Radiological Insights into Sacroiliitis: A Narrative Review
Abstract
:1. Introduction
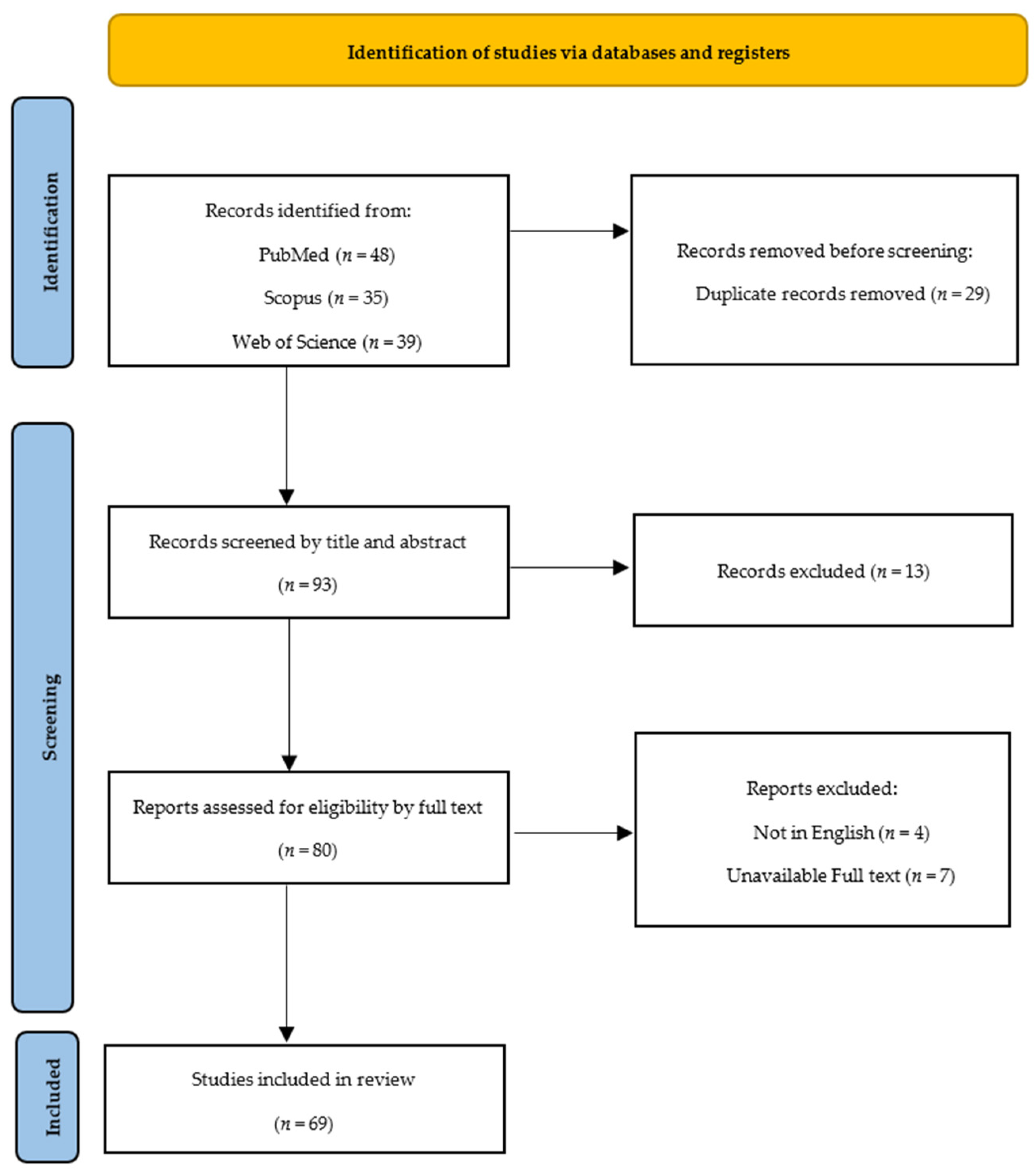
2. Materials and Methods
3. Results and Discussion
3.1. Anatomy of the Sacroiliac Joint
3.2. Clinical Presentation and Etiology of Sacroiliitis
3.3. Radiological Findings and Imaging Modalities
3.3.1. Plain Radiographs
3.3.2. Computed Tomography
3.3.3. Magnetic Resonance Imaging
3.3.4. Nuclear Medicine—Bone Scans
3.4. Radiological Criteria and Scoring Systems
3.5. Management of Sacroiliitis
3.6. Emerging Technologies and Future Perspectives
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baronio, M.; Sadia, H.; Paolacci, S.; Prestamburgo, D.; Miotti, D.; Guardamagna, V.A.; Natalini, G.; Bertelli, M. Etiopathogenesis of sacroiliitis: Implications for assessment and management. Korean J. Pain. 2020, 33, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Vleeming, A.; Schuenke, M.D.; Masi, A.T.; Carreiro, J.E.; Danneels, L.; Willard, F.H. The sacroiliac joint: An overview of its anatomy, function and potential clinical implications. J. Anat. 2012, 221, 537–567. [Google Scholar] [CrossRef]
- Lee, A.; Gupta, M.; Boyinepally, K.; Stokey, P.J.; Ebraheim, N.A. Sacroiliitis: A Review on Anatomy, Diagnosis, and Treatment. Adv. Orthop. 2022, 2022, 3283296. [Google Scholar] [CrossRef] [PubMed]
- Canella, C.; Schau, B.; Ribeiro, E.; Sbaffi, B.; Marchiori, E. MRI in Seronegative Spondyloarthritis: Imaging Features and Differential Diagnosis in the Spine and Sacroiliac Joints. Am. J. Roentgenol. 2013, 200, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Triantafyllou, M.; Klontzas, M.E.; Koltsakis, E.; Papakosta, V.; Spanakis, K.; Karantanas, A.H. Radiomics for the Detection of Active Sacroiliitis Using MR Imaging. Diagnostics 2023, 13, 2587. [Google Scholar] [CrossRef] [PubMed]
- Zilber, K.; Gorenberg, M.; Rimar, D.; Boulman, N.; Kaly, L.; Rozenbaum, M.; Rosner, I.; Slobodin, G. Radionuclide Methods in the Diagnosis of Sacroiliitis in Patients with Spondyloarthritis: An Update. Rambam Maimonides Med. J. 2016, 7, e0037. [Google Scholar] [CrossRef]
- Hemke, R.; Herregods, N.; Jaremko, J.L.; Åström, G.; Avenarius, D.; Becce, F.; Bielecki, D.K.; Boesen, M.; Dalili, D.; Giraudo, C.; et al. Imaging assessment of children presenting with suspected or known juvenile idiopathic arthritis: ESSR-ESPR points to consider. Eur. Radiol. 2020, 30, 5237–5249. [Google Scholar] [CrossRef]
- Proft, F.; Vahldiek, J.; Nicolaes, J.; Tham, R.; Hoepken, B.; Ufuktepe, B.; Bressem, K.; Poddubnyy, D. POS0896 Analysis of the performance of an artificial intelligence algorithm for the detection of radiographic sacroiliitis in an independent cohort of axspa patients including both nr-axspa and r-axspa. Ann. Rheum. Dis. 2023, 82, 755–756. [Google Scholar] [CrossRef]
