | ||||||
|---|---|---|---|---|---|---|---|
| t(23) | p | Hedges’ g | t(23) | p | Hedges’ g | ||
| BaseGait | DTCalc | 6.445 | <0.001 *** | 0.565 | 5.423 | <0.001 *** | 0.567 |
| DTListen | 4.409 | 0.001 ** | 0.369 | 5.353 | <0.001 *** | 0.512 | |
| DTCalc | DTListen | −3.209 | 0.012 * | −0.204 | −0.466 | >0.99 | −0.040 |
| Stride Time | |||||||
| OFF | ON | ||||||
| t(23) | p | Hedges’ g | t(23) | p | Hedges’ g | ||
| BaseGait | DTCalc | −3.304 | 0.019 * | −0.303 | −6.568 | <0.001 *** | −0.554 |
| DTListen | −0.563 | >0.999 | −0.048 | −4.212 | 0.002 ** | −0.255 | |
| DTCalc | DTListen | 4.984 | <0.001 *** | 0.259 | 3.656 | 0.008 ** | 0.319 |
| Gait Velocity | Step Length | Stride Time | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure | F(2, 46) | p | F(2, 46) | p | F(2, 46) | p | |||
| Task | 32.962 | <0.001 *** | 0.040 | 22.246 | <0.001 *** | 0.017 | 30.259 | <0.001 *** | 0.037 |
| HA status | 0.767 | 0.390 | 0.000 | 1.214 | 0.282 | 0.000 | 0.098 | 0.757 | 0.000 |
| Task: HA status | 0.974 | 0.380 | 0.00 | 0.626 | 0.530 | 0.000 | 4.361 | 0.020 * | 0.001 |
References
- World Health Organization—WHO. Deafness and Hearing Loss. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss (accessed on 17 February 2025).
- Lawrence, B.J.; Jayakody, D.M.P.; Bennett, R.J.; Eikelboom, R.H.; Gasson, N.; Friedland, P.L. Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis. Gerontologist 2020, 60, e137–e154. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Yaffe, K.; Xia, J.; Xue, Q.L.; Harris, T.B.; Purchase-Helzner, E.; Satterfield, S.; Ayonayon, H.N.; Ferrucci, L.; Simonsick, E.M.; et al. Hearing loss and cognitive decline in older adults. JAMA Intern. Med. 2013, 173, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Agmon, M.; Lavie, L.; Doumas, M. The association between hearing loss, postural control, and mobility in older adults: A systematic review. J. Am. Acad. Audiol. 2017, 28, 575–588. [Google Scholar] [CrossRef] [PubMed]
- Besser, J.; Stropahl, M.; Urry, E.; Launer, S. Comorbidities of hearing loss and the implications of multimorbidity for audiological care. Hear. Res. 2018, 369, 3–14. [Google Scholar] [CrossRef]
- Martinez-Amezcua, P.; Powell, D.; Kuo, P.L.; Reed, N.S.; Sullivan, K.J.; Palta, P.; Szklo, M.; Sharrett, R.; Schrack, J.A.; Lin, F.R.; et al. Association of age-related hearing impairment with physical functioning among community-dwelling older adults in the US. JAMA Netw. Open 2021, 4, e2113742. [Google Scholar] [CrossRef]
- Foster, J.I.; Williams, K.L.; Timmer, B.H.B.; Brauer, S.G. The association between hearing impairment and postural stability in older adults: A systematic review and meta-analysis. Trends Hear. 2022, 26, 233121652211441. [Google Scholar] [CrossRef]
- Viljanen, A.; Kaprio, J.; Pyykkö, I.; Sorri, M.; Pajala, S.; Kauppinen, M.; Koskenvuo, M.; Rantanen, T. Hearing as a predictor of falls and postural balance in older female twins. J. Gerontol. Ser. Biol. Sci. Med Sci. 2009, 64A, 312–317. [Google Scholar] [CrossRef]
- Chen, D.S.; Betz, J.; Yaffe, K.; Ayonayon, H.N.; Kritchevsky, S.; Martin, K.R.; Harris, T.B.; Purchase-Helzner, E.; Satterfield, S.; Xue, Q.L.; et al. Association of hearing impairment with declines in physical functioning and the risk of disability in older adults. J. Gerontol. Ser. Biol. Sci. Med Sci. 2015, 70, 654–661. [Google Scholar] [CrossRef]
