Association of Urinary Mycotoxins with Sperm Quality: A Case-Control Study in Southern Nigeria
Abstract
1. Introduction
2. Results
2.1. Variation in the Metabolites by Sperm Parameters
2.2. Estimating the Effect of the Metabolites of Mycotoxins on Sperm Parameters
3. Discussion
4. Conclusions
5. Material and Methods
5.1. Study Design and Population
5.2. Sample Size
5.3. Data Collection
5.4. Semen Collection and Analysis
5.5. Analysis of Metabolites of Mycotoxins from Filtered Urine Samples
5.5.1. Solid-Phase Extraction (SPE)
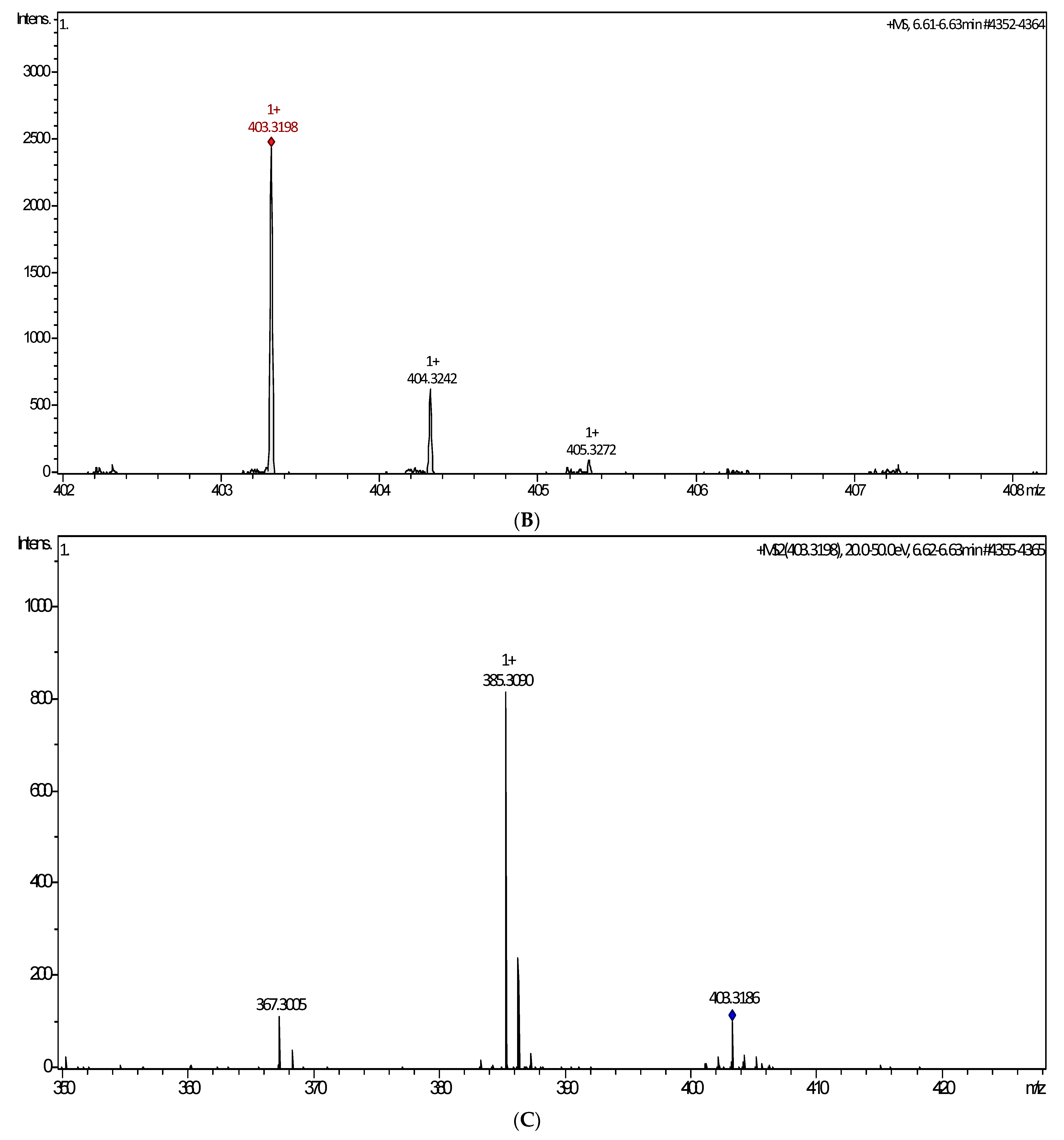
5.5.2. Liquid Chromatography–Mass Spectrometry (LCMS) Method
5.6. Validation
5.7. Data Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Auger, J.; Eustache, F.; Chevrier, C.; Jégou, B. Spatiotemporal trends in human semen quality. Nat. Rev. Urol. 2022, 19, 597–626. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, P.; Nwagha, U.; Dutta, S.; Krajewska-Kulak, E.; Izuka, E. Evidence for decreasing sperm count in African population from 1965 to 2015. Afr. Health Sci. 2017, 17, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Barratt, C.L.; Björndahl, L.; De Jonge, C.J.; Lamb, D.J.; Osorio Martini, F.; McLachlan, R.; Oates, R.D.; van der Poel, S.; St John, B.; Sigman, M.; et al. The diagnosis of male infertility: An analysis of the evidence to support the development of global WHO guidance—Challenges and future research opportunities. Hum. Reprod. Update 2017, 23, 660–680. [Google Scholar] [CrossRef] [PubMed]
- Abebe, M.S.; Afework, M.; Abaynew, Y. Primary and secondary infertility in Africa: Systematic review with meta-analysis. Fertil. Res. Pract. 2020, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Eldib, A.; Tashani, O.A. Infertility in the Middle East and North Africa Region: A systematic review with meta-Analysis of prevalence surveys. Libyan J. Med. Sci. 2018, 2, 37–44. [Google Scholar] [CrossRef]
- Osegbe, D.N.; Amaku, E.O. The causes of male infertility in 504 consecutive Nigerian patients. Int. Urol. Nephrol. 1985, 17, 349–358. [Google Scholar] [CrossRef]
- Abdullah, A.A.; Ahmed, M.; Oladokun, A. Prevalence of infertility in Sudan: A systematic review and meta-analysis. Qatar Med. J. 2021, 2021, 47. [Google Scholar]
- Okonofua, F.; Menakaya, U.; Onemu, S.O.; Omo-Aghoja, L.O.; Bergstrom, S. A case-control study of risk factors for male infertility in Nigeria. Asian J. Androl. 2005, 7, 351–361. [Google Scholar] [CrossRef]
