Pulmonary Hyalinizing Granuloma: A Rare Cause of a Benign Lung Mass
Abstract
:1. Introduction
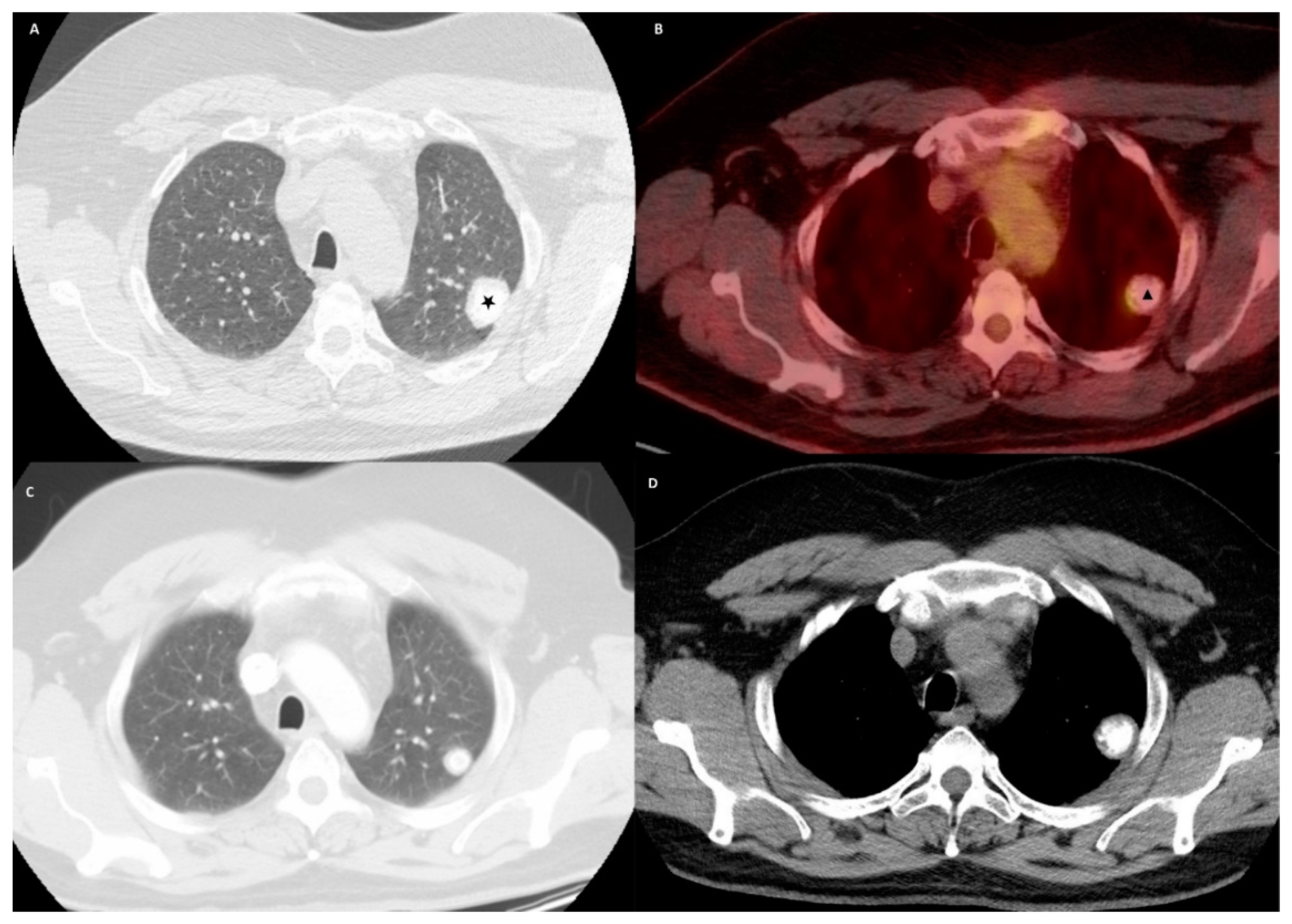
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Benfield, J.R.; Harrison, R.W.; Moulder, P.V.; Lyon, E.S.; Graff, P.W. Bilateral nodular pulmonary granulomas and retroperitoneal fibrosis. Simulated metastatic malignant neoplasm and spontaneous remission of ureteral obstruction. JAMA 1962, 182, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Peng, M.; Xu, W.B.; Shi, J.H.; Cai, B.Q.; Tian, X.L.; Liu, T.; Zhang, H.; Xiao, Y.; Liu, W.; Feng, R.; et al. The diagnostic value of CT-guided percutaneous needle lung biopsy in diffuse parenchymal lung diseases. Zhonghua Jie He He Hu Xi Za Zhi 2012, 35, 171–175. [Google Scholar] [PubMed]
- Brandão, V.; Marchiori, E.; Zanetti, G.; Abdalla, G.; Ventura, N.; Constantino, C.L.; Pereira, M.L.; Martins, P.; Canellas, R.; Muccillo, A.; et al. Hyalinizing granuloma: An unusual case of a pulmonary mass. Case Rep. Med. 2010, 2010, 984765. [Google Scholar] [CrossRef] [PubMed]
- Engleman, P.; Liebow, A.A.; Gmelich, J.; Friedman, P.J. Pulmonary hyalinizing granuloma. Am. Rev. Respir. Dis. 1977, 115, 997–1008. [Google Scholar] [PubMed]
- Weisenberg, E. Hyalinizing Granuloma. Available online: https://www.pathologyoutlines.com/topic/lungnontumorhyalinizinggran.html (accessed on 28 January 2021).
