Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women
Abstract
:1. Introduction
2. Results
3. Discussion
4. Conclusions
5. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blaivas, J.G. Pathophysiology of lower urinary tract dysfunction. Urol. Clin. N. Am. 1985, 12, 215–224. [Google Scholar]
- Carson, C.C.; Segura, J.W.; Osborne, D.M. Evaluation and treatment of the female urethral syndrome. J. Urol. 1980, 124, 609–610. [Google Scholar] [CrossRef]
- Massey, J.A.; Abrams, P.H. Obstructed voiding in the female. Br. J. Urol. 1988, 61, 36–39. [Google Scholar] [CrossRef]
- Nitti, V.W.; Fiske, J. Cystometrogram versus cystometrogram plus voiding pressure-flow studies in women with lower urinary tract symptoms. J. Urol. 1999, 161, 201. [Google Scholar] [CrossRef]
- Groutz, A.; Blaivas, J.G.; Pies, C.; Sassone, A.M. Learned voiding dysfunction (non-neurogenic, neurogenic bladder) among adults. Neurourol. Urodyn. 2001, 20, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, S.M.; Lin, H.H.; Kuo, H.C. Videourodynamic Studies of Women with Voiding Dysfunction. Sci. Rep. 2017, 7, 6845. [Google Scholar] [CrossRef] [PubMed]
- Chuang, F.C.; Huang, K.H.; Kuo, H.C. Lower urinary tract symptoms and vdeo urodynamic characteristics of women with clinically unsuspected bladder outlet obstruction. Low Urin. Tract Symptoms 2013, 5, 23–27. [Google Scholar] [CrossRef]
- Chen, Y.C.; Kuo, H.C. Clinical and video urodynamic characteristics of adult women with dysfunctional voiding. J. Formosan Med. Assoc. 2014, 113, 161–165. [Google Scholar] [CrossRef] [Green Version]
- Haylen, B.T.; de Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol. Urodyn. 2010, 29, 4–20. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.D.; Bright, T.C., 3rd. Urodynamic patterns in children with dysfunctional voiding problems. J. Urol. 1978, 119, 247–249. [Google Scholar] [CrossRef]
- Minardi, D.; d’Anzeo, G.; Parri, G.; Polito, M., Jr.; Piergallina, M.; El Asmar, Z.; Marchetti, M.; Muzzonigro, G. The role of uroflowmetry biofeedback and biofeedback training of the pelvic floor muscles in the treatment of recurrent urinary tract infections in women with dysfunctional voiding: A randomized controlled prospective study. Urology 2010, 75, 1299–1304. [Google Scholar] [CrossRef] [PubMed]
