Acute Appendicitis or Appendiceal Diverticulitis? A Case Report and Systematic Literature Review
Abstract
1. Introduction
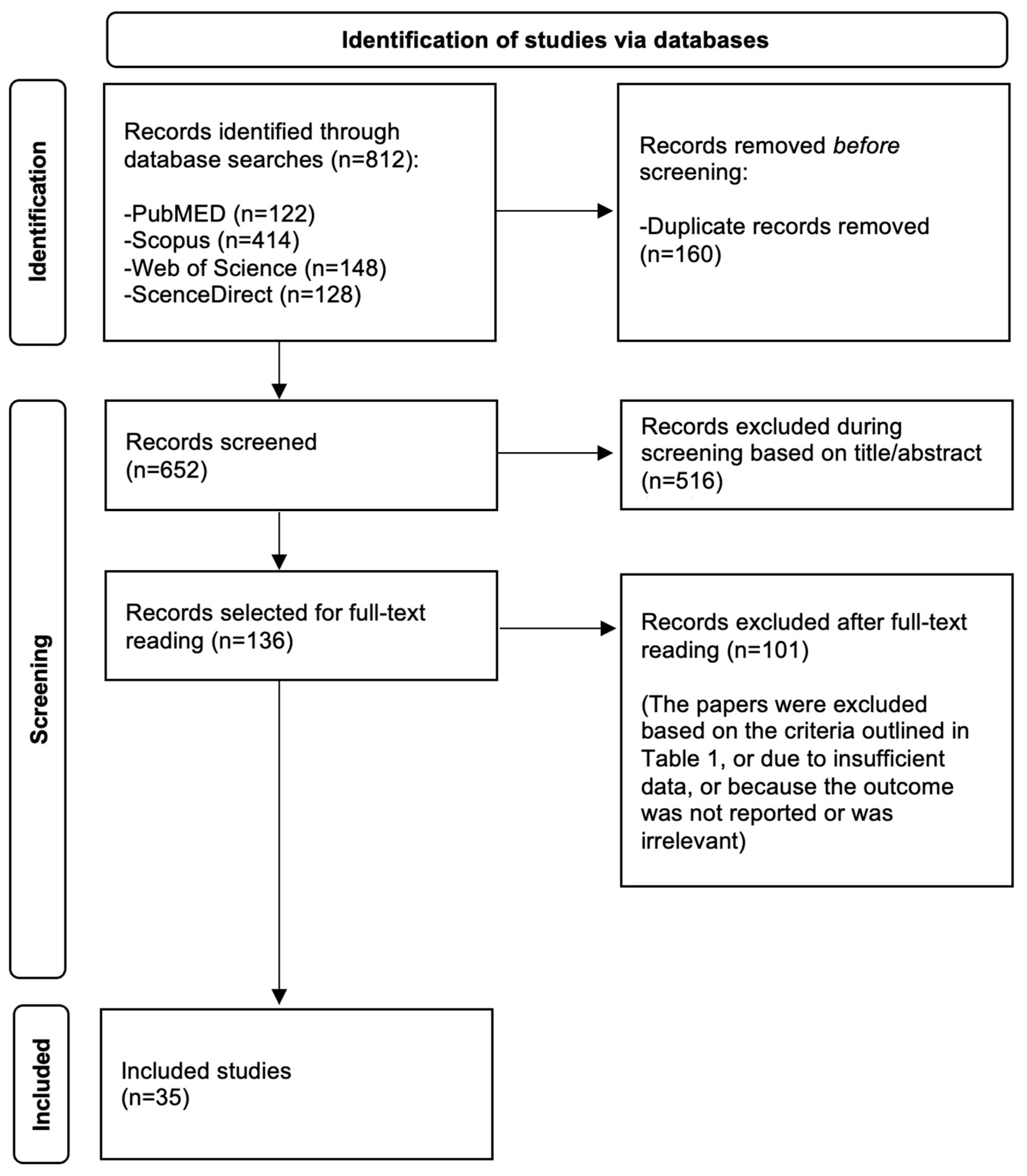
2. Methods
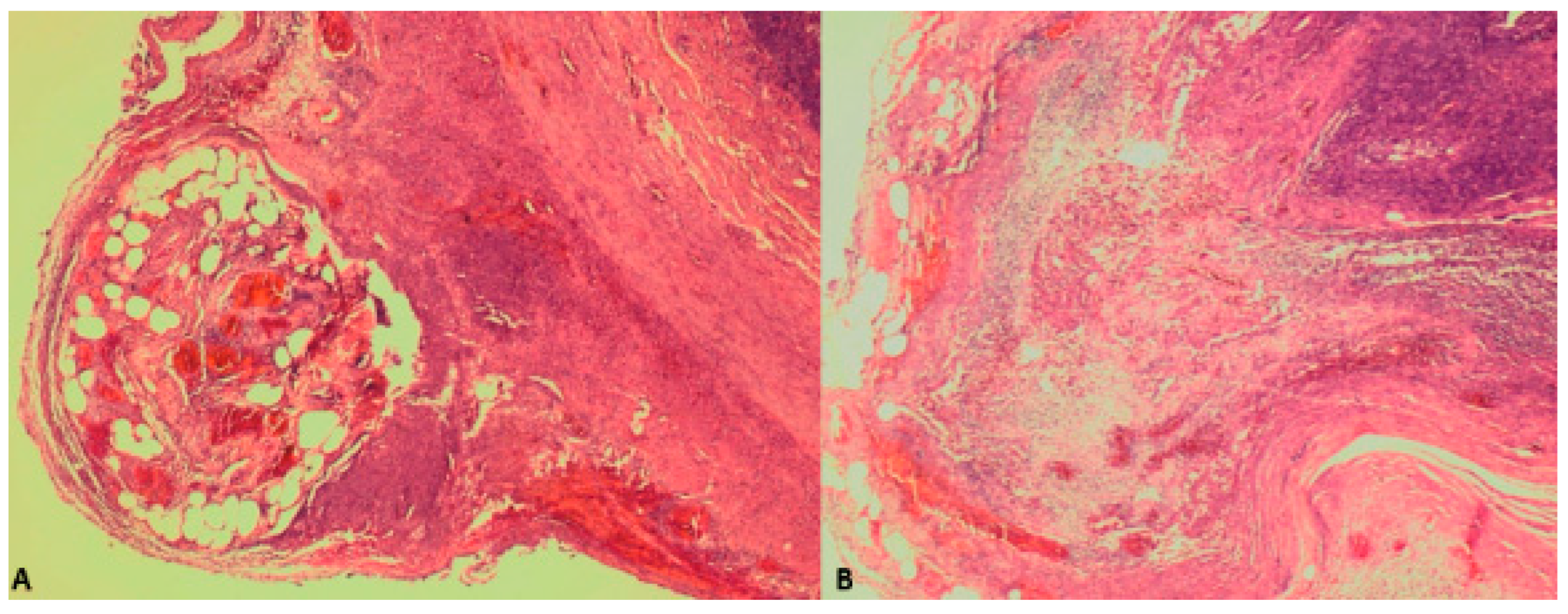
3. Case Report
4. Discussion
4.1. Review of the Literature
4.2. Comparison Between the Clinical and Laboratory Findings of Acute Appendicitis and Appendiceal Diverticulitis
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Constantin, M.; Petrescu, L.; Mătanie, C.; Vrancianu, C.O.; Niculescu, A.-G.; Andronic, O.; Bolocan, A. The Vermiform Appendix and Its Pathologies. Cancers 2023, 15, 3872. [Google Scholar] [CrossRef] [PubMed]
- Jukić, M.; Nizeteo, P.; Matas, J.; Pogorelić, Z. Trends and Predictors of Pediatric Negative Appendectomy Rates: A Single-Centre Retrospective Study. Children 2023, 10, 887. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Letourneau, I.D.; Abate, Y.H.; Abdelmasseh, M.; Abu-Gharbieh, E.; Adane, T.D.; Ahinkorah, B.O.; Ahmad, A.; Ahmadi, A.; Ahmed, A.; et al. Trends and Levels of the Global, Regional, and National Burden of Appendicitis between 1990 and 2021: Findings from the Global Burden of Disease Study 2021. Lancet Gastroenterol. Hepatol. 2024, 9, 825–858. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Janković Marendić, I.; Čohadžić, T.; Jukić, M. Clinical outcomes of daytime versus nighttime laparoscopic appendectomy in children. Children 2023, 10, 750. [Google Scholar] [CrossRef]
- Lamm, R.; Kumar, S.S.; Collings, A.T.; Haskins, I.N.; Abou-Setta, A.; Narula, N.; Nepal, P.; Hanna, N.M.; Athanasiadis, D.I.; Scholz, S.; et al. Diagnosis and Treatment of Appendicitis: Systematic Review and Meta-Analysis. Surg. Endosc. 2023, 37, 8933–8990. [Google Scholar] [CrossRef]
- Males, I.; Boban, Z.; Kumric, M.; Vrdoljak, J.; Berkovic, K.; Pogorelic, Z.; Bozic, J. Applying an explainable machine learning model might reduce the number of negative appendectomies in pediatric patients with a high probability of acute appendicitis. Sci. Rep. 2024, 14, 12772. [Google Scholar] [CrossRef]
- AbdullGaffar, B. Diverticulosis and Diverticulitis of the Appendix. Int. J. Surg. Pathol. 2009, 17, 231–237. [Google Scholar] [CrossRef]
- Kelynack, T.N. A Contribution to the Pathology of the Vermiform Appendix; Lewis: London, UK, 1893. [Google Scholar]
- Pogorelić, Z.; Mihanović, J.; Ninčević, S.; Lukšić, B.; Elezović Baloević, S.; Polašek, O. Validity of Appendicitis Inflammatory Response Score in Distinguishing Perforated from Non-Perforated Appendicitis in Children. Children 2021, 8, 309. [Google Scholar] [CrossRef]
- Dupre, M.P.; Jadavji, I.; Matshes, E.; Urbanski, S.J. Diverticular Disease of the Vermiform Appendix: A Diagnostic Clue to Underlying Appendiceal Neoplasm. Hum. Pathol. 2008, 39, 1823–1826. [Google Scholar] [CrossRef]
- Williams, J.M.; Adamo, D.A.; Olson, M.C. Acute Appendiceal Diverticulitis: A Case Report. Radiol. Case Rep. 2021, 16, 1072–1074. [Google Scholar] [CrossRef]
- Altieri, M.L.; Piozzi, G.N.; Salvatori, P.; Mirra, M.; Piccolo, G.; Olivari, N. Appendiceal Diverticulitis, a Rare Relevant Pathology: Presentation of a Case Report and Review of the Literature. Int. J. Surg. Case Rep. 2017, 33, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Zubieta-O’Farrill, G.; Guerra-Mora, J.R.; Gudiño-Chávez, A.; Gonzalez-Alvarado, C.; Cornejo-López, G.B.; Villanueva-Sáenz, E. Appendiceal Diverticulum Associated with Chronic Appendicitis. Int. J. Surg. Case Rep. 2014, 5, 961–963. [Google Scholar] [CrossRef] [PubMed]
