Adverse Effects of Intravesical OnabotulinumtoxinA Injection in Patients with Idiopathic Overactive Bladder or Neurogenic Detrusor Overactivity: A Systematic Review and Meta-Analysis of Randomized Controlled Studies
Abstract
:1. Introduction
2. Results
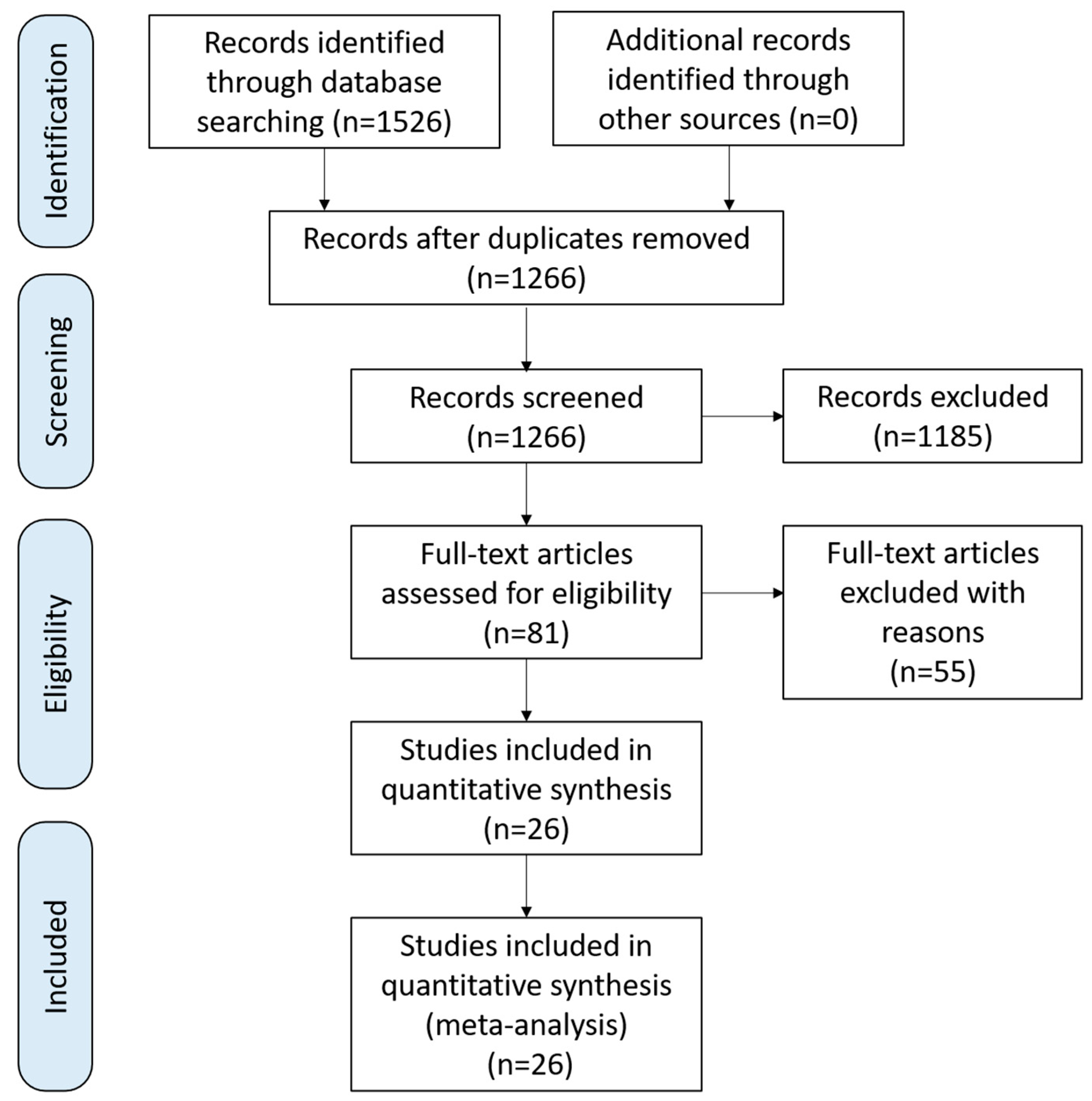
2.1. Study Selection, Characteristics, and Risk of Bias
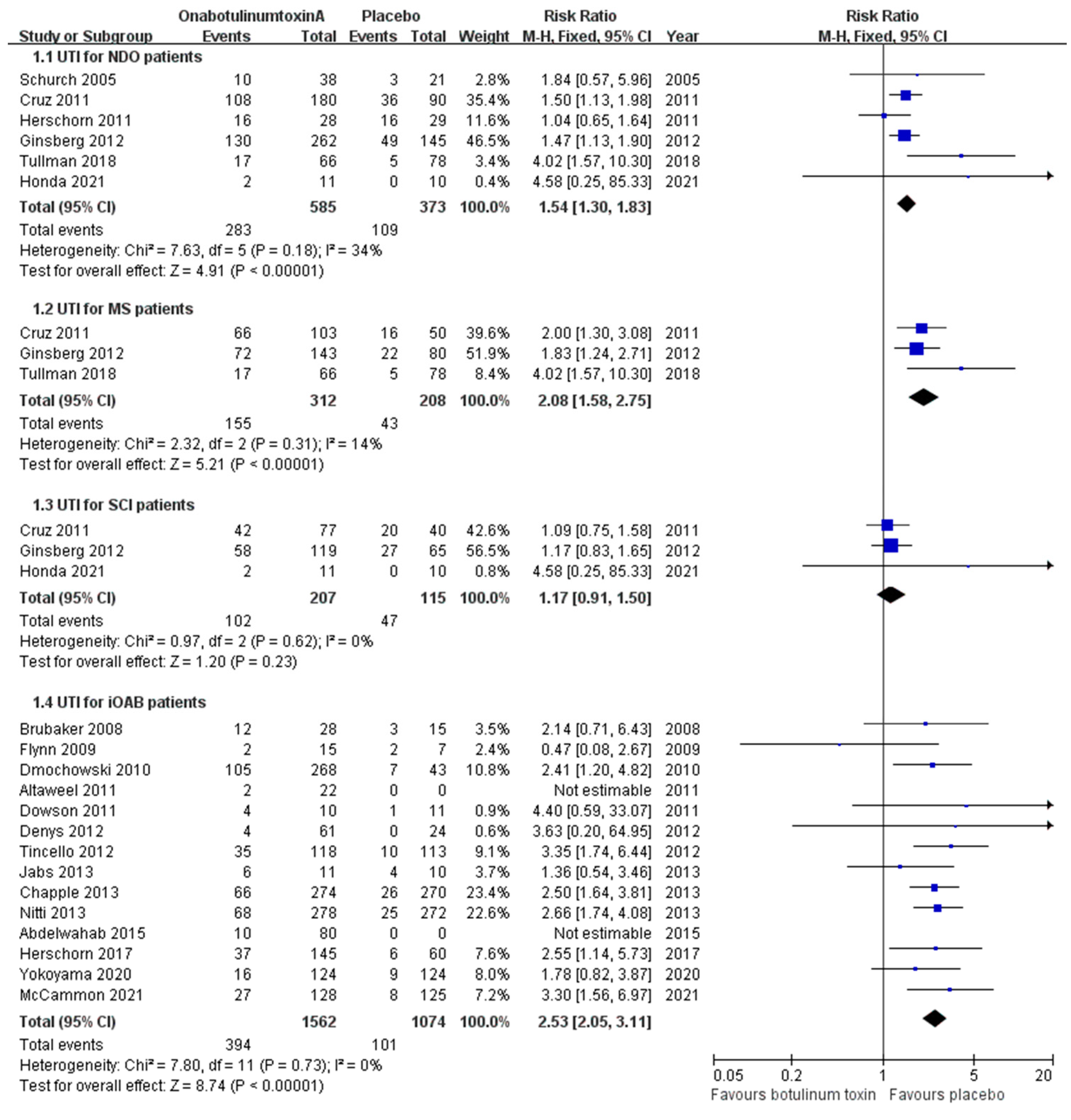
2.2. Adverse Effects Localized to Urinary Tract
2.2.1. Urinary Tract Infections
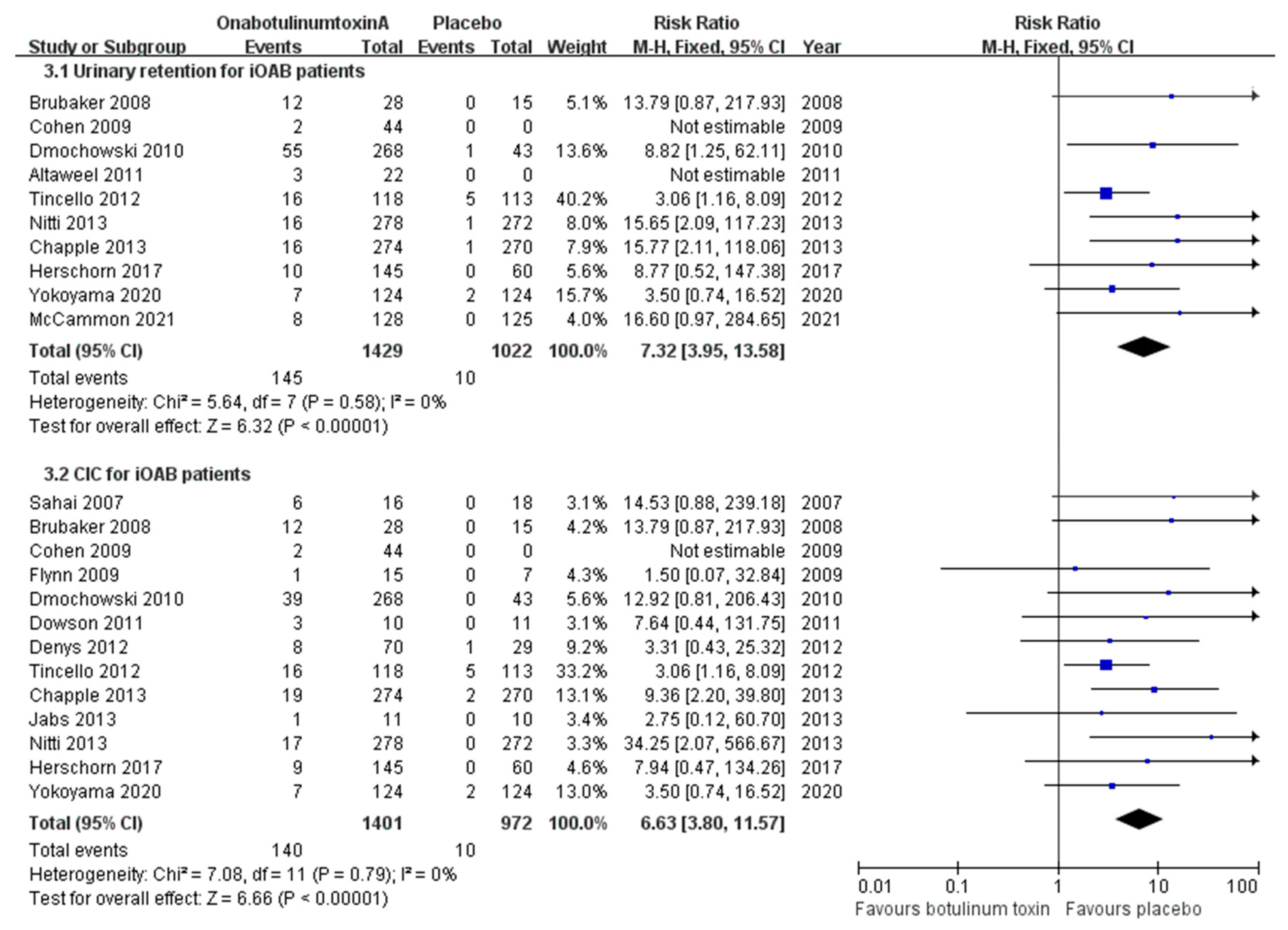
2.2.2. Urinary Retention
2.2.3. Voiding Difficulty
2.2.4. Hematuria
2.2.5. Bladder Pain
2.3. Systemic Adverse Effects
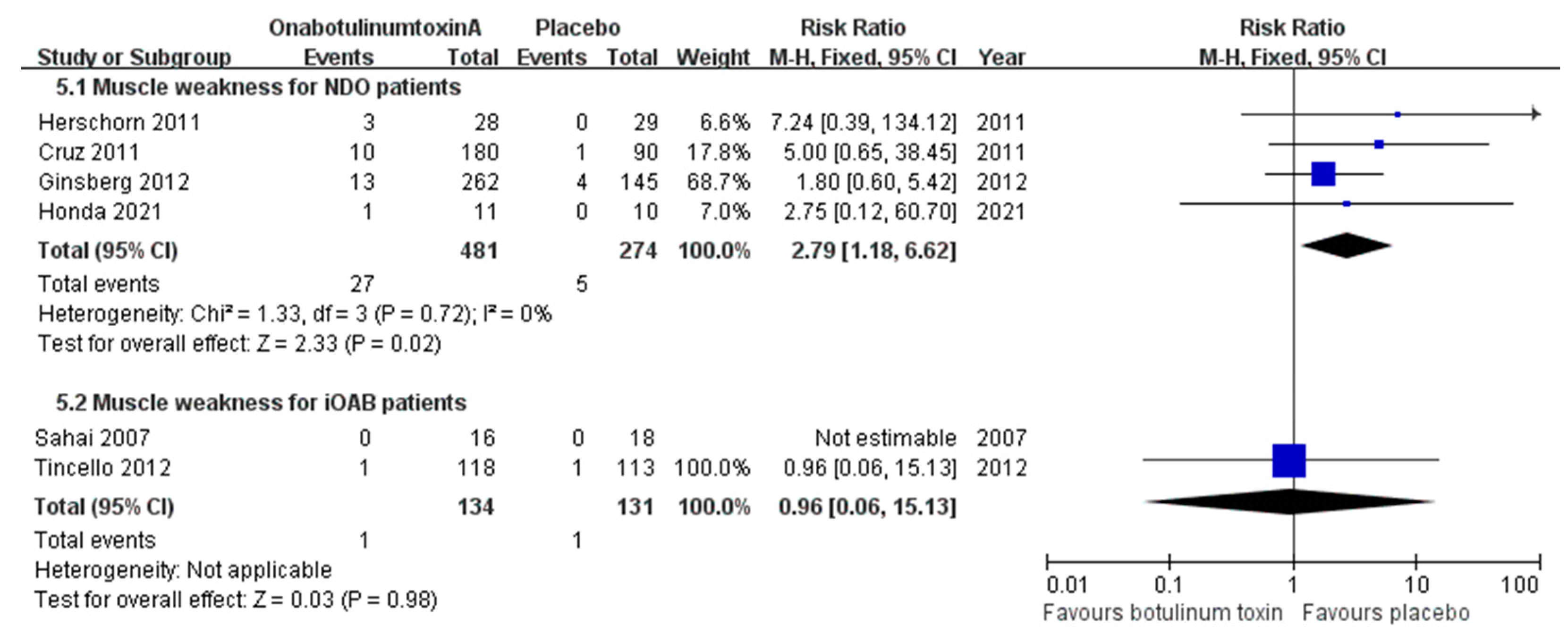
2.3.1. Muscle Weakness
2.3.2. Fatigue
2.3.3. Symptoms Related to the Digestive System (Nausea, Diarrhea, and Constipation)
2.3.4. Pyrexia
2.3.5. Autonomic Dysreflexia
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Search Strategy
5.2. Inclusion and Exclusion Criteria
5.3. Quality Assessment
5.4. Data Extraction
5.5. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A.; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: Report from the standardisation sub-committee of the International Continence Society. Urology 2003, 61, 37–49. [Google Scholar] [CrossRef] [PubMed]
- White, N.; Iglesia, C.B. Overactive bladder. Obstet. Gynecol. Clin. N. Am. 2016, 43, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Stewart, W.F.; Van Rooyen, J.B.; Cundiff, G.W.; Abrams, P.; Herzog, A.R.; Corey, R.; Hunt, T.L.; Wein, A.J. Prevalence and burden of overactive bladder in the United States. World J. Urol. 2003, 20, 327–336. [Google Scholar] [CrossRef]
- Lawrence, J.M.; Lukacz, E.S.; Nager, C.W.; Hsu, J.W.; Luber, K.M. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet. Gynecol. 2008, 111, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Durden, E.; Walker, D.; Gray, S.; Fowler, R.; Juneau, P.; Gooch, K. The economic burden of overactive bladder (OAB) and its effects on the costs associated with other chronic, age-related comorbidities in the United States. Neurourol. Urodyn. 2018, 37, 1641–1649. [Google Scholar] [CrossRef] [PubMed]
- Irwin, D.E.; Milsom, I.; Hunskaar, S.; Reilly, K.; Kopp, Z.; Herschorn, S.; Coyne, K.; Kelleher, C.; Hampel, C.; Artibani, W.; et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur. Urol. 2006, 50, 1306–1315. [Google Scholar] [CrossRef]
- Giarenis, I.; Cardozo, L. Management of refractory overactive bladder. Minerva. Ginecol. 2013, 65, 41–52. [Google Scholar]
- Rai, B.P.; Cody, J.D.; Alhasso, A.; Stewart, L. Anticholinergic drugs versus non-drug active therapies for non-neurogenic overactive bladder syndrome in adults. Cochrane Database Syst. Rev. 2012, 12, CD003193. [Google Scholar] [CrossRef]
- Majumdar, A.; Toozs-Hobson, P. Detrusor overactivity. Curr. Obstet. Gynaecol. 2004, 14, 395–404. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Cerruto, M.A.; Del Popolo, G.; La Martina, M.; Artibani, W.; Carone, R.; Finazzi-Agrò, E. An overview on mixed action drugs for the treatment of overactive bladder and detrusor overactivity. Urol. Int. 2012, 89, 259–269. [Google Scholar] [CrossRef]