- Düzgün, N.; Kurtipek, E.; Esme, H.; Eren Karanis, M.; Tolu, İ. Pulmonary Hyalinizing Granuloma Mimicking Metastatic Lung Cancer. Case Rep. Pulmonol. 2015, 2015, 610417. [Google Scholar] [CrossRef] [PubMed]
- Guccion, J.G.; Rohatgi, P.K.; Saini, N. Pulmonary hyalinizing granuloma. Electron microscopic and immunologic studies. Chest 1984, 85, 571–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lhote, R.; Haroche, J.; Duron, L.; Girard, N.; Lafourcade, M.P.; Martin, M.; Begueret, H.; Taytard, A.; Capron, F.; Grenier, P.; et al. Pulmonary hyalinizing granuloma: A multicenter study of 5 new cases and review of the 135 cases of the literature. Immunol. Res. 2017, 65, 375–385. [Google Scholar] [CrossRef] [PubMed]
- Winger, D.I.; Spiegler, P.; Trow, T.K.; Goyal, A.; Yu, H.; Yung, E.; Katz, D.S. Radiology-Pathology Conference: Pulmonary hyalinizing granuloma associated with lupus-like anticoagulant and Morvan’s Syndrome. Clin. Imaging 2007, 31, 264–268. [Google Scholar] [CrossRef]
- Arumugam, S.; Raju, R.; Nicholson, A.G. Pulmonary hyalinising granuloma: A rare cause of multiple lung nodules in lung cancer clinic. Respir. Med. Case Rep. 2018, 25, 55–57. [Google Scholar] [CrossRef] [PubMed]
- Coleman, C.; Nassar, A.; McComb, B. Pulmonary hyalinizing granuloma associated with idiopathic thrombocytopenic purpura. J. Clin. Imaging Sci. 2014, 4, 8. [Google Scholar] [CrossRef] [PubMed]
- Schlosnagle, D.C.; Check, I.J.; Sewell, C.W.; Plummer, A.; York, R.M.; Hunter, R.L. Immunologic abnormalities in two patients with pulmonary hyalinizing granuloma. Am. J. Clin. Pathol. 1982, 78, 231–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.T.; Wang, Q.P.; Li, J.; Zhang, T.; Zhang, L.; Mao, Y.Y. Amyloidosis secondary to intrapulmonary Castleman disease mimicking pulmonary hyalinizing granuloma-like clinical features: A rare case report. Medicine 2019, 98, e15039. [Google Scholar] [CrossRef] [PubMed]
- Ünlü, Y. Pulmonary HyalInIzIng Granuloma. Selcuk Med. J. 2006, 23, 91–94. [Google Scholar]
- Ren, Y.; Raitz, E.N.; Lee, K.R.; Pingleton, S.K.; Tawfik, O. Pulmonary small lymphocytic lymphoma (mucosa-associated lymphoid tissue type) associated with pulmonary hyalinizing granuloma. Chest 2001, 120, 1027–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamona, A.; Al Lawati, F.; Kamona, A.; Al Busaidi, N.; Al Mahrooqi, Y.; Al-Tai, S.; Al Lawati, N.; Al-Umairi, R.S. Pulmonary Hyalinising Granuloma: A report of two cases. Sultan Qaboos Univ. Med. J. 2019, 19, e157–e160. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.N.; Al-Jahdali, H.H.; Allen, C.M.; Irion, K.L.; Al Ghanem, S.; Koteyar, S.S. The calcified lung nodule: What does it mean? Ann. Thorac. Med. 2010, 5, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Kawase, S.; Matsumoto, R.; Imai, S.; Kawaguchi, K.; Hata, Y.; Horita, N.; Shiota, Y. Pulmonary Hyalinizing Granuloma Mimicking Primary Lung Cancer. Intern. Med. 2018, 57, 3615–3617. [Google Scholar] [CrossRef] [Green Version]
- Gooty, V.; Harris, C.; Muelenaer, A.; Watson, B.; Safford, S.D. A rare case of pulmonary hyalinizing granuloma with calcification in a 5 year old boy. J. Pediatric Surg. Case Rep. 2015, 3, 123–126. [Google Scholar] [CrossRef] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahi, M.S.; Gunasekaran, K.; Amoah, K.; Chowdhury, F.; Kwon, J. Pulmonary Hyalinizing Granuloma: A Rare Cause of a Benign Lung Mass. Clin. Pract. 2021, 11, 37-42. https://doi.org/10.3390/clinpract11010007
Rahi MS, Gunasekaran K, Amoah K, Chowdhury F, Kwon J. Pulmonary Hyalinizing Granuloma: A Rare Cause of a Benign Lung Mass. Clinics and Practice. 2021; 11(1):37-42. https://doi.org/10.3390/clinpract11010007
Chicago/Turabian StyleRahi, Mandeep Singh, Kulothungan Gunasekaran, Kwesi Amoah, Farheen Chowdhury, and Jeff Kwon. 2021. "Pulmonary Hyalinizing Granuloma: A Rare Cause of a Benign Lung Mass" Clinics and Practice 11, no. 1: 37-42. https://doi.org/10.3390/clinpract11010007
APA StyleRahi, M. S., Gunasekaran, K., Amoah, K., Chowdhury, F., & Kwon, J. (2021). Pulmonary Hyalinizing Granuloma: A Rare Cause of a Benign Lung Mass. Clinics and Practice, 11(1), 37-42. https://doi.org/10.3390/clinpract11010007