- Ikechebelu, J.I.; Adinma, J.I.; Orie, E.F.; Ikegwuonu, S.O. High prevalence of male infertility in southeastern Nigeria. J. Obstet. Gynaecol. 2003, 23, 657–659. [Google Scholar] [CrossRef]
- Abarikwu, S.O. Causes and risk factors for male-factor infertility in Nigeria: A review. Afr. J. Reprod. Health 2013, 17, 150–166. [Google Scholar]
- Okonofua, F.E. Female and Male Infertility in Nigeria: Studies on the Epidemiology of Infertility in Nigeria with Special Reference to the Role of Genital Tract Infections and Sexual and Reproductive Risk Factors; Karolinska Institutet: Solna, Sweden, 2005. [Google Scholar]
- Ahmed, A.; Bello, A.; Mbibu, N.H.; Maitama, H.Y.; Kalayi, G.D. Epidemiological and aetiological factors of male infertility in northern Nigeria. Niger. J. Clin. Pract. 2010, 13, 205–209. [Google Scholar] [PubMed]
- Emokpae, M.A.; Brown, S.I. Effects of lifestyle habits on fertility; practical recommendations for modification. Reprod. Fertil. 2021, 2, R13–R26. [Google Scholar] [CrossRef] [PubMed]
- Colaco, S.; Modi, D. Genetics of the human Y chromosome and its association with male infertility. Reprod. Biol. Endocrinol. 2018, 16, 14. [Google Scholar] [CrossRef] [PubMed]
- Duvuru, R.; Halabi, M.; Omolaoye, T.S.; Du Plessis, S.S. The genetic causes of male infertility: A Middle East and North Africa perspective. F1000Research 2022, 11, 125. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, P.; Banerjee, R. Environmental toxins: Alarming impacts of pesticides on male fertility. Hum. Exp. Toxicol. 2014, 33, 1017–1039. [Google Scholar] [CrossRef]
- Akinloye, O.; Arowojolu, A.O.; Shittu, O.B.; Anetor, J.I. Cadmium toxicity: A possible cause of male infertility in Nigeria. Reprod. Biol. 2006, 6, 17–30. [Google Scholar] [PubMed]
- Rodprasert, W.; Toppari, J.; Virtanen, H.E. Environmental toxicants and male fertility. Best Pract. Res. Clin. Obstet. Gynaecol. 2023, 86, 102298. [Google Scholar] [CrossRef] [PubMed]
- Okonofua, F.E.; Ntoimo, L.F.; Omonkhua, A.; Ayodeji, O.; Olafusi, C.; Unuabonah, E.; Ohenhen, V. Causes and risk factors for Male infertility: A scoping review of published studies. Int. J. Gen. Med. 2022, 15, 5985–5997. [Google Scholar] [CrossRef]
- Eze, U.A.; Routledge, M.N.; Okonofua, F.E.; Huntriss, J.; Gong, Y.Y. Mycotoxin exposure and adverse reproductive health outcomes in Africa: A review. World Mycotoxin J. 2018, 11, 321–339. [Google Scholar] [CrossRef]
- El Khoury, D.; Fayjaloun, S.; Nassar, M.; Sahakian, J.; Aad, P.Y. Updates on the effect of mycotoxins on male reproductive efficiency in mammals. Toxins 2019, 11, 515. [Google Scholar] [CrossRef]