- Bessot, N.; Denise, P.; Toupet, M.; Van Nechel, C.; Chavoix, C. Interference between walking and a cognitive task is increased in patients with bilateral vestibular loss. Gait Posture 2012, 36, 319–321. [Google Scholar] [CrossRef]
- Wollesen, B.; Scrivener, K.; Soles, K.; Billy, Y.; Leung, A.; Martin, F.; Iconomou, N.; McMahon, C.; Dean, C. Dual-task walking performance in older persons with hearing impairment: Implications for interventions from a preliminary observational study. Ear Hear. 2018, 39, 337–343. [Google Scholar] [CrossRef]
- Viljanen, A.; Kaprio, J.; Pyykkö, I.; Sorri, M.; Koskenvuo, M.; Rantanen, T. Hearing acuity as a predictor of walking difficulties in older women. J. Am. Geriatr. Soc. 2009, 57, 2282–2286. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, A.; Tun, P.A.; McCoy, S.L. Hearing loss in older adulthood: What it is and how it interacts with cognitive performance. Curr. Dir. Psychol. Sci. 2005, 14, 144–148. [Google Scholar] [CrossRef]
- Campos, J.; Ramkhalawansingh, R.; Pichora-Fuller, M.K. Hearing, self-motion perception, mobility, and aging. Hear. Res. 2018, 369, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, M.V.; Slade, K.; Kingsnorth, A.P.; Urry, E.; Maidment, D.W. Can hearing aids improve physical activity in adults with hearing loss? A feasibility study. Audiol. Res. 2025, 15, 5. [Google Scholar] [CrossRef]
- Martinez-Amezcua, P.; Kuo, P.L.; Reed, N.S.; Simonsick, E.M.; Agrawal, Y.; Lin, F.R.; Deal, J.A.; Ferrucci, L.; Schrack, J.A. Association of hearing impairment with higher-level physical functioning and walking endurance: Results from the Baltimore Longitudinal Study of Aging. J. Gerontol. Ser. A 2021, 76, e290–e298. [Google Scholar] [CrossRef]
- Mahafza, M.T.; Wilson, W.J.; Brauer, S.; Timmer, B.H.B.; Hickson, L. A systematic review of the effect of hearing aids on static and dynamic balance in adults with hearing impairment. Trends Hear. 2022, 26, 233121652211210. [Google Scholar] [CrossRef]
- Borsetto, D.; Corazzi, V.; Franchella, S.; Bianchini, C.; Pelucchi, S.; Obholzer, R.; Soulby, A.J.; Amin, N.; Ciorba, A. The influence of hearing aids on balance control: A systematic review. Audiol. Neurotol. 2021, 26, 209–217. [Google Scholar] [CrossRef]
- Röddiger, T.; Clarke, C.; Breitling, P.; Schneegans, T.; Zhao, H.; Gellersen, H.; Beigl, M. Sensing with earables: A systematic literature review and taxonomy of phenomena. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2022, 6, 1–57. [Google Scholar] [CrossRef]
- Diao, Y.; Ma, Y.; Xu, D.; Chen, W.; Wang, Y. A novel gait parameter estimation method for healthy adults and postoperative patients with an ear-worn sensor. Physiol. Meas. 2020, 41, 05NT01. [Google Scholar] [CrossRef]
- Decker, J.; Boborzi, L.; Schniepp, R.; Jahn, K.; Wuehr, M. Mobile spatiotemporal gait segmentation using an ear-worn motion sensor and deep learning. Sensors 2024, 24, 6442. [Google Scholar] [CrossRef]
- Seifer, A.K.; Dorschky, E.; Küderle, A.; Moradi, H.; Hannemann, R.; Eskofier, B.M. EarGait: Estimation of temporal gait parameters from hearing aid integrated inertial sensors. Sensors 2023, 23, 6565. [Google Scholar] [CrossRef] [PubMed]
- Seifer, A.K.; Küderle, A.; Dorschky, E.; Moradi, H.; Hannemann, R.; Eskofier, B.M. Step length and gait speed estimation using a hearing aid integrated accelerometer: A comparison of different algorithms. IEEE J. Biomed. Health Inform. 2024, 28, 6619–6628. [Google Scholar] [CrossRef] [PubMed]
- Freepik. Designed by Stories Freepik. Available online: www.freepik.com (accessed on 11 November 2024).