- Fiordaliso, M.; De Marco, A.F.; Costantini, R. A Case of Type 2 Appendiceal Diverticulum Perforated and a Review of the Literature. Int. J. Surg. Case Rep. 2020, 77, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Phillips, B.J.; Perry, C.W. Appendiceal Diverticulitis. Mayo Clin. Proc. 1999, 74, 890–892. [Google Scholar] [CrossRef]
- Abdelrahim, A.; Yusuf, Y.; Ali, O.; Abudeeb, H. Acute Diverticulitis of the Appendix. BMJ Case Rep. 2024, 17, e259552. [Google Scholar] [CrossRef]
- Cadena, M.; López, R.; Cardoso, L.; García, D.; Cabrera-Vargas, L.F.; Velásquez-Candamil, D.; Lozada Martinez, I.D. Acute Diverticulitis of the Appendix: A Case Report. Ann. Mediterr. Surg. 2023, 6, 17–22. [Google Scholar] [CrossRef]
- Laamiri, G.; Ezzine, R.; Feriani, N.; Rchidi, J.; Debbiche, A.; Hedfi, M. Appendiceal Diverticulitis: A Case Report. Clin. Case Rep. Int. 2023, 7, 1586. [Google Scholar]
- Bonomo, L.D.; Zago, M.; Quirico, C.; Ottinetti, A.; Panzera, F.; Galli, A.; Gattoni, L.; Canova, G.; Nicotera, A. Surgical Rarities: Case Report of Appendicular Diverticulitis and Literature Review. J. Surg. Case Rep. 2022, 2022, rjac319. [Google Scholar] [CrossRef]
- Ergenç, M.; Uprak, T.K. Appendiceal Diverticulitis Presenting as Acute Appendicitis and Diagnosed After Appendectomy. Cureus 2022, 14, e23050. [Google Scholar] [CrossRef]
- Elkhawaga, M.; Mundasad, B.; Hampton, J.; Alam, A.S. Appendiceal Diverticulitis Presenting as Acute Appendicitis: A Case Report. Cureus 2022, 14, e32626. [Google Scholar] [CrossRef]
- Abdulmomen, A.A.; AlZahrani, A.S.; Al Mulla, L.A.; Alaqeel, F.O. Acute Perforated Appendicitis Associated with Appendiceal Diverticulitis in a Young Man: A Case Report with Literature Review. Am. J. Case Rep. 2021, 23, e934838-1. [Google Scholar] [CrossRef] [PubMed]
- Onafowokan, O.O.; Khairat, A.; Bonatti, H.J.R. Appendiceal Diverticulitis in a Young Female Diagnosed on Pathology after Laparoscopic Appendectomy for Acute Appendicitis. Case Rep. Med. 2021, 2021, 2508956. [Google Scholar] [CrossRef] [PubMed]
- Bujold-Pitre, K.; Mailloux, O. Diverticulitis of the Appendix—Case Report and Literature Review. J. Surg. Case Rep. 2021, 2021, rjab488. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.; Stoeckle, D.B. Incidental Finding of Diverticulosis of the Appendix with Sessile Serrated Adenoma. Cureus 2020, 12, e8230. [Google Scholar] [CrossRef]
- Albeeshi, M.Z.; Alwanyan, A.A.; Salim, A.A.; Albabtain, I.T. Appendiceal Diverticulitis Presenting as Acute Appendicitis Diagnosed Postoperatively. J. Surg. Case Rep. 2019, 2019, rjz332. [Google Scholar] [CrossRef]
- Hwala, S.; Aoun, C.; El Hajj, I.; Malek, A.; Saber, T.; Farhat, S.; Asmar, A.E.; Saad, J.; Khoury, M.E. Appendiceal Diverticulitis Presenting with Clinical Features of Acute Appendicitis: Case Report and Literature Review. World J. Surg. Surg. Res. 2019, 2, 1137. [Google Scholar]
- Vass, T.; Zaránd, A.; Horányi, D.; Harsányi, L. A féregnyúlvány diverticulosisa, diverticulitise. Esetismertetés És Irod. Áttekintés. Orv. Hetil. 2018, 159, 768–772. [Google Scholar] [CrossRef]
- Singh-Ranger, D.; Mangalika, M. Appendix Diverticula—A Serious Diagnosis: Case Report and Literature Review. Clin. Surg. 2018, 3, 2270. [Google Scholar]
- Ogawa, Y.; Asayama, N.; Nagata, S. Acute Gastrointestinal Bleeding from Appendiceal Diverticulitis Diagnosed Preoperatively by Combined Short-interval Computed Tomography and Colonoscopy: A Case Report. Dig. Endosc. 2018, 30, 392–394. [Google Scholar] [CrossRef]
- Lourenço, R.B.; Pinho, M.D.C.; Schraibman, V.; Macedo, A.L.D.V.; Francisco Neto, M.J.; Funari, M.B.D.G. Perforated Diverticulitis of the Appendix: Ultrasonographic Diagnosis. Einstein São Paulo 2011, 9, 75–77. [Google Scholar] [CrossRef]