- Matthew, J.P.; Joanne, E.M.; Patrick, M.B.; Isabelle, B.; Tammy, C.H.; Cynthia, D.M.; Larissa, S.; Jennifer, M.T.; Elie, A.A.; Sue, E.B.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Calvillo, O.; Skaribas, I.; Turnipseed, J. Anatomy and pathophysiology of the sacroiliac joint. Curr. Rev. Pain. 2000, 4, 356–361. [Google Scholar] [CrossRef]
- Gartenberg, A.; Nessim, A.; Cho, W. Sacroiliac joint dysfunction: Pathophysiology, diagnosis, and treatment. Eur. Spine J. 2021, 30, 2936–2943. [Google Scholar] [CrossRef] [PubMed]
- Navallas, M.; Ares, J.; Beltrán, B.; Lisbona, M.P.; Maymó, J.; Solano, A. Sacroiliitis associated with axial spondyloarthropathy: New concepts and latest trends. Radiographics 2013, 33, 933–956. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, C.; Griffith, J.F.; Lee, R.K.L.; Wong, P.C.H.; Tam, L.S. Imaging of sacroiliitis: Current status, limitations and pitfalls. Quant. Imaging Med. Surg. 2019, 9, 318–335. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P. Sacroiliac joint pain: A comprehensive review of anatomy, diagnosis, and treatment. Anesth. Analg. 2005, 101, 1440–1453. [Google Scholar] [CrossRef] [PubMed]
- Foley, B.S.; Buschbacher, R.M. Sacroiliac joint pain: Anatomy, biomechanics, diagnosis, and treatment. Am. J. Phys. Med. Rehabil. 2006, 85, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Kiapour, A.; Joukar, A.; Elgafy, H.; Erbulut, D.U.; Agarwal, A.K.; Goel, V.K. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int. J. Spine Surg. 2020, 14, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Ashby, K.; Yilmaz, E.; Mathkour, M.; Olewnik, Ł.; Hage, D.; Iwanaga, J.; Loukas, M.; Tubbs, R.S. Ligaments stabilizing the sacrum and sacroiliac joint: A comprehensive review. Neurosurg. Rev. 2022, 45, 357–364. [Google Scholar] [CrossRef]
- Cox, M.; Ng, G.; Mashriqi, F.; Iwanaga, J.; Alonso, F.; Tubbs, K.; Loukas, M.; Oskouian, R.J.; Tubbs, R.S. Innervation of the Anterior Sacroiliac Joint. World Neurosurg. 2017, 107, 750–752. [Google Scholar] [CrossRef]
- Roberts, S.L.; Burnham, R.S.; Ravichandiran, K.; Agur, A.M.; Loh, E.Y. Cadaveric study of sacroiliac joint innervation: Implications for diagnostic blocks and radiofrequency ablation. Reg. Anesth. Pain. Med. 2014, 39, 456–464. [Google Scholar] [CrossRef]
- Kennedy, D.J.; Engel, A.; Kreiner, D.S.; Nampiaparampil, D.; Duszynski, B.; MacVicar, J. Fluoroscopically Guided Diagnostic and Therapeutic Intra-Articular Sacroiliac Joint Injections: A Systematic Review. Pain. Med. 2015, 16, 1500–1518. [Google Scholar] [CrossRef]
