Abstract
(1) Background: Vertebro-medullary trauma (VMT) causes osteo-articular injuries in a varied anatomical lesion associated with multiple clinical manifestations and therapeutic indications. The neurological evaluation of patients who have suffered a spinal cord injury (SCI) is costly in testing the motor and sensory function. To standardize the assessment, several scales are used that measure the neurological deficit in order to guide subsequent treatment according to complete or incomplete SCI. The aim of this study is to identify and present the relevant tools for assessing SCI. (2) Methods: Relevant SCI studies were used for a fact-finding investigation from a rational and critical perspective of this field of research. The relationship between clinical tools and those with a psychosocial component was assessed based on studies reported in the literature. (3) Results: SCI severity scales have been proposed throughout to be able to estimate the functional prognosis of victims of these traumatic events. These tools can be divided into scales for assessing the neurological deficit due to trauma, and functional scales that assess the ability to perform daily activities, self-care, etc. (4) Conclusions: The closest scale to the need for standardization and the most accurate assessment of neurological deficits secondary to SCI is ASIA/IMSOP.
1. Introduction
Vertebro-medullary trauma (VMT) causes osteo-articular injuries of the vertebrae and their contents (marrow, nerve roots, meninges and vessels) in a varied anatomical lesional association, with multiple clinical manifestations and therapeutic indications [1]. The occurrence of a spinal cord injury (SCI) causes a disability that can manifest itself in different levels of severity, the patient having difficulties in the family, social and economic context of functioning and integration [2,3]. SCI patients face poor financial situations and poor socio-economic achievements, and the life expectancy of the disabled person is much lower [4,5]. Worldwide, there has been an obvious concern for the development and implementation of policies and programs to improve the quality of life of people with disabilities [6,7]. The aim is to ensure people’s access to specific medical services, education and viable employment opportunities [8,9,10]. It is important to add that SCI mainly affects the active population, the average age being 35 years, so the economic impact is great [11,12,13]. Another worrying aspect is the increasing incidence of patients with complete spinal cord section and quadriplegia, which implies increased care needs [14,15,16].