- Fernández Gómez-Cruzado, L.; Prieto Calvo, M.; Pérez González, C.; Larrea Oleaga, J. Diverticulitis of the Appendix as Debut of Appendicular Cystadenoma and Carcinoid Tumor. Rev. Esp. Enferm. Dig. 2017, 109, 145–146. [Google Scholar] [PubMed]
- El-Saady, A. Diverticulitis of the Appendix: Is It Clinically Significant? Egypt. J. Surg. 2016, 35, 150. [Google Scholar] [CrossRef]
- Lange, J.; Bachmann, R.; Königsrainer, A.; Zdichavsky, M. Appendiceal Diverticulitis Shortly after a Performed Laparoscopic Sigma Resection. J. Surg. Case Rep. 2015, 2015, rjv086. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, M.; Chawla, A.; Chokkappan, K.; Liu, H. Diverticulitis of the Appendix, a Distinctive Entity: Preoperative Diagnosis by Computed Tomography. Emerg. Radiol. 2015, 22, 609–612. [Google Scholar] [CrossRef]
- Yardimci, A.H.; Bektas, C.T.; Pasaoglu, E.; Kinaci, E.; Ozer, C.; Sevinc, M.M.; Mahmutoglu, A.S.; Kilickesmez, O. Retrospective Study of 24 Cases of Acute Appendiceal Diverticulitis: CT Findings and Pathological Correlations. Jpn. J. Radiol. 2017, 35, 225–232. [Google Scholar] [CrossRef]
- Patil, A.Y.; Levine, M.S.; Grujic, E.; Goren, R.A. Clinical and CT Findings in Appendiceal Diverticulitis. Clin. Imaging 2014, 38, 350–352. [Google Scholar] [CrossRef]
- Sohn, T.J.; Chang, Y.S.; Kang, J.H.; Kim, D.H.; Lee, T.S.; Han, J.K.; Kim, S.H.; Hong, Y.O. Clinical Characteristics of Acute Appendiceal Diverticulitis. J. Korean Surg. Soc. 2013, 84, 33. [Google Scholar] [CrossRef]
- Heffernan, D.S.; Saqib, N.; Terry, M. A Case of Appendiceal Diverticulitis, and a Review of the Literature. Ir. J. Med. Sci. 2009, 178, 519–521. [Google Scholar] [CrossRef]
- Yamana, I.; Kawamoto, S.; Inada, K.; Nagao, S.; Yoshida, T.; Yamashita, Y. Clinical Characteristics of 12 Cases of Appendiceal Diverticulitis: A Comparison with 378 Cases of Acute Appendicitis. Surg. Today 2012, 42, 363–367. [Google Scholar] [CrossRef]
- Käser, S.A.; Willi, N.; Maurer, C.A. Prevalence and Clinical Implications of Diverticulosis of the Vermiform Appendix. J. Int. Med. Res. 2013, 41, 1350–1356. [Google Scholar] [CrossRef]
- Kubota, T. Sonographic Findings of Acute Appendiceal Diverticulitis. World J. Gastroenterol. 2006, 12, 4104. [Google Scholar] [CrossRef] [PubMed]
- Lanthaler, M.; Nehoda, H. It Is Not Always Appendicitis. Wien. Klin. Wochenschr. 2004, 116, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Iki, K.; Echigo, M.; Nogami, A.; Iwamoto, S.; Takeo, T.; Tsunoda, T.; Eto, T. Preoperative Diagnosis of Acute Appendiceal Diverticulitis by Ultrasonography. Surgery 2001, 130, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Lipton, S.; Estrin, J.; Glasser, I. Diverticular Disease of the Appendix. Surg. Gynecol. Obstet. 1989, 168, 13–16. [Google Scholar]
- Osada, H.; Ohno, H.; Saiga, K.; Watanabe, W.; Okada, T.; Honda, N. Appendiceal Diverticulitis: Multidetector CT Features. Jpn. J. Radiol. 2012, 30, 242–248. [Google Scholar] [CrossRef]
- Lee, K.H.; Lee, H.S.; Park, S.H.; Bajpai, V.; Choi, Y.S.; Kang, S.-B.; Kim, K.J.; Kim, Y.H. Appendiceal Diverticulitis: Diagnosis and Differentiation From Usual Acute Appendicitis Using Computed Tomography. J. Comput. Assist. Tomogr. 2007, 31, 763–769. [Google Scholar] [CrossRef]
- Motos Micó, J.; Ferrer Márquez, M.; Berenguel Ibáñez, M.D.M.; Belda Lozano, R.; Moreno Serrano, A. Appendiceal Diverticulitis: A Possible Diagnosis in Acute Abdomen. Cirugía Esp. Engl. Ed. 2015, 93, e49–e51. [Google Scholar] [CrossRef]
- Nitta, N.; Takahashi, M.; Furukawa, A.; Murata, K.; Mori, M.; Fukushima, M. MR Imaging of the Normal Appendix and Acute Appendicitis. J. Magn. Reson. Imaging 2005, 21, 156–165. [Google Scholar] [CrossRef]