- Manouchehri, A.; Shokri, S.; Pirhadi, M.; Karimi, M.; Abbaszadeh, S.; Mirzaei, G.; Bahmani, M. The effects of toxic heavy metals lead, cadmium and copper on the epidemiology of male and female infertility. JBRA Assist. Reprod. 2022, 26, 627. [Google Scholar] [CrossRef]
- López-Botella, A.; Velasco, I.; Acién, M.; Sáez-Espinosa, P.; Todolí-Torró, J.L.; Sánchez-Romero, R.; Gómez-Torres, M.J. Impact of heavy metals on human male fertility—An overview. Antioxidants 2021, 10, 1473. [Google Scholar] [CrossRef] [PubMed]
- Eze, U.A.; Okonofua, F.E. High prevalence of male infertility in Africa: Are Mycotoxins to blame? Afr. J. Reprod. Health 2015, 19, 9–17. [Google Scholar] [PubMed]
- Tkachev, A.V.; Tkacheva, O.L.; Zubova, T.V.; Pleshkov, V.A.; Smolovskaya, O.V. Effect of Mycotoxins on the Spermatozoa and Embryos of Animals. Adv. Anim. Vet. Sci. 2020, 8, 47–55. [Google Scholar] [CrossRef]
- Atanda, O.; Makun, H.A.; Ogara, I.M.; Edema, M.; Idahor, K.O.; Eshiett, M.E.; Oluwabamiwo, B.F. Fungal and mycotoxin contamination of Nigerian foods and feeds. Mycotoxin Food Saf. Dev. Ctries. 2013, 68, 1455–1458. [Google Scholar]
- Chilaka, C.A.; De Boevre, M.; Atanda, O.O.; De Saeger, S. Prevalence of Fusarium mycotoxins in cassava and yam products from some selected Nigerian markets. Food Control. 2018, 84, 226–231. [Google Scholar] [CrossRef]
- WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen, 6th ed.; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Carballo, D.; Pallarés, N.; Ferrer, E.; Barba, F.J.; Berrada, H. Assessment of human exposure to deoxynivalenol, ochratoxin A, zearalenone and their metabolites biomarker in urine samples using LC-ESI-qTOF. Toxins 2021, 13, 530. [Google Scholar] [CrossRef]
- Fan, K.; Xu, J.; Jiang, K.; Liu, X.; Meng, J.; Di Mavungu, J.D.; Guo, W.; Zhang, Z.; Jing, J.; Li, H.; et al. Determination of multiple mycotoxins in paired plasma and urine samples to assess human exposure in Nanjing, China. Environ. Pollut. 2019, 248, 865–873. [Google Scholar] [CrossRef]
- Huang, Q.; Jiang, K.; Tang, Z.; Fan, K.; Meng, J.; Nie, D.; Zhao, Z.; Wu, Y.; Han, Z. Exposure Assessment of Multiple Mycotoxins and Cumulative Health Risk Assessment: A Biomonitoring-Based Study in the Yangtze River Delta, China. Toxins 2021, 13, 103. [Google Scholar] [CrossRef]
- Šarkanj, B.; Ezekiel, C.N.; Turner, P.C.; Abia, W.A.; Rychlik, M.; Krska, R.; Sulyok, M.; Warth, B. Ultra-sensitive, stable isotope assisted quantification of multiple urinary mycotoxin exposure biomarkers. Anal. Chim. Acta 2018, 1019, 84–92. [Google Scholar] [CrossRef]
