Delphi Analysis: Optimizing Anatomy Teaching and Ultrasound Training for Botulinum Neurotoxin Type A Injection in Spasticity and Dystonia
Abstract
1. Introduction
2. Results
2.1. Round 1
2.2. Round 2
2.3. Round 3
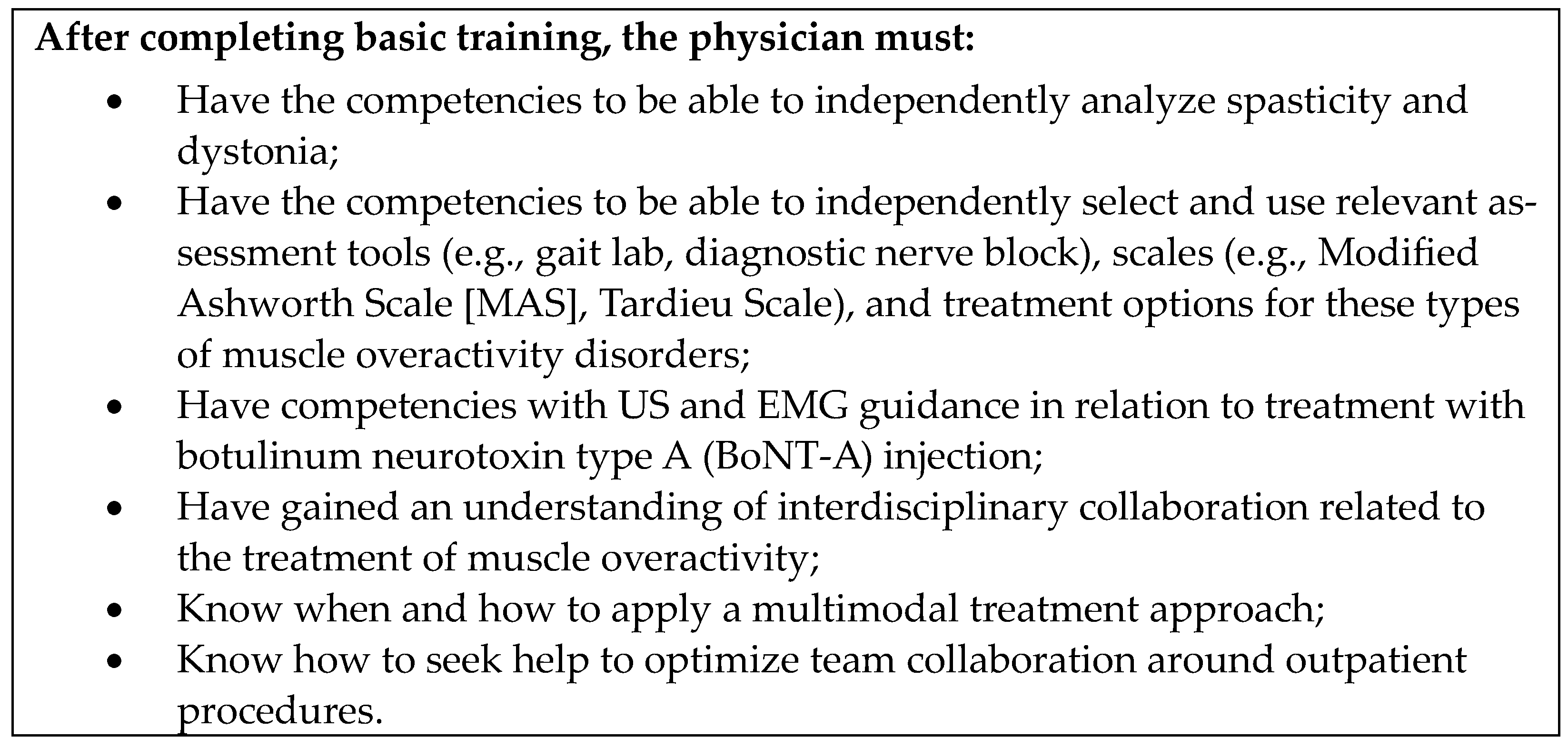
2.4. Consensus Recommendations
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Study Design
5.2. Participants
5.3. Delphi Survey Rounds
5.3.1. Round 1
5.3.2. Round 2
5.3.3. Round 3
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alter, K.E.; Karp, B.I. Ultrasound guidance for botulinum neurotoxin chemodenervation procedures. Toxins 2017, 10, 18. [Google Scholar] [CrossRef]
- Simpson, D.M.; Hallett, M.; Ashman, E.J.; Comella, C.L.; Green, M.W.; Gronseth, G.S.; Armstrong, M.J.; Gloss, D.; Potrebic, S.; Jankovic, J.; et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2016, 86, 1818–1826. [Google Scholar] [CrossRef] [PubMed]
- Fietzek, U.M.; Nene, D.; Schramm, A.; Appel-Cresswell, S.; Košutzká, Z.; Walter, U.; Wissel, J.; Berweck, S.; Chouinard, S.; Bäumer, T. The role of ultrasound for the personalized botulinum toxin treatment of cervical dystonia. Toxins 2021, 13, 365. [Google Scholar] [CrossRef] [PubMed]
- Chung, T.M.; Jacinto, L.J.; Colosimo, C.; Bhatia, K.P.; Tiley, J.; Bhidayasiri, R. Botulinum neurotoxin-A injection in adult cervical dystonia and spastic paresis: Results from the INPUT (INjection Practice, Usage and Training) survey. Front. Neurol. 2020, 11, 570671. [Google Scholar] [CrossRef] [PubMed]
- Asimakidou, E.; Sidiropoulos, C. A Bayesian network meta-analysis and systematic review of guidance techniques in botulinum toxin injections and their hierarchy in the treatment of limb spasticity. Toxins 2023, 15, 256. [Google Scholar] [CrossRef]
- Lapatki, B.G.; van Diyk, J.P.; van de Warrenburg, B.P.C.; Zwarts, M.J. Botulinum toxin has an increased effect when targeted toward the muscle’s endplate zone: A high-density surface EMG guided study. Clin. Neurophysiol. 2011, 122, 1611–1616. [Google Scholar] [CrossRef]
- Heckert, K. (Department of Rehabilitation Medicine, Thomas Jefferson University, Philadelphia, PA, USA); Personal communication, 2024.
- Walter, U. Muscle ultrasound in clinical neurology: Diagnostic uses and guidance of botulinum toxin injection. J. Neurosonol. Neuroimag. 2023, 15, 38–53. [Google Scholar] [CrossRef]