In order to determine the neurological and functional deficit in patients with vertebral-medullary injuries, different evaluation scales were developed. These scales have been validated and improved over the years to determine a predictive tool for the functional outcomes of patients with SCI [17,18].
Our objective is to analyze the advantages and limitations of the current scales for evaluating the neurological and functional deficit in patients with SCI.
2. Materials and Methods
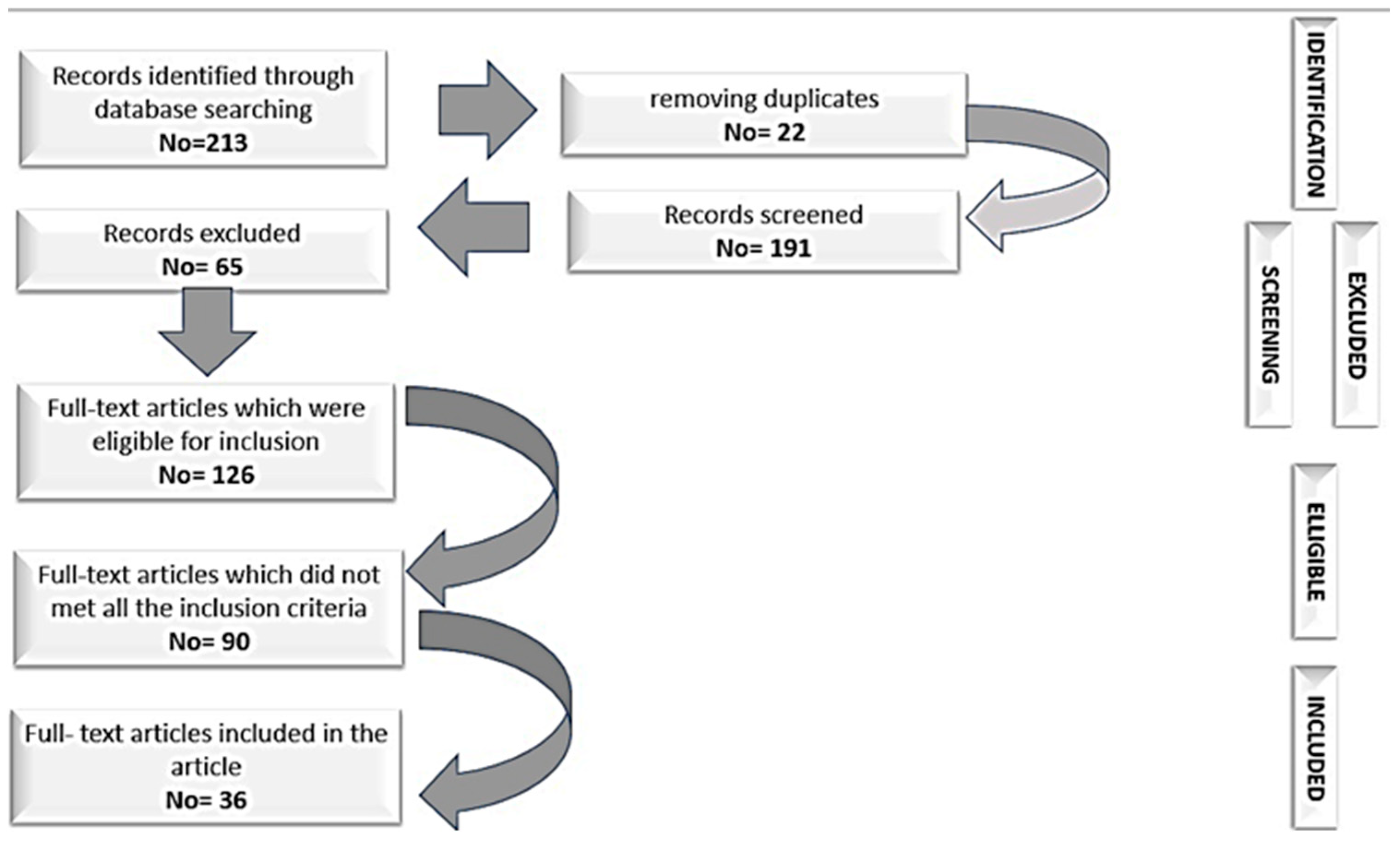
We present the tools that have proven to be a reliable standard and have direct utility in the work of clinicians. Studies supporting the fidelity and validity of SCI research and assessment tools will be presented according to the instrument presented. Relevant SCI studies were used for a fact-finding investigation from a rational and critical perspective of this field of research. The relationship between clinical tools and those with a psychosocial component was assessed based on studies reported in the literature. To achieve this goal, SCI severity and functional prognosis scales were analyzed using Medline, PubMed, Scopus, Proquest, Science Direct, Springerlink, and WOS bases, including relevant keywords supported by internationally established sites in the field, or regionally (such as the International Spinal Cord Society). In order to select the articles, we utilized the following keywords: scales, spinal cord injury, vertebro-medullary trauma, neurologic recovery, functional recovery, neurologic deficit. Studies evaluating SCI in children were excluded due to the multitude of factors that would have distorted the presented information. The study will reveal the screening criteria for inclusion and the exclusion of studies. First of all, we selected from international journals the studies that validated these scales and which presented as relevant sources of empirical and meta-analytical data. Second, to avoid misinterpretation, the selected works included only articles published in English. Thirdly, in terms of chronology, a period of 20 years was selected. The selection of studies has been implemented to ensure sufficient time to observe the evolution of international research on SCI. We believe that we offer a sufficiently long time-frame to be able to identify the elements relevant to our SCI investigation. The eligibility of studies with relevant statistical data was the last step in which an additional and more in-depth examination of the literature was performed. Consequently, this step was aimed at reviewing the titles, abstracts, and main content of each type of study, research article, validation study, and quantitative meta-analysis to ensure that they meet the inclusion criteria. The selection process for this article is illustrated in Figure 1.