- Sherif, H.; Khalil, M.; Omar, R. Management of refractory idiopathic overactive bladder: Intradetrusor injection of botulinum toxin type A versus posterior tibial nerve stimulation. Can. J. Urol. 2017, 24, 8838–8846. [Google Scholar]
- Lo, C.W.; Wu, M.Y.; Yang, S.S.; Jaw, F.S.; Chang, S.J. Comparing the efficacy of onabotulinumtoxinA, sacral neuromodulation, and peripheral tibial nerve stimulation as third line treatment for the management of overactive bladder symptoms in adults: Systematic review and network meta-analysis. Toxins 2020, 12, 128. [Google Scholar] [CrossRef]
- Duthie, J.B.; Vincent, M.; Herbison, G.P.; Wilson, D.I.; Wilson, D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst. Rev. 2011, CD005493. [Google Scholar] [CrossRef]
- Dong, M.; Yeh, F.; Tepp, W.H.; Dean, C.; Johnson, E.A.; Janz, R.; Chapman, E.R. SV2 is the protein receptor for botulinum neurotoxin A. Science 2006, 312, 592–596. [Google Scholar] [CrossRef]
- Simpson, L.L. Kinetic studies on the interaction between botulinum toxin type A and the cholinergic neuromuscular junction. J. Pharmacol. Exp. Ther. 1980, 212, 16–21. [Google Scholar]
- Schurch, B.; Schmid, D.M.; Stöhrer, M. Treatment of neurogenic incontinence with botulinum toxin A. N. Engl. J. Med. 2000, 342, 665. [Google Scholar] [CrossRef]
- Schurch, B. Botulinum toxin for the management of bladder dysfunction. Drugs 2006, 66, 1301–1318. [Google Scholar] [CrossRef]
- Gormley, E.A.; Lightner, D.J.; Faraday, M.; Vasavada, S.P.; American Urological Association; Society of Urodynamics; Female Pelvic Medicine. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J. Urol. 2015, 193, 1572–1580. [Google Scholar] [CrossRef]
- Lucas, M.G.; Bosch, R.J.; Burkhard, F.C.; Cruz, F.; Madden, T.B.; Nambiar, A.K.; Neisius, A.; de Ridder, D.J.; Tubaro, A.; Turner, W.H.; et al. EAU guidelines on assessment and nonsurgical management of urinary incontinence. Eur. Urol. 2012, 62, 1130–1142. [Google Scholar] [CrossRef]
- Nitti, V.; Haag-Molkenteller, C.; Kennelly, M.; Chancellor, M.; Jenkins, B.; Schurch, B. Treatment of neurogenic detrusor overactivity and overactive bladder with Botox (onabotulinumtoxinA): Development, insights, and impact. Medicine 2023, 102, e32377. [Google Scholar] [CrossRef]
- Product Information. Available online: https://www.rxabbvie.com/pdf/botox_pi.pdf (accessed on 3 May 2024).
- Linsenmeyer, T.A.; Linsenmeyer, M.A. Impact of annual urodynamic evaluations on guiding bladder management in individuals with spinal cord injuries. J. Spinal Cord Med. 2013, 36, 420–426. [Google Scholar] [CrossRef]
- Cruz, F.; Herschorn, S.; Aliotta, P.; Brin, M.; Thompson, C.; Lam, W.; Daniell, G.; Heesakkers, J.; Haag-Molkenteller, C. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: A randomised, double-blind, placebo-controlled trial. Eur. Urol. 2011, 60, 742–750. [Google Scholar] [CrossRef]
- Ginsberg, D.; Gousse, A.; Keppenne, V.; Sievert, K.D.; Thompson, C.; Lam, W.; Brin, M.F.; Jenkins, B.; Haag-Molkenteller, C. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J. Urol. 2012, 187, 2131–2139. [Google Scholar] [CrossRef]