- Espuña-Pons, M.; Cardozo, L.; Chapple, C.; Sievert, K.D.; van Kerrebroeck, P.; Kirby, M.G. Overactive bladder symptoms and voiding dysfunction in neurologically normal women. Neurourol. Urodyn. 2012, 31, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.W.; Wu, M.Y.; Yang, S.S.; Jaw, F.S.; Chang, S.J. Comparing the Efficacy of OnabotulinumtoxinA, Sacral Neuromodulation, and Peripheral Tibial Nerve Stimulation as Third Line Treatment for the Management of Overactive Bladder Symptoms in Adults: Systematic Review and Network Meta-Analysis. Toxins 2020, 12, 128. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.H.; Chen, S.F.; Jhang, J.F.; Kuo, H.C. Therapeutic effect of urethral sphincter onabotulinumtoxinA injection for urethral sphincter hyperactivity. Neurourol. Urodyn. 2018, 37, 2651–2657. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.L.; Huang, K.H.; Kuo, H.C.; Ou, Y.C. The Therapeutic Effects and Pathophysiology of Botulinum Toxin A on Voiding Dysfunction Due to Urethral Sphincter Dysfunction. Toxins 2019, 11, 728. [Google Scholar] [CrossRef] [Green Version]
- Kuo, H.C. Dysfunctional voiding in women with lower urinary tract symptoms. Tzu Chi Med. J. 2000, 12, 217–223. [Google Scholar]
- Kuo, H.C. Botulinum A toxin urethral injection for the treatment of lower urinary tract dysfunction. J. Urol. 2003, 170, 1908–1912. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, W.; Firlit, C.F.; Schoenberg, H.W. The female urethral syndrome: External sphincter spasm as etiology. J. Urol. 1980, 124, 48–49. [Google Scholar] [CrossRef]
- Deindl, F.M.; Vodusek, D.B.; Bischoff, C.H.; Hofmann, R.; Hartung, R. Dysfunctional voiding in women: Which muscles are responsible? Br. J. Urol. 1998, 82, 814–819. [Google Scholar] [CrossRef]
- Hinman, F., Jr. Nonneurogenic neurogenic bladder (the Hinmann syndrome)—15 years later. J. Urol. 1986, 136, 769–777. [Google Scholar] [CrossRef]
