Abstract
Thalassemia is one of the most prevalent genetic disorders worldwide and has previously been found to have an association with several physiological and organ complications. Several studies have found both its positive and inverse correlation with the glomerular filtration rate (GFR). Therefore, in this meta-analysis, we tried to assess the accurate correlation of β-thalassemia major (β-TM) with GFR. We searched in Google Scholar, PubMed, and ScienceDirect, and from the initial 96 articles, we finally included 12 studies. The quality and publication bias assessment confirmed that all the studies were of high to moderate quality with no publication bias. The main outcome of the mean difference (MD) was −6.94, 95%CI: −20.69, 6.80 (p < 0.00001), which indicated a negative correlation of the GFR with β-TM. The sensitivity analyses found one study to be a slight outlier, and reanalyzing the data excluding that study, an MD was achieved of −16.46, 95%CI: −26.81, −6.11 (p < 0.00001), which provides even stronger support for our main outcome. Our result determined that the GFR is generally higher in healthy people as compared to β-TM patients.
1. Introduction
There are several inherited disorders that are associated with hemoglobin. Thalassemia is one of the major disorders of hemoglobin related to unusual hemoglobin formation [1]. Thalassemia can be of different types such as α-thalassemia, β-thalassemia, sickle thalassemia, etc. [2,3]. Among them, β-thalassemia is one of the most prominent types of thalassemia caused by single gene alteration. Approximately, throughout the world, 7% of the population bear hemoglobinopathies as carriers, of which 1.5% (~80–90 million) are carriers or heterozygotes of β-thalassemia [4,5]. The highest frequencies of β-thalassemia have been observed in the Mediterranean and European regions, especially in countries such as Cyprus (15%), Sardinia (10–12%), Greece (8%), Italy (4–5%), Spain (1–2%), and the UK (0.4%), as well as in Eastern and Central Europe (0.2–5%) among other continents such as Africa, America, and Asia. In North Africa, the frequency of β-thalassemia was highest in Egypt (2–9%) followed by Morocco (6–7%), Tunisia (5%), and Libya (4–5%). The Maldives displayed the highest rate (18%) of this genetic disease followed by Indonesia (3–10%), India (1–10%), Thailand (3–9%), Pakistan (1–8%), and China–Hong Kong (3–6%) in the South-East region of Asia, whereas Iran, Syria, and Oman showed a similar rate (4–5%), which was the highest among the other countries of the Middle East and Western regions of Asia [4]. This prevalence rate clearly highlights the current global burden of thalassemia.
As mentioned earlier, thalassemia can be mainly of two different types: α-thalassemia and β-thalassemia, based on the globin chain that is affected. β-thalassemia occurs when the β-globin gene is mutated, whereas α-thalassemia occurs due to α-globin gene mutation [2]. Again, thalassemia major (TM) refers to the severity of the clinical condition or phenotype that necessitates red blood cell (RBC) transfusion more than eight times in a year, and thalassemia intermedia (TI) refers to the condition where infrequent or absolutely no transfusion is required. Thalassemia minor refers to the condition of being an asymptomatic carrier who might have mild anemia [2,6]. Clinical symptoms such as diarrhea, fever, irritability, abdominal distention, nutritional complications, and enlargement of the liver and spleen are usually expressed within 6–24 months of birth in thalassemia major. In thalassemia intermedia, symptoms might appear between 2 and 6 years of age with milder anemia, where irregular blood transfusions may be required depending on the physical condition [6].
Glomerular filtration is a physiological process by which impure blood carrying nitrogenous and other waste materials is converted to ultrafiltrate blood after flowing through the glomerular capillaries of the kidney [7]. Estimating the glomerular filtration rate (GFR) is a crucial practice for diagnosis, prognosis, monitoring, and drug dose management for kidney diseases in particular [7,8]. Theoretically, the GFR is the outcome of the total number of nephrons times the average single-nephron GFR; however, in practical conditions, many of the survey-based studies were unable to employ the more sophisticated and quantitative tests used in clinical nephrology to specifically assess the kidney, such as with a time clearance of imaging dyes [7]. Although the GFR is a primary index of kidney disease, changes in the GFR were also found to be associated with other diseases such as coronary heart disease (CHD), cardiovascular disease (CVD), fatty liver, UTI, etc. [9,10,11,12]. Interestingly, the GFR was also found to have a correlation with β-thalassemia major (β-TM); however, in several investigations, a positive correlation between GFR and β-TM was identified, and in some other cases, the GFR was detected to have an inverse relation with β-TM [13,14]. Therefore, in this meta-analysis, we tried to evaluate the exact association between GFR and β-TM.
2. Materials and Methods
2.1. Search Strategy
Primarily, three different databases, Google Scholar, PubMed, and ScienceDirect, were searched, respectively, with specific keywords, which included “glomerular”, “GFR”, “thalassemia”, “randomized control trial”, “RCT”, “case-control”, and “healthy”. An “Advanced” search mode was used to search articles in PubMed and ScienceDirect. “Title and abstract” and “Title, abstract, keywords” were used in the “advanced” mode for PubMed and ScienceDirect, respectively. However, “allintitle” was used during the search in Google Scholar. The search was adjusted with Boolean operators where necessary. The detailed search strategy is described in Supplementary Table S1.
2.2. Eligibility Criteria
Narrative or systematic reviews, documents, correspondence, book chapters, letters to editors, editorials, or articles that did not focus on β-TM and GFR were not considered eligible. Duplicate articles assessed from different databases were removed carefully. Only English-language-written articles were considered for this study. However, no year restriction was applied.
2.3. Quality Assessment
To investigate the quality of all the included studies, a number of questions were acquired from the Study Quality Assessment Tools, NIH, and Systematic Reviews: Step 6: Assess Quality of Included Studies, UNC [15,16]. The score was given either as 1 or 0 for an individual question depending on the answer (i.e., Yes = 1, No = 0, Unclear = 0, NR = no score, NA = no score). The overall score was divided by 9 for a study and then the score was converted into a percentage. If any answer was identified as either NR or NA for a particular question, the question was assumed to be invalid for that individual study and removed from the calculation. The total scores of ≤50, 60–70, and ≥80 were classified as relating to low-scoring studies (high risk of bias), moderate-scoring studies (moderate risk of bias), and high-scoring studies (low risk of bias), respectively.
2.4. Data Extraction and Analyses
Based on the eligibility criteria, data extraction was performed carefully from the included studies. Several data regarding the general characteristics of the included studies were extracted along with the data of the mean ± standard deviation (SD) of the GFR and the number of total participants in the case and control sections for meta-analysis. Endnote (version X8) software was operated for data extraction.
