Understanding the Significance of Biochemistry in the Storage, Handling, Purification, and Sampling of Amphiphilic Mycolactone
Abstract
1. Introduction
2. Results
2.1. Purification of Natural Mycolactone Is Inconsistent
2.2. Mycolactone Forms Aggregates in Aqueous Solution
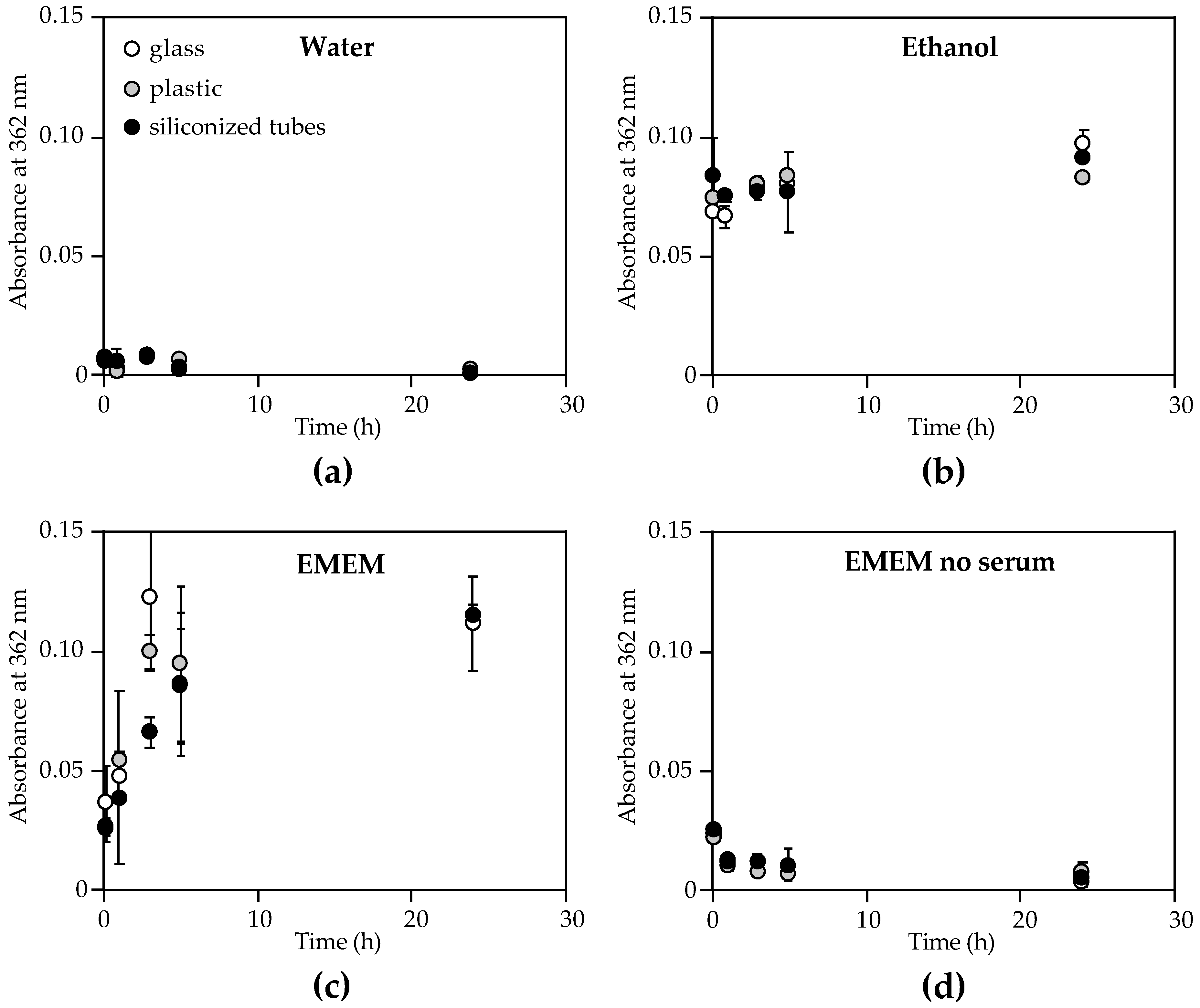
2.3. Storage Media, but not Container Material, Affect Mycolactone Measurement by UV-Vis
2.4. Mycolactone A/B Binds to Human High- and Low-Density Lipoproteins (HDL and LDL)
3. Discussion
4. Materials and Methods
4.1. Materials and Reagents
4.2. Natural Mycolactone Purification
4.3. Electron Spray Ionization Mass Spectrometry (MS)
4.4. Cytotoxicity Assays
4.5. Mycolactone Quantification by UV-Vis
4.6. Critical Micelle Concentration (CMC)
4.7. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gunawardana, G.; Chatterjee, D.; George, K.M.; Brennan, P.; Whittern, D.; Small, P.L.C. Characterization of Novel Macrolide Toxins, Mycolactones A and B, from a Human Pathogen, Mycobacterium ulcerans. J. Am. Chem. Soc. 1999, 121, 6092–6093. [Google Scholar] [CrossRef]
- George, K.M.; Chatterjee, D.; Gunawardana, G.; Welty, D.; Hayman, J.; Lee, R.; Small, P.L. Mycolactone: A polyketide toxin from Mycobacterium ulcerans required for virulence. Science 1999, 283, 854–857. [Google Scholar] [CrossRef] [PubMed]
- George, K.M.; Barker, L.P.; Welty, D.M.; Small, P.L. Partial purification and characterization of biological effects of a lipid toxin produced by Mycobacterium ulcerans. Infect. Immun. 1998, 66, 587–593. [Google Scholar]
- Adusumilli, S.; Mve-Obiang, A.; Sparer, T.; Meyers, W.; Hayman, J.; Small, P.L. Mycobacterium ulcerans toxic macrolide, mycolactone modulates the host immune response and cellular location of M. ulcerans in vitro and in vivo. Cell Microbiol. 2005, 7, 1295–1304. [Google Scholar] [CrossRef] [PubMed]
- Read, J.K.; Heggie, C.M.; Meyers, W.M.; Connor, D.H. Cytotoxic activity of Mycobacterium ulcerans. Infect. Immun. 1974, 9, 1114–1122. [Google Scholar]
- George, K.M.; Pascopella, L.; Welty, D.M.; Small, P.L. A Mycobacterium ulcerans toxin, mycolactone, causes apoptosis in guinea pig ulcers and tissue culture cells. Infect. Immun. 2000, 68, 877–883. [Google Scholar] [CrossRef]
- Pimsler, M.; Sponsler, T.A.; Meyers, W.M. Immunosuppressive properties of the soluble toxin from Mycobacterium ulcerans. J. Infect. Dis. 1988, 157, 577–580. [Google Scholar] [CrossRef]