- Soriano, J.; Dragacci, S. Occurrence of fumonisins in foods. Food Res. Int. 2004, 37, 985–1000. [Google Scholar] [CrossRef]
- Filannino, A.; Stout, T.A.; Gadella, B.M.; Sostaric, E.; Pizzi, F.; Colenbrander, B.; Dell’Aquila, M.E.; Minervini, F. Dose-response effects of estrogenic mycotoxins (zearalenone, alpha-and beta-zearalenol) on motility, hyperactivation and the acrosome reaction of stallion sperm. Reprod. Biol. Endocrinol. 2011, 9, 134. [Google Scholar] [CrossRef] [PubMed]
- Benzoni, E.; Minervini, F.; Giannoccaro, A.; Fornelli, F.; Vigo, D.; Visconti, A. Influence of in vitro exposure to mycotoxin zearalenone and its derivatives on swine sperm quality. Reprod. Toxicol. 2008, 25, 461–467. [Google Scholar] [CrossRef]
- Balló, A.; Busznyákné Székvári, K.; Czétány, P.; Márk, L.; Török, A.; Szántó, Á.; Máté, G. Estrogenic and Non-Estrogenic Disruptor Effect of Zearalenone on Male Reproduction: A Review. Int. J. Mol. Sci. 2023, 24, 1578. [Google Scholar] [CrossRef] [PubMed]
- Furian, A.F.; Fighera, M.R.; Royes, L.F.; Oliveira, M.S. Recent advances in assessing the effects of mycotoxins using animal models. Curr. Opin. Food Sci. 2022, 47, 100874. [Google Scholar] [CrossRef]
- Minervini, F.; Lacalandra, G.M.; Filannino, A.; Nicassio, M.; Visconti, A.; Dell’Aquila, M.E. Effects of in vitro exposure to natural levels of zearalenone and its derivatives on chromatin structure stability in equine spermatozoa. Theriogenology 2010, 73, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Menkveld, R. Clinical significance of the low normal sperm morphology value as proposed in the fifth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen. Asian J. Androl. 2010, 12, 47. [Google Scholar] [CrossRef] [PubMed]
- Esteves, S.C. Clinical relevance of routine semen analysis and controversies surrounding the 2010 World Health Organization criteria for semen examination. Int. Braz. J. Urol. 2014, 40, 433–453. [Google Scholar] [CrossRef]
- Dickey, R.P.; Pyrzak, R.; Lu, P.Y.; Taylor, S.N.; Rye, P.H. Comparison of the sperm quality necessary for successful intrauterine insemination with World Health Organization threshold values for normal sperm. Fertil. Steril. 1999, 71, 684–689. [Google Scholar] [CrossRef]
- National Population Commission (NPC); ICF. Nigeria Demographic and Health Survey 2018; NPC: Abuja, Nigeria; ICF: Rockville, MD, USA, 2019.