- Wissel, J.; Ward, A.B.; Erztgaard, P.; Bensmail, D.; Hecht, M.J.; Lejeune, T.M.; Schnider, P. European consensus table on the use of botulinum toxin type A in adult spasticity. J. Rehabil. Med. 2009, 41, 13–25. [Google Scholar] [CrossRef]
- Reebye, R.; Balbert, A.; Bensmail, D.; Walker, H.; Wissel, J.; Deltombe, T.; Francisco, G.E. Module 2: Nonsurgical management of spasticity. J. Int. Soc. Phys. Rehabil. Med. 2022, 5, S23–S37. [Google Scholar] [CrossRef]
- Francisco, G.E.; Balbert, A.; Bavikatte, G.; Bensmail, D.; Carda, S.; Deltombe, T.; Draulans, N.; Escaldi, S.; Gross, R.; Jacinto, J.; et al. A practical guide to optimizing the benefits of post-stroke spasticity interventions with botulinum toxin A: An international group consensus. J. Rehabil. Med. 2021, 53, jrm00134. [Google Scholar] [CrossRef]
- Loens, S.; Brüggemann, N.; Steffen, A.; Bäumer, T. Localization of salivary glands for botulinum toxin treatment: Ultrasound versus landmark guidance. Mov. Disord. Clin. Pract. 2019, 7, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Orsini, M.; Leite, M.A.; Chung, T.M.; Bocca, W.; de Souza, J.A.; de Souza, O.G.; Moreira, R.P.; Bastos, V.H.; Teixeira, S.; Oliveira, A.B.; et al. Botulinum neurotoxin type A in neurology: Update. Neurol. Int. 2015, 7, 5886. [Google Scholar] [CrossRef] [PubMed]
- Wissel, J.; Camões-Barbosa, A.; Carda, S.; Hoad, D.; Jacinto, J. A practical guide to botulinum neurotoxin treatment of shoulder spasticity 2: Injection techniques, outcome measurement scales, and case studies. Front. Neurol. 2022, 13, 1022549. [Google Scholar] [CrossRef] [PubMed]
- Escaldi, S.; Bianchi, F.; Bavikatte, G.; Molteni, F.; Moraleda, S.; Deltombe, T.; Francisco, G.E. Module 1: Pathophysiology and assessment of spasticity; goal setting. J. Int. Soc. Phys. Rehabil. Med. 2022, 5, S3–S22. [Google Scholar] [CrossRef]
- Fitterer, J.W.; Picelli, A.; Winston, P. A novel approach to new-onset hemiplegic shoulder pain with decreased range of motion using targeted diagnostic nerve blocks: The ViVe algorithm. Front. Neurol. 2021, 12, 668370. [Google Scholar] [CrossRef]
- Royal College of Physicians, British Society of Rehabilitation Medicine, The Chartered Society of Physiotherapy, Association of Chartered Physiotherapists in Neurology and the Royal College of Occupational Therapists. Spasticity in Adults: Management Using Botulinum Toxin. National Guidelines. 2018. Available online: https://www.rcp.ac.uk/improving-care/resources/spasticity-in-adults-management-using-botulinum-toxin/ (accessed on 30 July 2024).