- Slobodin, G.; Rimar, D.; Boulman, N.; Kaly, L.; Rozenbaum, M.; Rosner, I.; Odeh, M. Acute sacroiliitis. Clin. Rheumatol. 2016, 35, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Vyskocil, J.J.; McIlroy, M.A.; Brennan, T.A.; Wilson, F.M. Pyogenic infection of the sacroiliac joint. Case reports and review of the literature. Medicine 1991, 70, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Cohn, S.M.; Schoetz, D.J., Jr. Pyogenic sacroiliitis: Another imitator of the acute abdomen. Surgery 1986, 100, 95–98. [Google Scholar] [PubMed]
- Cohen, S.P.; Chen, Y.; Neufeld, N.J. Sacroiliac joint pain: A comprehensive review of epidemiology, diagnosis and treatment. Expert. Rev. Neurother. 2013, 13, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Prather, H. Sacroiliac joint pain: Practical management. Clin. J. Sport. Med. 2003, 13, 252–255. [Google Scholar] [CrossRef] [PubMed]
- Zelle, B.A.; Gruen, G.S.; Brown, S.; George, S. Sacroiliac joint dysfunction: Evaluation and management. Clin. J. Pain. 2005, 21, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Prather, H.; Hunt, D. Conservative management of low back pain, part I. Sacroiliac joint pain. Dis. Mon. 2004, 50, 670–683. [Google Scholar] [CrossRef] [PubMed]
- Kurnutala, L.N.; Ghatol, D.; Upadhyay, A. Clostridium Sacroiliitis (Gas Gangrene) Following Sacroiliac Joint Injection--Case Report and Review of the Literature. Pain. Physician 2015, 18, E629–E632. [Google Scholar] [CrossRef]
- Doita, M.; Yoshiya, S.; Nabeshima, Y.; Tanase, Y.; Nishida, K.; Miyamoto, H.; Watanabe, Y.; Kurosaka, M. Acute pyogenic sacroiliitis without predisposing conditions. Spine 2003, 28, E384–E389. [Google Scholar] [CrossRef]
- Horowitz, D.L.; Katzap, E.; Horowitz, S.; Barilla-LaBarca, M.L. Approach to septic arthritis. Am. Fam. Physician 2011, 84, 653–660. [Google Scholar]
- Moreno Martinez, M.J.; Moreno Ramos, M.J.; Linares Ferrando, L.F. Sacroiliitis due to calcium pyrophosphate deposition disease. Reum. Clin. 2018, 14, 175–176. [Google Scholar] [CrossRef] [PubMed]
- Carovac, A.; Smajlovic, F.; Junuzovic, D. Application of ultrasound in medicine. Acta Inf. Med. 2011, 19, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Müller, K.; Aichert, A.; Unberath, M.; Thies, J.; Choi, J.H.; Fahrig, R.; Maier, A. Marker-free motion correction in weight-bearing cone-beam CT of the knee joint. Med. Phys. 2016, 43, 1235–1248. [Google Scholar] [CrossRef] [PubMed]
- Raza, K.; Lee, C.Y.; Pilling, D.; Heaton, S.; Situnayake, R.D.; Carruthers, D.M.; Buckley, C.D.; Gordon, C.; Salmon, M. Ultrasound guidance allows accurate needle placement and aspiration from small joints in patients with early inflammatory arthritis. Rheumatology 2003, 42, 976–979. [Google Scholar] [CrossRef] [PubMed]