Figure 1.
The selection process.
3. Results and Discussion
The need for standardization and accurate assessment of neurological deficits secondary to SCI has led to the development of various scales for their quantification, but none of them can be considered ideal, as each has its advantages and disadvantages. The choice of one or another of the scales also depends on the preferences of the doctor who uses them [19,20,21].
SCI severity scales have been proposed throughout to be able to estimate the functional prognosis of victims of these traumatic events. These tools can be divided into scales for assessing the neurological deficit due to trauma, and functional scales that assess the ability to perform daily activities, self-care, etc.
3.1. Neurological Deficit Assessment Scales
Table 1 is the neurological deficit assessment scales.

Table 1.
Neurological deficit assessment scales.
3.2. Scales for Functional Assessment of Spinal Cord Injuries
Table 2 is scales for functional assessment of spinal cord injuries. These instruments are used specifically by specialists in the field of medical and neuromotor recovery, being represented by: the Barthel Index (BI), Modified Barthel Index (MBI), Functional Independence Measure (FIM), Quadriplegic Index of Function (QIF), Spinal Cord Independence Measure (SCIM), Walking Index for Spinal Cord Injury (WISCI), and Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI). Scales of functional assessment of spinal cord injuries determine a person’s ability to perform their activities of daily living (ADL), thus determining the ability of an individual to self-care, walk alone, etc. These clinical tools are usable for a wide range of neurological conditions, especially for VMT lesions: QIF, SCIM, and SCI-FAI. Of these scales, the Barthel Index is the most widely used.

Table 2.
Functional evaluation scales of SCI.
3.3. Scales That Evaluate Both the Neurological Deficit and Functional Assessment of Patients with SCI
Table 3 is scales that evaluate both the neurological deficit and functional assessment of patients with SCI.

Table 3.
Scale for the evaluation of the neurological deficit and functional assessment of patients with SCI.
4. Conclusions
The closest scale to the need for standardization and the most accurate assessment of neurological deficits secondary to SCI is ASIA/IMSOP, adopted as the international standard for the neurological assessment of spinal cord trauma patients. The WISCI is a more accurate tool than the FIM for documenting changes in walking levels, but the FIM is more reliable in measuring patient self-care and independence.
Author Contributions
Conceptualization, C.F.L., C.L.B., G.M.M., M.B., R.B.B., G.A.C., I.B.V. and M.D.P.; methodology, C.F.L., G.M.M. and M.D.P.; software, C.F.L., G.M.M. and M.D.P.; validation, C.L.B., M.B., R.B.B., G.A.C. and I.B.V.; formal analysis, C.F.L., G.M.M. and M.D.P.; investigation, C.F.L., G.M.M. and M.D.P.; resources, C.F.L., G.M.M. and M.D.P.; data curation, C.F.L., G.M.M. and M.D.P.; writing—original draft preparation, C.F.L., C.L.B., G.M.M., M.B., R.B.B., G.A.C., I.B.V. and M.D.P.; writing—review and editing, C.F.L., G.M.M. and M.D.P.; visualization, C.F.L., C.L.B., G.M.M., M.B., R.B.B., G.A.C., I.B.V. and M.D.P.; supervision, C.F.L., G.M.M. and M.D.P.; project administration, C.F.L., G.M.M. and M.D.P.; funding acquisition, C.F.L., G.M.M. and M.D.