- En, J.; Goto, M.; Nakanaga, K.; Higashi, M.; Ishii, N.; Saito, H.; Yonezawa, S.; Hamada, H.; Small, P.L. Mycolactone is responsible for the painlessness of Mycobacterium ulcerans infection (buruli ulcer) in a murine study. Infect. Immun. 2008, 76, 2002–2007. [Google Scholar] [CrossRef]
- Hong, H.; Coutanceau, E.; Leclerc, M.; Caleechurn, L.; Leadlay, P.F.; Demangel, C. Mycolactone diffuses from Mycobacterium ulcerans-infected tissues and targets mononuclear cells in peripheral blood and lymphoid organs. PLoS Negl. Trop. Dis. 2008, 2, e325. [Google Scholar] [CrossRef] [PubMed]
- Converse, P.J.; Xing, Y.; Kim, K.H.; Tyagi, S.; Li, S.Y.; Almeida, D.V.; Nuermberger, E.L.; Grosset, J.H.; Kishi, Y. Accelerated detection of mycolactone production and response to antibiotic treatment in a mouse model of Mycobacterium ulcerans disease. PLoS Negl. Trop. Dis. 2014, 8, e2618. [Google Scholar] [CrossRef]
- Marion, E.; Jarry, U.; Cano, C.; Savary, C.; Beauvillain, C.; Robbe-Saule, M.; Preisser, L.; Altare, F.; Delneste, Y.; Jeannin, P.; et al. FVB/N Mice Spontaneously Heal Ulcerative Lesions Induced by Mycobacterium ulcerans and Switch M. ulcerans into a Low Mycolactone Producer. J. Immunol. 2016, 196, 2690–2698. [Google Scholar] [CrossRef]
- Sarfo, F.S.; Phillips, R.O.; Rangers, B.; Mahrous, E.A.; Lee, R.E.; Tarelli, E.; Asiedu, K.B.; Small, P.L.; Wansbrough-Jones, M.H. Detection of Mycolactone A/B in Mycobacterium ulcerans-Infected Human Tissue. PLoS Negl. Trop. Dis. 2010, 4, e577. [Google Scholar] [CrossRef]
- Sarfo, F.S.; Le Chevalier, F.; Aka, N.; Phillips, R.O.; Amoako, Y.; Boneca, I.G.; Lenormand, P.; Dosso, M.; Wansbrough-Jones, M.; Veyron-Churlet, R.; et al. Mycolactone diffuses into the peripheral blood of Buruli ulcer patients—Implications for diagnosis and disease monitoring. PLoS Negl. Trop. Dis. 2011, 5, e1237. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Phillips, R.O.; Zhang, J.; Abass, M.K.; Abotsi, J.; Amoako, Y.A.; Adu-Sarkodie, Y.; Robinson, C.; Wansbrough-Jones, M.H. Kinetics of mycolactone in human subcutaneous tissue during antibiotic therapy for Mycobacterium ulcerans disease. BMC Infect. Dis. 2014, 14, 202. [Google Scholar] [CrossRef]
- Fidanze, S.; Song, F.; Szlosek-Pinaud, M.; Small, P.L.; Kishi, Y. Complete structure of the mycolactones. J. Am. Chem. Soc. 2001, 123, 10117–10118. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.; Demangel, C.; Pidot, S.J.; Leadlay, P.F.; Stinear, T. Mycolactones: Immunosuppressive and cytotoxic polyketides produced by aquatic mycobacteria. Nat. Prod. Rep. 2008, 25, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Kishi, Y. Chemistry of mycolactones, the causative toxins of Buruli ulcer. Proc. Natl. Acad. Sci. USA 2011, 108, 6703–6708. [Google Scholar] [CrossRef]