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Dias, N.; Kempen, G.; Todd, C.; Beyer, N.; Freiberger, E.; Piot-Ziegler, C.; Yardley, L.; Hauer, K. The German version of the falls efficacy scale-international version (FES-I). Z. Gerontol. Geriatr. 2006, 39, 297–300. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Pavasini, R.; Guralnik, J.; Brown, J.C.; di Bari, M.; Cesari, M.; Landi, F.; Vaes, B.; Legrand, D.; Verghese, J.; Wang, C.; et al. Short physical performance battery and all-cause mortality: Systematic review and meta-analysis. BMC Med. 2016, 14, 1–9. [Google Scholar] [CrossRef]
- Keidser, G.; Dillon, H.; Carter, L.; O’Brien, A. NAL-NL2 empirical adjustments. Trends Amplif. 2012, 16, 211–223. [Google Scholar] [CrossRef]
- Hahlbrock, K.H. Über Sprachaudiometrie und neue Wörterteste. Arch. Ohren-Nasen-und Kehlkopfheilkd. 1953, 162, 394–431. [Google Scholar] [CrossRef]
- Amboni, M.; Barone, P.; Hausdorff, J.M. Cognitive contributions to gait and falls: Evidence and implications. Mov. Disord. 2013, 28, 1520–1533. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [CrossRef]
- Dalrymple-Alford, J.; MacAskill, M.; Nakas, C.; Livingston, L.; Graham, C.; Crucian, G.; Melzer, T.; Kirwan, J.; Keenan, R.; Wells, S.; et al. The MoCA: Well-suited screen for cognitive impairment in Parkinson disease. Neurology 2010, 75, 1717–1725. [Google Scholar] [CrossRef] [PubMed]
- Delbaere, K.; Close, J.C.T.; Mikolaizak, A.S.; Sachdev, P.S.; Brodaty, H.; Lord, S.R. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing 2010, 39, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Seifer, A.K.; Küderle, A. EarGait: A Gait Analysis Package for Ear-Worn IMU Sensors. (GitHub, Version 2.11.0). 2022. Available online: https://github.com/mad-lab-fau/eargait (accessed on 5 September 2024).
- Küderle, A.; Ullrich, M.; Roth, N.; Ollenschläger, M.; Ibrahim, A.A.; Moradi, H.; Richer, R.; Seifer, A.K.; Zürl, M.; Sîmpetru, R.C.; et al. Gaitmap—An open ecosystem for IMU-based human gait analysis and algorithm benchmarking. IEEE Open J. Eng. Med. Biol. 2024, 5, 163–172. [Google Scholar] [CrossRef]
- Pingouin: Pingouin Is an Open-Source Statistical Package Written in Python. Version 0.5.4. Available online: https://pingouin-stats.org (accessed on 2 February 2025).