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ramírez-Villaescusa, J.; Hidalgo, J.L.; Ruiz-Picazo, D.; Martin-Benlloch, A.; Torres-Lozano, P.; Portero-Martinez, E. The impact of urgent intervention on the neurologic recovery in patients with thoracolumbar fractures. J. Spine Surg. 2018, 4, 388. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Schmit, B.D.; Kurpad, S.N.; Budde, M.D. Acute Magnetic Resonance Imaging Predictors of Chronic Motor Function and Tissue Sparing in Rat Cervical Spinal Cord Injury. J. Neurotrauma 2022, 39, 1727–1740. [Google Scholar] [CrossRef] [PubMed]
- Moga, T.D.; Moga, I.; Sabau, S.; Nistor-Cseppento, C.D.; Iovanovici, D.C.; Cavalu, S.; Dogaru, B.G. Sarcopenia, a major clinical problem in old age, potential causes, clinical consequences and therapeutic possibilities. Balneo PRM Res. J. 2022, 13, 492. [Google Scholar] [CrossRef]
- Zürcher, C.; Tough, H.; Fekete, C.; SwiSCI, Study Group. Mental health in individuals with spinal cord injury: The role of socioeconomic conditions and social relationships. PLoS ONE 2019, 14, e0206069. [Google Scholar] [CrossRef]
- Ahmed, N.; Quadir, M.M.; Rahman, M.A.; Alamgir, H. Community integration and life satisfaction among individuals with spinal cord injury living in the community after receiving institutional care in Bangladesh. Disabil. Rehabil. 2018, 40, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Rico-Blázquez, M.; Quesada-Cubo, V.; Polentinos-Castro, E.; Sánchez-Ruano, R.; Rayo-Gómez, M.Á.; Del Cura-González, I.; CuidaCare Group. Health-related quality of life in caregivers of community-dwelling individuals with disabilities or chronic conditions. A gender-differentiated analysis in a cross-sectional study. BMC Nurs. 2022, 21, 69. [Google Scholar] [CrossRef] [PubMed]
- Moga, T.D.; Moga, I.; Venter, A.; Cavalu, S. Sarcopenia of Iliopsoas and Abdominal Muscles and Coexistence with Osteoporosis—Case Presentation. Pharmacophore 2021, 12, 61–66. [Google Scholar] [CrossRef]
- Holmlund, L.; Guidetti, S.; Eriksson, G.; Asaba, E. Return to work in the context of everyday life 7–11 years after spinal cord injury–a follow-up study. Disabil. Rehabil. 2018, 40, 2875–2883. [Google Scholar] [CrossRef]
- Mekeres, G.M.; Voiţă-Mekereş, F.; Tudoran, C.; Buhaş, C.L.; Tudoran, M.; Racoviţă, M.; Voiţă, N.C.; Pop, N.O.; Marian, M. Predictors for Estimating Scars’ Internalization in Victims with Post-Traumatic Scars versus Patients with Postsurgical Scars. Healthcare 2022, 10, 550. [Google Scholar] [CrossRef]
- Krause, J.S.; Terza, J.V.; Erten, M.; Focht, K.L.; Dismuke, C.E. Prediction of postinjury employment and percentage of time worked after spinal cord injury. Arch. Phys. Med. Rehabil. 2012, 93, 373–375. [Google Scholar] [CrossRef]
- McDaid, D.; Park, A.L.; Gall, A.; Purcell, M.; Bacon, M. Understanding and modelling the economic impact of spinal cord injuries in the United Kingdom. Spinal Cord 2019, 57, 778–788. [Google Scholar] [CrossRef] [PubMed]
- Badhiwala, J.H.; Ahuja, C.S.; Fehlings, M.G. Time is spine: A review of translational advances in spinal cord injury. J. Neurosurg. Spine 2018, 30, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Zehravi, M.; Kabir, J.; Akter, R.; Malik, S.; Ashraf, G.M.; Tagde, P.; Ramproshad, S.; Mondal, B.; Rahman, M.H.; Mohan, A.G.; et al. A Prospective Viewpoint on Neurological Diseases and Their Biomarkers. Molecules 2022, 27, 3516. [Google Scholar] [CrossRef] [PubMed]