A random effects model of mean difference (MD) with 95% confidence intervals (CIs) was the preferred method to analyze the difference in the GFR levels between the case and control participants within the included studies. Heterogeneity of the included studies was determined using I2 statistics (I2 > 75% implies substantial heterogeneity). RevMan (version-5.4) software was used for the meta-analysis.
2.5. Publication Bias and Sensitivity Analyses
Publication bias and sensitivity analyses were performed using different methods of analysis to investigate the strength of the result following a previous study with slight modifications [17,18]. Primarily, a funnel plot was created to identify the publication bias, followed by a Galbraith plot, which was constructed to visualize any outlier studies. Furthermore, a forest plot was constructed using the random effects model considering the non-outlier homogenous studies. Again, a forest plot was constructed using the fixed effects model with all the included studies to reconfirm the main outcome. To construct the funnel and Galbraith plots, RStudio software (version 4.3.0) and the “metafor” package (version 4.2-0) of R were used.
3. Results
3.1. Inclusion of the Study
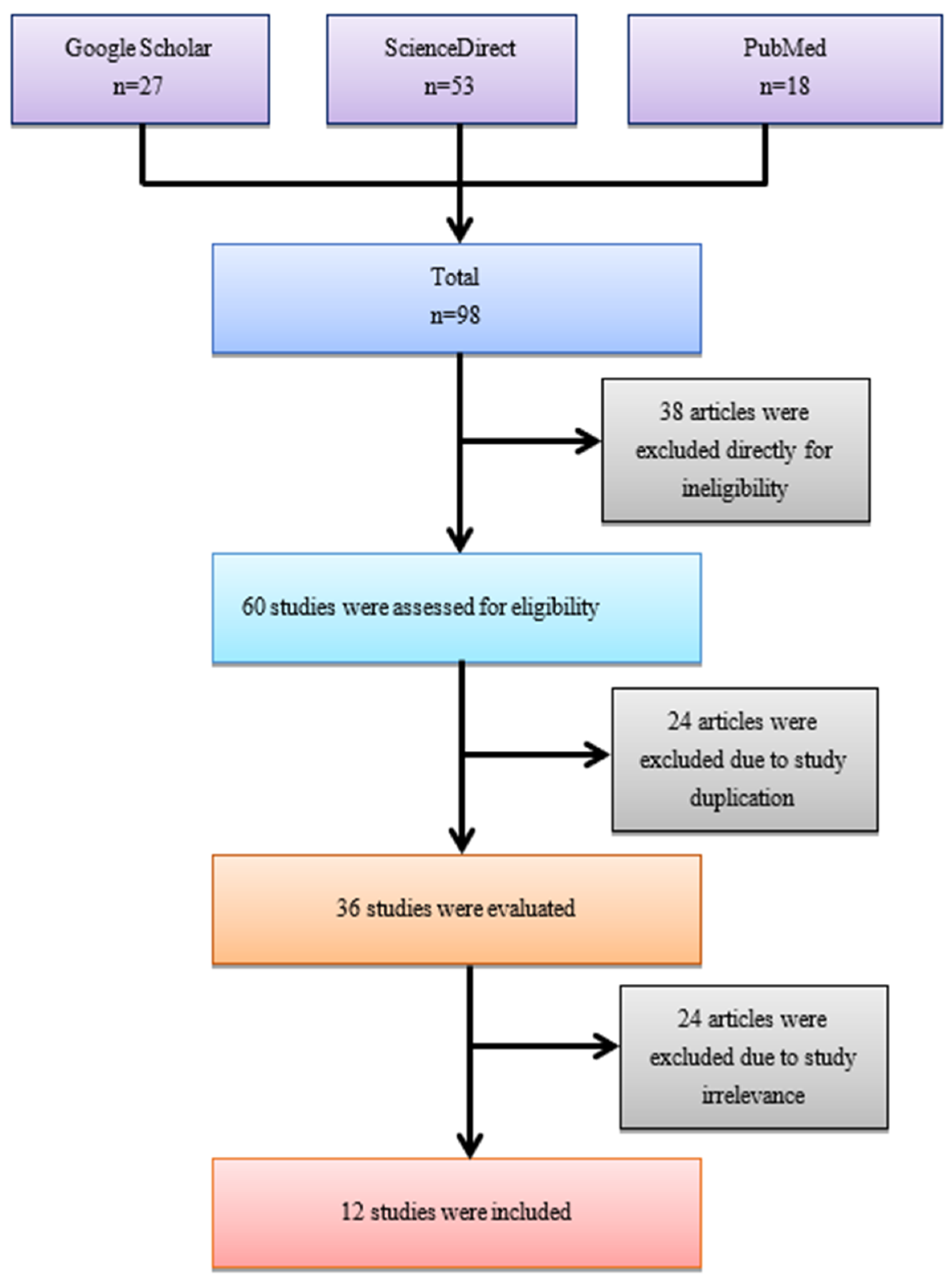
After the initial search, a total of 96 articles were identified from three online databases (i.e., PubMed, ScienceDirect, and Google Scholar). From those articles, 36 were immediately excluded due to their ineligibility as they were case reports, review articles, correspondence, letters, editorials or original articles working with an animal model, or in vitro or in silico experiments other than full-length research articles working with a human case–control model. From the remaining 60 articles, 24 were excluded due to study duplication. From the remaining 36 articles, 24 were eliminated for not matching with our focus and study criteria (i.e., including different types of control, a lack of data, assessing other diseases, etc.). Finally, 12 articles were included for this meta-analysis (Figure 1).
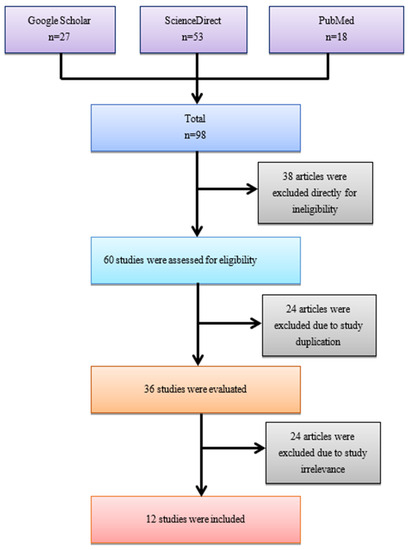
Figure 1.
A simplified flow diagram of methodology.
3.2. Assessment of Quality
The quality assessment of the study determined that all the included studies were of moderate (moderate risk of bias) or high quality (low risk of bias) (Table 1). No study had a score of ≤50 with a high risk of bias.

Table 1.
Quality assessment of the included studies.