- Jaboury, I.A. Diverticulitis of the vermiform appendix. ANZ J. Surg. 2007, 77, 803–804. [Google Scholar] [CrossRef]
- Simpson, J.; Lobo, D.N.; Spiller, R.C.; Scholefield, J.H. Diverticular Abscess of the Appendix: Report of a Case and Review of the Literature. Dis. Colon Rectum 2003, 46, 832–834. [Google Scholar] [CrossRef]
- Pai, R.K.; Beck, A.H.; Norton, J.A.; Longacre, T.A. Appendiceal Mucinous Neoplasms: Clinicopathologic Study of 116 Cases With Analysis of Factors Predicting Recurrence. Am. J. Surg. Pathol. 2009, 33, 1425–1439. [Google Scholar] [CrossRef] [PubMed]
- Yantiss, R.K.; Shia, J.; Klimstra, D.S.; Hahn, H.P.; Odze, R.D.; Misdraji, J. Prognostic Significance of Localized Extra-Appendiceal Mucin Deposition in Appendiceal Mucinous Neoplasms. Am. J. Surg. Pathol. 2009, 33, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Lamps, L.W.; Gray, G.F.; Dilday, B.R.; Washington, M.K. The Coexistence of Low-Grade Mucinous Neoplasms of the Appendix and Appendiceal Diverticula: A Possible Role in the Pathogenesis of Pseudomyxoma Peritonei. Mod. Pathol. 2000, 13, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Stockl, T.; Ross, J.S.; Walter, O.; Dresser, K.; Lee, H. Appendiceal Mucosal Schwann Cell Proliferation: A Putative Histologic Marker of Appendiceal Diverticular Disease. Int. J. Surg. Pathol. 2013, 21, 603–609. [Google Scholar] [CrossRef]
- Marcacuzco, A.A.; Manrique, A.; Calvo, J.; Loinaz, C.; Justo, I.; Caso, O.; Cambra, F.; Fakih, N.; Sanabria, R.; Jimenez-Romero, L.C. Clinical Implications of Diverticular Disease of the Appendix. Experience Over the Past 10 Years. Cirugía Esp. Engl. Ed. 2016, 94, 44–47. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Ercegović, V.; Bašković, M.; Jukić, M.; Karaman, I.; Mrklić, I. Incidence and Management of Appendiceal Neuroendocrine Tumors in Pediatric Population: A Bicentric Experience with 6285 Appendectomies. Children 2023, 10, 1899. [Google Scholar] [CrossRef]
- Tintor, G.; Jukić, M.; Šupe-Domić, D.; Jerončić, A.; Pogorelić, Z. Diagnostic Accuracy of Leucine-Rich α-2-Glycoprotein 1 as a Non-Invasive Salivary Biomarker in Pediatric Appendicitis. Int. J. Mol. Sci. 2023, 24, 6043. [Google Scholar] [CrossRef]

| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Study design | Case report and retrospective study (case series or case-control study) | Conference abstracts, editorials, commentaries, and personal communications |
| Study period | All available literature to date | / |
| Language | English | Languages that are not English |
| Population | Human participants of all age groups | Animal studies |
| Study topic | Appendiceal diverticulitis with/without the clinical presentation of acute appendicitis | Topics that are not associated with appendiceal diverticulitis with/without the clinical presentation of acute appendicitis |
| Type 1 | Primary acute diverticulitis, with or without acute peridiverticulitis |
| Type 2 | Acute diverticulitis secondary to acute appendicitis |
| Type 3 | Diverticulum without inflammation |
| Type 4 | Diverticulum with acute appendicitis |
| Type 5 | Chronic peridiverticulitis with acute appendicitis |
| Author (Study Period, Country), Study Design | Sample Size (Male/Female) | Age | Symptoms | Physical Examination and Laboratory Findings | Method of Diagnosis | Associated Neoplasms |
|---|---|---|---|---|---|---|
| Abdelrahim et al. (2024, United Kingdom), case report [16] | 1 (1/0) | 50 | Right iliac fossa abdominal pain | NA | Computer tomography (CT) | No neoplasm |