- Lövdén, M.; Schaefer, S.; Pohlmeyer, A.E.; Lindenberger, U. Walking variability and working-memory load in aging: A dual-process account relating cognitive control to motor control performance. J. Gerontol. 2008, 63, 121–128. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Muir, S.W.; Speechley, M. Dual-task complexity affects gait in people with mild cognitive impairment: The interplay between gait variability, dual tasking, and risk of falls. Arch. Phys. Med. Rehabil. 2012, 93, 293–299. [Google Scholar] [CrossRef]
- Smith, E.; Cusack, T.; Blake, C. The effect of a dual task on gait speed in community dwelling older adults: A systematic review and meta-analysis. Gait Posture 2016, 44, 250–258. [Google Scholar] [CrossRef]
- Beurskens, R. Does the walking task matter? Influence of different walking conditions on dual-task performances in young and older persons. Hum. Mov. Sci. 2013, 32, 1456–1466. [Google Scholar] [CrossRef]
- Beauchet, O.; Dubost, V.; Aminian, K.; Gonthier, R.; Kressig, R.W. Dual-task-related gait changes in the elderly: Does the type of cognitive task matter? J. Mot. Behav. 2005, 37, 259–264. [Google Scholar]
- Hausdorff, J.M.; Schweiger, A.; Herman, T.; Yogev-Seligmann, G.; Giladi, N. Dual-task decrements in gait: Contributing factors among healthy older adults. J. Gerontol. Ser. Biol. Sci. Med Sci. 2008, 63, 1335–1343. [Google Scholar] [CrossRef]
- Lee, J.; Park, S. Effects of a priority-based dual task on gait velocity and variability in older adults with mild cognitive impairment. J. Exerc. Rehabil. 2018, 14, 993–997. [Google Scholar] [CrossRef]
- Yogev-Seligmann, G.; Rotem-Galili, Y.; Mirelman, A.; Dickstein, R.; Giladi, N.; Hausdorff, J.M. How does explicit prioritization alter walking during dual-task performance? Effects of age and sex on gait speed and variability. Phys. Ther. 2010, 90, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Alberti, G.; Portelli, D.; Loteta, S.; Galletti, C.; D’Angelo, M.; Ciodaro, F. Open-fitting hearing aids: A comparative analysis between open behind-the-ear and open completely-in-the-canal instant-fit devices. Eur. Arch. Oto-Rhino-Laryngol. 2024, 281, 6009–6019. [Google Scholar] [CrossRef] [PubMed]
- Weaver, T.; Shayman, C.; Hullar, T. The effect of hearing aids and cochlear implants on balance during gait. Otol. Neurotol. 2017, 38, 1327–1332. [Google Scholar] [CrossRef] [PubMed]
- Cornwell, T.; Woodward, J.; Wu, M.; Jackson, B.; Souza, P.; Siegel, J.; Dhar, S.; Gordon, K.E. Walking with ears: Altered auditory feedback impacts gait step length in older adults. Front. Sport. Act. Living 2020, 2, 38. [Google Scholar] [CrossRef]
- Shayman, C.S.; Earhart, G.M.; Hullar, T.E. Improvements in gait with hearing aids and cochlear implants. Otol. Neurotol. 2017, 38, 484–486. [Google Scholar] [CrossRef]
- Lau, S.T.; Pichora-Fuller, M.K.; Li, K.Z.H.; Singh, G.; Campos, J.L. Effects of hearing loss on dual-task performance in an audiovisual virtual reality simulation of listening while walking. J. Am. Acad. Audiol. 2016, 27, 567–587. [Google Scholar] [CrossRef]
- Hollman, J.H.; Watkins, M.K.; Imhoff, A.C.; Braun, C.E.; Akervik, K.A.; Ness, D.K. A comparison of variability in spatiotemporal gait parameters between treadmill and overground walking conditions. Gait Posture 2016, 43, 204–209. [Google Scholar] [CrossRef]