- Little, T.A. Establishing Acceptance Criteria for Analytical Methods. BioPharm Int. 2016, 29, 1705–1717. Available online: https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods (accessed on 10 June 2019).


| Variable | Case (Infertile) N = 136 | Control (Fertile) N = 154 | p-Value |
|---|---|---|---|
| Median (inter-quartile range) | |||
| Age (n = 290) | 40 (10) | 40 (9) | 0.4253 |
| Weight (n = 288) | 81 (21.5) | 80 (22) | 0.4177 |
| Height (n = 287) | 1.72 (0.22) | 1.75 (0.28) | 0.8271 |
| Body mass index (BMI) (n = 287) | 27 (6.79) | 26 (6.65) | 0.0216 * |
| Frequency (percentage) | |||
| Marital status (n = 277) | |||
| Single | 11 (8.33) | 13 (8.97) | |
| Married | 121 (91.67) | 132 (91.03) | 0.852 |
| Religion | |||
| Muslim | 14 (7.79) | 12 (7.79) | |
| Christian | 118 (86.76) | 138 (89.61) | |
| Traditional/other | 4 (2.94) | 4 (2.60) | 0.760 |
| Education | |||
| Primary | 7 (5.15) | 7 (4.55) | |
| Secondary | 39 (28.68) | 35 (22.73) | |
| Tertiary | 86 (63.24) | 107 (69.48) | |
| Other | 4 (2.94) | 5 (3.25) | 0.676 |
| Occupation | |||
| Agriculture | 5 (3.68) | 5 (3.25) | |
| Business | 38 (27.94) | 47 (30.52) | |
| skilled manual | 15 (11.03) | 19 (12.34) | |
| blue collar | 19 (13.97) | 22 (14.29) | |
| Professional | 28 (20.59) | 24 (15.58) | |
| civil servant | 13 (9.56) | 24 (15.58) | |
| Others | 18 (13.24) | 13 (8.44) | 0.553 |
| Frequency of alcohol intake (n = 281) | |||
| Always | 8 (6.06) | 4 (2.68) | |
| Often | 13 (9.85) | 14 (9.40) | |
| Occasionally | 61 (46.21) | 73 (48.99) | |
| Do not take | 50 (37.88) | 58 (38.93) | 0.585 |
| Frequency of smoking cigarettes (n = 268) | |||
| Often | 6 (4.69) | 1 (0.71) | |
| Occasionally | 4 (3.13) | 7 (5.00) | |
| Do not take | 118 (92.19) | 132 (94.29) | 0.097 |
| Fertility Status | Sperm Count | Active Motility | Total Motility | Morphology | Volume |
|---|---|---|---|---|---|
| Case (median) | 7 | 10 | 20 | 20 | 2 |
| IQR | 16.8 | 24 | 31 | 38 | 1 |
| Min | 0 | 0 | 0 | 0 | 0.5 |
| Max | 76 | 100 | 309 | 80 | 7.5 |
| Control (median) | 46 | 40 | 60 | 57 | 3 |
| IQR | 26 | 18 | 17 | 18 | 1.5 |
| Min | 4.6 | 9 | 27 | 17 | 0.7 |
| Max | 143 | 85 | 95 | 82 | 7.5 |
| Total (median) | 28 | 30 | 50 | 48 | 2.5 |
| IQR | 40 | 29 | 38 | 40 | 1.2 |
| Min | 0 | 0 | 0 | 0 | 0.5 |
| Max | 143 | 100 | 309 | 82 | 7.5 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | 0.0060 |