- McCaughey, E.J.; Purcell, M.; McLean, A.N.; Fraser, M.H.; Bewick, A.; Borotkanics, R.J.; Allan, D.B. Changing demographics of spinal cord injury over a 20-year period: A longitudinal population-based study in Scotland. Spinal Cord 2016, 54, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Ahn, H.; Lewis, R.; Santos, A.; Cheng, C.L.; Noonan, V.K.; Dvorak, M.F.; Singh, A.; Linassi, A.G.; Christie, S.; Goytan, M.; et al. Forecasting Financial Resources for Future Traumatic Spinal Cord Injury Care Using Simulation Modeling. J. Neurotrauma 2017, 15, 2917–2923. [Google Scholar] [CrossRef]
- Voiță-Mekeres, F.; Buhaș, C.L.; Mekeres, G.M.; Tudoran, C.; Racovita, M.; Faur, C.I.; Tudoran, M.; Abu-Awwad, A.; Voiță, N.C.; Maghiar, T.A. Mekeres’ Psychosocial Internalization Scale: A Scale for the Evaluation of Aesthetic Prejudice in Victims of Accidents and Violence. Healthcare 2021, 9, 1440. [Google Scholar] [CrossRef]
- van Diemen, T.; Craig, A.; van Nes, I.J.W.; SELF-SCI Group; Stolwijk-Swuste, J.M.; Geertzen, J.H.B.; Middleton, J.; Post, M.W.M. Enhancing our conceptual understanding of state and trait self-efficacy by correlational analysis of four self-efficacy scales in people with spinal cord injury. BMC Psychol. 2020, 18, 108. [Google Scholar] [CrossRef]
- Oşvar, F.N.; Raţiu, A.C.; Voiţă-Mekereş, F.; Voiţă, G.F.; Bonţea, M.G.; Racoviţă, M.; Mekereş, G.M.; Bodog, F.D. Cardiac axis evaluation as a screening method for detecting cardiac abnormalities in the first trimester of pregnancy. Rom. J. Morphol. Embryol. 2020, 61, 137–142. [Google Scholar] [CrossRef]
- Schuld, C.; Franz, S.; Brüggemann, K.; Heutehaus, L.; Weidner, N.; Kirshblum, S.C.; Rupp, R.; EMSCI study group. International standards for neurological classification of spinal cord injury: Impact of the revised worksheet (revision 02/13) on classification performance. J. Spinal Cord Med. 2016, 39, 504–512. [Google Scholar] [CrossRef]
- Szabó, R.; Voiță-Mekereș, F.; Tudoran, C.; Abu-Awwad, A.; Tudoran, M.; Mihancea, P.; Ilea, C.D.N. Evaluation of Sleep Disturbances in Patients with Nocturnal Epileptic Seizures in a Romanian Cross-Sectional Study. Healthcare 2022, 10, 588. [Google Scholar] [CrossRef]
- Bremer, E.; Liska, T.M.; Arbour-Nicitopoulos, K.P.; Best, K.L.; Sweet, S.N. Examining long-term motivational and behavioral outcomes of two physical activity interventions. J. Spinal Cord Med. 2022, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Frankel, H.L.; Hancock, D.O.; Hyslop, G.; Melzak, J.; Michaelis, L.S.; Ungar, G.H.; Vernon, J.D.; Walsh, J.J. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 1969, 7, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Kirshblum, S.; Botticello, A.; Benedetto, J.; Donovan, J.; Marino, R.; Hsieh, S.; Wagaman, N. A Comparison of Diagnostic Stability of the ASIA Impairment Scale Versus Frankel Classification Systems for Traumatic Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2020, 101, 1556–1562. [Google Scholar] [CrossRef] [PubMed]
- Furlan, J.C.; Fehlings, M.G.; Tator, C.H.; Davis, A.M. Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: Psychometric properties of the ASIA Standards. J. Neurotrauma 2008, 25, 1273–1301. [Google Scholar] [CrossRef] [PubMed]
- van Middendorp, J.J.; Goss, B.; Urquhart, S.; Atresh, S.; Williams, R.P.; Schuetz, M. Diagnosis and prognosis of traumatic spinal cord injury. Glob. Spine J. 2011, 1, 1–8. [Google Scholar] [CrossRef]