- Carotti, M.; Benfaremo, D.; Di Carlo, M.; Ceccarelli, L.; Luchetti, M.M.; Piccinni, P.; Giovagnoni, A.; Salaffi, F. Dual-energy computed tomography for the detection of sacroiliac joints bone marrow oedema in patients with axial spondyloarthritis. Clin. Exp. Rheumatol. 2021, 39, 1316–1323. [Google Scholar] [CrossRef]
- Sanghavi, P.S.; Jankharia, B.G. Applications of dual energy CT in clinical practice: A pictorial essay. Indian J. Radiol. Imaging 2019, 29, 289–298. [Google Scholar] [CrossRef]
- Ulas, S.T.; Proft, F.; Diekhoff, T.; Rios Rodriguez, V.; Rademacher, J.; Poddubnyy, D.; Ziegeler, K. HLA-B27 status and inflammatory MRI lesions of the sacroiliac joints: A post hoc analysis in patients without axial spondyloarthritis. RMD Open 2023, 9, e003357. [Google Scholar] [CrossRef]
- Alqatari, S.; Visevic, R.; Marshall, N.; Ryan, J.; Murphy, G. An unexpected cause of sacroiliitis in a patient with gout and chronic psoriasis with inflammatory arthritis: A case report. BMC Musculoskelet. Disord. 2018, 19, 126. [Google Scholar] [CrossRef]
- Mathews, C.J.; Kingsley, G.; Field, M.; Jones, A.; Weston, V.C.; Phillips, M.; Walker, D.; Coakley, G. Management of septic arthritis: A systematic review. Ann. Rheum. Dis. 2007, 66, 440–445. [Google Scholar] [CrossRef]
- Zell, M.; Zhang, D.; FitzGerald, J. Diagnostic advances in synovial fluid analysis and radiographic identification for crystalline arthritis. Curr. Opin. Rheumatol. 2019, 31, 134–143. [Google Scholar] [CrossRef]
- Zahar, A.; Lausmann, C.; Cavalheiro, C.; Dhamangaonkar, A.C.; Bonanzinga, T.; Gehrke, T.; Citak, M. How Reliable Is the Cell Count Analysis in the Diagnosis of Prosthetic Joint Infection? J. Arthroplast. 2018, 33, 3257–3262. [Google Scholar] [CrossRef] [PubMed]
- Tian, Q.; Na, L.; Cao, S.; Tian, Z.; Guo, Z. Clinical features and surgical management of tuberculous arthritis of the sacroiliac joint: A retrospective analysis of 33 patients. BMC Surg. 2022, 22, 322. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.G.; Jaremko, J.L.; Rumsey, D.G.; Stimec, J.; Tse, S.M.L.; Otobo, T.M.; Adams-Webber, T.; Doria, A.S. Diagnostic Accuracy of MRI-Based Sacroiliitis Scoring Systems: A Systematic Review. Am. J. Roentgenol. 2019, 212, 1112–1125. [Google Scholar] [CrossRef] [PubMed]
- Sudoł-Szopinska, I.; Urbanik, A. Diagnostic imaging of sacroiliac joints and the spine in the course of spondyloarthropathies. Pol. J. Radiol. 2013, 78, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Al-Zaghal, A.; Yellanki, D.P.; Kothekar, E.; Werner, T.J.; Høilund-Carlsen, P.F.; Alavi, A. Sacroiliac Joint Asymmetry Regarding Inflammation and Bone Turnover: Assessment by FDG and NaF PET/CT. Asia Ocean. J. Nucl. Med. Biol. 2019, 7, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Pialat, J.B.; Di Marco, L.; Feydy, A.; Peyron, C.; Porta, B.; Himpens, P.H.; Ltaief-Boudrigua, A.; Aubry, S. Sacroiliac joints imaging in axial spondyloarthritis. Diagn. Interv. Imaging 2016, 97, 697–708. [Google Scholar] [CrossRef]