| Fertility Status | Zearalenone (N = 179) Median (IQR) [Range] | Ochratoxin A (N = 179) Median (IQR) [Range] | Deoxyvinelol (N = 179) Median (IQR) [Range] |
|---|---|---|---|
| Cases | 326 (550) [0–989.22] | 41 (144) [0–2128] | 0 (374.58) [0–1236.95] |
| Controls | 298.5 (663) [0–2926.32] | 46.5 (87) [0–2381] | 0 (358.835) [0–1380.53] |
| Total | 314 (642) [0–2926.32] | 46 (131) [0–2381] | 0 (368) [0–1380.53] |
| p-value | 0.9883 | 0.5588 | 0.5155 |
| Metabolite | Median (IQR) [Min-Max] | p-Value | Median (IQR) [Min-Max] | p-Value | ||
|---|---|---|---|---|---|---|
| Case | Control | |||||
| Sperm count | Normal | Low | Normal | Low | ||
| N = 5 | N = 82 | N = 54 | N = 38 | |||
| Zearalenone | 334 (326) [0–989.22] | 321 (537) [0–984.56] | 0.5645 | 223 (459) [0–975.88] | 376 (691) [0–986.57 | 0.0124 * |
| Ochratoxin A | 81 (130) [0–156] | 39.5 (144) [0–2128] | 0.9696 | 45 (87) 0–2381] | 49 (87) [0–2352] | 0.8120 |
| Deoxyvinelol | 0 (418.41) [0–560] | 0 (319) [0–1236.95] | 0.9125 | 0 (0) [0–1296.2] | 0 (679.89) [0–1380.53] | 0.1995 |
| Normal | Abnormal | Normal | Abnormal | |||
| Active motility | N = 14 | N = 69 | N = 76 | N = 16 | ||
| Zearalenone | 253.5 (359) [0–950.7] | 364 (713) [0–989.22] | 0.3212 | 289.66 (612.5) [0–986.57] | 315.5 (609.5) [0–970.47] | 0.2195 |
| Ochratoxin A | 39.5 (94) [0–825] | 32 (150) [0–2128] | 0.6603 | 28.5 (80.5) [0–2352] | 80.5 (643.5) [0–2381] | 0.0430 * |
| Deoxyvinelol | 0 (82.61) [0–1236.95] | 0 (418.41) [0–1210.26] | 0.8511 | 0 (207.835) [0–1380.53] | 0 (631.47) [0–791] | 0.8204 |
| Total motility | N = 24 | N = 62 | N = 89 | N = 3 | ||
| Zearalenone | 303 (711.81) [0–989.22] | 326.5 (537) [0–984.56] | 0.9883 | 298 (642) [0–986.57] | 298 (581) [192–773] | 0.7643 |
| Ochratoxin A | 0 (101) [0–825] | 72.5 (156) [0–2128] | 0.1585 | 43 (87) [0–2381] | 77 (2109) [52–2161] | 0.1456 |
| Deoxyvinelol | 0 (852.265) [0–1236.95] | 0 (36) [0–1210.26] | 0.1836 | 0 (368) [0–1380.53] | 0 (0) [0–0] | 0.2804 |
| Morphology | N = 60 | N = 23 | N = 154 | N = 0 | ||
| Zearalenone | 291 (543.5) [0–989.22] | 327 (493) [0–976.53] | 0.6361 | 298 (649.5) [0–986.57] | - | - |
| Ochratoxin A | 30.5 (103) [0–2128] | 101 (466.99) [0–1926] | 0.1385 | 46.5 (87) [0–2381] | - | - |
| Deoxyvinelol | 0 (718) [0–1236.95] | 0 (0) [0–1074] | 0.1265 | 0 (358.835) [0–1380.53] | - | - |
| Volume | N = 74 | N = 10 | N = 85 | N = 5 | ||
| Zearalenone | 321 (550) [0–989.22] | 415.5 (542) [0–984.56] | 0.3612 | 299 (669) [0–986.57] | 160 (332) [0–476] | 0.3023 |