- De Paepe, H.; Renson, C.; Van Laecke, E.; Raes, A.; Vande Walle, J.; Hoebeke, P. Pelvic-floor therapy and toilet training in young children with dysfunctional voiding and obstipation. BJU Int. 2000, 85, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Lee, K.S.; Choo, M.S.; Kim, J.C.; Lee, J.G.; Seo, J.T.; Lee, J.Z.; Lee, J.Y.; Oh, S.J.; Na, Y.G. Efficacy of an Alpha-Blocker for the Treatment of Nonneurogenic Voiding Dysfunction in Women: An 8-Week, Randomized, Double-Blind, Placebo-Controlled Trial. Int. Neurourol. J. 2018, 22, 30–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGuire, E.J.; Savastano, J.A. Urodynamic studies in enuresis and the non-neurogenic neurogenic bladder. J. Urol. 1984, 132, 29–302. [Google Scholar] [CrossRef]
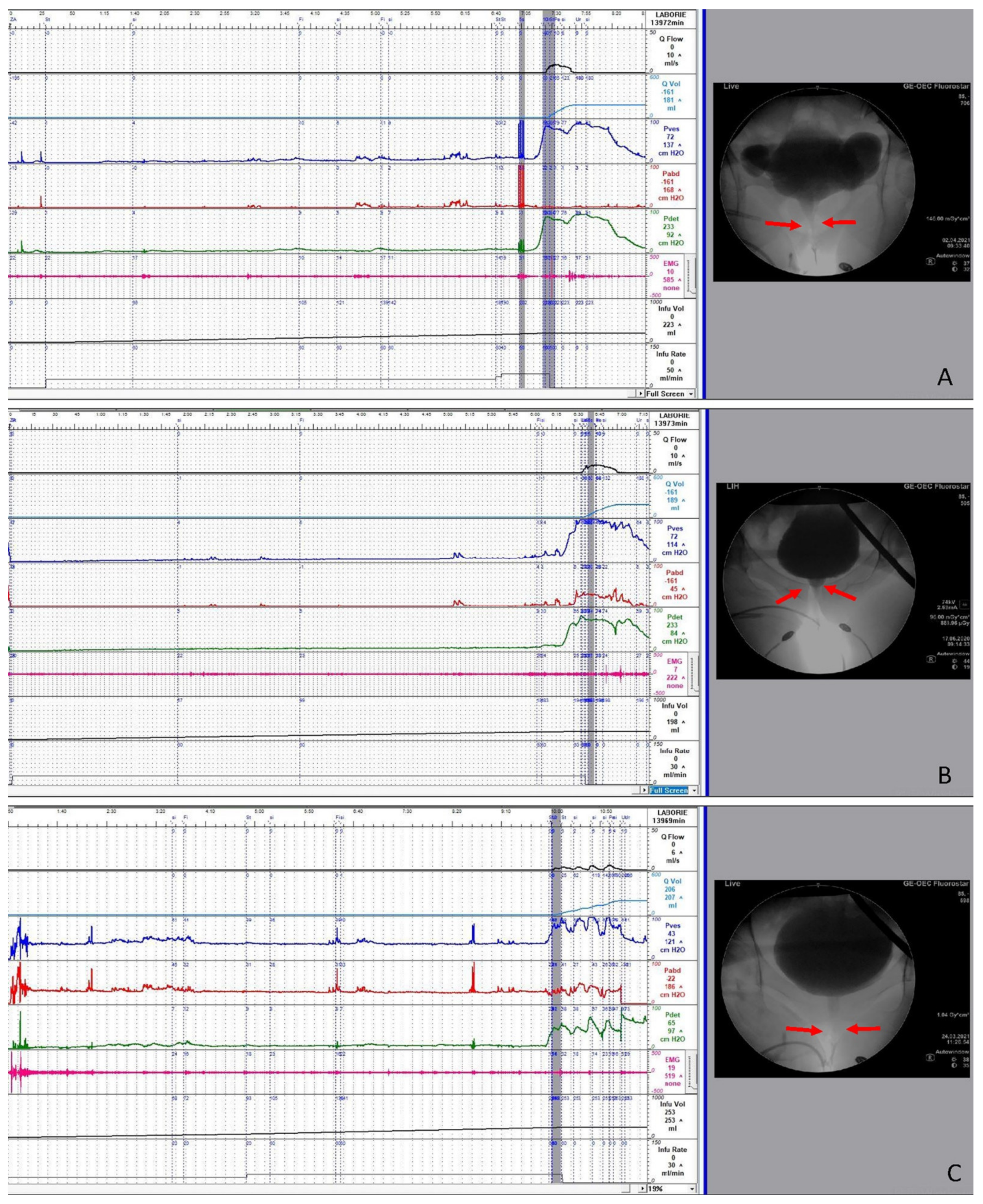
- Peng, C.H.; Chen, S.F.; Kuo, H.C. Videourodynamic analysis of the urethral sphincter overactivity and the poor relaxing pelvic floor muscles in women with voiding dysfunction. Neurourol. Urodyn. 2017, 36, 2169–2175. [Google Scholar] [CrossRef] [PubMed]
- Chow, P.M.; Hsiao, S.M.; Kuo, H.C. Obstructive patterns in videourodynamic studies predict responses of female dysfunctional voiding treated with or without urethral botulinum toxin injection: A long-term follow-up study. Int. Urogynecol. J. 2020, 31, 2557–2564. [Google Scholar] [CrossRef]
- Fam, B.A.; Sarkarati, M.; Yalla, S.V. Spinal cord injury. In Neurourology and Urodynamics; Yalla, S.V., McGuire, E.J., Elbadawi., A., Eds.; Macmillan Publishing Company: New York, NY, USA, 1988; pp. 291–302. [Google Scholar]
- Kuo, T.L.C.; Ng, L.G.; Chapple, C.R. Pelvic floor spasm as a cause of voiding dysfunction. Curr. Opin. Urol. 2015, 25, 311–316. [Google Scholar] [CrossRef]
| Parameter | Successful (n = 55) | Failure (n = 26) | p-Value |
|---|---|---|---|
| Age | 59.7 ± 13.9 | 60.4 ± 19.3 | 0.857 |
| FSF (mL) | 146.6 ± 70.6 | 115.0 ± 52.8 | 0.046 |
| FS (mL) | 216.2 ± 86.4 | 184.9 ± 68.3 | 0.109 |
| US (mL) | 254.7 ± 99.3 | 215.5 ± 84.2 | 0.086 |
| Pdet.Qmax (cmH2O) | 59.0 ± 44.5 | 50.8 ± 35.2 | 0.414 |
| Compliance | 71.0 ± 66.6 | 58.9 ± 67.2 | 0.451 |
| Qmax (mL/s) | 8.06 ± 5.77 | 6.88 ± 4.09 | 0.352 |
| Volume (mL) | 158.3 ± 110.8 | 122.9 ± 78.7 | 0.104 |
| PVR (mL) | 179.8 ± 141.7 | 167.7 ± 101.9 | 0.698 |
| CBC (mL) | 338.1 ± 137.3 | 290.6 ± 105.1 | 0.123 |
| VE | 48.5 ± 32.5 | 44.8 ± 28.3 | 0.614 |
| BOOI | 42.8 ± 47.0 | 37.0 ± 35.7 | 0.578 |
| DO | 42(76.4%) | 18 (69.2%) | 0.629 |
| DV subtype | 0.376 | ||