- Schurch, B.; de Sèze, M.; Denys, P.; Chartier-Kastler, E.; Haab, F.; Everaert, K.; Plante, P.; Perrouin-Verbe, B.; Kumar, C.; Fraczek, S.; et al. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: Results of a single treatment, randomized, placebo controlled 6-month study. J. Urol. 2005, 174, 196–200. [Google Scholar] [CrossRef]
- Herschorn, S.; Gajewski, J.; Ethans, K.; Corcos, J.; Carlson, K.; Bailly, G.; Bard, R.; Valiquette, L.; Baverstock, R.; Carr, L.; et al. Efficacy of botulinum toxin A injection for neurogenic detrusor overactivity and urinary incontinence: A randomized, double-blind trial. J. Urol. 2011, 185, 2229–2235. [Google Scholar] [CrossRef]
- Ginsberg, D.; Cruz, F.; Herschorn, S.; Gousse, A.; Keppenne, V.; Aliotta, P.; Sievert, K.D.; Brin, M.F.; Jenkins, B.; Thompson, C.; et al. OnabotulinumtoxinA is effective in patients with urinary incontinence due to neurogenic detrusor overactivity [corrected] regardless of concomitant anticholinergic use or neurologic etiology. Adv. Ther. 2013, 30, 819–833. [Google Scholar] [CrossRef]
- Rovner, E.; Dmochowski, R.; Chapple, C.; Thompson, C.; Lam, W.; Haag-Molkenteller, C. OnabotulinumtoxinA improves urodynamic outcomes in patients with neurogenic detrusor overactivity. Neurourol. Urodyn. 2013, 32, 1109–1115. [Google Scholar] [CrossRef]
- Tullman, M.; Chartier-Kastler, E.; Kohan, A.; Keppenne, V.; Brucker, B.M.; Egerdie, B.; Mandle, M.; Nicandro, J.P.; Jenkins, B.; Denys, P. Low-dose onabotulinumtoxinA improves urinary symptoms in noncatheterizing patients with MS. Neurology 2018, 91, e657–e665. [Google Scholar] [CrossRef]
- Honda, M.; Yokoyama, O.; Takahashi, R.; Matsuda, T.; Nakayama, T.; Mogi, T. Botulinum toxin injections for Japanese patients with urinary incontinence caused by neurogenic detrusor overactivity: Clinical evaluation of onabotulinumtoxinA in a randomized, placebo-controlled, double-blind trial with an open-label extension. Int. J. Urol. 2021, 28, 906–912. [Google Scholar] [CrossRef]
- Sahai, A.; Khan, M.S.; Dasgupta, P. Efficacy of botulinum toxin-A for treating idiopathic detrusor overactivity: Results from a single center, randomized, double-blind, placebo controlled trial. J. Urol. 2007, 177, 2231–2236. [Google Scholar] [CrossRef]
- Brubaker, L.; Richter, H.E.; Visco, A.; Mahajan, S.; Nygaard, I.; Braun, T.M.; Barber, M.D.; Menefee, S.; Schaffer, J.; Weber, A.M.; et al. Refractory idiopathic urge urinary incontinence and botulinum A injection. J. Urol. 2008, 180, 217–222. [Google Scholar] [CrossRef]
- Cohen, B.L.; Barboglio, P.; Rodriguez, D.; Gousse, A.E. Preliminary results of a dose-finding study for botulinum toxin-A in patients with idiopathic overactive bladder: 100 versus 150 units. Neurourol. Urodyn. 2009, 28, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.K.; Amundsen, C.L.; Perevich, M.; Liu, F.; Webster, G.D. Outcome of a randomized, double-blind, placebo controlled trial of botulinum A toxin for refractory overactive bladder. J. Urol. 2009, 181, 2608–2615. [Google Scholar] [CrossRef]