| Cadena et al. (2023, Colombia), case report [17] | 1 (1/0) | 42 | 3-day history of right inferior quadrant pain, fever, and hyporexia | A white-blood-cell count of 13.6 × 109/L | Histopathology | No neoplasm |
| Laamiri et al. (2023, Tunisia), case report [18] | 1 (1/0) | 59 | 1-day history of right iliac fossa pain, nausea, and vomiting | A mean white-blood-cell count of 13 × 109/L and elevated CRP levels (CRP = 55 mg/dL) | Histopathology | No neoplasm |
| Bonomo et al. (2022, Italy), case report [19] | 1 (1/0) | 22 | 1-day history of right iliac fossa pain without fever or vomiting | C-reactive protein (0.71 mg/dL) | Histopathology | No neoplasm |
| Ergenç, and Uprak (January 2016–January 2022, Turkey), retrospective study [20] | 10 (8/2) | 34.4 ± 17.2 | All patients had right lower quadrant abdominal pain | A mean white-blood-cell count (WBC) of 13.5 × 109/L (±5.02) and a mean neutrophil percentage of 70.6 (±7.82) (leukocytosis was observed in 7 patients and neutrophilia in 5 patients) | Histopathology (n = 10) | Sessile serrated adenoma (n = 1) and low-grade appendiceal mucinous neoplasm (n = 1) |
| Elkhawaga et al. (2022, Austria), case report [21] | 1 (1/0) | 71 | 1-day history of right iliac fossa pain | Right iliac fossa tenderness and rebound tenderness | Histopathology | NA |
| Abdulmomen et al. (2021, Saudi Arabia), case report [22] | 1 (1/0) | 35 | 1-day history of right lower quadrant abdominal pain that radiated to the left lower quadrant | Leukocytosis (11 × 109/L) and CT scan revealed acute perforated appendicitis with early mass formation | Histopathology | NA |
| Wiliams et al. (2021, USA), case report [11] | 1 (1/0) | 85 | Right lower quadrant abdominal pain | Mildly protuberant abdomen without significant guarding or rebound | CT | NA |
| Onafowokan et al. (2021, USA), case report [23] | 1 (0/1) | 23 | Acute onset of severe right lower quadrant abdominal pain, nausea | Tenderness in the right lower quadrant and a positive Murphy’s sign | Histopathology | NA |
| Bujold-Pitre et al. (2021, Canada), case report [24] | 1 (1/0) | 72 | 2-day history of abdominal pain (left upper quadrant) | Leukocytosis (13.0 × 109/L) | Histopathology | No neoplasm |
| Fiordaliso et al. (2020, Italy), case report [14] | 1 (1/0) | 68 | 5-day history abdominal pain. The pain was progressive in severity and was associated with constipation and fever. | Bilateral lower quadrant tenderness, leukocytosis (14 × 109/L), and fever (38 °C) | Histopathology | NA |
| Memon et al. (2020, USA), case report [25] | 1 (0/1) | 52 | 1-day history of generalized abdominal pain, vomiting (once) | Mild diffuse tenderness to palpation with most pronounced pain in the right upper quadrant | Histopathology | Sessile serrated adenoma |
| Albeeshi et al. (2019, Saudi Arabia), case report [26] | 1 (0/1) | 28 | 2-day history of periumbilical pain, shifting to the right lower quadrant, associated with nausea and anorexia. No fever. | Tenderness at the right lower quadrant with positive rebound tenderness | Histopathology | NA |
| Hwala et al. (2019, Lebanon), case report [27] | 1 (1/0) | 44 | 2-day history of periumbilical pain (intermittent, without radiation), without nausea, vomiting or fever | Positive McBurney’s sign, leukocytosis (11.4 × 109/L), neutrophils of 85.2%, and lymphocytes of 9% | Histopathology | NA |
| Vass et al. (2018, China), case report [28] | 1 (0/1) | 65 | 2-day history of intermittent pain in the right iliac fossa | NA | Histopathology | NA |
| Singh-Ranger and Mangalika (2018, United Kingdom), case report [29] | 1 (1/0) | 54 | 3-day history of cramping peri-umbilical abdominal pain that radiated to the right iliac fossa, nausea | Guarding and rebound in the right iliac fossa, leukocyte count (12 × 109/L, neutrophil count (10 × 109/L), and CRP (325 mg/dL) | Histopathology | NA |