| BND + DV | 4 (7.3%) | 3 (11.5%) | |
| Mid-urethra DV | 40 (72.7%) | 15 (57.7%) | |
| Distal urethra DV | 11 (20%) | 8 (30.8%) | |
| CNS lesion | 13 (24.1%) | 2 (7.7%) | 0.125 |
| Storage LUTS | 37 (67.3%) | 20 (76.9%) | 0.375 |
| Voiding LUTS | 49 (89.1%) | 22 (84.6%) | 0.719 |
| Parameter | BND + DV (n = 7) | Mid-Urethra DV (n = 55) | Distal Urethra DV (n = 19) | p Value |
|---|---|---|---|---|
| Age | 58.3 ± 20.5 | 57.1 ± 15.4 | 68.7 ± 11.6 | 0.018 |
| FSF (mL) | 140.9 ± 75.1 | 137.7 ± 72.1 | 131.3 ± 47.9 | 0.923 |
| FS (mL) | 215.7 ± 117.2 | 196.4 ± 80.5 | 230.7 ± 69.6 | 0.279 |
| US (mL) | 265.4 ± 109.1 | 226.4 ± 92.4 | 279.1 ± 94.5 | 0.093 |
| Pdet.Qmax (cmH2O) | 86.9 ± 60.6 | 61.8 ± 41.2 | 29.4 ± 14.3 | 0.001 |
| Compliance | 65.7 ± 55.7 | 61.7 ± 64.7 | 83.2 ± 75.9 | 0.483 |
| Qmax (mL/s) | 5.7 ± 4.0 | 7.9 ± 5.6 | 7.7 ± 4.8 | 0.588 |
| Volume (mL) | 98.1 ± 55.6 | 155.6 ± 112.4 | 139.8 ± 80.8 | 0.359 |
| PVR (mL) | 211.4 ± 159.9 | 160.0 ± 134.4 | 209.0 ± 98.4 | 0.277 |
| CBC (mL) | 309.6 ± 126.3 | 315.6 ± 129.1 | 348.8 ± 133.7 | 0.608 |
| VE | 0.407 ± 0.322 | 0.513 ± 0.337 | 0.384 ± 0.196 | 0.252 |
| BOOI | 75.4 ± 62.4 | 45.9 ± 43.7 | 13.9 ± 10.2 | 0.001 |
| DO | 6 (85.7%) | 41 (74.5%) | 9 (47.4%) | 0.063 |
| CNS lesion | 0 | 11 (20.4%) | 4 (21.1%) | 0.539 |
| Storage LUTS | 5 (71.4%) | 40 (72.7%) | 12 (63.2%) | 0.798 |
| Voiding LUTS | 6 (85.7%) | 48 (87.3) | 17 (89.5%) | 1.000 |
| Successful outcome | 4 (57.1%) | 40 (72.7%) | 11 (57.9%) | 0.376 |
| GRA= +3 | 0 | 12 (21.8%) | 3 (15.8%) | |
| GRA= +2 | 2 (28.6%) | 18 (32.7%) | 5 (26.3%) | |
| GRA= +1 | 2 (28.6%) | 10 (18.2%) | 3 (15.8%) | |
| GRA= 0 | 3 (42.9%) | 12 (21.8%) | 8 (42.1%) | |
| GRA= −1 | 0 | 3 (5.5%) | 0 |
| Total DV (n = 81) | BND + DV (n = 7) | Mid-Urethra DV (n = 55) | Distal Urethra DV (n = 19) | |||||
|---|---|---|---|---|---|---|---|---|
| BL | FU | BL | FU | BL | FU | BL | FU | |
| Storage LUTS | 57 (70.4%) | 41 (50.6%) | 5 (71.4%) | 3 (42.9%) | 40 (72.7%) | 30 (54.5%) | 12 (63.2%) | 8 (42.1%) |
| Frequency/urgency/nocturia | 19 | 17 | 1 | 1 | 10 | 10 | 8 | 6 |
| Urgency incontinence | 38 | 24 | 4 | 2 | 30 | 20 | 4 | 2 |
| Voiding LUTS | 71 (87.7%) | 34 (42.0%) | 6 (85.7%) | 2 (28.6%) | 48 (87.3%) | 21 (38.2%) | 17 (89.5%) | 11 (57.9%) |