- Dmochowski, R.; Chapple, C.; Nitti, V.W.; Chancellor, M.; Everaert, K.; Thompson, C.; Daniell, G.; Zhou, J.; Haag-Molkenteller, C. Efficacy and safety of onabotulinumtoxinA for idiopathic overactive bladder: A double-blind, placebo controlled, randomized, dose ranging trial. J. Urol. 2010, 184, 2416–2422. [Google Scholar] [CrossRef]
- Altaweel, W.; Mokhtar, A.; Rabah, D.M. Prospective randomized trial of 100u vs 200u botox in the treatment of idiopathic overactive bladder. Urol. Ann. 2011, 3, 66–70. [Google Scholar] [CrossRef]
- Dowson, C.; Sahai, A.; Watkins, J.; Dasgupta, P.; Khan, M.S. The safety and efficacy of botulinum toxin-A in the management of bladder oversensitivity: A randomised double-blind placebo-controlled trial. Int. J. Clin. Pract. 2011, 65, 698–704. [Google Scholar] [CrossRef]
- Rovner, E.; Kennelly, M.; Schulte-Baukloh, H.; Zhou, J.; Haag-Molkenteller, C.; Dasgupta, P. Urodynamic results and clinical outcomes with intradetrusor injections of onabotulinumtoxinA in a randomized, placebo-controlled dose-finding study in idiopathic overactive bladder. Neurourol. Urodyn. 2011, 30, 556–562. [Google Scholar] [CrossRef]
- Denys, P.; Le Normand, L.; Ghout, I.; Costa, P.; Chartier-Kastler, E.; Grise, P.; Hermieu, J.F.; Amarenco, G.; Karsenty, G.; Saussine, C.; et al. Efficacy and safety of low doses of onabotulinumtoxinA for the treatment of refractory idiopathic overactive bladder: A multicentre, double-blind, randomised, placebo-controlled dose-ranging study. Eur. Urol. 2012, 61, 520–529. [Google Scholar] [CrossRef]
- Tincello, D.G.; Kenyon, S.; Abrams, K.R.; Mayne, C.; Toozs-Hobson, P.; Taylor, D.; Slack, M. Botulinum toxin a versus placebo for refractory detrusor overactivity in women: A randomised blinded placebo-controlled trial of 240 women (the RELAX study). Eur. Urol. 2012, 62, 507–514. [Google Scholar] [CrossRef]
- Chapple, C.; Sievert, K.D.; MacDiarmid, S.; Khullar, V.; Radziszewski, P.; Nardo, C.; Thompson, C.; Zhou, J.; Haag-Molkenteller, C. OnabotulinumtoxinA 100 U significantly improves all idiopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: A randomised, double-blind, placebo-controlled trial. Eur. Urol. 2013, 64, 249–256. [Google Scholar] [CrossRef]
- Nitti, V.W.; Dmochowski, R.; Herschorn, S.; Sand, P.; Thompson, C.; Nardo, C.; Yan, X.; Haag-Molkenteller, C.; EMBARK Study Group. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: Results of a phase 3, randomized, placebo controlled trial. J. Urol. 2013, 189, 2186–2193. [Google Scholar] [CrossRef] [PubMed]
- Jabs, C.; Carleton, E. Efficacy of botulinum toxin a intradetrusor injections for non-neurogenic urinary urge incontinence: A randomized double-blind controlled trial. J. Obstet. Gynaecol. Can 2013, 35, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Sievert, K.D.; Chapple, C.; Herschorn, S.; Joshi, M.; Zhou, J.; Nardo, C.; Nitti, V.W. OnabotulinumtoxinA 100U provides significant improvements in overactive bladder symptoms in patients with urinary incontinence regardless of the number of anticholinergic therapies used or reason for inadequate management of overactive bladder. Int. J. Clin. Pract. 2014, 68, 1246–1256. [Google Scholar] [CrossRef] [PubMed]