(1) Was the research question appropriate? (2) Was the study population clearly defined? (3) Were the controls selected from the same or a similar population including within the same timeframe? (4) Did the authors follow the proper inclusion and exclusion criteria regarding case–control selection? (5) Were the cases clearly defined and differentiated from the controls? (6) Were the assessors of exposure/risk blinded to the case or control status of participants? (7) If fewer than 100 participants of eligible cases and/or controls were selected for the study, were the cases and/or controls randomly selected from those eligible? (8) Did the authors use statistical analyses? (9) Were the GFR measurement equations valid to conduct the study? Y = Yes, N = No, NR = not reported, U = Unclear, NA = not applicable.
3.3. Study Characteristics
Major characteristics such as the study location, study type, demographics of the study participants (i.e., male, female ratio in study, BMI, age, case and control type, etc.) and the GFR measuring method were extracted from each of the included studies (Table 2). However, the age range among the study participants had variations (i.e., minimum 8.3 years to maximum 33.5 years). In Table 2, not reported (NR) was used if any information was not provided in any of the studies. Among the studies, only the data regarding participants’ BMI were not reported in Ahmed 2022, Ali 2013, Bekhit 2017, Centinkaya 2020, Mahmoud 2021, Sen 2015, and Uzun 2015 [19,20,21,22,23,24,25]. Percentages of the male and female participants were missing in Capolongo 2020 [26]. All data were reported in Bilir 2020, Behairy 2017, Hamed 2010, and Mahmoud 2012 [13,14,27,28].

Table 2.
Characteristics of the included studies.
3.4. Main Outcome
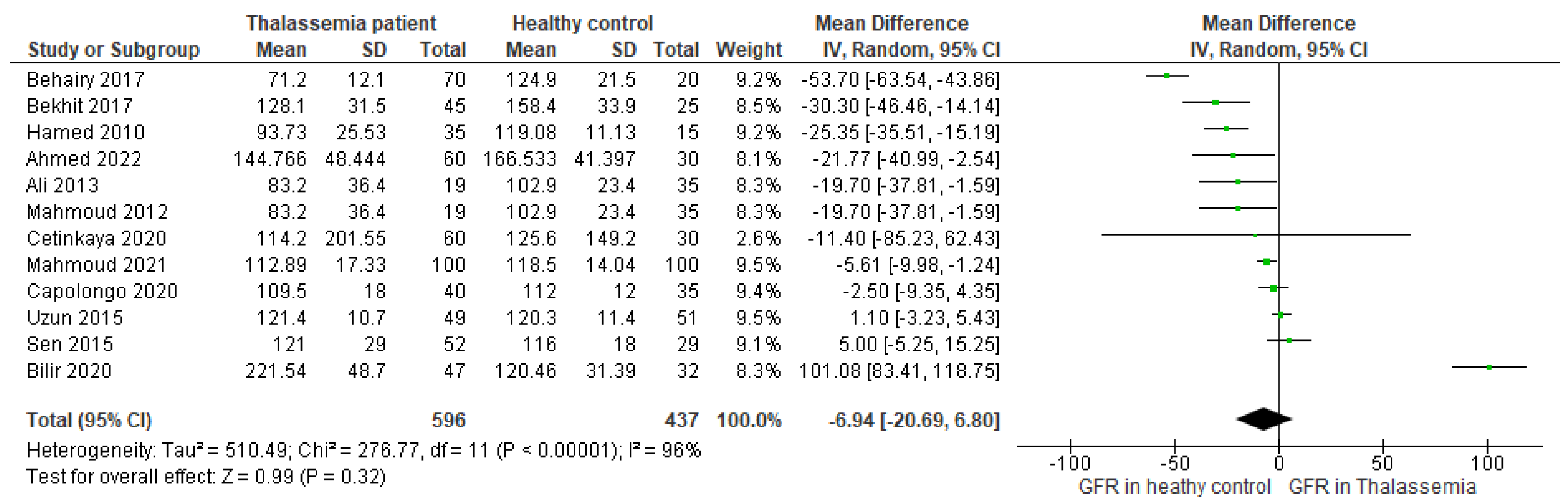
The forest plot including all the studies (n = 12) (Figure 2) found that the mean difference (MD) of the GFR level was −6.94, 95%CI: −20.69, 6.80 (p < 0.00001), favoring the healthy control as compared to the β-TM patient. The determined I2 > 96% for the analysis implied that the heterogeneity of the included studies was significantly high.
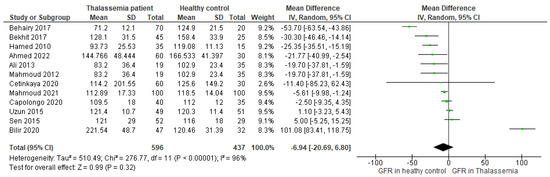
Figure 2.
Forest plot showing the mean difference (MD) of GFR in patients with β-TM as compared to healthy controls in the random effects model.