- Bracken, M.B.; Webb, S.B., Jr.; Wagner, F.C. Classification of the severity of acute spinal cord injury: Implications for management. Paraplegia 1978, 15, 319–326. [Google Scholar] [CrossRef]
- Burns, S.P.; Tansey, K.E. The Expedited International Standards for Neurological Classification of Spinal Cord Injury (E-ISNCSCI). Spinal Cord 2020, 58, 633–634. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.T.; Ducker, T.B. Motor classification of spinal cord injuries with mobility, morbidity and recovery indices. Am. Surg. 1979, 45, 151–158. [Google Scholar]
- Poplawski, M.M.; Alizadeh, M.; Oleson, C.V.; Fisher, J.; Marino, R.J.; Gorniak, R.J.; Leiby, B.E.; Flanders, A.E. Application of Diffusion Tensor Imaging in Forecasting Neurological Injury and Recovery after Human Cervical Spinal Cord Injury. J. Neurotrauma 2019, 36, 3051–3061. [Google Scholar] [CrossRef]
- Chehrazi, B.; Wagner, F.C., Jr.; Collins, W.F., Jr.; Freeman, D.H., Jr. A scale for evaluation of spinal cord injury. J. Neurosurg. 1981, 54, 310–315. [Google Scholar] [CrossRef]
- Tator, C.H. Sunnybrook cord injury scales for assessing neurological injury and neurological recovery. In Early Management of Acute Spinal Cord Injury; Tator, C.H., Ed.; Raven Press: New York, NY, USA, 1982. [Google Scholar]
- Badhiwala, J.H.; Wilson, J.R.; Kwon, B.K.; Casha, S.; Fehlings, M.G. A Review of Clinical Trials in Spinal Cord Injury Including Biomarkers. J. Neurotrauma 2018, 15, 1906–1917. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, J.A.S.; Sharif, S.; Costa, F.; Rangel, J.A.I.R.; Anania, C.D.; Zileli, M. Early Management of Spinal Cord Injury: WFNS Spine Committee Recommendations. Neurospine 2020, 17, 759–784. [Google Scholar] [CrossRef] [PubMed]
- Hadley, M.N.; Walters, B.C.; Grabb, P.A.; Oyesiku, N.M.; Przybylski, G.J.; Resnick, D.K.; Ryken, T.C. Clinical assessment after acute cervical spinal cord injury. Neurosurgery 2002, 50, S21–S29. [Google Scholar] [CrossRef] [PubMed]
- El Masry, W.S.; Tsubo, M.; Katoh, S.; El Miligui, Y.H.; Khan, A. Validation of the American Spinal Injury Association (ASIA) motor score and the National Acute Spinal Cord Injury Study (NASCIS) motor score. Spine 1996, 1, 614–619. [Google Scholar] [CrossRef]
- Yugué, I.; Okada, S.; Maeda, T.; Ueta, T.; Shiba, K. Sensitivity and specificity of the ‘knee-up test’ for estimation of the American Spinal Injury Association Impairment Scale in patients with acute motor incomplete cervical spinal cord injury. Spinal Cord 2018, 56, 347–354. [Google Scholar] [CrossRef]
- Roberts, T.T.; Leonard, G.R.; Cepela, D.J. Classifications in Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin. Orthop. Relat. Res. 2017, 475, 1499–1504. [Google Scholar] [CrossRef]
- Botsford, D.J.; Esses, S.I. A new scale for the clinical assessment of spinal cord function. Orthopedics 1992, 15, 1309–1313. [Google Scholar] [CrossRef]
- Eli, I.; Lerner, D.P.; Ghogawala, Z. Acute Traumatic Spinal Cord Injury. Neurol. Clin. 2021, 39, 471–488. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Ohura, T.; Hase, K.; Nakajima, Y.; Nakayama, T. Validity and reliability of a performance evaluation tool based on the modified Barthel Index for stroke patients. BMC Med. Res. Methodol. 2017, 17, 131. [Google Scholar] [CrossRef] [PubMed]
- Forer, S.; Granger, C.V. Functional Independence Measure; The Buffalo General Hospital State University of New York at Buffalo: Buffalo, NY, USA, 1987. [Google Scholar]