- Abdelwahab, O.; Sherif, H.; Soliman, T.; Elbarky, I.; Eshazly, A. Efficacy of botulinum toxin type A 100 Units versus 200 units for treatment of refractory idiopathic overactive bladder. Int. Braz. J. Urol. 2015, 41, 1132–1140. [Google Scholar] [CrossRef] [PubMed]
- Herschorn, S.; Kohan, A.; Aliotta, P.; McCammon, K.; Sriram, R.; Abrams, S.; Lam, W.; Everaert, K. The efficacy and safety of onabotulinumtoxinA or solifenacin compared with placebo in solifenacin naïve patients with refractory overactive bladder: Results from a multicenter, randomized, double-blind phase 3b trial. J. Urol. 2017, 198, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, O.; Honda, M.; Yamanishi, T.; Sekiguchi, Y.; Fujii, K.; Nakayama, T.; Mogi, T. OnabotulinumtoxinA (botulinum toxin type A) for the treatment of Japanese patients with overactive bladder and urinary incontinence: Results of single-dose treatment from a phase III, randomized, double-blind, placebo-controlled trial (interim analysis). Int. J. Urol. 2020, 27, 227–234. [Google Scholar] [CrossRef] [PubMed]
- McCammon, K.; Gousse, A.; Kohan, A.; Glazier, D.; Gruenenfelder, J.; Bai, Z.; Patel, A.; Hale, D. Early and consistent improvements in urinary symptoms and quality of life with onabotulinumtoxinA in patients with overactive bladder and urinary incontinence: Results from a randomized, placebo-controlled, phase IV clinical trial. Female Pelvic Med. Reconstr. Surg. 2021, 27, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Engeler, D.S.; Meyer, D.; Abt, D.; Müller, S.; Schmid, H.P. Sacral neuromodulation for the treatment of neurogenic lower urinary tract dysfunction caused by multiple sclerosis: A single-centre prospective series. BMC Urol. 2015, 15, 105. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, A.O.; Smith, M.J.; Miller, L.A.; Doyle, J.; Ariely, R. Persistence, adherence, and switch rates among extended-release and immediate-release overactive bladder medications in a regional managed care plan. J. Manag. Care Pharm. 2008, 14, 291–301. [Google Scholar] [CrossRef]
- Benner, J.S.; Nichol, M.B.; Rovner, E.S.; Jumadilova, Z.; Alvir, J.; Hussein, M.; Fanning, K.; Trocio, J.N.; Brubaker, L. Patient-reported reasons for discontinuing overactive bladder medication. BJU Int. 2010, 105, 1276–1282. [Google Scholar] [CrossRef]
- Krhut, J.; Gärtner, M.; Petzel, M.; Sykora, R.; Nemec, D.; Tvrdik, J.; Skoupa, J. Persistence with first line anticholinergic medication in treatment-naïve overactive bladder patients. Scand. J. Urol. 2014, 48, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Reitz, A.; Stöhrer, M.; Kramer, G.; Del Popolo, G.; Chartier-Kastler, E.; Pannek, J.; Burgdörfer, H.; Göcking, K.; Madersbacher, H.; Schumacher, S.; et al. European experience of 200 cases treated with botulinum-A toxin injections into the detrusor muscle for urinary incontinence due to neurogenic