| Ogawa et al. (2018, Japan), case report [30] | 1 (1/0) | 63 | Hematochezia 3 h prior to admission | Rectal examination showed bloody stools, colonoscopy showed continuous bleeding from the orifice of the appendix | Histopathology | NA |
| Altieri et al. (2017, Italy), case report [12] | 1 (1/0) | 40 | Right lower quadrant pain, vomiting, and fever | Abdominal tenderness and leukocytosis (11.93 × 109/L) | Histopathology | NA |
| Constantin et al. (2017, Romania), case report [1] | 1 (0/1) | 50 | Right lower quadrant abdominal pain (intermittent) | Guarding in the right iliac fossa and a positive psoas sign | Intra-operative | No neoplasm |
| Lourenço et al. (2011, Brazil), case report [31] | 1 (1/0) | 61 | Constipation and tenderness in the lower right abdominal quadrant | Fever (38.4 °C) and leukocytosis (15.7 × 109/L) | Histopathology | No neoplasm |
| Fernández Gómez-Cruzado et al. (2017, Spain), case report [32] | 1 (1/0) | 61 | 4-day history of lower quadrant pain | Leukocytosis (9.7 × 109/L) and elevated CRP levels (CRP = 1.57 mg/dL) | CT | Carcinoid tumor |
| El-Saady (2016, Egypt), case report [33] | 1 (1/0) | 32 | 2-day history of diffuse periumbilical pain that shifted to the right iliac fossa and suprapubic areas within 6 h from onset, vomiting (once), constipation, and fever | Tender Mc-Burney point with rebound tenderness in the right iliac fossa, fever (38.1 °C), and leukocytosis (9 × 109/L) | Histopathology | NA |
| Lange et al. (2015, Germany), case report [34] | 1 (1/0) | 52 | 4-day history of the right lower quadrant pain | CRP was slightly elevated (3.5 mg/dL) | Histopathology | No neoplasm |
| Subramanian et al. (2015, Singapore), case report [35] | 1 (1/0) | 50 | 7-day history of intermittent moderate pain in the right lower quadrant | Mild localized tenderness in the right lower quadrant | CT | NA |
| Yardimci et al. (January 2010–July 2015, Japan), retrospective study [36] | 24 (17/7) | 42.0 ± 11.4 | NA | NA | Histopathology (n = 24) | None of the patients had an associated neoplasm |
| Zubieta- O’Farrill et al. (2014, Mexico), case report [13] | 1 (0/1) | 73 | Right lower quadrant pain lasting three days, occurring five times over a four-month period prior to admission | Complete blood work was within normal range | Histopathology | No neoplasm |
| Patil et al. (2014, USA), case report [37] | 1 (0/1) | 61 | Intermittent abdominal pain in the right lower quadrant, nausea, and anorexia | Afebrile and had a normal white-blood-cell count | CT | No neoplasm |
| Sohn et al. (January 2009–May 2011, South Korea), retrospective study [38] | 38 (19/19) | 49.0 ± 15.2 | Right lower quadrant abdominal pain (n = 34, 89.5%), fever (n = 12, 31.5%), nausea (n = 18, 47.4%), vomiting (n = 8, 21.1%), and diarrhea (n = 4, 10.5%) | Tenderness, rebound tenderness, and muscle guarding were found (n = 16, 42.1%) | Histopathology (n = 38) | NA |
| Heffernan et al. (2009, USA) [39] | 1 (0/1) | 46 | 10-day history of right sided abdominal pain | Right lower quadrant tenderness, fever (38.7 °C), and leukocytosis (16 × 109/L) | Histopathology | No neoplasm |
| Yamana et al. (January 2005–June 2008, Japan), retrospective study [40] | 12 (10/2) | 42.7 ± 15.4 | NA | The mean leukocyte count at the time of the admission was 11,332 ± 4658 µ/L (8 patients had leukocytosis), the mean CRP level was 8.7 ± 8.9 mg/dL (6 patients had elevated CRP levels), and perforation was observed in 4 patients | Histopathology (n = 12) | None of the patients had an associated neoplasm |