- Slobodin, G.; Hussein, H.; Rosner, I.; Eshed, I. Sacroiliitis—Early diagnosis is key. J. Inflamm. Res. 2018, 11, 339–344. [Google Scholar] [CrossRef]
- Koppula, B.R.; Morton, K.A.; Al-Dulaimi, R.; Fine, G.C.; Damme, N.M.; Brown, R.K.J. SPECT/CT in the Evaluation of Suspected Skeletal Pathology. Tomography 2021, 7, 581–605. [Google Scholar] [CrossRef]
- Bonadio, M.B.; Filho, A.G.O.; Helito, C.P.; Stump, X.M.; Demange, M.K. Bone Marrow Lesion: Image, Clinical Presentation, and Treatment. Magn. Reson. Insights 2017, 10, 1178623x17703382. [Google Scholar] [CrossRef]
- Wagle, S.; Gu, J.T.; Courtier, J.L.; Phelps, A.S.; Lin, C.; MacKenzie, J.D. Value of dedicated small-field-of-view sacroiliac versus large-field-of-view pelvic magnetic resonance imaging for evaluating pediatric sacroiliitis. Pediatr. Radiol. 2019, 49, 933–940. [Google Scholar] [CrossRef]
- Patnaik, S.; Jyotsnarani, Y.; Uppin, S.G.; Susarla, R. Imaging features of primary tumors of the spine: A pictorial essay. Indian J. Radiol. Imaging 2016, 26, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Mugera, C.; Suh, K.J.; Huisman, T.A.G.M.; Weber, K.; Belzberg, A.J.; Carrino, J.A.; Chhabra, A. Sclerotic lesions of the spine: MRI assessment. J. Magn. Reson. Imaging 2013, 38, 1310–1324. [Google Scholar] [CrossRef] [PubMed]
- Kehl, A.S.; Corr, M.; Weisman, M.H. Review: Enthesitis: New Insights Into Pathogenesis, Diagnostic Modalities, and Treatment. Arthritis Rheumatol. 2016, 68, 312–322. [Google Scholar] [CrossRef] [PubMed]
- Kinno, M.; Sutter, J. Gadolinium-Based Contrast Agents. In Magnetic Resonance Imaging of Congenital Heart Disease; Syed, M.A., Mohiaddin, R.H., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 51–57. [Google Scholar]
- Del Grande, F.; Santini, F.; Herzka, D.A.; Aro, M.R.; Dean, C.W.; Gold, G.E.; Carrino, J.A. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics 2014, 34, 217–233. [Google Scholar] [CrossRef] [PubMed]
- Delfaut, E.M.; Beltran, J.; Johnson, G.; Rousseau, J.; Marchandise, X.; Cotten, A. Fat suppression in MR imaging: Techniques and pitfalls. Radiographics 1999, 19, 373–382. [Google Scholar] [CrossRef] [PubMed]
- van der Linden, S.; Valkenburg, H.A.; Cats, A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984, 27, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Maraghelli, D.; Brandi, M.L.; Matucci Cerinic, M.; Peired, A.J.; Colagrande, S. Edema-like marrow signal intensity: A narrative review with a pictorial essay. Skelet. Radiol. 2021, 50, 645–663. [Google Scholar] [CrossRef]