| Ochratoxin A | 33.5 (144) [0–2128] | 95 (763) [0–1331] | 0.2080 | 46 (87) [0–2381] | 70 (70) [0–1457] | 0.7918 |
| Deoxyvinelol | 0 (374.58) [0–1236.95] | 0 (0) [0–822] | 0.3991 | 0 (416.75) [0–1380.53] | 0 (0) [0–0] | 0.1525 |
| Metabolites. | Case | Control | ||
|---|---|---|---|---|
| Unadjusted (SE) [95% CI] | Adjusted (SE) [95% CI] | Unadjusted (SE) [95% CI] | Adjusted (SE) [95% CI] | |
| Sperm count | ||||
| Zearalenone | 0.0081 (0.0050) [−0.0018–0.0180] | 0.0041 (0.0090) [−0.0135–0.0217] | −0.0115 (0.0050) [−0.0213–−0.0016] * | −0.0010 (0.0190) [−0.0382–0.0362] |
| Ochratoxin A | 0.0003 (0.0026) [−0.0049–0.0055] | −0.0085 (0.0177) [−0.0431–0.0331] | 0.0045 (0.0086) [−0.0124–0.0261] | 0.0323 (0.0589) [−0.0832–0.1479] |
| Deoxyvinelol | 0.0124 (0.0075) [−0.0023–0.0271] | −0.0410 (0.1162) [−0.2688–0.1867] | −0.0107 (0.0057) [−0.0219–0.0004] | 0.0360 (0.1224) [−0.2040–0.2759] |
| Active motility | ||||
| Zearalenone | −0.0006 (0.0051) [−0.0107–0.0094] | −0.0302 (0.0089) [−0.0475–−0.0130] ** | −0.0065 (0.0039) [−0.0140–0.0011] | −0.0012 (0.0126) [−0.0259–0.0236] |
| Ochratoxin A | −0.0037 (0.0028) [−0.0092–0.0019] | −0.0189 (0.0176) [−0.0533–0.0157] | −0.0042 (0.0040) [−0.0120–0.0037] | −0.0051 (0.0367) [−0.0770–0.0668] |
| Deoxyvinelol | 0.0023 (0.0037) [−0.0051–0.0096] | −0.0161 (0.0733) [−0.1598–0.1275] | 0.0021 (0.0091) [−0.0157–0.0199] | 0.0194 (0.0418) [−0.0624–0.1013] |
| Total motility | ||||
| Zearalenone | 0.0097 (0.0189) [−0.0274–0.0468] | −0.0500 (0.0212) [−0.0915–−0.0085] * | −0.0012 (0.0029) [−0.0069–0.0045] | −0.0040 (0.0117) [−0.0269–0.0189] |
| Ochratoxin A | −0.0106 (0.0060) [−0.0223–0.0010] | −0.0579 (0.0255) [−0.1079–−0.0079] * | −0.0041 (0.0028) [−0.0097–0.0014] | −0.0028 (0.0225) [−0.0470–0.0414] |
| Deoxyvinelol | 0.0254 (0.0183) [−0.0103–0.0612] | −0.0130 (0.1033) [−0.2155–0.1895] | −0.0017 (0.0026) [−0.0068–0.0035] | −0.0018 (0.0677) [−0.1344–0.1308] |
| Morphology | ||||
| Zearalenone | −0.0066 (0.0091) [−0.0244–0.0112] | −0.0079 (0.0151) [−0.0375–0.0217] | 0.0042 (0.0042) [−0.0040–0.0123] | 0.0003 (0.0115) [−0.0223–0.0230] |
| Ochratoxin A | −0.0268 (0.0106) [−0.0475–−0.0061] * | −0.0417 (0.0284) [−0.0975–0.0140] | −0.0007 (0.0137) [−0.0276–0.0262] | −0.0161 (0.0271) [−0.0693–0.0371] |
| Deoxyvinelol | −0.0047 (0.0055) [−0.0156–0.0062] | −0.0701 (0.1876) [−0.4378–0.2977] | 0.0007 (0.0039) [−0.0069–0.0083] | 0.0036 (0.0618) [−0.1175–0.1248] |