- Khamnon, N.; Amatachaya, S.; Wattanapan, P.; Musika, N.; Jitmongkolsri, P.; Kongngoen, N.; Haisirikul, M.; Jaikarsen, K.; Thaweewannakij, T.; Namwong, W. Reliability and concurrent validity of the Spinal Cord Independence Measure III among rehabilitation professionals. Spinal Cord 2022, 60, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Kidd, D.; Stewart, G.; Baldry, J.; Johnson, J.; Rossiter, D.; Petruckevitch, A.; Thompson, A.J. The Functional Independence Measure: A comparative validity and reliability study. Disabil. Rehabil. 1995, 17, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Gresham, G.E.; Labi, M.L.; Dittmar, S.S.; Hicks, J.T.; Joyce, S.Z.; Stehlik, M.A. The Quadriplegia Index of Function (QIF): Sensitivity and reliability demonstrated in a study of thirty quadriplegic patients. Paraplegia 1986, 24, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Brizuela, G.; Sinz, S.; Aranda, R.; Martínez-Navarro, I. The effect of arm-crank exercise training on power output, spirometric and cardiac function and level of autonomy in persons with tetraplegia. Eur. J. Sport Sci. 2020, 20, 926–934. [Google Scholar] [CrossRef]
- Catz, A.; Itzkovich, M.; Agranov, E.; Ring, H.; Tamir, A. SCIM–spinal cord independence measure: A new disability scale for patients with spinal cord lesions. Spinal Cord 1997, 35, 850–856. [Google Scholar] [CrossRef]
- Harvey, L.A.; Glinsky, J.V.; Chu, J. Do any physiotherapy interventions increase spinal cord independence measure or functional independence measure scores in people with spinal cord injuries? A systematic review. Spinal Cord 2021, 59, 705–715. [Google Scholar] [CrossRef]
- Itzkovich, M.; Gelernter, I.; Biering-Sorensen, F.; Weeks, C.; Laramee, M.T.; Craven, B.C.; Tonack, M.; Hitzig, S.L.; Glaser, E.; Zeilig, G.; et al. The Spinal Cord Independence Measure (SCIM) version III: Reliability and validity in a multi-center international study. Disabil. Rehabil. 2007, 29, 1926–1933. [Google Scholar] [CrossRef]
- Burns, A.S.; Delparte, J.J.; Patrick, M.; Marino, R.J.; Ditunno, J.F. The reproducibility and convergent validity of the walking index for spinal cord injury (WISCI) in chronic spinal cord injury. Neurorehabil. Neural Repair. 2011, 25, 149–157. [Google Scholar] [CrossRef]
- Dittuno, P.L.; Ditunno, J.F., Jr. Walking index for spinal cord injury (WISCI II): Scale revision. Spinal Cord 2001, 39, 654–656, Erratum in: Spinal Cord 2009, 47, 349. [Google Scholar] [CrossRef]
- Ditunno, J.; Scivoletto, G. Clinical relevance of gait research applied to clinical trials in spinal cord injury. Brain Res. Bull. 2009, 78, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Field-Fote, E.C.; Fluet, G.G.; Schafer, S.D.; Schneider, E.M.; Smith, R.; Downey, P.A.; Ruhl, C.D. The Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI). J. Rehabil. Med. 2001, 33, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Eckert, M.J.; Martin, M.J. Trauma: Spinal Cord Injury. Surg. Clin. N. Am. 2017, 97, 1031–1045. [Google Scholar] [CrossRef] [PubMed]
- Kirshblum, S.; Snider, B.; Rupp, R.; Read, M.S. International Standards Committee of ASIA and ISCoS. Updates of the International Standards for Neurologic Classification of Spinal Cord Injury: 2015 and 2019. Phys. Med. Rehabil. Clin. N. Am. 2020, 31, 319–330. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).