3.5. Assessment of Publication Bias and Sensitivity Analysis
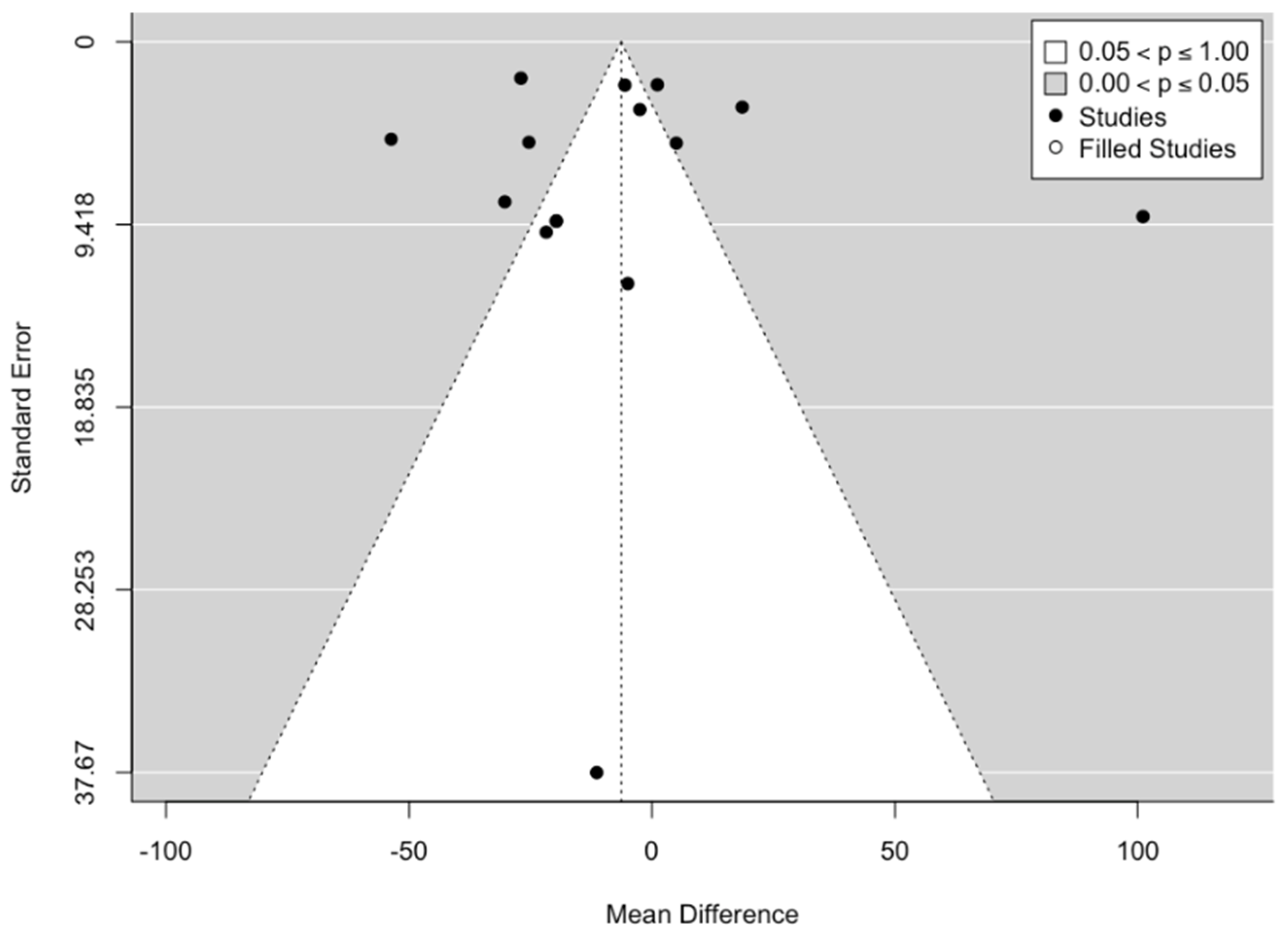
The funnel plot constructed based on all the included studies confirmed there was no high asymmetry in the plot (Figure 3).
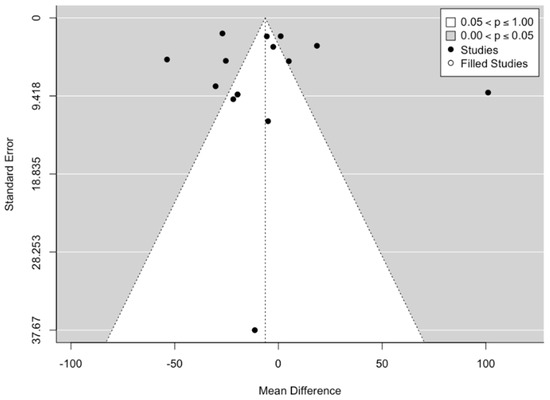
Figure 3.
Funnel plot investigating the publication bias reporting GFR in β-TM patients in comparison to healthy controls.
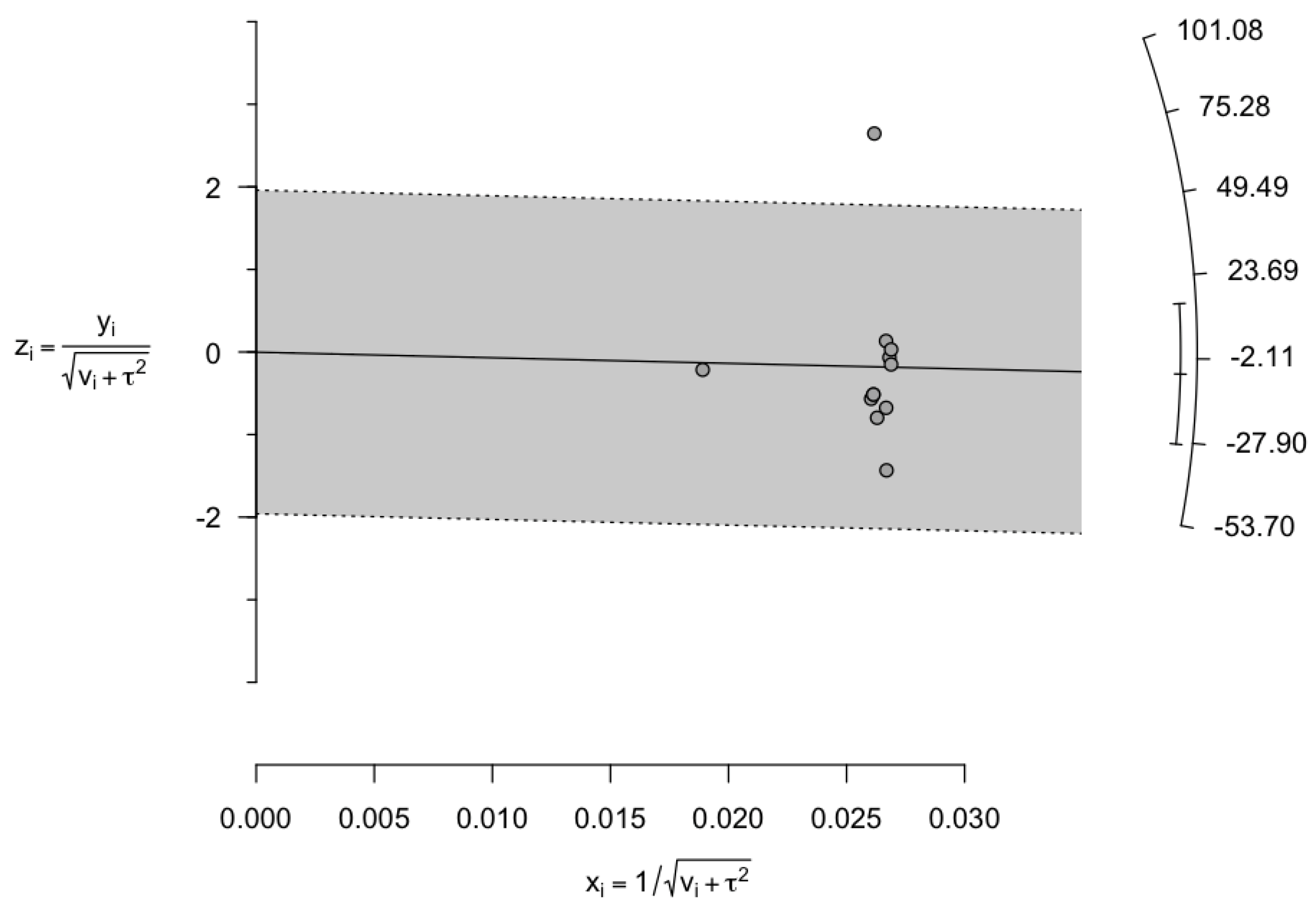
This confirmed the absence of any publication bias. Again, due to high heterogeneity, we considered the data for sensitivity analysis. For sensitivity analyses, we initially constructed a Galbraith plot. From the Galbraith’s plot, Bilir 2020 was considered to be a single outlier study (Figure 4).