- Wang, X.; Hunter, D.J.; Jin, X.; Ding, C. The importance of synovial inflammation in osteoarthritis: Current evidence from imaging assessments and clinical trials. Osteoarthr. Cartil. 2018, 26, 165–174. [Google Scholar] [CrossRef]
- Walsh, J.A.; Magrey, M. Clinical Manifestations and Diagnosis of Axial Spondyloarthritis. J. Clin. Rheumatol. 2021, 27, e547–e560. [Google Scholar] [CrossRef]
- Mease, P.; Deodhar, A. Differentiating nonradiographic axial spondyloarthritis from its mimics: A narrative review. BMC Musculoskelet. Disord. 2022, 23, 240. [Google Scholar] [CrossRef]
- Manolios, N.; Ali, M.; Camden, B.; Aflaky, E.; Pavic, K.; Markewycz, A.; De Costa, R.; Angelides, S. Evaluating disease activity in patients with ankylosing spondylitis and rheumatoid arthritis using 99mtc-glucosamine. Eur. J. Rheumatol. 2016, 3, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Van den Wyngaert, T.; Strobel, K.; Kampen, W.U.; Kuwert, T.; van der Bruggen, W.; Mohan, H.K.; Gnanasegaran, G.; Delgado-Bolton, R.; Weber, W.A.; Beheshti, M.; et al. The EANM practice guidelines for bone scintigraphy. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1723–1738. [Google Scholar] [CrossRef] [PubMed]
- Koç, Z.P.; Kin Cengiz, A.; Aydın, F.; Samancı, N.; Yazısız, V.; Koca, S.S.; Karayalçın, B. Sacroiliac indicis increase the specificity of bone scintigraphy in the diagnosis of sacroiliitis. Mol. Imaging Radionucl. Ther. 2015, 24, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Heindel, W.; Gübitz, R.; Vieth, V.; Weckesser, M.; Schober, O.; Schäfers, M. The diagnostic imaging of bone metastases. Dtsch. Arztebl. Int. 2014, 111, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Wahl, R.L.; Herman, J.M.; Ford, E. The promise and pitfalls of positron emission tomography and single-photon emission computed tomography molecular imaging-guided radiation therapy. Semin. Radiat. Oncol. 2011, 21, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.C. Radiation risk from medical imaging. Mayo Clin. Proc. 2010, 85, 1142–1146. [Google Scholar] [CrossRef] [PubMed]
- Maksymowych, W.P.; Inman, R.D.; Salonen, D.; Dhillon, S.S.; Williams, M.; Stone, M.; Conner-Spady, B.; Palsat, J.; Lambert, R.G. Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. Arthritis Rheum. 2005, 53, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, T.T.; Manchikanti, L.; Gupta, S.; Aydin, S.M.; Kim, C.H.; Solanki, D.; Nampiaparampil, D.E.; Singh, V.; Staats, P.S.; Hirsch, J.A. Systematic Review of the Diagnostic Accuracy and Therapeutic Effectiveness of Sacroiliac Joint Interventions. Pain Physician 2015, 18, E713–E756. [Google Scholar] [CrossRef]