- Gehringer, M.; Altmann, K.H. The chemistry and biology of mycolactones. Beilstein J. Org. Chem. 2017, 13, 1596–1660. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Phillips, R.; Wansbrough-Jones, M.; Simmonds, R.E. Recent advances: Role of mycolactone in the pathogenesis and monitoring of Mycobacterium ulcerans infection/Buruli ulcer disease. Cell. Microbiol. 2016, 18, 17–29. [Google Scholar] [CrossRef]
- Snyder, D.S.; Small, P.L. Uptake and cellular actions of mycolactone, a virulence determinant for Mycobacterium ulcerans. Microb. Pathog. 2003, 34, 91–101. [Google Scholar] [CrossRef]
- Chany, A.C.; Casarotto, V.; Schmitt, M.; Tarnus, C.; Guenin-Mace, L.; Demangel, C.; Mirguet, O.; Eustache, J.; Blanchard, N. A diverted total synthesis of mycolactone analogues: An insight into Buruli ulcer toxins. Chemistry 2011, 17, 14413–14419. [Google Scholar] [CrossRef] [PubMed]
- Gersbach, P.; Jantsch, A.; Feyen, F.; Scherr, N.; Dangy, J.P.; Pluschke, G.; Altmann, K.H. A ring-closing metathesis (RCM)-based approach to mycolactones A/B. Chemistry 2011, 17, 13017–13031. [Google Scholar] [CrossRef] [PubMed]
- Scherr, N.; Gersbach, P.; Dangy, J.P.; Bomio, C.; Li, J.; Altmann, K.H.; Pluschke, G. Structure-activity relationship studies on the macrolide exotoxin mycolactone of Mycobacterium ulcerans. PLoS Negl. Trop. Dis. 2013, 7, e2143. [Google Scholar] [CrossRef] [PubMed]
- Chany, A.C.; Veyron-Churlet, R.; Tresse, C.; Mayau, V.; Casarotto, V.; Le Chevalier, F.; Guenin-Mace, L.; Demangel, C.; Blanchard, N. Synthetic variants of mycolactone bind and activate Wiskott-Aldrich syndrome proteins. J. Med. Chem. 2014, 57, 7382–7395. [Google Scholar] [CrossRef] [PubMed]
- Mve-Obiang, A.; Lee, R.E.; Portaels, F.; Small, P.L. Heterogeneity of mycolactones produced by clinical isolates of Mycobacterium ulcerans: Implications for virulence. Infect. Immun. 2003, 71, 774–783. [Google Scholar] [CrossRef]
- Guenin-Mace, L.; Veyron-Churlet, R.; Thoulouze, M.I.; Romet-Lemonne, G.; Hong, H.; Leadlay, P.F.; Danckaert, A.; Ruf, M.T.; Mostowy, S.; Zurzolo, C.; et al. Mycolactone activation of Wiskott-Aldrich syndrome proteins underpins Buruli ulcer formation. J. Clin. Investig. 2013, 123, 1501–1512. [Google Scholar] [CrossRef] [PubMed]
- Bieri, R.; Scherr, N.; Ruf, M.T.; Dangy, J.P.; Gersbach, P.; Gehringer, M.; Altmann, K.H.; Pluschke, G. The Macrolide Toxin Mycolactone Promotes Bim-Dependent Apoptosis in Buruli Ulcer through Inhibition of mTOR. ACS Chem. Biol. 2017, 12, 1297–1307. [Google Scholar] [CrossRef] [PubMed]