| Käser et al. (June 1998–June 2008, Switzerland), retrospective study [41] | 9 (NA) | 33.3 ± 18.3 | NA | 4 patients had leukocytosis and 8 patients had elevated CRP levels | Histopathology (n = 9) | Neuroendocrine carcinoid (n = 2) |
| Kubota et al. (2006, Japan) [42] | 1 (0/1) | 30 | 4-day history of abdominal pain in right lower quadrant, fever, and mild anorexia | Localized tenderness in the right lower quadrant of abdomen, fever (37.4 °C), and leukocytosis (count of 11.0 × 109/L) | Abdominal ultrasound sonography | No neoplasm |
| Lanthaler et al. (2004, Austria), case report [43] | 1 (1/0) | 39 | 10-day history of right lower-quadrant abdominal pain | Abdominal examination revealed right lower-quadrant pain with localized guarding, leukocytosis (18,000 g/dL), and elevated CRP levels (CRP = 8.9 mg/dL) | Histopathology | No neoplasm |
| Iki et al. (2001, Japan), case report [44] | 1 (1/0) | 84 | 4-day history of right lower quadrant abdominal pain and fever | Tenderness in the right lower quadrant region with peritoneal signs | Abdominal ultrasound sonography | NA |
| Symptoms | Characteristics | Onset |
|---|---|---|
| Abdominal pain in the right lower quadrant | Intermittent, insidious, and originates in right lower quadrant | 2–13 days |
| Fever | Often absent | Variable |
| Anorexia, nausea, and emesis | Temperature of 38.4 °C or more | Variable |
| Author (Study Period, Country), Study Design | Management | Intraoperative Complications | Postoperative Complications | Length of Hospital Stay (Days) | Mortality |
|---|---|---|---|---|---|
| Abdelrahim et al. (2024, United Kingdom), case report [16] | Laparoscopic appendectomy | None | None | NA | 0 |
| Cadena et al. (2023, Colombia), case report [17] | Laparoscopic appendectomy | None | None | 2 | 0 |
| Laamiri et al. (2023, Tunisia), case report [18] | Laparoscopic appendectomy | None | None | 2 | 0 |
| Bonomo et al. (2022, Italy), case report [19] | Laparoscopic appendectomy | None | None | 3 | 0 |
| Ergenç, and Uprak (January 2016–January 2022, Turkey), retrospective study [20] | Open appendectomy (n = 8), appendectomy-midline laparotomy (n = 1), and laparoscopic appendectomy (n = 1) | None | None | 2 (2–12) | 0 |
| Elkhawaga et al. (2022, Austria), case report [21] | Laparoscopic appendectomy | None | None | 2 | 0 |
| Abdulmomen et al. (2021, Saudi Arabia), case report [22] | Laparoscopic appendectomy | None | None | 4 | 0 |
| Wiliams et al. (2021, USA), case report [11] | Nonoperatively (watchful waiting) | NA | NA | NA | NA |
| Onafowokan et al. (2021, USA), case report [23] | Laparoscopic appendectomy | None | None | 2 | 0 |
| Bujold-Pitre et al. (2021, Canada), case report [24] | Laparoscopic right hemicolectomy | None | None | NA | 0 |
| Fiordaliso et al. (2020, Italy), case report [14] | Laparoscopic appendectomy | None | None | 6 | 0 |
| Memon et al. (2020, USA), case report [25] | Laparoscopic appendectomy | None | None | NA | 0 |
| Albeeshi et al. (2019, Saudi Arabia), case report [26] | Laparoscopic appendectomy | None | None | NA | 0 |
| Hwala et al. (2019, Lebanon), case report [27] | Laparoscopic appendectomy | None | None | NA | 0 |
| Vass et al. (2018, China), case report [28] | Laparoscopic appendectomy | None | None | NA | 0 |
| Singh-Ranger and Mangalika (2018, United Kingdom), case report [29] | Laparoscopic appendectomy | None | None | 4 | 0 |
| Ogawa et al. (2018, Japan), case report [30] | Laparoscopic appendectomy | None | None | 4 | 0 |
| Altieri et al. (2017, Italy), case report [12] | Appendectomy unspecified | None | None | 4 | 0 |