- Polsunas, P.J.; Sowa, G.; Fritz, J.M.; Gentili, A.; Morone, N.E.; Raja, S.N.; Rodriguez, E.; Schmader, K.; Scholten, J.D.; Weiner, D.K. Deconstructing Chronic Low Back Pain in the Older Adult—Step by Step Evidence and Expert-Based Recommendations for Evaluation and Treatment: Part X: Sacroiliac Joint Syndrome. Pain. Med. 2016, 17, 1638–1647. [Google Scholar] [CrossRef]
- Kim, S.; Lee, K.L.; Baek, H.L.; Jang, S.J.; Moon, S.M.; Cho, Y.K. A Case of Acute Pyogenic Sacroiliitis and Bacteremia Caused by Community-Acquired Methicillin-Resistant Staphylococcus aureus. Infect. Chemother. 2013, 45, 441–445. [Google Scholar] [CrossRef]
- Feldman, L.S. Salmonella septic sacroiliitis: Case report and review. Pediatr. Infect. Dis. J. 2006, 25, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Borges, A.P.; Antunes, C.; Curvo-Semedo, L. Pros and Cons of Dual-Energy CT Systems: “One Does Not Fit All”. Tomography 2023, 9, 195–216. [Google Scholar] [CrossRef] [PubMed]
- Odedra, D.; Narayanasamy, S.; Sabongui, S.; Priya, S.; Krishna, S.; Sheikh, A. Dual Energy CT Physics-A Primer for the Emergency Radiologist. Front. Radiol. 2022, 2, 820430. [Google Scholar] [CrossRef] [PubMed]
- Wolharn, L.; Guggenberger, R.; Higashigaito, K.; Sartoretti, T.; Winklhofer, S.; Chung, C.B.; Finkenstaedt, T. Detailed bone assessment of the sacroiliac joint in a prospective imaging study: Comparison between computed tomography, zero echo time, and black bone magnetic resonance imaging. Skelet. Radiol. 2022, 51, 2307–2315. [Google Scholar] [CrossRef] [PubMed]
- Cornejo, J.; Cornejo-Aguilar, J.A.; Vargas, M.; Helguero, C.G.; Milanezi de Andrade, R.; Torres-Montoya, S.; Asensio-Salazar, J.; Rivero Calle, A.; Martínez Santos, J.; Damon, A.; et al. Anatomical Engineering and 3D Printing for Surgery and Medical Devices: International Review and Future Exponential Innovations. Biomed. Res. Int. 2022, 2022, 6797745. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals-Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef]
- Aranke, M.; McCrudy, G.; Rooney, K.; Patel, K.; Lee, C.A.; Hasoon, J.; Kaye, A.D. Minimally Invasive and Conservative Interventions for the Treatment of Sacroiliac Joint Pain: A Review of Recent Literature. Orthop. Rev. 2022, 14, 34098. [Google Scholar] [CrossRef]
- Huang, Y.; Chen, Y.; Liu, T.; Lin, S.; Yin, G.; Xie, Q. Impact of tumor necrosis factor α inhibitors on MRI inflammation in axial spondyloarthritis assessed by Spondyloarthritis Research Consortium Canada score: A meta-analysis. PLoS ONE 2020, 15, e0244788. [Google Scholar] [CrossRef]