- Fheodoroff, K.; Bhidayasiri, R.; Jacinto, L.J.; Chung, T.M.; Bhatia, K.; Landreau, T.; Colosimo, C. Ixcellence Network®: An international educational network to improve current practice in the management of cervical dystonia or spastic paresis by botulinum toxin injection. Funct. Neurol. 2017, 32, 103–110. [Google Scholar] [CrossRef]
- Colosimo, C.; Bhidayasiri, R.; Fheodoroff, K.; Bhatia, K.; Chung, T.M.; Landreau, T.; Jacinto, L.J. Management of spastic paresis and cervical dystonia: Access to therapeutic innovations through an international program of practical courses. Clin. Ther. 2019, 41, 2321–2330.e4. [Google Scholar] [CrossRef]
- International Society of Physical and Rehabilitation Medicine. EURO-MUSCULUS Course in Lisbon in December 2019. Available online: https://isprm.org/euro-musculus-course-in-lisbon-in-december-2019/ (accessed on 30 July 2024).
- Scandinavian Education Society for Dystonia and Spasticity Treatment. Courses. Available online: https://www.skandyspas.com/en/kurser (accessed on 30 July 2024).
- DGN (The Botulinum Toxin Working Group of the German Society for Neurology). Available online: https://www.ak-botulinumtoxin.de/ (accessed on 30 July 2024).
- Jourdan, C.; Bévalot, J.; Denormandie, P.; Dionnet, A.; Parratte, B. Training evaluation for a practice in spasticity-related techniques. Ann. Phys. Rehabil. Med. 2015, 58, 114–115. [Google Scholar] [CrossRef]
- American Academy of Physical Medicine and Rehabilitation. STEP Interventional Spasticity Certificate Program. Available online: https://www.aapmr.org/education/step-certificate-programs/step-interventional-spasticity-certificate-program (accessed on 30 July 2024).
- Raja, A.E.; Emam, M.; Shustorovich, A.; Tatini, A.L.; Coslick, A.; Dreher, G.M.; Singh, A.D.; Friedlander, T.; Morice, K.; Kim, S.Y. A hybrid musculoskeletal ultrasound curriculum for physical medicine and rehabilitation residents-a multi-center pilot program. Curr. Phys. Med. Rehabil. Rep. 2023, 11, 51–61. [Google Scholar] [CrossRef]
- Deltombe, T.; Francisco, G.E. Comprehensive curriculum on spasticity assessment and management. J. Int. Soc. Phys. Rehabil. Med. 2022, 5, S1–S2. [Google Scholar] [CrossRef]
- Gross, R.; Verduzco-Gutierrez, M.; Draulans, N.; Zimerman, M.; Francisco, G.E.; Deltombe, T. Module 3: Surgical management of spasticity. J. Int. Soc. Phys. Rehabil. Med. 2022, 5, S38–S49. [Google Scholar] [CrossRef]
- Ketchum, N.; Carda, S.; O’Dell, M.W.; Säterö, P.; Jacinto, J.; Deltombe, T.; Francisco, G.E. Module 4: Optimizing outcomes in spasticity treatment. J. Int. Soc. Phys. Rehabil. Med. 2022, 5, S50–S60. [Google Scholar] [CrossRef]
- Ali, M.F.; Nadeem, N.; Khalid, F.; Anwar, N.M.; Nabie, G.; Docherty, C. SonoGames: Sounds of the right kind introducing gamification into radiology training. BMC Res. Notes 2021, 14, 341. [Google Scholar] [CrossRef]
- Picelli, A.; Tamburin, S.; Bonetti, P.; Fontana, C.; Barausse, M.; Dambruoso, F.; Gajofatto, F.; Santilli, V.; Smania, N. Botulinum toxin type A injection into the gastrocnemius muscle for spastic equinus in adults with stroke: A randomized controlled trial comparing manual needle placement, electrical stimulation and ultrasonography-guided injection techniques. Am. J. Phys. Med. Rehabil. 2012, 91, 957–964. [Google Scholar] [CrossRef]
- Chan, A.K.; Finlayson, H.; Mills, P.B. Does the method of botulinum neurotoxin injection for limb spasticity affect outcomes? A systematic review. Clin. Rehabil. 2017, 31, 713–721. [Google Scholar] [CrossRef]
- Grigoriu, A.I.; Dinomais, M.; Rémy-Néris, O.; Brochard, S. Impact of injection-guiding techniques on the effectiveness of botulinum toxin for the treatment of focal spasticity and dystonia: A systematic review. Arch. Phys. Med. Rehabil. 2015, 96, 2067–2078.e1. [Google Scholar] [CrossRef]