| Difficult urination | 67 | 34 | 5 | 2 | 45 | 21 | 17 | 11 |
| Urinary retention | 4 | 0 | 1 | 0 | 3 | 0 | 0 | 0 |
| Painful LUTS | 11 (13.6%) | 4 (4.9%) | 1 (14.3%) | 0 (0%) | 5 (9.1%) | 2 (3.6%) | 0 | 0 |
| Bladder pain | 6 | 2 | 1 | 0 | 5 | 2 | 0 | 0 |
| Miction pain | 5 | 2 | 2 | 1 | 3 | 1 | 0 | 0 |
| Parameter | Successful (n = 55) | Failure (n = 26) | p | |
|---|---|---|---|---|
| FSF (mL) | BL FU | 152.3 ± 79.5 150.4 ± 94.3 | 119.2 ± 52.4 131.7 ± 105.6 | 0.652 |
| FS (mL) | BL FU | 225.2 ± 97.0 206.9 ± 102.8 | 195.4 ± 67.7 173.1 ± 125.9 | 0.910 |
| US (mL) | BL FU | 257.8 ± 107.6 232.1 ± 119.9 | 226.0 ± 82.6 192.8 ± 136.3 | 0.839 |
| Pdet.Qmax (cmH2O) | BL FU | 59.9 ± 38.8 44.4 ± 33.6 * | 51.2 ± 36.0 36.2 ± 35.7 | 0.959 |
| Compliance | BL FU | 60.9 ± 52.8 64.2 ± 63.8 | 69.6 ± 84.7 57.3 ± 61.2 | 0.526 |
| Qmax (mL/s) | BL FU | 8.51 ± 6.21 8.83 ± 8.19 | 7.53 ± 4.72 4.85 ± 4.33 | 0.254 |
| Volume (mL) | BL FU | 146.2 ± 108.2 160.1 ± 140.7 | 126.5 ± 87.1 82.9 ± 73.4 | 0.185 |
| PVR (mL) | BL FU | 206.0 ± 137.5 132.6 ± 156.1 * | 195.3 ± 101.6 243.3 ± 239.2 | 0.032 |
| CBC (mL) | BL FU | 352.2 ± 145.2 292.6 ± 136.9 * | 321.9 ± 116.6 326.2 ± 215.4 | 0.185 |
| Voiding efficiency | BL FU | 42.7 ± 28.3 58.2 ± 36.8 * | 40.3 ± 27.4 34.3 ± 32.4 | 0.057 |
| BOOI | BL FU | 42.9 ± 41.8 26.7 ± 39.5 * | 36.1 ± 37.4 26.5 ± 32.8 | 0.630 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, Y.-H.; Lee, C.-L.; Chen, S.-F.; Kuo, H.-C. Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins 2021, 13, 362. https://doi.org/10.3390/toxins13050362
Jiang Y-H, Lee C-L, Chen S-F, Kuo H-C. Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins. 2021; 13(5):362. https://doi.org/10.3390/toxins13050362
Chicago/Turabian StyleJiang, Yuan-Hong, Cheng-Ling Lee, Sheng-Fu Chen, and Hann-Chorng Kuo. 2021. "Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women" Toxins 13, no. 5: 362. https://doi.org/10.3390/toxins13050362
APA StyleJiang, Y.-H., Lee, C.-L., Chen, S.-F., & Kuo, H.-C. (2021). Therapeutic Effects of Urethral Sphincter Botulinum Toxin A Injection on Dysfunctional Voiding with Different Videourodynamic Characteristics in Non-Neurogenic Women. Toxins, 13(5), 362. https://doi.org/10.3390/toxins13050362