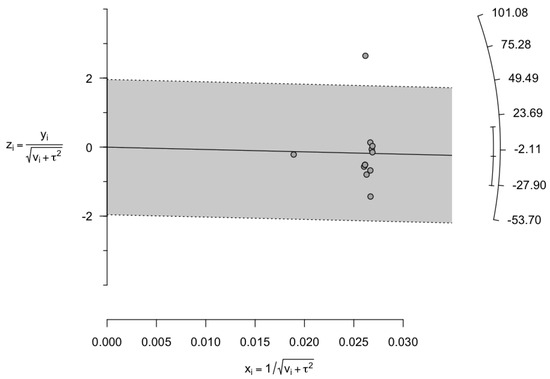
Figure 4.
Galbraith plot displaying the plausible sources of heterogeneity. Studies within the limits are interpreted as homogeneous. Studies outside the limits may be outliers. According to the plot, one study (Bilir 2020) was found to be an outlier.
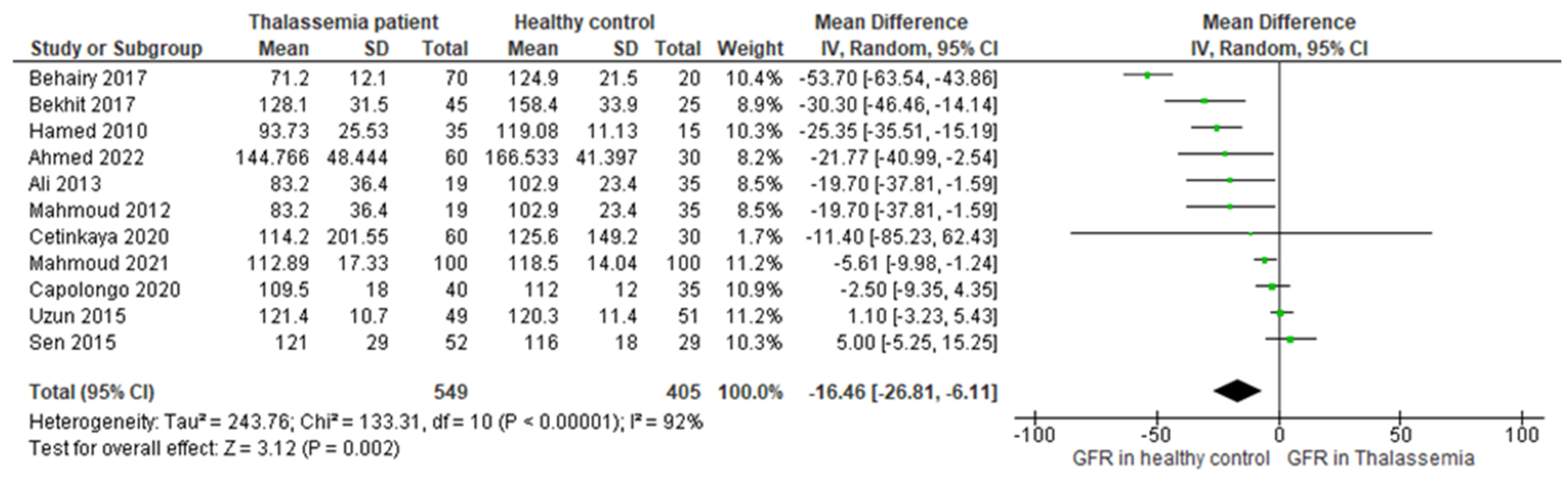
Therefore, excluding Bilir 2020, a further forest plot was constructed using 11 studies (Figure 5), where the mean difference (MD: −16.46, 95%CI: −26.81, −6.11) (p < 0.00001)) was found to be two times higher than the main outcome (−6.45, 95%CI: −18.50, 5.60 (p < 0.00001) (Figure 2)), favoring the higher GFR in healthy controls. Moreover, the heterogeneity reduced (I2 = 95%) in comparison to the main result.
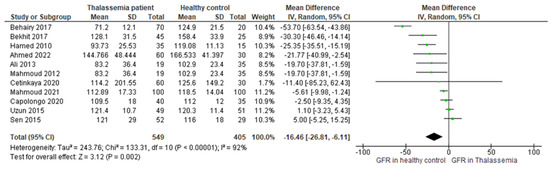
Figure 5.
Forest plot showing the mean difference (MD) of GFR in patients with β-TM as compared to healthy controls in the random effects model excluding the outlier study (n = 1).
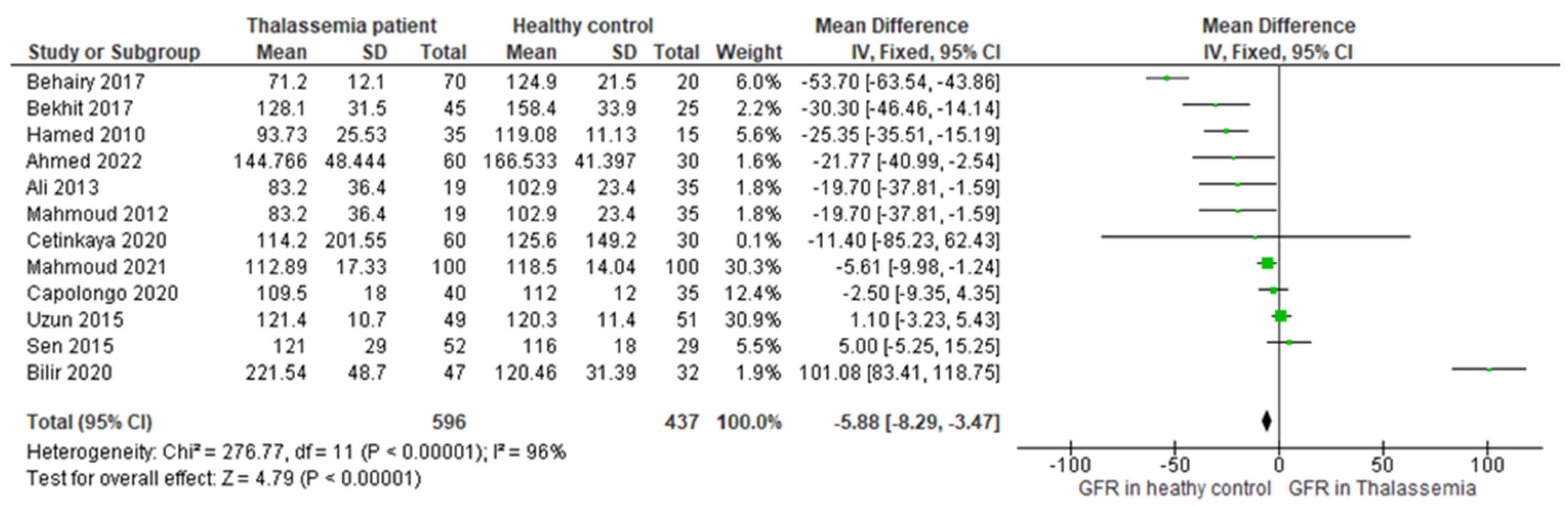
Similarly, reconstruction of the forest plot including all the included studies using a fixed effects model was found to favor healthy controls as compared to β-TM patients (MD: −5.88, 95%CI: −8.29, −3.47) (Figure 6), which also supported the main outcome. These sensitivity analyses further supported the strength of our primary result.