- Shang, Z. Use of Delphi in health sciences research: A narrative review. Medicine 2023, 102, e32829. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, S.H.; Khan, M.M.; Patrick-Smith, M.; Martinez-Devesa, P.; Stapleton, E.; Williams, O.M.; Pretorius, P.; McNally, M.; Andersson, M.I. UK consensus definitions for necrotising otitis externa: A Delphi study. BMJ Open 2023, 13, e061349. [Google Scholar] [CrossRef]
- Rahaghi, F.F.; Baughman, R.P.; Saketkoo, L.A.; Sweiss, N.J.; Barney, J.B.; Birring, S.S.; Costabel, U.; Crouser, E.D.; Drent, M.; Gerke, A.K.; et al. Delphi consensus recommendations for a treatment algorithm in pulmonary sarcoidosis. Eur. Respir. Rev. 2020, 29, 190146. [Google Scholar] [CrossRef]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS ONE 2011, 6, e20476. [Google Scholar] [CrossRef]
- Krämer, J.; Baerwald, C.; Heimbold, C.; Kamrath, C.; Parhofer, K.G.; Reichert, A.; Rutsch, F.; Stolz, S.; Weinhold, N.; Muntau, A.C. Two years of pegvaliase in Germany: Experiences and best practice recommendations. Mol. Genet. Metab. 2023, 139, 107564. [Google Scholar] [CrossRef] [PubMed]
- Watson, K.E.; Dhaliwal, K.; Robertshaw, S.; Verdin, N.; Benterud, E.; Lamont, N.; Drall, K.M.; McBrien, K.; Donald, M.; Tsuyuki, R.T.; et al. Consensus recommendations for sick day medication guidance for people with diabetes, kidney, or cardiovascular disease: A modified Delphi process. Am. J. Kidney Dis. 2023, 81, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Hai, Y.; Liu, J.; Liu, Y.; Liu, T.; Zhang, X.; Pan, A.; Zhang, Y.; Ding, H.; Wu, Y.; Han, B.; et al. Expert consensus on clinical application of lateral lumbar interbody fusion: Results from a modified Delphi study. Global Spine J. 2023, 13, 995–1004. [Google Scholar] [CrossRef] [PubMed]
- Bodó, I.; Amine, I.; Boban, A.; Bumbea, H.; Kulagin, A.; Lukina, E.; Piekarska, A.; Zupan, I.P.; Sokol, J.; Windyga, J.; et al. Complement inhibition in paroxysmal nocturnal hemoglobinuria (PNH): A systematic review and expert opinion from central Europe on special patient populations. Adv. Ther. 2023, 40, 2752–2772. [Google Scholar] [CrossRef]
- Feo, R.; Conroy, T.; Jangland, E.; Muntlin Athlin, Å.; Brovall, M.; Parr, J.; Blomberg, K.; Kitson, A. Towards a standardised definition for fundamental care: A modified Delphi study. J. Clin. Nurs. 2018, 27, 2285–2299. [Google Scholar] [CrossRef]
- Lagnau, P.; Lo, A.; Sandarage, R.; Alter, K.; Picelli, A.; Wissel, J.; Verduzco-Gutierrez, M.; Suputtitada, A.; Munin, M.C.; Carda, S.; et al. Ergonomic recommendations in ultrasound-guided botulinum neurotoxin chemodenervation for spasticity: An international expert group opinion. Toxins 2021, 13, 249. [Google Scholar] [CrossRef]
- Eubank, B.H.; Mohtadi, N.G.; Lafave, M.R.; Wiley, J.P.; Bois, A.J.; Boorman, R.S.; Sheps, D.M. Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med. Res. Methodol. 2016, 16, 56. [Google Scholar] [CrossRef]
- Barlassina, A.; González-López, T.J.; Cooper, N.; Zaja, F. European Delphi panel to build consensus on tapering and discontinuing thrombopoietin receptor agonists in immune thrombocytopenia. Platelets 2023, 34, 2170999. [Google Scholar] [CrossRef]
- Boel, A.; Navarro-Compán, V.; Landewé, R.; van der Heijde, D. Two different invitation approaches for consecutive rounds of a Delphi survey led to comparable final outcome. J. Clin. Epidemiol. 2021, 129, 31–39. [Google Scholar] [CrossRef]
- Jones, J.; Hunter, D. Consensus methods for medical and health services research. BMJ 1995, 311, 376–380. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Sandford, B.A. The Delphi technique: Making sense of consensus. Pract. Assess. Res. Eval. 2007, 12, 10. [Google Scholar] [CrossRef]