- Converse, P.J.; Almeida, D.V.; Nuermberger, E.L.; Grosset, J.H. BCG-mediated protection against Mycobacterium ulcerans infection in the mouse. PLoS Negl. Trop. Dis. 2011, 5, e985. [Google Scholar] [CrossRef]
- Spangenberg, T.; Kishi, Y. Highly sensitive, operationally simple, cost/time effective detection of the mycolactones from the human pathogen Mycobacterium ulcerans. Chem. Commun. 2010, 46, 1410–1412. [Google Scholar] [CrossRef]
- Wadagni, A.; Frimpong, M.; Phanzu, D.M.; Ablordey, A.; Kacou, E.; Gbedevi, M.; Marion, E.; Xing, Y.; Babu, V.S.; Phillips, R.O.; et al. Simple, Rapid Mycobacterium ulcerans Disease Diagnosis from Clinical Samples by Fluorescence of Mycolactone on Thin Layer Chromatography. PLoS. Negl. Trop. Dis. 2015, 9, e0004247. [Google Scholar] [CrossRef]
- Song, F.; Fidanze, S.; Benowitz, A.B.; Kishi, Y. Total synthesis of the mycolactones. Org. Lett. 2002, 4, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Song, F.; Fidanze, S.; Benowitz, A.B.; Kishi, Y. Total Synthesis of Mycolactones A and B. Tetrahedron 2007, 63, 5739–5753. [Google Scholar] [CrossRef] [PubMed]
- Saint-Auret, S.; Chany, A.C.; Casarotto, V.; Tresse, C.; Parmentier, L.; Abdelkafi, H.; Blanchard, N. Total Syntheses of Mycolactone A/B and its Analogues for the Exploration of the Biology of Buruli Ulcer. Chim. (Aarau) 2017, 71, 836–840. [Google Scholar] [CrossRef]
- Kubicek-Sutherland, J.Z.; Vu, D.M.; Mendez, H.M.; Jakhar, S.; Mukundan, H. Detection of Lipid and Amphiphilic Biomarkers for Disease Diagnostics. Biosensors (Basel) 2017, 7, 25. [Google Scholar] [CrossRef] [PubMed]
- Sakamuri, R.M.; Price, D.N.; Lee, M.; Cho, S.N.; Barry, C.E., 3rd; Via, L.E.; Swanson, B.I.; Mukundan, H. Association of lipoarabinomannan with high density lipoprotein in blood: Implications for diagnostics. Tuberculosis (Edinb) 2013, 93, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Stromberg, L.R.; Mendez, H.M.; Kubicek-Sutherland, J.Z.; Graves, S.W.; Hengartner, N.W.; Mukundan, H. Presentation matters: Impact of association of amphiphilic LPS with serum carrier proteins on innate immune signaling. PLoS ONE 2018, 13, e0198531. [Google Scholar] [CrossRef]
- Vu, D.M.; Sakamuri, R.M.; Waters, W.R.; Swanson, B.I.; Mukundan, H. Detection of Lipomannan in Cattle Infected with Bovine Tuberculosis. Anal. Sci. 2017, 33, 457–460. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.A.; Unkefer, C.J.; Swanson, B.I.; Swanson, J.M.J.; Gnanakaran, S. Membrane perturbing properties of toxin mycolactone from Mycobacterium ulcerans. PLoS Comput. Biol. 2018, 14, e1005972. [Google Scholar] [CrossRef] [PubMed]