detrusor overactivity. Eur. Urol. 2004, 45, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Giannantoni, A.; Mearini, E.; Del Zingaro, M.; Porena, M. Six-year follow-up of botulinum toxin A intradetrusorial injections in patients with refractory neurogenic detrusor overactivity: Clinical and urodynamic results. Eur. Urol. 2009, 55, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Azadzoi, K.M.; Pontari, M.; Vlachiotis, J.; Siroky, M.B. Canine bladder blood flow and oxygenation: Changes induced by filling, contraction and outlet obstruction. J. Urol. 1996, 155, 1459–1465. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Yan, H.L.; Cui, Y.S.; Zong, H.T.; Zhang, Y. Efficacy and safety of onabotulinumtoxinA in treating neurogenic detrusor overactivity: A systematic review and meta-analysis. Chin. Med. J. 2015, 128, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.; Shuang, W.B.; Jia, D.D.; Zhang, M.; Tong, X.N.; Yang, W.D.; Jia, X.M.; Li, S. Efficacy and safety of onabotulinumtoxinA in patients with neurogenic detrusor overactivity: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2016, 11, e0159307. [Google Scholar] [CrossRef] [PubMed]
- Gu, H.Y.; Song, J.K.; Zhang, W.J.; Xie, J.; Yao, Q.S.; Zeng, W.J.; Zhang, C.; Niu, Y.M. A systematic review and meta-analysis of effectiveness and safety of therapy for overactive bladder using botulinum toxin A at different dosages. Oncotarget 2017, 8, 90338–90350. [Google Scholar] [CrossRef]
- Nuanthaisong, U.; Abraham, N.; Goldman, H.B. Incidence of adverse events after high doses of onabotulinumtoxinA for multiple indications. Urology 2014, 84, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Linsenmeyer, T.A.; Campagnolo, D.I.; Chou, I.H. Silent autonomic dysreflexia during voiding in men with spinal cord injuries. J. Urol. 1996, 155, 519–522. [Google Scholar] [CrossRef]
- Acute management of autonomic dysreflexia: Adults with spinal cord injury presenting to health-care facilities. Consortium for spinal cord. J. Spinal Cord Med. 1997, 20, 284–308. [CrossRef]
- Schurch, B.; Stöhrer, M.; Kramer, G.; Schmid, D.M.; Gaul, G.; Hauri, D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: A new alternative to anticholinergic drugs? Preliminary results. J. Urol. 2000, 164, 692–697. [Google Scholar] [CrossRef]
- Dmochowski, R.R.; Gomelsky, A. Overactive bladder in males. Ther. Adv. Urol. 2009, 1, 209–221. [Google Scholar] [CrossRef]
- Chen, Y.C.; Kuo, H.C. The therapeutic effects of repeated detrusor injections between 200 or 300 units of onabotulinumtoxinA in chronic spinal cord injured patients. Neurourol. Urodyn. 2014, 33, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Kennelly, M.; Dmochowski, R.; Ethans, K.; Karsenty, G.; Schulte-Baukloh, H.; Jenkins, B.; Thompson, C.; Li, D.; Haag-Molkenteller, C. Long-term efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: An interim analysis. Urology 2013, 81, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. The Cochrane Collaboration. Available online: http://www.cochrane-handbook.org (accessed on 5 March 2011).