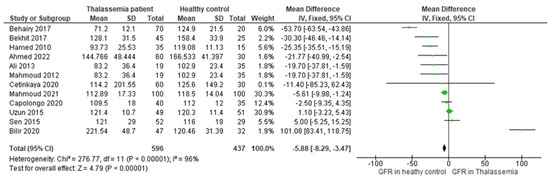
Figure 6.
Forest plot showing the mean difference (MD) of GFR in patients with β-thalassemia as compared to healthy controls in the fixed effects model.
4. Discussion
To the best of our knowledge, this is the only meta-analysis to have focused on the association between β-TM and GFR, compiling research data from all over the world. The research says that thalassemia can alter the GFR through mechanisms such as renal hypoxia, iron overload, oxidative stress, and renal tubular dysfunction [29,30].
Thalassemia results in chronic anemia from the decreased synthesis of functional hemoglobin. Anemia lowers the blood’s ability to transport oxygen, which causes tissue hypoxia, notably in the kidneys, thus causing renal hypoxia. Renal hypoxia may result in diminished renal performance, including a drop in the GFR. Again, to treat their anemia, people with thalassemia frequently need blood transfusions. Iron overload in the body may result from these transfusions. The kidneys, among other organs, can become overloaded with iron, which can cause tissue damage and malfunction. Damaged kidneys brought on by iron excess may lower the GFR [29].
An upsurge in oxidative stress after the creation of an imbalance between the antioxidant defense mechanism and the generation of reactive oxygen species (ROS) inside the body may occur because of thalassemia. The renal vasculature and glomeruli may be harmed through the oxidative stress, ultimately impairing the GFR. Thalassemia can also interfere with the renal tubules, which are crucial for reabsorbing filtered chemicals and preserving fluid and electrolyte balance. Electrolyte imbalances and poor water absorption caused by renal tubule dysfunction can eventually have an negative impact on the GFR [30].
Through the MD value of our main outcome (MD: −6.45, 95%CI: −18.50, 5.60) (Figure 2), we determined that the GFR was higher in the healthy population as compared to people with β-TM. This finding ultimately indicates that the GFR is generally disrupted in thalassemia patients regardless of whether an individual has a current or a previous history of any types of kidney disease, which is further supported by previous researches [29,30].
From our analysis, we found exceptional results where the MD value of the GFR was higher in thalassemia patients in comparison to healthy controls (Figure 2). Among the included studies, the MD value of the GFR was found to be the highest in β-TM patients in Bilir 2020 (MD: 101.08, 95%CI: 83.41, 118.75) followed by Sen 2015 (MD: 5, 95%CI: −5.25,15.25) and Uzun 2015 (MD: 1.1, 95%CI: −3.23, 5.46).
Bilir et al. mentioned that the small sample size of their study could be one of the reasons for such an unusual positive correlation between thalassemia and GFR. Moreover, age, prolonged anemia, and medicinal side effects or toxicity were suggested as having an association with this incident [13,31]. Deferoxamine is a popular medicine that is used in thalassemia as a chelating agent. This was used in thalassemia in the study of Bilir 2020 [13]. Research observed the effect of subcutaneous deferoxamine on 27 patients with thalassemia major, where, interestingly, it was identified that after the deferoxamine treatment, 41% of the patients’ GFR values were above the normal range [32]. Therefore, the argument that deferoxamine toxicity plays a role in increasing GFR might be possible but needs to be confirmed through further rigorous research. Again, increased proteinuria in thalassemia patients was investigated in the study of Bilir 2020. According to Ghobrial et al., if the muscle mass and diet are not strictly maintained, it may lead to increased serum protein, which translates into enhanced proteinuria [13,33]. A previous study claimed that the high prevalence of microalbuminuria in patients with sickle cell leads to macroproteinuria and, ultimately, chronic renal failure, where glomerular hyperfiltration is the early step [34]. Therefore, enhanced proteinuria might be another plausible cause of an increased GFR in β-TM patients.
The disease thalassemia has a wide range of morbidities and affects practically all organ systems. Among thalassemia patients who depend on blood transfusions, renal illness is one of the leading causes of death. The early detection of kidney illness is crucial to avoid impairment since it might arise from progressive renal tubular and glomerular damage [35]. The results indicate a substantial relationship between β-TM and GFR. The GFR can be helpful for the early detection and prevention of renal failure in thalassemia patients since this study demonstrated a notable difference between the GFR in healthy control and that in β-TM patients. Hence, it is important for thalassemia patients to periodically monitor their GFR rate. Thus, the above finding can help patients with β-TM in identifying renal diseases, lowering the fatality rates.
It is necessary to evaluate GFR using a more precise approach. An approach such as this could make it possible to identify GFR decline early in β-TM patients and stop or slow its progression to acute kidney injury (AKI), chronic kidney disease (CKD), or any other kidney-related complications, and the requirement for renal replacement therapy (RRT) [36]. The GFR can be determined through the identification of the clearance rate of different endogenous or exogenous biomarkers such as inulin, creatinine, cystatin C, iohexol, etc., and all are clinically accepted [23,37,38]. According to previous research, the Schwartz formula is better at estimating the GFR in a younger population (age ≤21 years) and the chronic kidney disease epidemiology collaboration creatinine equations (CKD-EPI) are better at assessing the GFR in adult [39]. This was maintained in all the included studies as all of them used the Schwartz formula as the ages of their study participants were ≤21.5 years, except for Capolong 2020 (Table 2). Therefore, Capolongo 2020 used the CKD-EPI to estimate the GFR in adults (age ≤ 33 years) and the Schwartz formula to assess the GFR in younger participants (age ≤ 21 years) [26]. However, other than the Schwartz formula and CKD-EPI, different methods such as Modification of Diet in Renal Disease (MDRD) and the Cockcroft–Gault formulas are also used, and, interestingly, the equations are sometimes slightly changed based on sex and race [40]. Therefore, the measurement methods and biomarkers need to be specified further to obtain highly accurate results, which is crucial for the proper diagnosis, prognosis, medication, and treatment of patients. The adoption of a highly precise and specified technique could enable the early diagnosis of a decreased GFR in β-TM and delay the steady decline towards kidney dysfunction.