- Nasa, P.; Jain, R.; Juneja, D. Delphi methodology in healthcare research: How to decide its appropriateness. World J. Methodol. 2021, 11, 116–129. [Google Scholar] [CrossRef] [PubMed]

| Statement | Consensus Level |
|---|---|
| Consensus | |
| 100% |
| 100% |
| 100% |
| 100% |
| 100% |
| 88% |
| 89% |
| 100% |
| 100% |
| 100% |
| 100% |
| 89% |
| 100% |
| 100% |
| 89% |
| 89% |
| 89% |
| 88% |
| 88% |
| 100% |
| 100% |
| 100% |
| 100% |
| 100% |
| 100% |
| 88% |
| 100% |
| No consensus | |
| 78% |
| Advantages of Using Cadavers | |
|---|---|
| Cadaver dissection allows for a detailed understanding of muscle anatomy, including the size, shape, and location of individual muscles and their relationship to surrounding structures. This is crucial when targeting specific muscles for injection of BoNT-A. |
| Cadaver dissection can help clinicians understand the nerve supply to different muscles. This is important for BoNT-A injections, as the toxin must be injected directly into affected muscles to maximize effectiveness. Furthermore, comprehensive understanding of muscle nerve supply allows clinicians to practice diagnostic nerve blocks, which can be an important part of patient assessment. This knowledge also has broader implications for current and developing spasticity treatments, such as chemoneurolysis and cryolysis. |
| Cadavers can provide an opportunity to practice injection techniques in a realistic setting. This can help clinicians improve their skills and become more comfortable with the procedure. |
| Each human body is unique. By studying cadavers, clinicians can gain a better understanding of the variations that exist in human anatomy, which can help them tailor their injection techniques to individual patients. |
| In some cases, the muscles affected by post-stroke spasticity may be deep within the body. Cadaver dissection can help clinicians visualize these deep structures and understand how to target them with BoNT-A injections. |
| Understanding the precise location of muscles, nerves, and blood vessels can help prevent complications, such as injecting the toxin into blood vessels or causing damage to nerves during BoNT-A administration. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heckert, K.; Biering-Sørensen, B.; Bäumer, T.; Khan, O.; Pagan, F.; Paulin, M.; Stitik, T.; Verduzco-Gutierrez, M.; Reebye, R. Delphi Analysis: Optimizing Anatomy Teaching and Ultrasound Training for Botulinum Neurotoxin Type A Injection in Spasticity and Dystonia. Toxins 2024, 16, 371. https://doi.org/10.3390/toxins16080371
Heckert K, Biering-Sørensen B, Bäumer T, Khan O, Pagan F, Paulin M, Stitik T, Verduzco-Gutierrez M, Reebye R. Delphi Analysis: Optimizing Anatomy Teaching and Ultrasound Training for Botulinum Neurotoxin Type A Injection in Spasticity and Dystonia. Toxins. 2024; 16(8):371. https://doi.org/10.3390/toxins16080371
Chicago/Turabian StyleHeckert, Kimberly, Bo Biering-Sørensen, Tobias Bäumer, Omar Khan, Fernando Pagan, Mitchell Paulin, Todd Stitik, Monica Verduzco-Gutierrez, and Rajiv Reebye. 2024. "Delphi Analysis: Optimizing Anatomy Teaching and Ultrasound Training for Botulinum Neurotoxin Type A Injection in Spasticity and Dystonia" Toxins 16, no. 8: 371. https://doi.org/10.3390/toxins16080371
APA StyleHeckert, K., Biering-Sørensen, B., Bäumer, T., Khan, O., Pagan, F., Paulin, M., Stitik, T., Verduzco-Gutierrez, M., & Reebye, R. (2024). Delphi Analysis: Optimizing Anatomy Teaching and Ultrasound Training for Botulinum Neurotoxin Type A Injection in Spasticity and Dystonia. Toxins, 16(8), 371. https://doi.org/10.3390/toxins16080371