- Deeks, J.J. Issues in the selection of a summary statistic for meta-analysis of clinical trials with binary outcomes. Stat. Med. 2002, 21, 1575–1600. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]


| First Author | Year | Region | No. of Patients (Female) | Ages, Means (SD) | Design | Classification | Basic Diseases | Randomization | AEs Follow-Up (Weeks) |
|---|---|---|---|---|---|---|---|---|---|
| Schurch [25] | 2005 | Switzerland, Belgium, and France | 59 (23) | 41 | RCT | NDO | MS6, SCI53 | BTX 200U 19, BTX 300U 19, Placebo 21 | 2, 6, 12, 18, 24 |
| Herschorn [26] | 2011 | Canada | 57 (23) | 42.8 | RCT | NDO | MS19, SCI38 | BTX 300U 28, Placebo 29 | 6, 24, 36 |
| Cruz [23] | 2011 | Europe, North America, Latin America, South Africa, and Asia Pacific | 275 (155) | 46 (13.1), 44.4 (13.9), 46.9 (13.4) | RCT | NDO | MS154, SCI121 | BTX 200U 92, BTX 300U 91, Placebo 92 | At least 12 |
| Ginsberg [24] | 2012 | USA and Europe | 416 (245) | 46 (13) | RCT | NDO | MS227, SCI189 | BTX 200U 135, BTX 300U 132, Placebo 149 | At least 12 |
| Ginsberg [27] | 2013 | Europe, North America, Latin America, South Africa, and Asia Pacific | 691 (400) | 45.9 | RCT | NDO | MS381, SCI310 | BTX 200U 227, BTX 300U 223, Placebo 241 | At least 12 |
| Rovner [28] | 2013 | Europe, North America, Latin America, South Africa, and Asia Pacific | 691 (400) | 45.9 (13.3), 45.6 (13.0), 46.2 (13.3) | RCT | NDO | MS381, SCI310 | BTX 200U 227, BTX 300U 223, Placebo 241 | At least 12 |
| Tullman [29] | 2018 | Europe, North America | 144 (127) | 51.6 (10.3) | RCT | NDO | MS144 | BTX 100U 66, Placebo 78 | 2, 6, 12 |
| Honda [30] | 2021 | Japan | 21 (4) | 50.9 (14.1), 47.2 (18.3) | RCT | NDO | SCI21 | BTX 200U 11, Placebo 10 | At least 12 |
| Sahai [31] | 2007 | UK | 34 (19) | 49.8, 50.8 | RCT | iOAB | NA | BTX 200U 16, Placebo 18 | 4, 12, 24 |
| Brubaker [32] | 2008 | USA | 43 (43) | 64.7 (14.5), 69.2 (13.5) | RCT | iOAB | NA | BTX 200U 28, Placebo 15 | Within 52 |
| Cohen [33] | 2009 | USA | 44 | NA | RCT | iOAB | NA | BTX 150U 22, BTX 100U 22 | 2, 6, 12, 24 |
| Flynn [34] | 2009 | USA | 22 | 66 | RCT | iOAB | NA | BTX 200U or 300U 15, Placebo 7 | 3, 6 |
| Dmochowski [35] | 2010 | North America, Europe | 313 (288) | 58.8 | RCT | iOAB | NA | BTX 50U 57, BTX 100U 54, BTX 150U 49, BTX 200U 53, BTX 300U 56, Placebo 44 | 2, 6, 12, 18, 24, 30, 36 |
| Altaweel [36] | 2011 | Saudi Arabia | 22 | NA | RCT | iOAB | NA | BTX 100U 11, BTX 200U 11 | 2, 12 |
| Dowson [37] | 2011 | UK | 23 | NA | RCT | iOAB | NA | BTX 100U 10, Placebo 13 | 4, 12 |
| Rovner [38] | 2011 | North America, Europe | 313 (288) | 58.8 | RCT | iOAB | NA | BTX 50U 57, BTX 100U 54, BTX 150U 49, BTX 200U 53, BTX 300U 56, Placebo 44 | 2, 6, 12, 18, 24, 30, 36 |
| Denys [39] | 2012 | France | 99 (87) | 61.6 (14.0) | RCT | iOAB | NA | BTX 50U 23, BTX 100U 23, BTX 150U 30, Placebo 31 | 4, 12, 20, 24 |
| Tincello [40] | 2012 | UK | 240 (240) | 60.7, 58.2 | RCT | iOAB | NA | BTX 200U 122, Placebo 118 | 6, 12, 24 |
| Chapple [41] | 2013 | USA and Europe | 548 (473) | 59.5 (15.5), 59.2 (14.1) | RCT | iOAB | NA | BTX 100U 277, Placebo 271 | Within 24 |
| Nitti [42] | 2013 | USA, Canada | 557 (497) | 61.7 (12.7), 61 (13.1) | RCT | iOAB | NA | BTX 100U 280, Placebo 277 | Within 24 |
| Jabs [43] | 2013 | Canada | 21 (21) | 63 (9.4), 63.8 (11.2) | RCT | iOAB | NA | BTX 100U 11, Placebo 10 | 6, 12, 24 |
| Sievert [44] | 2014 | Europe, North America | 1105 (970) | 60.6 (14.2), 60.1 (13.6) | RCT | iOAB | NA | BTX 100U 557, Placebo 548 | Within 24 |