5. Conclusions
In conclusion, β-TM patients are more susceptible to renal glomerular and tubular damage, which is rarely detected in conventional renal testing. The GFR in β-TM patients is a reliable indicator for evaluating glomerular damage and thus kidney dysfunction. In β-TM patients, the GFR can be useful for the early identification or even prevention of renal failure since it varies between healthy controls and cases.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/thalassrep13030018/s1, Table S1: Search strategy.
Author Contributions
Conceptualization, S.S.K. and E.S.; methodology, N.J., D.S., A.H.P., I.A.H. and S.S.K., software, S.S.K., J.Z. and E.S.; formal analysis, S.S.K., J.Z. and E.S.; investigation, S.S.K., N.J., D.S., A.H.P. and I.A.H., resources, E.S.; data curation, E.S. and M.N.U.; writing—original draft preparation, S.S.K. and E.S.; writing—review and editing, S.S.K. and E.S., visualization, S.S.K., J.Z. and E.S.; supervision, E.S.; project administration, E.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data relevant to this review are included in the text, Supplementary Materials, and References.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Helmi, N.; Bashir, M.; Shireen, A.; Ahmed, I.M. Thalassemia review: Features, dental considerations and management. Electron. Physician 2017, 9, 4003. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, M.J. Update on thalassemia: Clinical care and complications. Hematol. Oncol. Clin. N. Am. 2010, 24, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Aessopos, A.; Farmakis, D.; Tsironi, M.; Diamanti-Kandarakis, E.; Matzourani, M.; Fragodimiri, C.; Hatziliami, A.; Karagiorga, M. Endothelial function and arterial stiffness in sickle-thalassemia patients. Atherosclerosis 2007, 191, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Colah, R.; Gorakshakar, A.; Nadkarni, A. Global burden, distribution and prevention of β-thalassemias and hemoglobin E disorders. Expert Rev. Hematol. 2010, 3, 103–117. [Google Scholar] [CrossRef]
- Weatherall, D.; Akinyanju, O.; Fucharoen, S.; Olivieri, N.; Musgrove, P. Inherited disorders of hemoglobin. In Disease Control Priorities in Developing Countries, 2nd ed.; Oxford University Press: Oxford, UK, 2006. [Google Scholar]
- Tari, K.; Valizadeh Ardalan, P.; Abbaszadehdibavar, M.; Atashi, A.; Jalili, A.; Gheidishahran, M. Thalassemia an update: Molecular basis, clinical features and treatment. Int. J. Biomed. Public Health 2018, 1, 48–58. [Google Scholar] [CrossRef]
- Levey, A.S.; Inker, L.A.; Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. 2014, 63, 820–834. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.A.; Levey, A.S. Measured GFR as a confirmatory test for estimated GFR. J. Am. Soc. Nephrol. JASN 2009, 20, 2305–2313. [Google Scholar] [CrossRef]
- Matsushita, K.; Selvin, E.; Bash, L.D.; Franceschini, N.; Astor, B.C.; Coresh, J. Change in estimated GFR associates with coronary heart disease and mortality. J. Am. Soc. Nephrol. JASN 2009, 20, 2617. [Google Scholar] [CrossRef]
- Mathisen, U.D.; Melsom, T.; Ingebretsen, O.C.; Jenssen, T.; Njølstad, I.; Solbu, M.D.; Toft, I.; Eriksen, B.O. Estimated GFR associates with cardiovascular risk factors independently of measured GFR. J. Am. Soc. Nephrol. JASN 2011, 22, 927. [Google Scholar] [CrossRef]
- Di Bonito, P.; Valerio, G.; Licenziati, M.; Miraglia Del Giudice, E.; Baroni, M.; Morandi, A.; Maffeis, C.; Campana, G.; Spreghini, M.; Di Sessa, A. High uric acid, reduced glomerular filtration rate and non-alcoholic fatty liver in young people with obesity. J. Endocrinol. Investig. 2020, 43, 461–468. [Google Scholar] [CrossRef]
- Arnello, F.; Ham, H.; Tondeur, M.; Piepsz, A. Evolution of single kidney glomerular filtration rate in urinary tract infection. Pediatr. Nephrol. 1999, 13, 121–124. [Google Scholar] [CrossRef]
- Bilir, Ö.A.; Kirkiz, S.; Fettah, A.; Bozkaya, İ.O.; Kara, A.; Çakar, N.; Yaralı, N. Renal function and the oxidative status among children with thalassemia major and healthy controls: A cross-sectional study. Transfus. Apher. Sci. 2020, 59, 102746. [Google Scholar] [CrossRef] [PubMed]
- Behairy, O.G.; Abd Almonaem, E.R.; Abed, N.T.; Abdel Haiea, O.M.; Zakaria, R.M.; AbdEllaty, R.I.; Asr, E.H.; Mansour, A.I.; Abdelrahman, A.M.; Elhady, H.A. Role of serum cystatin-C and beta-2 microglobulin as early markers of renal dysfunction in children with beta thalassemia major. Int. J. Nephrol. Renov. Dis. 2017, 10, 261–268. [Google Scholar] [CrossRef]
- NIH. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 25 July 2023).
- UNC. Systematic Reviews: Step 6: Assess Quality of Included Studies. Available online: https://guides.lib.unc.edu/systematic-reviews/assess-quality (accessed on 25 July 2023).