| Volume | ||||
| Zearalenone | 0.0002 (0.0003) [−0.0003–0.0008] | 0.0023 (0.0005) [0.0012–0.0033] *** | −0.0001 (0.0003) [−0.0008–0.0006] | −0.0001 (0.0009) [−0.0018–0.0017] |
| Ochratoxin A | −0.0001 (0.0002) [−0.0005–0.0003] | 0.0006 (0.0022) [−0.0037–0.0048] | 0.0002 (0.0019) [−0.0035–0.0038] | −0.0004 (0.0020) [−0.0043–0.0035] |
| Deoxyvinelol | 0.0037 (0.0050) [−0.0061–0.0135] | 0.0065 (0.0603) [−0.1118–0.1247] | 2.54 × 10−6 (0.0057) [−0.0112–0.0112] | 0.0015 (0.0042) [−0.0068–0.0097] |
| Hospital Code | Freq. | Percent |
|---|---|---|
| Abel Guobadia | 18 | 6.2 |
| Central Hospital | 33 | 11.4 |
| Graceland | 43 | 14.8 |
| (UBTH) | 130 | 44.8 |
| (UNIMEDTH) | 66 | 22.8 |
| Total | 290 |
| Mycotoxin | Retention Time (min) | Linear Range * | Linearity R2 | LOD * | LOQ * | % Recovery | RSD |
|---|---|---|---|---|---|---|---|
| DON | 4.9 | 0.1–500 | 0.999 | 0.61 | 1.84 | 105.16 | 3.09 |
| ZEA | 5.9 | 1–1000 | 0.999 | 0.23 | 0.71 | 84.49 | 3.93 |
| OTA | 6.8 | 1–1000 | 0.998 | 0.16 | 0.48 | 122.44 | 1.61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okonofua, F.E.; Ntoimo, L.F.C.; Unuabonah, E.I.; Msagati, T.A.M.; Ayodeji, O.; Aziken, M.; Omonkhua, A.; Ohenhen, V.; Olafusi, C.; Alfred, M.O. Association of Urinary Mycotoxins with Sperm Quality: A Case-Control Study in Southern Nigeria. Toxins 2024, 16, 119. https://doi.org/10.3390/toxins16030119
Okonofua FE, Ntoimo LFC, Unuabonah EI, Msagati TAM, Ayodeji O, Aziken M, Omonkhua A, Ohenhen V, Olafusi C, Alfred MO. Association of Urinary Mycotoxins with Sperm Quality: A Case-Control Study in Southern Nigeria. Toxins. 2024; 16(3):119. https://doi.org/10.3390/toxins16030119
Chicago/Turabian StyleOkonofua, Friday Ebhodaghe, Lorretta Favour Chizomam Ntoimo, Emmanuel Iyayi Unuabonah, Titus Afred Makudali Msagati, Oladiran Ayodeji, Michael Aziken, Akhere Omonkhua, Victor Ohenhen, Celestina Olafusi, and Moses O. Alfred. 2024. "Association of Urinary Mycotoxins with Sperm Quality: A Case-Control Study in Southern Nigeria" Toxins 16, no. 3: 119. https://doi.org/10.3390/toxins16030119
APA StyleOkonofua, F. E., Ntoimo, L. F. C., Unuabonah, E. I., Msagati, T. A. M., Ayodeji, O., Aziken, M., Omonkhua, A., Ohenhen, V., Olafusi, C., & Alfred, M. O. (2024). Association of Urinary Mycotoxins with Sperm Quality: A Case-Control Study in Southern Nigeria. Toxins, 16(3), 119. https://doi.org/10.3390/toxins16030119