| Abdelwahab [45] | 2015 | Egypt | 80 (63) | 30.22 (8.37), 31.35 (7.61) | RCT | iOAB | NA | BTX 100U 40, BTX 200U 40 | 4, 12, 24, 36 |
| Herschorn [46] | 2017 | North America, Europe | 356 (308) | 62.0 (12.3) | RCT | iOAB | NA | BTX 100U 145, Solifenacin 151, Placebo 60 | 2, 6, 12, 18, 24 |
| Yokoyama [47] | 2020 | Japan | 248 (186) | 65.6 (12.4), 66.2 (12.2) | RCT | iOAB | NA | BTX 100U 124, Placebo 124 | 12 |
| McCammon [48] | 2021 | USA | 254 (226) | 60.8 (12.4) | RCT | iOAB | NA | BTX 100U 129, Placebo 125 | 12 |
| First Author | Year | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Blinding of Participants and Personnel (Performance Bias) | Blinding of Outcome Assessment (Detection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) | Other Bias |
|---|---|---|---|---|---|---|---|---|
| Schurch | 2005 | Low | Low | Low | Low | Low | Low | Unclear |
| Herschorn | 2011 | Low | Low | Low | Low | Low | Low | Unclear |
| Cruz | 2011 | Low | Low | Low | Low | Low | Low | Unclear |
| Ginsberg | 2012 | Low | Low | Low | Low | Low | Low | Unclear |
| Ginsberg | 2013 | Low | Low | Low | Low | Low | Low | Unclear |
| Rovner | 2013 | Low | Low | Low | Low | Low | Low | Unclear |
| Tullman | 2018 | Low | Low | Low | Low | Low | Low | Unclear |
| Honda | 2021 | Low | Unclear | Low | Low | Low | Low | Unclear |
| Sahai | 2007 | Low | Low | Low | Low | Unclear | Low | Unclear |
| Brubaker | 2008 | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| Cohen | 2009 | Low | Low | Low | Unclear | Low | Low | Unclear |
| Flynn | 2009 | Low | Low | Low | Unclear | Low | Low | Unclear |
| Dmochowski | 2010 | Low | Unclear | Low | Low | Low | Low | Unclear |
| Altaweel | 2011 | Low | Low | Low | Low | Low | Low | Unclear |
| Dowson | 2011 | Low | Low | Low | Low | Unclear | Low | Unclear |
| Rovner | 2011 | Low | Low | Unclear | Low | Low | Low | Unclear |
| Denys | 2012 | Low | Unclear | Low | Low | Low | Low | Unclear |
| Tincello | 2012 | Low | Low | Low | Low | Low | Low | Unclear |
| Chapple | 2013 | Low | Low | Low | Unclear | Low | Low | Unclear |
| Nitti | 2013 | Low | Low | Unclear | Low | Low | Low | Unclear |
| Jabs | 2013 | Unclear | Low | Low | Low | Low | Low | Unclear |
| Sievert | 2014 | Unclear | Low | Low | Unclear | Low | Low | Unclear |
| Abdelwahab | 2015 | Low | Unclear | Low | Unclear | Low | Low | Unclear |
| Herschorn | 2017 | Unclear | Unclear | Low | Low | Low | Low | Unclear |
| Yokoyama | 2020 | Unclear | Low | Low | Low | Low | Low | Unclear |
| McCammon | 2021 | Low | Low | Low | Low | Low | Low | Unclear |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, P.-H.; Wang, C.-C. Adverse Effects of Intravesical OnabotulinumtoxinA Injection in Patients with Idiopathic Overactive Bladder or Neurogenic Detrusor Overactivity: A Systematic Review and Meta-Analysis of Randomized Controlled Studies. Toxins 2024, 16, 343. https://doi.org/10.3390/toxins16080343
Yu P-H, Wang C-C. Adverse Effects of Intravesical OnabotulinumtoxinA Injection in Patients with Idiopathic Overactive Bladder or Neurogenic Detrusor Overactivity: A Systematic Review and Meta-Analysis of Randomized Controlled Studies. Toxins. 2024; 16(8):343. https://doi.org/10.3390/toxins16080343
Chicago/Turabian StyleYu, Ping-Hsuan, and Chung-Cheng Wang. 2024. "Adverse Effects of Intravesical OnabotulinumtoxinA Injection in Patients with Idiopathic Overactive Bladder or Neurogenic Detrusor Overactivity: A Systematic Review and Meta-Analysis of Randomized Controlled Studies" Toxins 16, no. 8: 343. https://doi.org/10.3390/toxins16080343