- Islam, M.A.; Khandker, S.S.; Alam, S.S.; Kotyla, P.; Hassan, R. Vitamin D status in patients with systemic lupus erythematosus (SLE): A systematic review and meta-analysis. Autoimmun. Rev. 2019, 18, 102392. [Google Scholar] [CrossRef]
- Islam, M.A.; Alam, S.S.; Kundu, S.; Prodhan, A.S.U.; Khandker, S.S.; Reshetnyak, T.; Kotyla, P.J.; Hassan, R.; Hossan, T. Prevalence of antiphospholipid antibodies in Behçet’s disease: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0227836. [Google Scholar] [CrossRef]
- Ahmed, H.M.; Georgy, D.B.; Meabed, M.H.; Botrous, O.E. The association between plasma microRNA-451 expression levels and chronic kidney disease in children with β-thalassemia major. Iran. J. Kidney Dis. 2022, 16, 188. [Google Scholar]
- Ali, B.A.; Mahmoud, A.M. Frequency of glomerular dysfunction in children with beta thalassaemia major. Sultan Qaboos Univ. Med. J. 2014, 14, e88. [Google Scholar] [CrossRef][Green Version]
- Bekhit, O.E.; El Dash, H.H.; Ahmed, M.S. Early detection of kidney dysfunction in Egyptian patients with beta-thalassemia major. Egypt. Pediatr. Assoc. Gaz. 2017, 65, 85–89. [Google Scholar] [CrossRef]
- Cetinkaya, P.U.; Azik, F.M.; Karakus, V.; Huddam, B.; Yilmaz, N. β2-microglobulin, neutrophil gelatinase-associated lipocalin, and endocan values in evaluating renal functions in patients with β-thalassemia major. Hemoglobin 2020, 44, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.A.; Elian, D.M.; Abd El Hady, N.M.; Abdallah, H.M.; Abdelsattar, S.; Khalil, F.O.; Abd El Naby, S.A. Assessment of subclinical renal glomerular and tubular dysfunction in children with beta thalassemia major. Children 2021, 8, 100. [Google Scholar] [CrossRef]
- Şen, V.; Ece, A.; Uluca, Ü.; Söker, M.; Güneş, A.; Kaplan, İ.; Tan, İ.; Yel, S.; Mete, N.; Sahin, C. Urinary early kidney injury molecules in children with beta-thalassemia major. Ren. Fail. 2015, 37, 607–613. [Google Scholar] [CrossRef]
- Uzun, E.; Balcı, Y.I.; Yüksel, S.; Aral, Y.Z.; Aybek, H.; Akdağ, B. Glomerular and tubular functions in children with different forms of beta thalassemia. Ren. Fail. 2015, 37, 1414–1418. [Google Scholar] [CrossRef]
- Capolongo, G.; Zacchia, M.; Beneduci, A.; Costantini, S.; Cinque, P.; Spasiano, A.; De Luca, G.; Di Pietro, M.E.; Ricchi, P.; Trepiccione, F. Urinary metabolic profile of patients with transfusion-dependent β-thalassemia major undergoing deferasirox therapy. Kidney Blood Press. Res. 2020, 45, 455–466. [Google Scholar] [CrossRef]
- Hamed, E.A.; ElMelegy, N.T. Renal functions in pediatric patients with beta-thalassemia major: Relation to chelation therapy: Original prospective study. Ital. J. Pediatr. 2010, 36, 39. [Google Scholar] [CrossRef]
- Mahmoud, A.; Ali, B. Cystatin C as an Early Marker of Glomerular Dysfunction in Children with Beta Thalassemia Major. Bull. Egypt. Soc. Physiol. Sci. 2012, 32, 265–278. [Google Scholar] [CrossRef]
- Saghir, S.; Riaz, A.; Hasan, A.; Bhatti, Y.A.; Ghuman, A.A.; Shakil, M. Cystatin C an early marker of Glomerular dysfunction in thalassemia major. Prof. Med. J. 2020, 27, 300–308. [Google Scholar] [CrossRef][Green Version]
- Cai, Q.; Dekker, L.H.; Bakker, S.J.; de Borst, M.H.; Navis, G.J. Dietary patterns based on estimated glomerular filtration rate and kidney function decline in the general population: The lifelines cohort study. Nutrients 2020, 12, 1099. [Google Scholar] [CrossRef]
- Jalali, A.; Khalilian, H.; Ahmadzadeh, A.; Sarvestani, S.; Rahim, F.; Zandian, K.; Asar, S. Renal function in transfusion-dependent pediatric beta-thalassemia major patients. Hematology 2011, 16, 249–254. [Google Scholar] [CrossRef]
- Koren, G.; Kochavi-Atiya, Y.; Bentur, Y.; Olivieri, N. The effects of subcutaneous deferoxamine administration on renal function in thalassemia major. Int. J. Hematol. 1991, 54, 371–375. [Google Scholar] [PubMed]
- Ghobrial, E.E.; Abdel-Aziz, H.A.; Kaddah, A.M.; Mubarak, N.A. Urinary transforming growth factor β-1 as a marker of renal dysfunction in sickle cell disease. Pediatr. Neonatol. 2016, 57, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Haymann, J.-P.; Stankovic, K.; Levy, P.; Avellino, V.; Tharaux, P.-L.; Letavernier, E.; Grateau, G.; Baud, L.; Girot, R.; Lionnet, F. Glomerular hyperfiltration in adult sickle cell anemia: A frequent hemolysis associated feature. Clin. J. Am. Soc. Nephrol. CJASN 2010, 5, 756. [Google Scholar] [CrossRef] [PubMed]
- Sleiman, J.; Tarhini, A.; Taher, A.T. Renal complications in thalassemia. Thalass. Rep. 2018, 8, 7481. [Google Scholar] [CrossRef]
- de Dreuzy, E.; Bhukhai, K.; Leboulch, P.; Payen, E. Current and future alternative therapies for beta-thalassemia major. Biomed. J. 2016, 39, 24–38. [Google Scholar] [CrossRef]
- Milo, G.; Nevo, R.F.G.; Pazgal, I.; Gafter-Gvili, A.; Shpilberg, O.; Gafter, U.; Erman, A.; Stark, P. GFR in Patients with β-Thalassemia Major. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 1350. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schwartz, G.J.; Furth, S.L. Glomerular filtration rate measurement and estimation in chronic kidney disease. Pediatr. Nephrol. 2007, 22, 1839–1848. [Google Scholar] [CrossRef] [PubMed]
- Grubb, A.; Nyman, U.; Björk, J.; Lindström, V.; Rippe, B.; Sterner, G.; Christensson, A. Simple cystatin C–based prediction equations for glomerular filtration rate compared with the modification of diet in renal disease prediction equation for adults and the Schwartz and the Counahan–Barratt prediction equations for children. Clin. Chem. 2005, 51, 1420–1431. [Google Scholar] [CrossRef]
- Michels, W.M.; Grootendorst, D.C.; Verduijn, M.; Elliott, E.G.; Dekker, F.W.; Krediet, R.T. Performance of the Cockcroft-Gault, MDRD, and new CKD-EPI formulas in relation to GFR, age, and body size. Clin. J. Am. Soc. Nephrol. CJASN 2010, 5, 1003. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).