- Nash, P.; Kerschbaumer, A.; Dörner, T.; Dougados, M.; Fleischmann, R.M.; Geissler, K.; McInnes, I.; Pope, J.E.; van der Heijde, D.; Stoffer-Marx, M.; et al. Points to consider for the treatment of immune-mediated inflammatory diseases with Janus kinase inhibitors: A consensus statement. Ann. Rheum. Dis. 2021, 80, 71–87. [Google Scholar] [CrossRef]
- Braun, J.; Kiltz, U.; Baraliakos, X. Management of Axial Spondyloarthritis—Insights into Upadacitinib. Drug Des. Dev. Ther. 2022, 16, 3609–3620. [Google Scholar] [CrossRef]
- Lee, S.; Jeon, U.; Lee, J.H.; Kang, S.; Kim, H.; Lee, J.; Chung, M.J.; Cha, H.S. Artificial intelligence for the detection of sacroiliitis on magnetic resonance imaging in patients with axial spondyloarthritis. Front. Immunol. 2023, 14, 1278247. [Google Scholar] [CrossRef] [PubMed]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Tao, X.; Liang, T.; Jiang, J.; Zhu, J.; Wu, S.; Chen, L.; Zhang, Z.; Zhou, C.; Sun, X.; et al. Comprehensive AI-assisted tool for ankylosing spondylitis based on multicenter research outperforms human experts. Front. Public Health 2023, 11, 1063633. [Google Scholar] [CrossRef] [PubMed]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, X.; Cao, X.; Huang, C.; Liu, E.; Qian, S.; Liu, X.; Wu, Y.; Dong, F.; Qiu, C.-W.; et al. Artificial intelligence: A powerful paradigm for scientific research. Innovation 2021, 2, 100179. [Google Scholar] [CrossRef]
- Lee, K.-H.; Lee, R.-W.; Lee, K.-H.; Park, W.; Kwon, S.-R.; Lim, M.-J. The Development and Validation of an AI Diagnostic Model for Sacroiliitis: A Deep-Learning Approach. Diagnostics 2023, 13, 3643. [Google Scholar] [CrossRef]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Mnayyis, A.; Obeidat, S.; Badr, A.; Jouryyeh, B.; Azzam, S.; Al Bibi, H.; Al-Gwairy, Y.; Al Sharie, S.; Varrassi, G. Radiological Insights into Sacroiliitis: A Narrative Review. Clin. Pract. 2024, 14, 106-121. https://doi.org/10.3390/clinpract14010009
Al-Mnayyis A, Obeidat S, Badr A, Jouryyeh B, Azzam S, Al Bibi H, Al-Gwairy Y, Al Sharie S, Varrassi G. Radiological Insights into Sacroiliitis: A Narrative Review. Clinics and Practice. 2024; 14(1):106-121. https://doi.org/10.3390/clinpract14010009
Chicago/Turabian StyleAl-Mnayyis, Asma’a, Shrouq Obeidat, Ammar Badr, Basil Jouryyeh, Saif Azzam, Hayat Al Bibi, Yara Al-Gwairy, Sarah Al Sharie, and Giustino Varrassi. 2024. "Radiological Insights into Sacroiliitis: A Narrative Review" Clinics and Practice 14, no. 1: 106-121. https://doi.org/10.3390/clinpract14010009
APA StyleAl-Mnayyis, A., Obeidat, S., Badr, A., Jouryyeh, B., Azzam, S., Al Bibi, H., Al-Gwairy, Y., Al Sharie, S., & Varrassi, G. (2024). Radiological Insights into Sacroiliitis: A Narrative Review. Clinics and Practice, 14(1), 106-121. https://doi.org/10.3390/clinpract14010009