- Nitenberg, M.; Benarouche, A.; Maniti, O.; Marion, E.; Marsollier, L.; Gean, J.; Dufourc, E.J.; Cavalier, J.F.; Canaan, S.; Girard-Egrot, A.P. The potent effect of mycolactone on lipid membranes. PLoS Pathog. 2018, 14, e1006814. [Google Scholar] [CrossRef]
- Marion, E.; Prado, S.; Cano, C.; Babonneau, J.; Ghamrawi, S.; Marsollier, L. Photodegradation of the Mycobacterium ulcerans toxin, mycolactones: Considerations for handling and storage. PLoS ONE 2012, 7, e33600. [Google Scholar] [CrossRef]
- Xing, Y.; Hande, S.M.; Kishi, Y. Photochemistry of mycolactone A/B, the causative toxin of Buruli ulcer. J. Am. Chem. Soc. 2012, 134, 19234–19239. [Google Scholar] [CrossRef]
- Hong, H.; Gates, P.J.; Staunton, J.; Stinear, T.; Cole, S.T.; Leadlay, P.F.; Spencer, J.B. Identification using LC-MSn of co-metabolites in the biosynthesis of the polyketide toxin mycolactone by a clinical isolate of Mycobacterium ulcerans. Chem. Commun. 2003, 2822–2823. [Google Scholar] [CrossRef]
- Corrin, M.L.; Harkins, W.D. Determination of the critical concentration for micelle formation in solutions of colloidal electrolytes by the spectral change of a dye. J. Am. Chem. Soc. 1947, 69, 679–683. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Laboratory Diagnosis of Buruli Ulcer: A Manual for Health Care Providers Portaels; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Feingold, K.R.; Grunfeld, C. The role of HDL in innate immunity. J. Lipid Res. 2011, 52, 1–3. [Google Scholar] [CrossRef]
- Levine, D.M.; Parker, T.S.; Donnelly, T.M.; Walsh, A.; Rubin, A.L. In vivo protection against endotoxin by plasma high density lipoprotein. Proc. Natl. Acad. Sci. USA 1993, 90, 12040–12044. [Google Scholar] [CrossRef] [PubMed]
- Levels, J.H.; Abraham, P.R.; van Barreveld, E.P.; Meijers, J.C.; van Deventer, S.J. Distribution and kinetics of lipoprotein-bound lipoteichoic acid. Infect. Immun. 2003, 71, 3280–3284. [Google Scholar] [CrossRef]
- Morin, E.E.; Guo, L.; Schwendeman, A.; Li, X.A. HDL in sepsis—Risk factor and therapeutic approach. Front. Pharm. 2015, 6, 244. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health and the Friends of the National Library of Medicine. Cholesterol Levels: What You Need to Know; Medline Plus; National Library of Medicine at the National Institutes of Health: Bethesda, MD, USA, 2012; pp. 6–7.