- Lazzarini, B.; Kataras, T.J. Treadmill walking is not equivalent to overground walking for the study of walking smoothness and rhythmicity in older adults. Gait Posture 2016, 46, 42–46. [Google Scholar] [CrossRef]
- Gorecka, M.M.; Vasylenko, O.; Rodríguez-Aranda, C. Dichotic listening while walking: A dual-task paradigm examining gait asymmetries in healthy older and younger adults. J. Clin. Exp. Neuropsychol. 2020, 42, 794–810. [Google Scholar] [CrossRef]
- Murray, D.; Viani, L.; Garvan, J.; Murphy, A.; Vance, R.; Simoes-Franklin, C.; Smith, J.; Meldrum, D. Balance, gait and dizziness in adult cochlear implant users: A cross sectional study. Cochlear Implant. Int. 2020, 21, 46–52. [Google Scholar] [CrossRef]
- Kaczmarczyk, K.; Błażkiewicz, M.; Wiszomirska, I.; Pietrasik, K.; Zdrodowska, A.; Wit, A.; Barton, G.; Skarżyński, H. Assessing Gait Stability before and after Cochlear Implantation. BioMed Res. Int. 2019, 2019, 1–8. [Google Scholar] [CrossRef]



| WRP in % Task | OFF | ON | |
|---|---|---|---|
| Sitting | 61.0 ± 21.8 | 84.2 ± 12.2 | |
| Walking | 54.2 ± 21.5 | 71.2 ± 17.5 | |
| RM ANOVA Measure | F(1, 24) | p | |
| Task | 2.876 | 0.103 | 0.043 |
| HA status | 43.570 | <0.001 *** | 0.240 |
| Task:HA status | 1.972 | 0.173 | 0.008 |
| DTCGait | DTCSpeech | ||||
|---|---|---|---|---|---|
| Dual Task | HA Status | Gait Velocity in m/s | Step Length in m | Stride Time in s | WRP in % |
| DTCalc | OFF | −0.061 | −0.017 | 0.022 | |
| ON | −0.075 | −0.015 | 0.042 | ||
| DTListen | OFF | −0.040 | −0.016 | 0.003 | −4.7 |
| ON | −0.049 | −0.014 | 0.018 | −11.2 | |
| Gait Velocity | Step Length | Stride Time | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure | F(2, 46) | p | F(2, 46) | p | F(2, 46) | p | |||
| Task | 26.744 | <0.001 *** | 0.055 | 21.551 | <0.001 *** | 0.064 | 22.200 | <0.001 *** | 0.035 |
| HA status | 1.490 | 0.235 | 0.001 | 2.368 | 0.137 | 0.001 | 0.723 | 0.404 | 0.000 |
| Task:HA status | 0.727 | 0.468 | 0.001 | 0.138 | 0.845 | 0.000 | 6.085 | 0.005 ** | 0.004 |
| AE | APE | Pearson | |
|---|---|---|---|
| Mean ± Std | Mean ± Std | Correlation r | |
| Gait velocity | m/s | 0.75 | |
| Step length | m | 0.74 | |
| Stride time | s | 0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifer, A.-K.; Küderle, A.; Strobel, K.; Hannemann, R.; Eskofier, B.M. The Effect of Hearing Aid Amplification on Gait Parameters: A Pilot Study Using Ear-Worn Motion Sensors. Audiol. Res. 2025, 15, 45. https://doi.org/10.3390/audiolres15030045
Seifer A-K, Küderle A, Strobel K, Hannemann R, Eskofier BM. The Effect of Hearing Aid Amplification on Gait Parameters: A Pilot Study Using Ear-Worn Motion Sensors. Audiology Research. 2025; 15(3):45. https://doi.org/10.3390/audiolres15030045
Chicago/Turabian StyleSeifer, Ann-Kristin, Arne Küderle, Kaja Strobel, Ronny Hannemann, and Björn M. Eskofier. 2025. "The Effect of Hearing Aid Amplification on Gait Parameters: A Pilot Study Using Ear-Worn Motion Sensors" Audiology Research 15, no. 3: 45. https://doi.org/10.3390/audiolres15030045
APA StyleSeifer, A.-K., Küderle, A., Strobel, K., Hannemann, R., & Eskofier, B. M. (2025). The Effect of Hearing Aid Amplification on Gait Parameters: A Pilot Study Using Ear-Worn Motion Sensors. Audiology Research, 15(3), 45. https://doi.org/10.3390/audiolres15030045