| Constantin et al. (2017, Romania), case report [1] | Open appendectomy | None | None | NA | 0 |
| Fernández Gómez-Cruzado et al. (2017, Spain), case report [32] | Open appendectomy | None | None | NA | 0 |
| El-Saady (2016, Egypt), case report [33] | Open appendectomy | None | None | NA | 0 |
| Lange et al. (2015, Germany), case report [34] | Laparoscopic appendectomy | None | None | 4 | 0 |
| Subramanian et al. (2015, Singapore), case report [35] | Laparoscopic appendectomy | None | None | 3 | 0 |
| Yardimci et al. (January 2010–July 2015, Japan), retrospective study [36] | NA | NA | NA | NA | NA |
| Zubieta-O’Farrill et al. (2014, Mexico), case report [13] | Laparoscopic appendectomy | None | None | 2 | 0 |
| Patil et al. (2014, USA), case report [37] | Laparoscopic appendectomy | None | None | 3 | 0 |
| Sohn et al. (January 2009–May 2011, South Korea), retrospective study [38] | Appendectomy, unspecified | NA | NA | 6.8 ± 3.4 | NA |
| Lourenço et al. (2011, Brazil), case report [31] | Open right hemicolectomy and appendectomy | None | None | NA | 0 |
| Heffernan et al. (2009, USA) [39] | Open appendectomy | None | None | NA | 0 |
| Yamana et al. (January 2005– June 2008, Japan), retrospective study [40] | Appendectomy, unspecified | NA | NA | 8.7 ± 4.86 | NA |
| Käser et al. (June 1998–June 2008, Switzerland), retrospective study [41] | Appendectomy, unspecified | NA | NA | NA | NA |
| Kubota et al. (2006, Japan) [42] | Appendectomy, unspecified | None | None | 3 | 0 |
| Lanthaler et al. (2004, Austria), case report [43] | Appendectomy, unspecified | None | None | 2 | 0 |
| Iki et al. (2001, Japan), case report [44] | Appendectomy, unspecified | None | None | NA | 0 |
| Feature | Appendiceal Diverticulitis | Acute Appendicitis |
|---|---|---|
| Onset of symptoms | Insidious, intermittent, 2–14 days | Sudden, progressive within 24–48 h |
| Age group | More common > 30 years | More common < 30 years |
| Pain localization | Initially diffuse, then localizing | Early periumbilical, then RLQ pain |
| Leukocytosis | Often > 15 × 109/L | Often < 15 × 109/L |
| CRP levels | Frequently elevated (>20 mg/L) | May be mildly elevated or normal |
| Perforation rate | 30–70% | 10–20% |
| Neoplasm association | Present in up to 20% of cases | Rare |
| Imaging findings (CT/US) | Appendiceal diverticula, wall thickening, peridiverticulitis | Enlarged, non-compressible appendix with periappendiceal fat stranding |
| AIR score | Might be lower compared to acute appendicitis AIR score | Might be higher compared to appendiceal diverticulitis AIR score |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vidović, S.; Čekić, N.; Šuvak, I.; Ugljarević, M.; Pogorelić, Z. Acute Appendicitis or Appendiceal Diverticulitis? A Case Report and Systematic Literature Review. Clin. Pract. 2025, 15, 60. https://doi.org/10.3390/clinpract15030060
Vidović S, Čekić N, Šuvak I, Ugljarević M, Pogorelić Z. Acute Appendicitis or Appendiceal Diverticulitis? A Case Report and Systematic Literature Review. Clinics and Practice. 2025; 15(3):60. https://doi.org/10.3390/clinpract15030060
Chicago/Turabian StyleVidović, Stipe, Nenad Čekić, Ivica Šuvak, Mladen Ugljarević, and Zenon Pogorelić. 2025. "Acute Appendicitis or Appendiceal Diverticulitis? A Case Report and Systematic Literature Review" Clinics and Practice 15, no. 3: 60. https://doi.org/10.3390/clinpract15030060
APA StyleVidović, S., Čekić, N., Šuvak, I., Ugljarević, M., & Pogorelić, Z. (2025). Acute Appendicitis or Appendiceal Diverticulitis? A Case Report and Systematic Literature Review. Clinics and Practice, 15(3), 60. https://doi.org/10.3390/clinpract15030060