- Pettit, J.H.; Marchette, N.J.; Rees, R.J. Mycobacterium ulcerans infection. Clinical and bacteriological study of the first cases recognized in South East Asia. Br. J. Derm. 1966, 78, 187–197. [Google Scholar] [CrossRef]
- Williamson, H.R.; Benbow, M.E.; Nguyen, K.D.; Beachboard, D.C.; Kimbirauskas, R.K.; McIntosh, M.D.; Quaye, C.; Ampadu, E.O.; Boakye, D.; Merritt, R.W.; et al. Distribution of Mycobacterium ulcerans in buruli ulcer endemic and non-endemic aquatic sites in Ghana. PLoS Negl. Trop. Dis. 2008, 2, e205. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, S.Y.; Converse, P.J.; Grosset, J.H.; Nuermberger, E.L. Rapid, serial, non-invasive assessment of drug efficacy in mice with autoluminescent Mycobacterium ulcerans infection. PLoS Negl. Trop. Dis. 2013, 7, e2598. [Google Scholar] [CrossRef]




| Sample | M. ulcerans Strain | Dry Weight of Bacteria (g) | Volume of Extract (µL) | TLC Band a | MS Peak b | Mycolactone Conc. (µg/mL) c |
|---|---|---|---|---|---|---|
| 1 | 1059AL | 0.218 | 150 | + | + | 53 |
| 2 | 1615 | 0.027 | 25 | – | n/a | n/a |
| 3 | 1059 | 0.110 | 100 | + | + | 17 |
| 4 | 1059AL | 0.250 | 150 | – | n/a | n/a |
| 5 | 1059AL | 0.244 | 235 | + | + | 8 |
| 6 | 1059AL | 0.102 | 150 | – | – | 6 |
| 7 | 1059AL | 0.153 | 150 | + | + | 10 |
| 8 | 1059AL | 0.132 | 150 | + | + | 19 |
| 9 | 1059AL | 0.211 | 200 | + | + | 9 |
| 10 | 1615 | 0.195 | 260 | – | + | 9 |
| 11 | 1059 | 0.130 | 90 | + | + | 42 |
| 12 d | 1059AL | n.d. | 375 | + | + | 11 |
| Mycolactone | CMC a | Fold-Change b |
|---|---|---|
| Synthetic | 30–60 µM | − |
| Biotinylated | 1–2 µM | 0.03 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubicek-Sutherland, J.Z.; Vu, D.M.; Anderson, A.S.; Sanchez, T.C.; Converse, P.J.; Martí-Arbona, R.; Nuermberger, E.L.; Swanson, B.I.; Mukundan, H. Understanding the Significance of Biochemistry in the Storage, Handling, Purification, and Sampling of Amphiphilic Mycolactone. Toxins 2019, 11, 202. https://doi.org/10.3390/toxins11040202
Kubicek-Sutherland JZ, Vu DM, Anderson AS, Sanchez TC, Converse PJ, Martí-Arbona R, Nuermberger EL, Swanson BI, Mukundan H. Understanding the Significance of Biochemistry in the Storage, Handling, Purification, and Sampling of Amphiphilic Mycolactone. Toxins. 2019; 11(4):202. https://doi.org/10.3390/toxins11040202
Chicago/Turabian StyleKubicek-Sutherland, Jessica Z., Dung M. Vu, Aaron S. Anderson, Timothy C. Sanchez, Paul J. Converse, Ricardo Martí-Arbona, Eric L. Nuermberger, Basil I. Swanson, and Harshini Mukundan. 2019. "Understanding the Significance of Biochemistry in the Storage, Handling, Purification, and Sampling of Amphiphilic Mycolactone" Toxins 11, no. 4: 202. https://doi.org/10.3390/toxins11040202
APA StyleKubicek-Sutherland, J. Z., Vu, D. M., Anderson, A. S., Sanchez, T. C., Converse, P. J., Martí-Arbona, R., Nuermberger, E. L., Swanson, B. I., & Mukundan, H. (2019). Understanding the Significance of Biochemistry in the Storage, Handling, Purification, and Sampling of Amphiphilic Mycolactone. Toxins, 11(4), 202. https://doi.org/10.3390/toxins11040202







